Trichostasis spinulosa
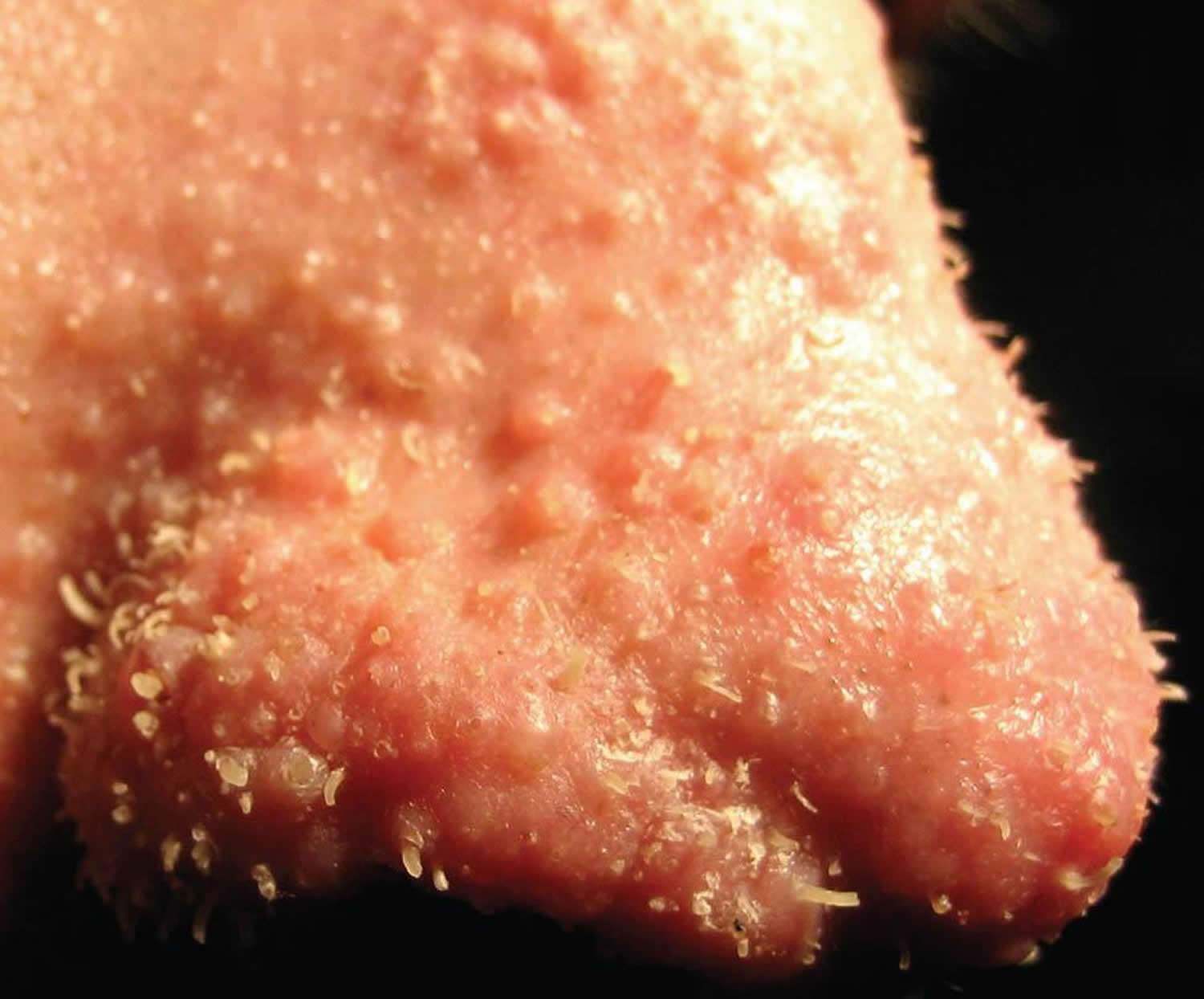
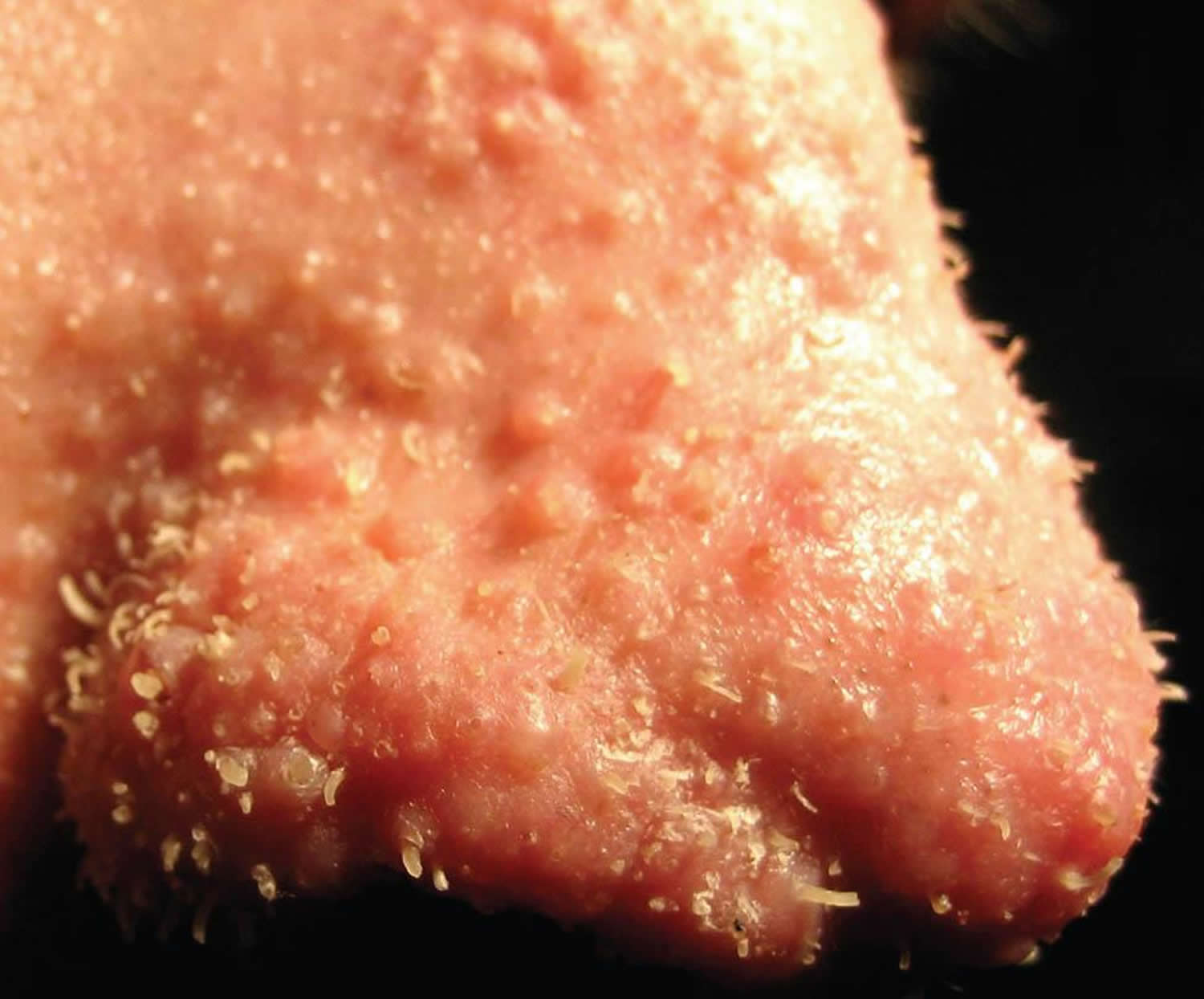
Trichostasis spinulosa is a condition where instead of one hair protruding from a hair follicle, a bundle or bush of hair come out of a single hair follicle. Each follicular plug may contain between 5–25 hairs and is usually less than 1 mm in size. This results in elevated, dark spiny papules on the head, face usually affects the skin of the nose of adults and trunk. In trichostasis spinulosa, there are numerous tiny open pores filled with multiple tiny short hairs, usually only visible with a magnifying glass. Trichostasis spinulosa is often confused with blackheads. Trichostasis spinulosa usually does not cause problems and may only be noticed as an incidental finding. The exact cause of trichostasis spinulosa is unknown.
Trichostasis spinulosa can affect both men and women and usually occurs in older adults. Trichostasis spinulosa is rarely seen in children.
No treatment is necessary. However, for cosmetic reasons, hairs within the individual plugs may be removed by pulling them out using tweezers, squeezing them out with a comedo extractor, or using depilatory wax or laser depilation.
Topical retinoids may be used to help prevent future lesions and improve the appearance.
Figure 1. Trichostasis spinulosa nose
Trichostasis spinulosa causes
The cause of trichostasis spinulosa is unknown. Trichostasis spinulosa results from successive production and retention of vellus telogen club hairs from a single hair matrix in a follicle. Hyperkeratosis plugs the follicle and results in the retention of the vellus hairs in the obstructed follicular infundibulum. The precise cause of this phenomenon remains undetermined.
Various explanations for the hyperkeratosis and plugging of the follicular apparatus are proposed. Internal mechanisms, such as endocrine or metabolic disturbances, are suggested. Widespread trichostasis spinulosus has been reported with renal failure 1. External mechanisms include the use of irritating soaps or paraffin-containing creams and prolonged exposure to dust, hydrocarbons, or industrial oils. Trichostasis spinulosa has also been associated with prolonged use of clobetasol 2.
Some consider trichostasis spinulosa to be a variant of the comedonal lesions of acne; they note the similar distribution of lesions and the rarity of trichostasis spinulosa among preadolescent patients.
Microorganisms are also suggested to have a causative role. Propionibacterium acnes and Pityrosporum species are implicated as possible organisms.
Trichostasis spinulosa symptoms
In most trichostasis spinulosa cases, the condition does not lead to any subjective complaint and is observed only as an incidental finding. Pruritus (itch) is occasionally present, as is roughness of the skin. Pruritus may be more common when lesions are present on the trunk and arms of young adults. In younger patients, the chief complaint may be a cosmetic concern about facial lesions, which are frequently confused with open comedones. In this setting, patients may report a history of unsuccessful treatment for acne.
Trichostasis spinulosa diagnosis
The diagnosis of trichostasis spinulosa can be made clinically without obtaining a biopsy specimen. Pertinent physical findings of trichostasis spinulosa are limited to the skin. Because spinous plugs may be inapparent to the naked eye, examination of suspected lesions under a hand lens or with a dermatoscope is recommended.
Lesions typically appear as dark, follicular plugs or papules. The lesions may have protruding tufts or spines of fine hair that can easily be removed with a comedo extractor or small-toothed forceps without discomfort to the patient. The horny plugs are soft and contain 5-25 hairs per plug. Scales may sometimes be present.
Lesions may occur anywhere on the body, but they characteristically appear on the face, especially the nose, and the upper part of the trunk and arms, especially the interscapular area. Lesions less typically appear on other areas of the head, neck, and cheeks.
Lesions are characteristically less than or equal to 1 mm.
Lesions characteristically are black.
If the diagnosis is in doubt, a specimen may easily be obtained by removing a hair plug with a forceps or comedone extractor. The specimen may be placed on a glass slide for microscopic examination. Treatment with potassium hydroxide dissolves the keratinous plug, leaving numerous vellus hairs in a characteristic tuft. Dermatoscopy may also be used to help confirm the diagnosis 3.
Trichostasis spinulosa treatment
Treatment for trichostasis spinulosa is usually administered for cosmetic purposes. The individual plugs of impacted hairs may be removed by means of the following:
- Tweezing with forceps
- Pressure expression with a comedone extractor
- Use of depilatory wax, adhesive strips 4 or laser depilation 5
- Laser treatment with a 755-nm long-pulsed alexandrite laser may also be considered 6.
Emollients and keratolytics may also be helpful. After the apparent lesions are removed, topical retinoic acids can be used to help prevent future lesions; however, recurrence of lesions is commonplace.
Trichostasis spinulosa prognosis
Trichostasis spinulosa persists and remains medically inconsequential; however, the condition may become more severe with age. Trichostasis spinulosa is primarily a cosmetic concern. Trichostasis spinulosa does not cause morbidity.
- Sidwell RU, Francis N, Bunker CB. Diffuse trichostasis spinulosa in chronic renal failure. Clin Exp Dermatol. 2006 Jan. 31(1):86-8.[↩]
- Janjua SA, McKoy KC, Iftikhar N. Trichostasis spinulosa: possible association with prolonged topical application of clobetasol propionate 0.05% cream. Int J Dermatol. 2007 Sep. 46(9):982-5.[↩]
- Pozo L, Bowling J, Perrett CM, Bull R, Diaz-Cano SJ. Dermoscopy of trichostasis spinulosa. Arch Dermatol. 2008 Aug. 144(8):1088.[↩]
- Elston DM, White LC. Treatment of trichostasis spinulosa with a hydroactive adhesive pad. Cutis. 2000 Jul. 66(1):77-8.[↩]
- Manuskiatti W, Tantikun N. Treatment of trichostasis spinulosa in skin phototypes III, IV, and V with an 800-nm pulsed diode laser. Dermatol Surg. 2003 Jan. 29(1):85-8.[↩]
- Badawi A, Kashmar M. Treatment of trichostasis spinulosa with 0.5-millisecond pulsed 755-nm alexandrite laser. Lasers Med Sci. 2011 Nov. 26(6):825-9.[↩]