What is venous thromboembolism
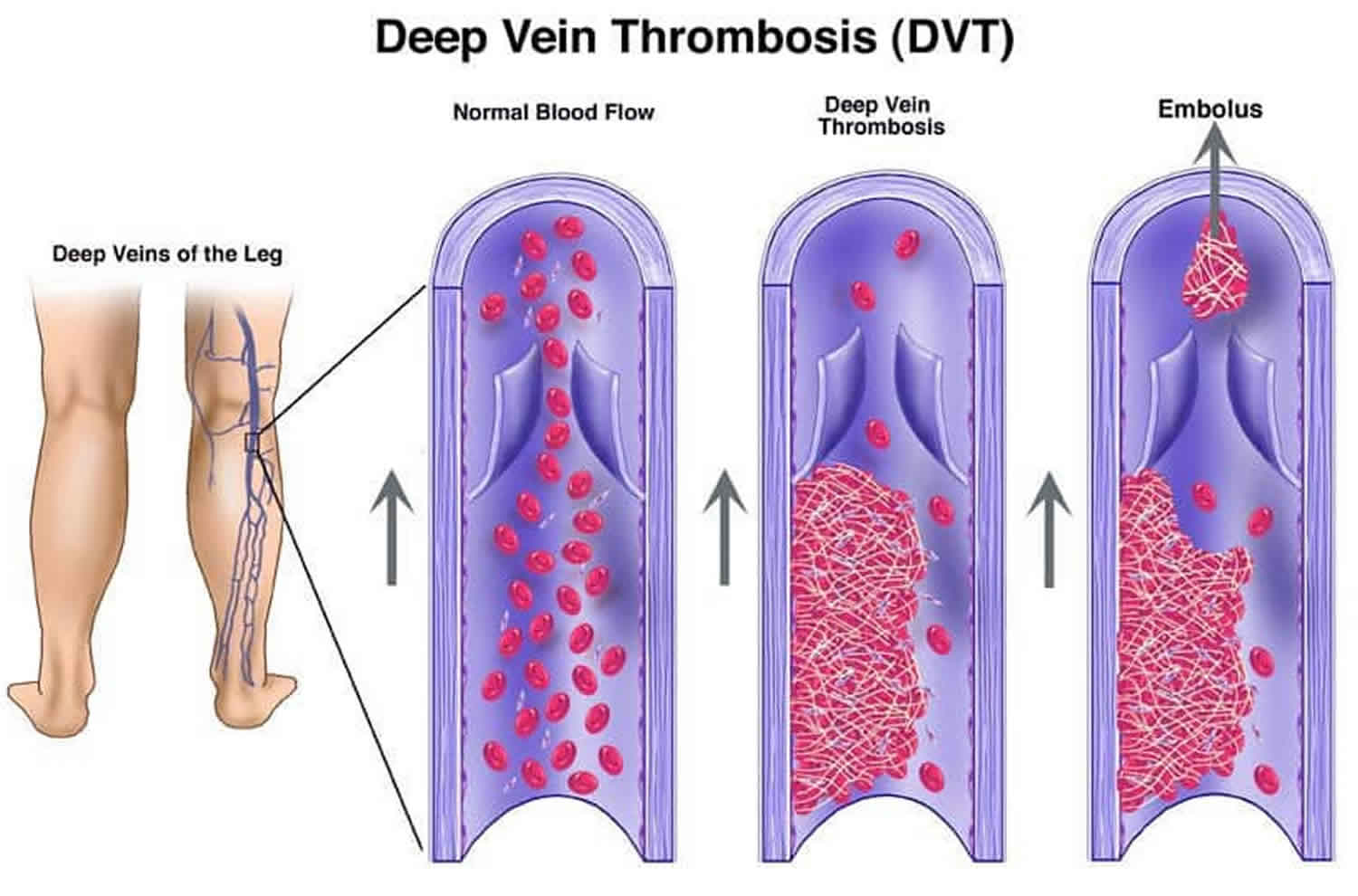
Venous thromboembolism (VTE) is a term referring to blood clot (a thrombus) in the veins. Venous thromboembolism describes two related conditions: deep vein thrombosis (DVT) and a more serious complication called pulmonary embolism (PE), which is an emergency. A deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in the lower leg, thigh, or pelvis. A pulmonary embolism (PE) occurs when a clot breaks loose and travels through the bloodstream to the lungs. Both are blood clots in the veins and highly preventable. There are ways to prevent and treat venous thromboembolism, but you can help identify the warning signs of venous thromboembolism to save lives.
The risk of developing venous thromboembolism is highest after major surgery or a major injury, or when you have heart failure, cancer, or a heart attack. Swelling, redness, and pain are some of the signs and symptoms of deep vein thrombosis. A pulmonary embolism can cause sudden chest pain and shortness of breath. Sometimes venous thromboembolism occurs without any obvious signs. Medicines that help prevent further blood clots from forming or that dissolve serious vein blockages are the main treatments for venous thromboembolism. Without treatment, venous thromboembolism can restrict or block blood flow and oxygen, which can damage the body’s tissue or organs. This can be especially serious in the case of a pulmonary embolism, which blocks blood flow to the lungs. If a blood clot is large or there are many clots, a pulmonary embolism can cause death.
Many factors can put you at risk for venous thromboembolism. Some of these factors seem obvious—lengthy surgery (especially orthopedic), pregnancy, being over age 40 and not exercising, cancer, obesity, use of birth control pills, hormone replacement therapy, family history of deep vein thrombosis (DVT), long distance travel (especially on airplanes) and spinal cord injuries. Others may not be as obvious such as heart failure, some types of lung disease, kidney disease, infections and other inflammatory diseases increase your risk. Smoking increases clotting risk as do obesity and inherited clotting conditions. These risk factors are additive: the more you have, the greater your risk. If you have several risk factors, such as a planned or a recent surgery, a fracture, been on bed rest, or will be immobilized for any length of time, you may want to discuss venous thromboembolism with your health care provider and develop a plan for preventing blood clots.
Deep vein thrombosis (DVT)
Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein. These clots usually develop in the lower leg or calf and can extend to involve the large deep veins of the upper legs or thighs, but they can also occur in the arm. Only rarely does DVT occur in an arm and usually occurs because of intravenous (IV) access lines, or in athletic individuals due to repetitive injury. It is important to know about DVT because it can happen to anybody and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
Your legs and arms have two major types of veins: superficial and deep. The superficial veins are near the surface of the skin where they are sometimes visible, whereas the deep veins are located near the bones and are surrounded by muscle. Contraction or squeezing of the muscles around the deep veins sends blood back to the heart. A blood clot that develops in a deep vein can block this flow of blood and may or may not cause symptoms. DVT is not usually life threatening, but it can be if the blood clots break loose and go into the lungs. This condition is known as pulmonary embolism (PE) which can be fatal if the traveling blood clot, called an “embolus,” clogs the main lung arteries. Many people die in the first hour from a pulmonary embolism (PE), about 100,000 death in the United States each year, making it the third most common cause of vascular death.
DVT can cause leg swelling that is usually treated with 3-6 months of a blood thinner. A long-term side effect of DVT is the development of the postthrombotic syndrome. About one-third of patients who experience a DVT (a higher percentage if the clot goes into the large veins in the pelvis or abdomen) can develop postthrombotic syndrome even after treatment with blood thinners. This condition can show up months to years later as chronic pain, swelling and discoloration of the leg, as well as the development of open sores or ulcers, caused by damage that is done by the clot to valves in the veins. The effects of postthrombotic syndrome can be long lasting and can lessen one’s quality of life.
Risk Factors for DVT
Almost anyone can have a DVT. However, certain factors can increase the chance of having this condition. The chance increases even more for someone who has more than one of these factors at the same time.
Following is a list of factors that increase the risk of developing DVT:
- Injury to a vein, often caused by:
- Fractures,
- Severe muscle injury, or
- Major surgery (particularly involving the abdomen, pelvis, hip, or legs).
- Slow blood flow, often caused by:
- Confinement to bed (e.g., due to a medical condition or after surgery);
- Limited movement (e.g., a cast on a leg to help heal an injured bone);
- Sitting for a long time, especially with crossed legs; or
- Paralysis.
- Increased estrogen, often caused by:
- Birth control pills
- Hormone replacement therapy, sometimes used after menopause
- Pregnancy, for up to 3 months after giving birth
- Certain chronic medical illnesses, such as:
- Heart disease
- Lung disease
- Cancer and its treatment
- Inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
- Other factors that increase the risk of DVT include:
- Previous DVT or pulmonary embolism (PE)
- Family history of DVT or pulmonary embolism (PE)
- Age (risk increases as age increases)
- Obesity
- A catheter located in a central vein
- Inherited clotting disorders
Pulmonary embolism
Pulmonary embolism occurs when a clump of material, most often a blood clot (thrombus or embolus), gets wedged in one of the pulmonary arteries in your lungs. These blood clots most commonly come from the deep veins of your legs and rarely from other parts of your body. This condition is known as deep vein thrombosis (DVT).
In most cases, multiple clots are involved but not necessarily all at once. The portions of lung served by each blocked artery are robbed of blood and may die. This is known as pulmonary infarction. This makes it more difficult for your lungs to provide oxygen to the rest of your body.
Occasionally, blockages in the blood vessels are caused by substances other than blood clots, such as:
- Fat from the marrow of a broken long bone
- Collagen or other tissue
- Part of a tumor
- Air bubbles
Because the clots block blood flow to the lungs, pulmonary embolism can be life-threatening. About one-third of people with undiagnosed and untreated pulmonary embolism don’t survive. When the condition is diagnosed and treated promptly, however, that number drops dramatically.
Pulmonary embolism can also lead to pulmonary hypertension, a condition in which the blood pressure in your lungs and in the right side of the heart is too high. When you have obstructions in the arteries inside your lungs, your heart must work harder to push blood through those vessels. This increases the blood pressure within these vessels and the right side of the heart, which can weaken your heart.
In rare cases, small emboli occur frequently and develop over time, resulting in chronic pulmonary hypertension, also known as chronic thromboembolic pulmonary hypertension.
Pulmonary embolism symptoms can vary greatly, depending on how much of your lung is involved, the size of the clots, and whether you have underlying lung or heart disease.
Pulmonary embolism common signs and symptoms include:
- Shortness of breath. This symptom typically appears suddenly and always gets worse with exertion.
- Chest pain. You may feel like you’re having a heart attack. The pain may become worse when you breathe deeply (pleurisy), cough, eat, bend or stoop. The pain will get worse with exertion but won’t go away when you rest.
- Cough. The cough may produce bloody or blood-streaked sputum.
Other signs and symptoms that can occur with pulmonary embolism include:
- Leg pain or swelling, or both, usually in the calf
- Clammy or discolored skin (cyanosis)
- Fever
- Excessive sweating
- Rapid or irregular heartbeat
- Lightheadedness or dizziness
Risk factors for getting pulmonary embolism
Although anyone can develop blood clots and subsequent pulmonary embolism, certain factors can increase your risk.
You’re at higher risk if you or any of your family members have had venous blood clots or pulmonary embolism in the past. This may be due to inherited disorders that affect blood, making it more prone to clot.
In addition, some medical conditions and treatments put you at risk, such as:
- Heart disease. Cardiovascular disease, specifically heart failure, makes clot formation more likely.
- Cancer. Certain cancers — especially pancreatic, ovarian and lung cancers, and many cancers with metastasis — can increase levels of substances that help blood clot, and chemotherapy further increases the risk. Women with a personal or family history of breast cancer who are taking tamoxifen or raloxifene also are at higher risk of blood clots.
- Surgery. Surgery is one of the leading causes of problem blood clots. For this reason, medication to prevent clots may be given before and after major surgery such as joint replacement.
Prolonged immobility
Blood clots are more likely to form during periods of inactivity, such as:
- Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness makes you more vulnerable to blood clots. When the lower extremities are horizontal for long periods, the flow of venous blood slows and blood can pool in the legs.
- Long trips. Sitting in a cramped position during lengthy plane or car trips slows blood flow in the legs, which contributes to the formation of clots.
Other risk factors
- Smoking. For reasons that aren’t well-understood, tobacco use predisposes some people to blood clot formation, especially when combined with other risk factors.
- Being overweight. Excess weight increases the risk of blood clots — particularly in women who smoke or have high blood pressure.
- Supplemental estrogen. The estrogen in birth control pills and in hormone replacement therapy can increase clotting factors in your blood, especially if you smoke or are overweight.
- Pregnancy. The weight of the baby pressing on veins in the pelvis can slow blood return from the legs. Clots are more likely to form when blood slows or pools.
Venous thromboembolism prophylaxis
The following tips can help prevent DVT (deep vein thrombosis):
- Move around as soon as possible after having been confined to bed, such as after surgery, illness, or injury.
- If you’re at risk for DVT, talk to your doctor about:
- Graduated compression stockings (sometimes called “medical compression stockings”)
- Medication (anticoagulants) to prevent DVT.
- When sitting for long periods of time, such as when traveling for more than four hours:
- Get up and walk around every 2 to 3 hours.
- Exercise your legs while you’re sitting by:
- Raising and lowering your heels while keeping your toes on the floor
- Raising and lowering your toes while keeping your heels on the floor
- Tightening and releasing your leg muscles
- Wear loose-fitting clothes.
- You can reduce your risk by maintaining a healthy weight, avoiding a sedentary lifestyle, and following your doctor’s recommendations based on your individual risk factors.
Preventing clots in the deep veins in your legs (deep vein thrombosis) will help prevent pulmonary embolism. For this reason, most hospitals are aggressive about taking measures to prevent blood clots, including:
- Blood thinners (anticoagulants). These medications are often given to people at risk of clots before and after an operation — as well as to people admitted to the hospital with a heart attack, stroke or complications of cancer.
- Compression stockings. Compression stockings steadily squeeze your legs, helping your veins and leg muscles move blood more efficiently. They offer a safe, simple and inexpensive way to keep blood from stagnating during and after general surgery.
- Leg elevation. Elevating your legs when possible and during the night also can be very effective. Raise the bottom of your bed 4 to 6 inches with blocks or books.
- Physical activity. Moving as soon as possible after surgery can help prevent pulmonary embolism and hasten recovery overall. This is one of the main reasons your nurse may push you to get up, even on your day of surgery, and walk despite pain at the site of your surgical incision.
- Pneumatic compression. This treatment uses thigh-high or calf-high cuffs that automatically inflate with air and deflate every few minutes to massage and squeeze the veins in your legs and improve blood flow.
Prevention while traveling
The risk of blood clots developing while traveling is low, but increases as travel increases. If you have risk factors for blood clots and you’re concerned about traveling, talk with your doctor.
Your doctor might suggest the following to help prevent blood clots during travel:
- Drink plenty of fluids. Water is the best liquid for preventing dehydration, which can contribute to the development of blood clots. Avoid alcohol, which contributes to fluid loss.
- Take a break from sitting. Move around the airplane cabin once an hour or so. If you’re driving, stop every hour and walk around the car a couple of times.
- Do a few deep knee bends.
- Fidget in your seat. Flex your ankles every 15 to 30 minutes.
- Wear support stockings. Your doctor may recommend these to help promote circulation and fluid movement in your legs. Compression stockings are available in a range of stylish colors and textures. There are even devices, called stocking butlers, to help you put on the stockings.
Venous thromboembolism symptoms
Deep vein thrombosis (DVT) signs and symptoms
People with DVT may develop pain, swelling and tenderness. Only about half the people with DVT have typical symptoms, so diagnosis is difficult. A big misconception is that there should be something visible with DVT. Most DVTs are associated with leg pain or mild swelling only, and the perception that there should be obvious symptoms has likely resulted in many delayed or missed diagnoses of venous thromboembolism. It is the combination of risk factors and these symptoms that is important.
When symptoms do occur the most common are:
- Sudden swelling of one leg. Rarely, there’s swelling in both legs.
- Pain or tenderness in the calf muscle or groin. The pain often starts in your calf and can feel like cramping or soreness.
- Skin that is warm to the touch on the legs
- Fullness of the veins just beneath the skin (seeing these veins more easily or if they look swollen)
- Changes in skin color (blue, red or very pale)
Symptoms like these can develop slowly, but can also develop suddenly. These symptoms are not unique to DVT and can be associated with other conditions. If you have these symptoms you should contact your health care provider immediately.
Pulmonary embolism signs and symptoms
Signs and symptoms of pulmonary embolism occur quickly and need prompt attention. The symptoms of pulmonary embolism are different than for DVT.
Pulmonary embolism symptoms include:
- Shortness of breath
- Sharp chest pain usually with breathing in or when taking a deep breath
- A feeling of apprehension
- Sudden collapse or fainting
- Rapid pulse
- Coughing
- Sweating
- Bloody phlegm (coughing up blood)
These symptoms are not unique to pulmonary embolism and can be associated with many other conditions. Unfortunately, a majority of people with pulmonary embolism, unlike DVT, will experience uncommon symptoms such as dizziness, back pain or wheezing. However, because pulmonary embolism can be fatal, if you experience these signs or symptoms seek medical attention right away.
Venous thromboembolism diagnosis
To diagnose deep vein thrombosis, your doctor will ask you about your symptoms. You’ll also have a physical exam so that your doctor can check for areas of swelling, tenderness or discoloration on your skin. Depending on how likely you are to have a blood clot, your doctor might suggest tests, including:
- Ultrasound. The easiest and most reliable method for diagnosing deep vein thrombosis is an ultrasound exam. This test is simple, painless, safe and widely available. A wandlike device (transducer) placed over the part of your body where there’s a clot sends sound waves into the area. As the sound waves travel through your tissue and reflect back, a computer transforms the waves into a moving image on a video screen. A clot might be visible in the image. Sometimes a series of ultrasounds are done over several days to determine whether a blood clot is growing or to check for a new one.
- Blood test. Almost all people who develop severe deep vein thrombosis have an elevated blood level of a substance called “D-dimer”. A specific blood test may be performed to measure “D-dimer” which is a sign of recent and active clotting. When this test is negative, it is very unlikely that you have suffered a DVT.
- Venography. A dye is injected into a large vein in your foot or ankle. An X-ray creates an image of the veins in your legs and feet, to look for clots. However, less invasive methods of diagnosis, such as ultrasound, can usually confirm the diagnosis.
- CT or MRI scans. Either can provide visual images of your veins and might show if you have a clot. Sometimes these scans performed for other reasons reveal a clot.
Pulmonary embolism may be diagnosed by a special type of chest CT scan, a lung scan or less commonly by an invasive procedure known as a pulmonary angiogram.
- Spiral CT scan: In a spiral (helical) CT scan, the scanner rotates around your body in a spiral — like the stripe on a candy cane — to create 3-D images. This type of CT can detect abnormalities within the arteries in your lungs with much greater precision than conventional CT scans. In some cases, contrast material is given intravenously during the CT scan to outline the pulmonary arteries.
- Pulmonary angiogram: Pulmonary angiogram test provides a clear picture of the blood flow in the arteries of your lungs. It’s the most accurate way to diagnose pulmonary embolism, but because it requires a high degree of skill to administer and has potentially serious risks, it’s usually performed when other tests fail to provide a definitive diagnosis. In a pulmonary angiogram, a flexible tube (catheter) is inserted into a large vein — usually in your groin — and threaded through into your heart and on into the pulmonary arteries. A special dye is then injected into the catheter, and X-rays are taken as the dye travels along the arteries in your lungs. One risk of this procedure is a temporary change in your heart rhythm. In addition, the dye may cause kidney damage in people with decreased kidney function.
- MRI scan: MRI scans use radio waves and a powerful magnetic field to produce detailed images of internal structures. Because MRI is expensive, it’s usually reserved for pregnant women (to avoid radiation to the fetus) and people whose kidneys may be harmed by dyes used in other tests.
Venous thromboembolism treatment
Deep vein thrombosis (DVT) treatment
Deep vein thrombosis (DVT) treatment is aimed at preventing the clot from getting bigger and preventing it from breaking loose and causing a pulmonary embolism. Then the goal becomes reducing your chances of deep vein thrombosis happening again.
Deep vein thrombosis treatment options include:
- Blood thinners. Deep vein thrombosis is most commonly treated with anticoagulants, also called blood thinners. These drugs, which can be injected or taken as pills, decrease your blood’s ability to clot. They don’t break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots. The injectable medications can be given as a shot under the skin or by injection into your arm vein (intravenous). Heparin is typically given intravenously. Other similar blood thinners, such as enoxaparin (Lovenox), dalteparin (Fragmin) or fondaparinux (Arixtra), are injected under the skin. You might receive an injectable blood thinner for a few days, after which pills such as warfarin (Coumadin, Jantoven) or dabigatran (Pradaxa) are started. Once warfarin has thinned your blood, the injectable blood thinners are stopped. Other blood thinners can be given in pill form without the need for an injectable blood thinner. These include rivaroxaban (Xarelto), apixaban (Eliquis) or edoxaban (Savaysa). You might need to take blood thinner pills for three months or longer. It’s important to take them exactly as your doctor instructs because taking too much or too little can cause serious side effects. If you take warfarin, you’ll need periodic blood tests to check how long it takes your blood to clot. Pregnant women shouldn’t take certain blood-thinning medications.
- Clot busters. If you have a more serious type of deep vein thrombosis or pulmonary embolism, or if other medications aren’t working, your doctor might prescribe drugs that break up clots quickly, called clot busters or thrombolytics. These drugs are either given through an IV line to break up blood clots or through a catheter placed directly into the clot. These drugs can cause serious bleeding, so they’re generally reserved for severe cases of blood clots.
- Filters. If you can’t take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs.
- Compression stockings. To help prevent swelling associated with deep vein thrombosis, these are worn on your legs from your feet to about the level of your knees. This pressure helps reduce the chances that your blood will pool and clot. You should wear these stockings during the day for at least two years, if possible.
Once you receive treatment for deep vein thrombosis (DVT), you need to watch your diet and watch for signs of excessive bleeding, as well as take steps to prevent another DVT. Some things you can do include:
- Check in with your doctor regularly to see if your treatment needs to be modified. If you’re taking warfarin (Coumadin, Jantoven), you’ll need a blood test to see how well your blood is clotting.
- Take your blood thinners as directed. If you’ve had DVT, you’ll be on blood thinners for at least three to six months.
- Watch for excessive bleeding, which can be a side effect of taking blood thinners. Talk to your doctor about activities that could cause you to bruise or get cut, as even a minor injury could become serious if you’re taking blood thinners.
- Move. If you’ve been on bed rest because of surgery or other factors, the sooner you get moving, the less likely blood clots will develop.
- Wear compression stockings to help prevent blood clots in the legs if your doctor recommends them.
Pulmonary embolism treatment
Pulmonary embolism treatment is aimed at keeping the blood clot from getting bigger and preventing new clots from forming. Prompt treatment is essential to prevent serious complications or death.
Medications
- Blood thinners (anticoagulants). These drugs prevent new clots from forming while your body works to break up the clots. Heparin is a frequently used anticoagulant that can be given through the vein or injected under the skin. It acts quickly and is often overlapped for several days with an oral anticoagulant, such as warfarin, until it becomes effective, which can take days. A newer class of anticoagulants, referred to as novel oral anticoagulants (NOACs), has been tested and approved for treatment of venous thromboembolism, including pulmonary embolism. These medications work quickly and have fewer interactions with other medications. Some NOACs have the advantage of being given by mouth, without the need for overlap with heparin. However, all anticoagulants have side effects, with bleeding being the most common.
- Clot dissolvers (thrombolytics). While clots usually dissolve on their own, there are medications given through the vein that can dissolve clots quickly. Because these clot-busting drugs can cause sudden and severe bleeding, they usually are reserved for life-threatening situations.
Surgical and other procedures
- Clot removal (thrombectomy or embolectomy). If you have a very large, life-threatening clot in your lung, your doctor may suggest removing it via a thin, flexible tube (catheter) threaded through your blood vessels.
- Vein filter. A catheter can also be used to position a filter in the body’s main vein — called the inferior vena cava — that leads from your legs to the right side of your heart. This filter can help keep clots from being carried into your lungs. This procedure is typically reserved for people who can’t take anticoagulant drugs or when anticoagulant drugs don’t work well enough or fast enough. Some filters can be removed when they are no longer needed.