What is thyroglossal duct cyst
Thyroglossal duct cyst or thyroglossal cyst, is a rare hereditary form of a benign congenital (present at birth) neck mass. Thyroglossal cyst is the most common congenital midline neck mass in children 1, accounting for >70–75% of these masses 2. Thyroglossal duct cysts are caused by abnormal development and migration of the cells forming the thyroid gland between the 4th and 8th week of fetal development 3. The thyroglossal duct is the area in which the cells that form the thyroid gland migrate during fetal development. It typically closes off and dissolves before birth, but may remain open in some individuals. When the thyroglossal duct fails to dissolve completely, a cyst (fluid filled sac) may form. It is not clear why occurs in some individuals. The cause of this abnormal development is largely not known and usually sporadic; however, in rare circumstances thyroglossal cysts can be inherited. Familial thyroglossal cyst are commonly inherited in an autosomal dominant pattern with rare reports of autosomal recessive inheritance 4.
Thyroglossal duct cysts can form anywhere along the thyroid’s route of migration from the tongue base to the inferior neck 5. Thyroglossal duct cysts often present as midline neck cysts closely associated with the hyoid bone 6.
Thyroglossal duct cyst usually presents in children, around 6 years of age, but rarely, they may present in adulthood 3. Thyroglossal duct cyst presents as a painless, palpable mass that develops around the midline and moves with swallowing. Other symptoms might include: fluctuation in size of mass, dysphagia, infection of mass, and mid-neck tenderness 1.
Thyroglossal duct cysts are present in about 7% of the adult population worldwide 7. They have an equal preponderance between male and female individuals. Although they are known to be the most common neck mass in children, thyroglossal duct cysts also present in adults with varying frequency. These types of cysts are closely associated with the hyoid bone. Thyroglossal duct cysts are about 20% to 25% present at the level of suprahyoid, 15% to 20% present at the level of hyoid, and 25% to 65 % present at the infrahyoid level 8.
Thyroglossal duct cysts are cystic structures lined by respiratory epithelium, squamous epithelium, or a combination of both 5. Due to a high frequency of infection, inflammatory infiltrates can be present. These can appear as granulation tissue or giant cells. In about 70% of cases, microscopic foci of ectopic thyroid gland tissue can be found, usually within the cyst wall.
Thyroglossal duct cyst treatment involves surgery to remove the cyst (mass) 1. However, if the cyst is infected, a surgical procedure should not be done until the infection is treated. Removing an infected cyst without adequately treating the infection can result in a more difficult surgery. If your child has an infected thyroglossal duct cyst, antibiotics will be prescribed to treat the infection before moving forward with surgical excision.
The surgical procedure to excise a thyroglossal duct cyst is called the Sistrunk procedure and is performed under general anesthesia. The procedure is usually a day surgery, meaning that your child will be able to go home the same day as the procedure.
A small incision is made over the cyst. The cyst and the entire tract are removed, as well as the middle portion of the hyoid bone, a small horseshoe-shaped bone that is found in the neck below the chin. It is important that the cyst and the attached tract are completely removed. If a portion is left, the cyst has a higher likelihood of recurrence, or coming back.
Any tissue that is removed will be sent to the pathology lab to confirm the diagnosis. The incision will be closed with dissolvable sutures with either DERMABOND (skin glue) or steri-strips on the skin. DERMABOND is a sterile, liquid adhesive that will hold the edges of your child’s wound together and act as a waterproof dressing. It usually stays in place for 5-10 days before it starts to fall off. You should not pick, peel or rub the DERMABOND, as this could cause your child’s wound to open before it is healed.
Once it sets, the adhesive can get wet (as in a shower) the same day as the procedure, but should not routinely be submerged under water (as in swimming) for 5-10 days. Do not apply any ointments such as Vaseline or Neosporin to the incision while the DERMABOND is in place.
After surgery, your child will recover in the General Surgery recovery area until he or she is stable and able to swallow without difficulty. Your child will be sent home on oral pain medication.
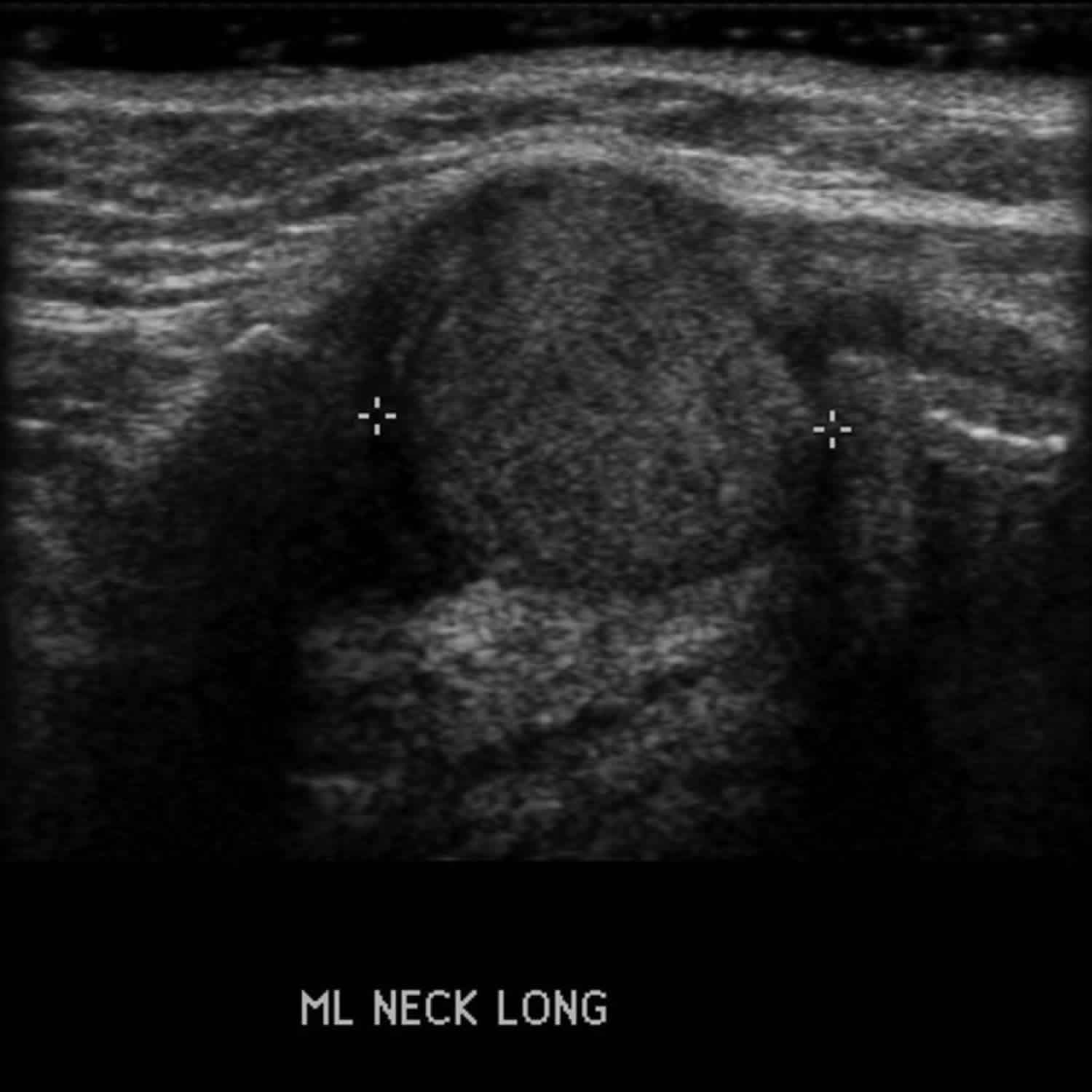
Figure 1. Thyroglossal duct cyst
Figure 2. Thyroglossal duct cyst CT scan
Figure 3. Thyroglossal duct cyst ultrasound
Thyroglossal duct cyst cancer
Less than 1% of thyroglossal duct cysts develop into a carcinoma 5. Papillary carcinoma is the most common malignancy found (92.1%) followed by squamous cell carcinoma (4.3%) 5. Thyroglossal duct cyst carcinoma typically presents with an asymptomatic midline neck mass. 73.3% of these types of carcinomas were diagnosed as an incidental finding on final pathologic analysis. Patients diagnosed with thyroglossal duct cyst carcinoma tend to be adults and have an older average age than the typical thyroglossal duct cyst patient. Treatment of thyroglossal duct cyst papillary carcinoma involves a Sistrunk procedure followed by evaluation of lateral neck lymph nodes and thyroid. Total thyroidectomy, lateral neck dissection and/or radioactive iodine may be indicated depending on the extent of disease. Overall prognosis is excellent, with a survival rate of 99.4% and a recurrence rate of 4.3%.
What causes thyroglossal duct cyst?
A thyroglossal duct cyst is an embryologic remnant that forms due to the failure of closure of the thyroglossal duct extending from the foramen cecum in the tongue to the thyroid’s location in the neck 5. The thyroid begins to develop in the third week of gestation as a median outgrowth from the primitive pharynx. The thyroid primordium originates at the foramen cecum at the junction of the anterior two-thirds and posterior one-third of the tongue. From there, the thyroid descends to the neck, passing anterior and in close relation to the developing hyoid bone. It reaches its final position in the inferior pre-tracheal neck by the seventh week of gestation.
The thyroglossal duct is the narrow tubular structure left from the thyroid’s descent and connects the thyroid gland to the foramen cecum. The distal part of the duct differentiates into the pyramidal lobe of the thyroid gland in about 50% of people. The thyroglossal duct normally involutes by the tenth week of gestation. If any portion of the thyroglossal duct persists, secretion from the epithelial lining can result in inflammation and thyroglossal duct cyst formation 9.
Thyroglossal duct cyst symptoms
Thyroglossal duct cysts typically present as small, mobile midline neck round or oval masses or lumps near the hyoid bone, in the center of the front part of the neck. Thyroglossal duct cysts often are asymptomatic. However, they can present as an abscess or intermittently draining sinus. The mass will elevate with tongue protrusion or swallowing. The mass is closely associated with the hyoid bone and most commonly found at or below the level of the hyoid.
Thyroglossal duct cysts usually appear in preschool-aged children through adolescence. They affect males and females equally. The cysts can become larger over time, especially in children with an upper respiratory infection. Sometimes large cysts can cause difficulty swallowing or breathing.
Thyroglossal duct cysts can become infected, causing redness and tenderness in the area of the cyst. Rarely, the cysts create sinuses, or openings, to the skin through which the cysts drain on their own. In these cases, children will have a small opening in their skin near the cyst which drains fluid or mucus. This is uncommon, and typically follows an episode of infection.
Thyroglossal duct cyst diagnosis
Imaging should be performed to both diagnose the thyroglossal duct cyst and evaluate for the presence of healthy thyroid tissue. If normal thyroid tissue in the inferior neck is absent, the patient and/or parents should receive counseling on the possibility of lifelong thyroid replacement therapy after surgery.
Ultrasound is the ideal initial imaging choice. Ultrasound is readily available, inexpensive, and noninvasive. It does not require ionizing radiation or sedation, which is important in treating children. CT scans and MRI can be used to evaluate thyroglossal duct cysts and the presence of normal thyroid tissue, but ultrasound alone in usually sufficient.
Some surgeons advocate for routine thyroid function testing preoperatively. This may be helpful if ectopic thyroid tissue is expected, but the literature does not support routine lab work for uncomplicated thyroglossal duct cysts 10.
Thyroglossal duct cyst treatment
The treatment for thyroglossal duct cysts is surgical removal to prevent recurrent infections due to the small risk of malignancy. Simple excision of thyroglossal duct cysts is associated with high recurrence rates (45% to 55%). The Sistrunk operation is considered the standard of surgical management and has dramatically reduced recurrence rates. This procedure requires a more extensive surgical resection including the central third of the hyoid bone and a core of base of tongue tissue 11.
The Sistrunk procedure should not be performed in the setting of acute infection. The patient should receive systemic antibiotics and removal should be planned after the infection has resolved. If preoperative evaluation reveals no other functional thyroid tissue, removal can still be performed with the acknowledgment that hormone replacement therapy may be necessary postoperatively.
Thyroglossal duct cyst surgery
The conventional thyroglossal duct cyst operation known as Sistrunk’s operation is the treatment of choice for symptomatic clinical thyroglossal duct cysts 12. The operation entails excision of the mid-portion of the hyoid bone with the cystic portion, as well as excision of the TGD between the foramen cecum at the tongue base and the hyoid bone to prevent cyst recurrence 13. Recurrence occurs in <10% of patients who receive the conventional thyroglossal duct cyst operation. However, it inevitably results in a scar on the neck 14. In addition, it is difficult to approach the full thyroglossal duct during the traditional operation in children because the thyroglossal duct cyst is located at the tongue base and is situated far away from the transcutaneous incision site, and there is a possibility of not identifying the duct, which is very soft. Considering the external operation scar and the embryological aspects, alternative surgical approaches need to be developed that can provide access to the full thyroglossal duct cyst and leave no scar.
Surgical technique
- Conventional thyroglossal duct cyst excision: To excise each thyroglossal duct cyst, the surgeon made an approximately 5 cm horizontal skin incision in the hyoid region and created a flap that extended 1 cm above the hyoid bone and 1 cm inferior to the thyroglossal duct cyst. After the surgeon divided the median raphe of the strap muscles, the dissection proceeded superior to the hyoid bone. After that, the surgeon dissected and cut the hyoid bone into fragments of 1 cm in length using bone-cutting forceps. The surgeon performed careful dissection of the thyroglossal duct, extending from the resected hyoid bone to the tongue base, from the attached tissues. After that, the surgeon sutured each subcutaneous layer and skin.
- Transoral thyroglossal duct cyst excision: Under general anesthesia, the surgeon retracted the tongue of the child superiorly after opening the mouth with a Denhart retractor, making an approximately 1 cm horizontal incision on the tongue’s frenulum mucosa above the submandibular gland opening. After the mucosal incision, the surgeon could identify the genioglossus muscle in the operation field. Surgical dissection was performed under a magnified endoscopic view. The genioglossus muscle is composed of two parts—a left side and a right side—and the surgeon dissected between the two parts of genioglossus muscle and found an avascular space in the middle. After the surgeon retracted the genioglossus muscles bilaterally with Sofield retractors, he identified the thyroglossal duct where it originated from the foramen cecum to the hyoid bone. The surgeon then dissected the thyroglossal duct apart from the tongue muscle. Next, the surgeon cut the thyroglossal duct just below the foramen cecum and the hyoid bone with an endoscopic dissector and ultrasonic scissors, after which the surgeon dissected the hyoid bone and cut it into 1 cm lengths using an Osteo Punch Rongeur. As the cutoff hyoid bone was pulled upwards, the attached thyroglossal duct cyst was also pulled upwards and the surgeon could carefully dissected each cyst and remove it through the oral cavity incision site. After irrigating the surgical field, the surgeon approximated the genioglossus muscle using 4-0 Vicryl and sutured the oral mucosa vertically. The surgeon encouraged frequent oral gargling (0.02% chlorhexidine) and prescribed antibiotics for three days, and oral feeding with a normal diet was allowed after one day.
Thyroglossal duct cyst surgery complications
The most common complication of the Sistrunk procedure is a recurrence of the thyroglossal duct cyst, which occurs in about 10% of cases. Contributing factors to recurrence include incomplete excision, intraoperative rupture, surgical proficiency and experience, and presence of infection. However, recurrence can still occur after technically proficient procedures.
A laryngotracheal injury is a rare and potentially devastating complication of the Sistrunk procedure, resulting in issues with the airway, swallowing, and/or voice. It can be caused by erroneous resection of the thyroid cartilage instead of the hyoid bone. Appropriate identification of the hyoid bone, thyroid cartilage, and the thyrohyoid membrane is essential to prevent this during surgery.
A hypoglossal injury is also rare but has been reported after the Sistrunk procedure, resulting in paralysis of half of the tongue. The hypoglossal nerve travels lateral to the hyoglossus muscle and medial to the stylohyoid muscle and lingual nerve near the lateral portion of the hyoid bone. It is important to keep the hyoid resection medial to the lesser cornu of the hyoid to avoid hypoglossal injury.
Call your surgeon if your child has any of the following symptoms:
- Fever (a temperature of 101.5 degrees F or higher)
- Any signs of infection, including redness, swelling or pain
- Any drainage from the incision
- Any pain that is not controlled with the prescribed pain medicine
- A mass or lump in the center of the neck
- Any further questions or concerns
Thyroglossal duct cyst surgery postoperative and rehabilitation care
Following the Sistrunk procedure, patients are instructed to avoid heavy lifting for 2 to 6 weeks. Depending on the size of the thyroglossal duct cyst, there may be a surgical drain in place, which would be removed within a few days of surgery. Pain medication or antibiotics may be prescribed postoperatively. Patients can usually return to work or school 1 week after surgery.
Thyroglossal duct cyst prognosis
Following the Sistrunk procedure, the prognosis is usually excellent. About 10% of thyroglossal duct cysts recur after Sistrunk. There is a much higher recurrence rate with simple excision without excising the middle third of the hyoid bone. 1% of thyroglossal duct cysts are malignant, which is usually diagnosed after surgical removal.
- Chrysostomos Kepertis,Kleanthis Anastasiadis,Vassilis Lambropoulos,Vassilis Mouravas,Ioannis Spyridakis. Diagnostic and Surgical Approach of Thyroglossal Duct Cyst in Children: Ten Years Data Review. J Clin Diagn Res. December 2015; 9(12):PC13-PC15. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4717790[↩][↩][↩]
- Allard RH 1982 The thyroglossal cyst. Head Neck Surg 5:134–146.[↩]
- Thyroglossal Duct Cyst Imaging. https://emedicine.medscape.com/article/1346365-overview[↩][↩]
- THYROGLOSSAL DUCT CYST, FAMILIAL. https://omim.org/entry/188455[↩]
- Amos J, Shermetaro C. Thyroglossal Duct Cyst. [Updated 2019 Feb 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519057[↩][↩][↩][↩][↩]
- Garcia E, Osterbauer B, Parham D, Koempel J. The incidence of microscopic thyroglossal duct tissue superior to the hyoid bone. Laryngoscope. 2018 Sep 08[↩]
- Ewing CA, Kornblut A, Greeley C, Manz H 1999 Presentations of thyroglossal duct cysts in adults. Eur Arch Otorhinolaryngol 256:136–138[↩]
- Ross J, Manteghi A, Rethy K, Ding J, Chennupati SK. Thyroglossal duct cyst surgery: A ten-year single institution experience. Int. J. Pediatr. Otorhinolaryngol. 2017 Oct;101:132-136[↩]
- Ma J, Ming C, Lou F, Wang ML, Lin K, Zeng WJ, Li ZC, Liu XF, Zhang TS. [Misdiagnosic analysis and treatment of pyriform sinus fistula in children]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2018 May 07;53(5):381-384[↩]
- Povey HG, Selvachandran H, Peters RT, Jones MO. Management of suspected thyroglossal duct cysts. J. Pediatr. Surg. 2018 Feb;53(2):281-282[↩]
- Pucher B, Jonczyk-Potoczna K, Kaluzna-Mlynarczyk A, Kurzawa P, Szydlowski J. The Central Neck Dissection or the Modified Sistrunk Procedure in the Treatment of the Thyroglossal Duct Cysts in Children: Our Experience. Biomed Res Int. 2018;2018:8016957[↩]
- No-Scar Transoral Thyroglossal Duct Cyst Excision in Children. Jin Pyeong Kim, Jung Je Park, and Seung Hoon Woo. Thyroid 2018 28:6, 755-761 https://www.liebertpub.com/doi/10.1089/thy.2017.0529[↩]
- Hirshoren N, Neuman T, Udassin R, Elidan J, Weinberger JM 2009 The imperative of the Sistrunk operation: review of 160 thyroglossal tract remnant operations. Otolaryngol Head Neck Surg 140:338–342[↩]
- Marianowski R, Ait Amer JL, Morisseau-Durand MP, Manach Y, Rassi S 2003 Risk factors for thyroglossal duct remnants after Sistrunk procedure in a pediatric population. Int J Pediatr Otorhinolaryngol 67:19–23[↩]