What is varicocele
Varicoceles are varicose veins or swelling of the veins inside your scrotum (pampiniform plexus veins in the scrotum become enlarged) 1. Varicoceles form in the veins that run along the spermatic cord (the cord that holds up a man’s testicles). Blood from the testicles flows back into the body through those veins. Like varicose veins in the legs, varicoceles form when blood builds up in the veins and they become permanently enlarged.
Varicoceles are common in prepubescent and adolescent boys. About 10 to 15 boys out of 100 have a varicocele 2. Varicoceles are uncommon in boys younger than age 10 and rarely develop after adolescence. Most varicoceles are found only on the left side because of the way blood drains from the left testicle 3. In some cases varicoceles can also develop above the right or in both testicles, but this is rare 2.
Varicoceles are more common in men ages 15 to 25 and are most often seen on the left side of the scrotum. About 15 out of 100 men have varicoceles. It’s hard to predict which of these 15 will have fertility problems caused by their varicocele. But about 4 in every 10 men tested for fertility problems have a varicocele and decreased sperm movement. There’s no link with other defects, race, place of birth, or ethnic group. Although varicoceles are often found in men tested for infertility, 8 out of 10 men who have a varicocele don’t have fertility problems.
Varicoceles usually are not painful and do not need treatment. However, treatment might be advised if a varicocele:
- Is painful
- Causes a testicle to under develop or shrink (testicular hypotrophy)
- Potentially affects the ability to father children (fertility)
Some varicoceles may cause infertility (problems fathering a child) and slow growth of the left testicle during puberty. Varicoceles may be the cause of fertility problems in about 4 out 0f 10 men who have problems fathering their first child. Varicoceles may also be the cause of fertility problems in about 8 out of 10 men who have problems fathering a child after their first.
Varicoceles can affect fertility by reducing blood flow and raising the temperature of the testicles 3. This can cause the testicles to produce fewer sperm, and sperm that is produced might not be healthy. Early treatment can help produce healthier sperm and even regrowth of a testicle.
Because a varicocele usually causes no symptoms, it often requires no treatment. Varicoceles might be discovered during a fertility evaluation or a routine physical exam.
However, if you experience pain or swelling in your scrotum, discover a mass on your scrotum, notice that your testicles are different sizes, or develop a varicocele in your youth, or you’re having problems with fertility, contact your doctor. A number of conditions can cause a scrotal mass or testicular pain, some of which require immediate treatment.
Figure 1. Testicle anatomy
Figure 2. Varicocele (varicoceles are usually found in the left side of the scrotum)
 What will happen if I choose not to get treated?
What will happen if I choose not to get treated?
Not treating a varicocele may result in the testicle shrinking and/or a drop in semen quality. This may lead to fertility problems, though this is rare. The varicocele may, over time, cause lasting harm to the testicle that can’t be fixed. If a semen analysis is normal, then it’s okay not to get treated. If the semen analysis isn’t normal, then action is called for. In some men, the “varicocele effect” on making sperm may get worse over time. Fertility issues may come up years later, even if not seen earlier.
My teenage son was diagnosed with a varicocele. Should this be fixed?
Treatment of teenagers depends on each case. It’s important to discuss options with a urologist or pediatric urologist. Varicocele repair in a teen may be considered if there is pain or if 1 testicle is more than 10% smaller than the other. Some families choose repair so they won’t have to worry about fertility issues in the future. Semen analyses can be done in older teens to see if repair would help.
I’m interested in having children and have no symptoms. Should I have my varicocele repaired?
As a rule, varicoceles with no symptoms aren’t repaired. Most health care providers don’t believe these varicoceles cause health problems if not treated. If there’s worry about fertility, semen analysis can be done to see if the varicocele is harming sperm quality.
I have pain with my varicocele. What can I do to ease the pain?
Supporting the scrotum with a jockstrap or briefs-style underwear can help varicocele pain. Lying on your back helps the varicocele drain, and often eases pain. Taking pain killers (such as acetaminophen and ibuprofen) may also help. You can also talk with your urologist about varicocele repair.
I’m thinking about having my varicocele repaired for fertility reasons. How long will I have to wait to see if my semen quality improves?
Semen analyses are often done every 3 to 4 months after the procedure. Improvement is often seen within 6 months, but might take a year.
I found a lump on my scrotum during a self-exam. Should I worry?
Abnormalities in the male reproductive tract may show up as a mass in the scrotum. Masses could be nothing to worry about and have little effect on your health. Or they could be a sign of life-threatening illness. It’s important to find out what is causing your mass. For example, testicular cancer is cause for concern and calls for prompt action. It’s important to seek medical attention when you find any lump or bump in your testicle.
Varicocele severity grade
The severity of a varicocele can be classified into three grades:
- Can be felt by hand only during straining
- Can be felt by hand when relaxed
- Can become clearly visible at a distance, even at complete rest.
What causes varicocele
It is not known why varicoceles develop. They may be associated with accelerated sexual organ growth in young boys, but no specific risk factors have been determined. A varicocele forms when valves inside the veins that run along the spermatic cord prevent blood from flowing properly. Blood backs up, leading to swelling and widening of the veins. Also, the larger veins moving from the testicles towards the heart are connected differently on the left and right side. So more pressure is needed on the left side to keep blood flowing through the veins towards the heart. If blood flows backwards or pools in the veins, that can cause them to swell. This is similar to varicose veins in the legs.
Rarely, swollen lymph nodes or other abnormal masses behind the abdomen block blood flow. This can lead to sudden swelling of the scrotal veins. This is often painful.
Most of the time, varicoceles develop slowly.
A varicocele in an older man that appears suddenly may be caused by a kidney tumor, which can block blood flow to a vein.
Varicocele symptoms
Most males with a varicocele have no symptoms.
Varicoceles usually have no symptoms. In rare cases, it may cause pain, which may:
- Vary from sharp to dull discomfort in the scrotum
- Increase with standing or physical exertion
- Worsen over the course of the day
- Be relieved when you lie on your back
Varicocele signs include:
- Enlarged, twisted veins in the scrotum
- Painless testicle lump, scrotal swelling, or bulge in the scrotum
- Possible problems with fertility or decreased sperm count.
With time, varicoceles might enlarge and become more noticeable. A varicocele has been described as looking like a “bag of worms.” The condition might cause a swollen testicle, almost always on the left side.
You may notice a varicocele, or it may be noticed by your parents or by a physician during a routine physical examination or during a fertility evaluation at an older age.
Varicocele possible complications
Infertility is a complication of varicocele.
A varicocele may cause:
- Shrinkage of the affected testicle (atrophy). Most of the testicle is made up of sperm-producing tubules. When they are damaged, as from a varicocele, the testicle shrinks and softens. It is not clear what causes the testicle to shrink, but the malfunctioning valves allow blood to pool in the veins. This pooling can result in increased pressure in the veins that may cause testicular damage.
- Problems fathering children (infertility). With a varicocele, the testicle may be too warm. This can affect sperm formation, movement (motility), and function.
Complications from treatment may include:
- Atrophic testis
- Blood clot formation
- Infection
- Injury to the scrotum or nearby blood vessel
Varicocele diagnosis
It is usually relatively simple to diagnose a varicocele. Your doctor will take a detailed medical history and ask questions about your symptoms, if any.
You will have an exam of your groin area, including the scrotum and testicles. A collection of swollen and tangled veins in the scrotum that can be felt more in the upright posture or during straining, suggests a varicocele. The swollen veins may feel like a “bag of worms”. Both testicles should be examined to compare their size. The testicle on the side of the varicocele may be smaller than the one on the other side.
Sometimes the growth may not be able to be seen or felt, especially when you are lying down.
You may also have an ultrasound of the scrotum and testicles, as well as an ultrasound of the kidneys.
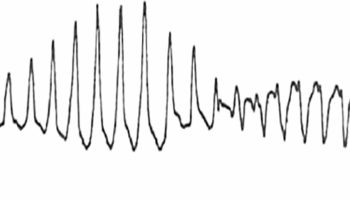
Backward flow of blood in the swollen testicular veins is usually confirmed by ultrasound of the scrotum. Signs of varicoceles on ultrasound are veins that are wider than 3 millimeters with blood flowing the wrong way during the Valsalva maneuver. The ultrasound can also show the size of the testicles. These are useful in deciding how to treat teenagers. An ultrasound isn’t needed if no problems are felt during the physical exam.
A right-side-only varicocele is uncommon. In extremely rare cases, it might be caused by a tumor of the kidney. Ultrasound of the kidneys should be performed to rule it out.
Varicocele treatment
Often, varicoceles are not treated. A jock strap or snug underwear may help ease discomfort. You may need other treatment if the pain does not go away or you develop other symptoms.
Surgery is the only way to treat varicoceles, but not all patients would benefit from surgery. Your doctor may recommend surgery if:
- The affected testicle is small
- Fertility is or could be affected
- Varicocele is present in both testicles
- The sperm is not healthy (in older adolescents)
- Pain, marked swelling, or physical discomfort is present
If none of these criteria apply to you, surgery is not needed. You should visit your doctor annually until sperm can be analyzed.
Boys with a smaller left testicle are thought to have a higher risk for fertility problems when they get older.
There are no drugs to treat or prevent varicoceles. But pain killers (such as acetaminophen or ibuprofen) may help with pain.
Varicocele surgery
There are many ways to do varicocele surgery. All involve blocking the blood flow in the pampiniform plexus veins.
The surgical procedure blocks the enlarged veins from draining blood from the testicle. This blockage redirects the blood flow to healthy veins.
During surgery, your doctor will try to protect nearby structures called lymphatic vessels. These tiny structures are usually invisible to the naked eye. They carry lymph, a clear, yellowish liquid that collects in all parts of the body. If they are injured, lymph cannot flow properly, and complications can develop. This surgery, called lymphatic-sparing varicocelectomy , can lower the chance of complications.
Surgery to correct a varicocele is called varicocelectomy. For this procedure:
- You will receive some type of numbing medicine (anesthesia).
- The urologist will make a small cut with the use of a surgical microscope, most often in the lower abdomen, and tie off the abnormal veins. This directs blood flow in the area to the normal veins. The operation may also be done as a laparoscopic procedure (through small incisions with a camera).
- You will be able to leave the hospital on the same day as your surgery.
- You will need to keep an ice pack on the area for the first 24 hours after surgery to reduce swelling.
Open Surgery
- Open surgery repair is done through a single 1 inch cut. The surgeon may use a magnifying glass or operating microscope to see small veins. The surgery can be done under local or general anesthesia.
This treatment usually is done on an outpatient basis, during general or local anesthetic. Commonly, your surgeon will approach the vein through your groin (inguinal or subinguinal), but it’s also possible to make an incision in your abdomen or below your groin.
Advances in varicocele repair have led to a reduction of post-surgical complications. One advance is the use of the surgical microscope, which enables the surgeon to see the treatment area better during surgery. Another is the use of Doppler ultrasound, which helps guide the procedure.
You might be able to return to normal, nonstrenuous activities after two days. As long as you’re not uncomfortable, you might return to more strenuous activity, such as exercising, after two weeks.
Pain from this surgery generally is mild but might continue for several days or weeks. Your doctor might prescribe pain medication for a limited period after surgery. After that, your doctor might advise you to take over-the-counter painkillers, such as acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others) to relieve discomfort.
Your doctor might advise you not to have sex for a period of time. Most often, it will take several months after surgery before improvements in sperm quality can be seen with a semen analysis. This is because it takes approximately three months for new sperm to develop.
Open surgery using a microscope and subinguinal approach (microsurgical subinguinal varicocelectomy) has the highest success rates when compared with other surgical methods.
Laparoscopic Surgery
- Laparoscopic surgery is done through thin tubes put into your body through a small cut. The surgeon uses a special camera to see inside your body.
- Laparoscopic surgery is done under general anesthesia.
What are the most common complications after surgery?
- Collection of fluid in the scrotum around the testicle (hydrocele formation)
- Shrinking of the testicle (testicular hypotrophy)
- Reduced function of the testicle
- Injury to the testicular artery
- Varicocele remaining (persistence) or coming back (recurrence)
There is a small chance surgery won’t correct the problem. In rare cases, injury to the testicular artery can lead to loss of the testicle. Persistence or recurrence of the varicocele happens in fewer than 1 of 10 patients who have surgery. Open surgery done with magnification has a low persistence rate or chance of varicocele coming back.
Recovery after surgery
Since surgeons have started using smaller cuts through the muscle for open surgery, healing time and pain are about the same with open and laparoscopic surgery.
You may be able to return to normal, nonstrenuous activities after 2 days. As long as you’re not uncomfortable, you may return to more strenuous activity, such as exercising, after 2–4 weeks.
Pain from this surgery is usually mild but may continue for several days or weeks. Your doctor may prescribe pain medication for a limited time after surgery. After that, your doctor may advise you to take over-the-counter medication like acetaminophen or ibuprofen. Wearing briefs or a jockstrap can also help by relieving pressure in the testicles.
It will take several months after surgery before improvements in sperm quality can be seen with a semen analysis, semen analysis is done 3 to 4 months later. This is because it takes approximately 3 months for new sperm to develop.
Follow up with your doctor if you have questions or concerns.
Varicocele embolization
Less often, a procedure called angiographic occlusion or varicocele embolization is used to treat varicocele. Embolization is done by a radiologist. Varicocele embolization collapses the twisted vein with a special substance. This method does not usually require you to be asleep (general anesthesia) and is less invasive than laparoscopic surgery. However, it uses X-ray, so you are exposed to radiation.
For varicocele embolization procedure:
- Percutaneous embolization is most often done with general anesthesia. It often takes several hours.
- A small hollow tube called a catheter (tube) is placed into a vein in your groin or neck area.
- Your doctor moves the tube into the varicocele using x-rays as a guide.
- A tiny coil passes through the tube into the varicocele. The coil blocks blood flow to the bad vein and sends it to normal veins.
- You will need to keep an ice pack on the area to reduce swelling and wear a scrotal support for a little while.
This method is also done without an overnight hospital stay. It uses a much smaller cut than surgery, so you will heal faster.
Some problems with varicocele embolization are:
- varicocele remaining (persistence) or coming back (recurrence)
- the coil moving from where it was placed
- a chance of infection where the tube was placed
Recovery after embolization
Healing after embolization is also relatively short with only mild pain. You should avoid exercise for 7 to 10 days after the procedure. You can often return to work 1 or 2 days later. The recurrence rate with embolization is often higher than with surgery. But there are cases where embolization is preferred over surgery.
Varicocele prognosis
A varicocele is often harmless and often does not need to be treated, unless there is a change in the size of your testicle.
If you have surgery, your sperm count will likely increase. However, it will not improve your fertility. In most cases, testicular wasting (atrophy) does not improve unless surgery is done early in adolescence.
The impact of varicocele repair on fertility isn’t clear. Some studies show fertility improves after varicocele repair while other studies don’t. Semen quality improves in about 6 out of 10 infertile men after varicocele repair. This treatment should be considered along with other fertility treatment choices.
In teens, where the main reason for surgery is slow testicular growth, catch-up growth occurs in 8 out of 10 patients.
- Informed Health Online [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Varicoceles: Overview. 2009 Aug 7 [Updated 2016 Jun 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279346[↩]
- What are Varicoceles? https://www.urologyhealth.org/urologic-conditions/varicoceles[↩][↩]
- Varicocele. https://patients.uroweb.org/varicocele/[↩][↩]