Transient neonatal pustular melanosis
Transient neonatal pustular melanosis is a rare, benign, self-limited pustular skin condition of unknown cause presenting in newborn infants 1. Transient neonatal pustular melanosis is also known as transient neonatal pustular dermatosis and transient neonatal pustulosis. Term or near-term infants are born with transient pustular melanosis. Pustules are usually uniformly sized and wipe off easily in the delivery suite.
Historically, neonatal pustular dermatosis was lumped together with vesicular and bullous lesions and called pemphigus neonatorum. Transient neonatal pustular melanosis was not described as a separate entity until 1976, although it may have been recognized as early as 1961 and published under the name of lentiginosis neonatorum.
Transient neonatal pustular melanosis affects 0.2–4% of newborn infants in the first few days of life 2. Transient neonatal pustulosis is more common in African-American babies, affecting 4.4% of African-American than in Caucasians (0.2% of whites) 3. Transient neonatal pustular melanosis affects both sexes with the same frequency 4.
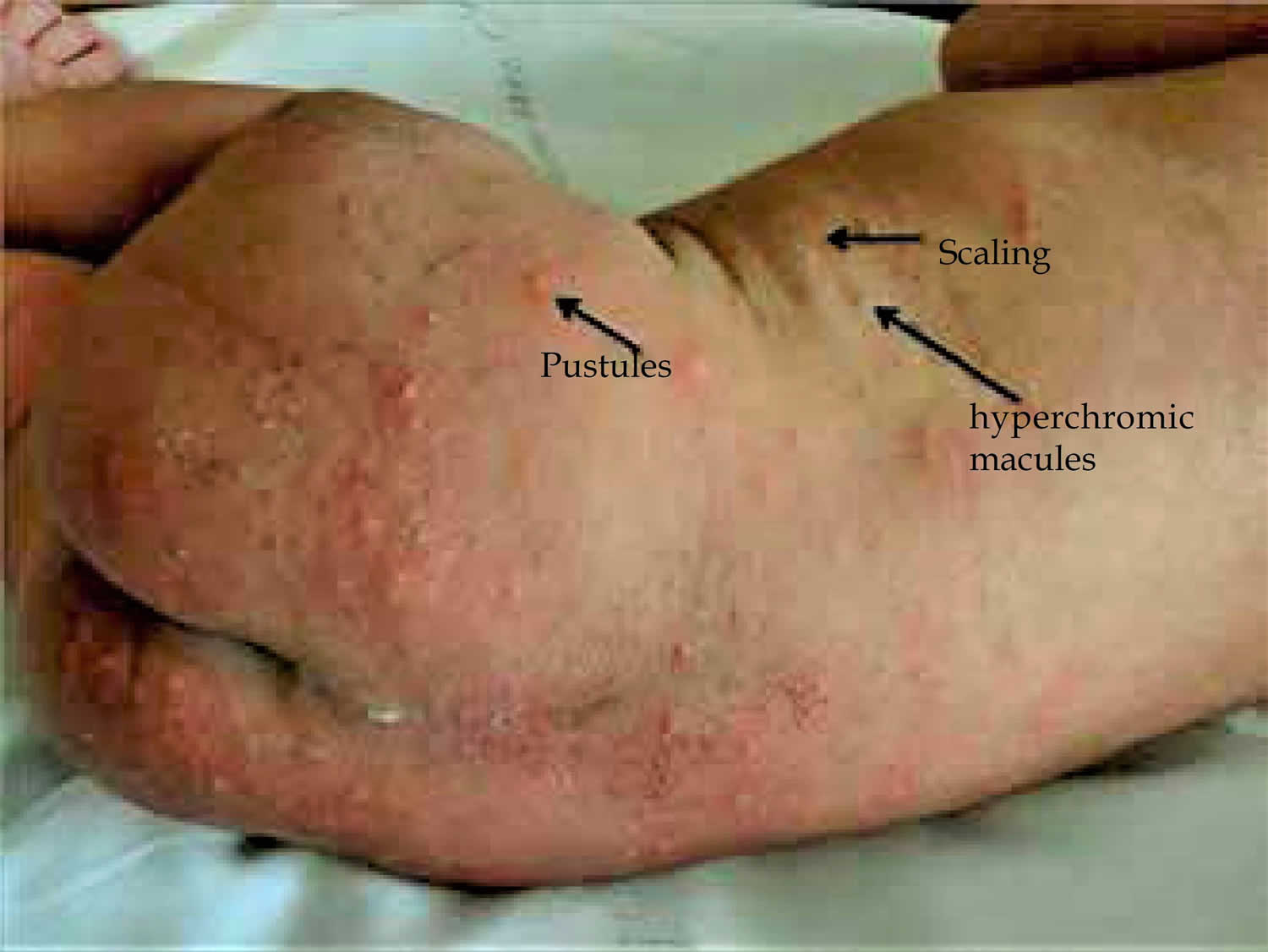
Figure 1. Transient neonatal pustular melanosis
Footnote: Transient neonatal pustular melanosis. Presence of pustules, hyperchromic macules and scaling in newborn with 24 hours of life.
[Source 5 ]What causes transient neonatal pustular melanosis?
The cause of transient neonatal pustular melanosis is unknown. Some authors have suggested it may be a variant of toxic erythema of the newborn (erythema toxicum neonatorum) 6.
What are the clinical features of transient neonatal pustular melanosis?
The key clinical feature of transient neonatal pustular melanosis is the presence of pustules. These occur on an unaffected, non-erythematous base 7.
- Any area can be involved, including the patient’s forehead, posterior ears, chin, neck, upper chest, back, buttocks, abdomen, thighs, palms, and soles 7.
- Lesions can be either solitary or occur in clusters 7.
- The pustules can rupture and crust, resolving within several days 7.
- The pustules may leave an area of hyperpigmentation, which fades within weeks to months 7.
- The pigmented macules can have a collarette of scale 2.
- The pustules are present at birth and evolve; new lesions usually do not develop after birth 7.
- There are no associated systemic symptoms or laboratory abnormalities.
The primary lesions in neonatal pustular melanosis progress through 3 stages of development. Initially, they appear as rather uniform round 2-mm to 4-mm nonerythematous pustules. They are not clear vesicles; rather, they contain milky, purulent exudate. The pustules rupture easily. They are frequently missed because they are superficial and are usually wiped off easily in the delivery suite when the newborn is cleansed of vernix. Pustules on the thicker areas of skin such as the knees or palms may persist for several days 8.
Next, a delicate collarette of thin white scale is left around the perimeter of each denuded pustule. Near-term infants, especially those delivered by cesarean delivery, may exhibit just the unbroken pustules, and term infants may have only macules remaining, usually with the telltale collarette of flaking epidermis.
Lastly, within hours of exposure to the terrestrial environment, the central pigmented brown macule becomes apparent. The macules are round, have smooth and distinct borders, and are frequently confused for freckles. They may be profuse or sparse and typically are found under the chin and on the neck, upper chest, back, and buttocks. Occasionally, the palms, soles, and scalp are affected.
How is transient neonatal pustular melanosis diagnosed?
The diagnosis of transient neonatal pustular melanosis is clinical. No investigations are required.
When considering suspected neonatal pustular melanosis, the following should also be considered:
- Erythema toxicum neonatorum: These lesions are small papules on an erythematous base, contain predominantly eosinophils, and do not heal with postinflammatory hyperpigmentation.
- Congenital cutaneous candidiasis: The pustules are usually very inflamed and contain organisms on laboratory smear or biopsy.
- Impetigo: Pustules are inflamed and contain organisms on laboratory smear and culture.
- Congenital Langerhans cell histiocytosis: Widely distributed papules and pustules form adherent crusts, not frecklelike macules.
- Congenital varicella: Pustules are larger, numerous, generalized, and widely dispersed in the setting of an ill neonate with unstable vital signs.
- Miliaria: This characterized by clear vesicles (crystallina) or pustules (pustulosa) that erupt in a setting of hyperthermia.
- Herpes simplex: Lesions begin as vesicles, become turbid, and develop into pustules. The vesicles are grouped or clustered and contain multinucleated giant cells.
- Milia: This is characterized by firm, white, superficial, pin-head–sized papulelike cysts filled with keratin debris.
- Acropustulosis: The pustules predominate on the palms and soles and are not present at birth.
A skin biopsy shows a neutrophilic infiltrate in the epidermis or dermis, commonly with subcorneal pustules, and occasional eosinophils 9. Pustules contain neutrophils with no organisms 7.
Transient neonatal pustular melanosis treatment
No treatment is necessary for transient neonatal pustular melanosis, as it is self-resolving and has no long-term complications 10.
Transient neonatal pustular melanosis prognosis
Transient neonatal pustular melanosis is a completely benign condition that is not known to cause any long-term complications 11. The prognosis is excellent. Postinflammatory pigmented macules resolve in 2-4 months.
- Eichenfield LF, Frieden IJ, Esterly NB, eds. Neonatal Dermatology. 2nd ed. Philadelphia, Pa: Saunders Elsevier; 2008. 142.[↩]
- Merlob P, Metzker A, Reisner SH. Transient neonatal pustular melanosis. Am J Dis Child 1982; 136: 521–2.[↩][↩]
- Brazzelli V, Grasso V, Croci G, Figar T, Borroni G. An unusual case of transient neonatal pustular melanosis: a diagnostic puzzle. Eur J Pediatr 2014; 173: 1655–8. DOI: 10.1007/s00431-013-2227-9.[↩]
- Reginatto FP, De Villa DM, Muller FM, Peruzzo J, Peres LP, Steglich RB, et al. Prevalence of neonatal dermatologic findings in 3 school hospitals of Porto Alegre. J Am Acad Dermatol. 2014;70:AB148.[↩]
- Reginatto, Flávia Pereira, Villa, Damie De, & Cestari, Tania Ferreira. (2016). Benign skin disease with pustules in the newborn. Anais Brasileiros de Dermatologia, 91(2), 124-134. https://dx.doi.org/10.1590/abd1806-4841.20164285[↩]
- Morgan AJ, Steen CJ, Schwartz RA, Janniger CK. Erythema toxicum neonatorum revisited. Cutis. 2009 Jan. 83(1):13-6.[↩]
- Schachner LA, Hansen RC, B Krafchik, et al (eds). Pediatric dermatology, 4th ed. Maryland Heights: Mosby, 2011.[↩][↩][↩][↩][↩][↩][↩]
- Goyal T, Varshney A, Bakshi SK. Incidence of Vesicobullous and Erosive Disorders of Neonates: Where and How Much to Worry?. Indian J Pediatr. 2011 Oct 25.[↩]
- Elder D, Elenitsas R, Jaworsky C, Johnson B Jr (eds). Lever’s histopathology of the skin, 8th edn. Philadelphia: Lippincott-Raven, 1997.[↩]
- Van Praag M, Van Rooij R, Folkers E, Spritzer R, Menke H, Oranje A. Diagnosis and treatment of pustular disorder in the neonate. Pediatr Dermatol 1997; 14(2): 131–43.[↩]
- O’Connor NR, McLaughlin MR, Ham P. Newborn skin: Part I. Common rashes. Am Fam Physician. 2008 Jan 1. 77(1):47-52.[↩]