Wartenberg syndrome
Wartenberg syndrome also called isolated superficial radial neuropathy or cheiralgia paresthetica, is an entrapment neuropathy of the superficial branch of the radial nerve at the level of the distal forearm and wrist 1. The superficial branch of the radial nerve has 3 or 4 terminal branches and is a purely sensory nerve as indicated by the shaded area. Sometimes the innervation area of the superficial radial nerve can overlap with the innervation of the lateral antebrachial cutaneous nerve. Patients with the diagnosis of Wartenberg syndrome usually complain of pain and numbness, over the distal radial forearm associated with paresthesias over the dorsal radial-side wrist and thumb. They frequently report symptom magnification with wrist movement or with tight pinching of the thumb and index digit. These individuals demonstrate a positive Tinel sign over the radial sensory nerve and local tenderness. Hyperpronation of the forearm can cause a positive Tinel sign. A high percentage of these patients reveal physical examination findings consistent with de Quervain tenosynovitis.
Wartenberg’s syndrome is more common to occur in women. Wartenberg’s syndrome may also be associated with de Quervain’s tenosynovitis. Therefore, de Quervain’s syndrome and intersection syndrome should be differentiated.
The superficial branch of the radial nerve is easily injured by trauma. The superficial branch of the radial nerve can be injured during the placement of fixator pins due to Colles fractures. The superficial branch of the radial nerve injury by penetrating trauma, and cephalic vein cannulation are also reported 2. Some physical activities require forearm pronation with simultaneous flexion and ulnar deviation of the hand predisposed to superficial radial nerve entrapment between the brachioradialis muscle and the extensor carpi radialis longus muscle 1. Wartenberg syndrome is commonly associated with de Quervain’s disease, although the reason for this is not yet known 3. Ultrasound is helpful in distinguishing Wartenberg’s syndrome from de Quervain’s tenosynovitis or arthritis of the trapeziometacarpal joint 1. High-resolution ultrasound may depict the abnormal changes of the superficial branch of the radial nerve 4. Ultrasound in patients with Wartenberg syndrome can show secondary nerve compression from the adjacent scar tissue or post-traumatic/postoperative changes of the soft tissue. These changes could appear as abnormal heterogeneous hypoechoic tissue 5.
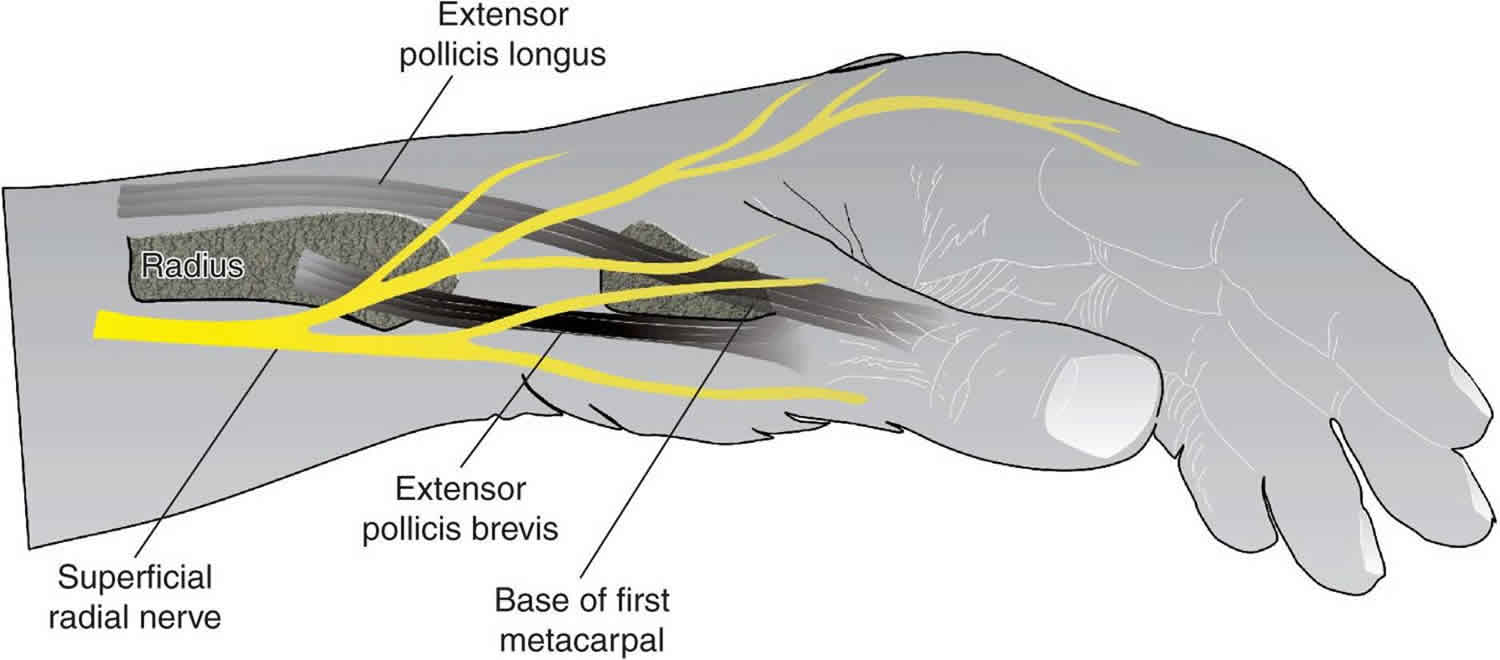
Superficial radial nerve anatomy
The superficial sensory branch of the radial nerve is purely sensory, runs under cover of the brachioradialis in the forearm. The superficial branch of the radial nerve passes along the front of the radial side of the forearm beneath the brachioradialis muscle. Eight centimeters proximal to the tip of the radial styloid, the superficial sensory branch of the radial nerve pierces the fascia medial to the brachioradialis to lie dorsal to the extensor tendons. It divides into a medial branch and a lateral branch to innervate the radial wrist (with some variable overlap from the lateral antebrachial cutaneous nerve), dorsal radial hand, and dorsum of the radial three-and-a-half digits (to approximately the middle phalanx level). Wartenberg’s syndrome is caused by entrapment of the superficial branch of the radial nerve at this point when the nerve arises from beneath the muscles. Entrapment of the superficial branch of the radial nerve occurs where the nerve pierces the antebrachial fascia approximately 2/3 the way down the forearm at the lateral border between the brachioradialis and extensor carpi radialis longus muscles. Entrapment occurs with repetitive pronation of the forearm and the brachioradialis muscles close the space between these two tendons in a scissor like fashion while rotating the nerve. Pain can be elicited with forced pronation and ulnar deviation of the wrist.
Figure 1. Radial nerve in the forearm
Figure 2. Radial nerve innervation
Wartenberg syndrome causes
The cause of the Wartenberg’s syndrome or isolated superficial radial nerve neuropathy is often associated with repeated use of wrist watches, forearm fractures, tight plaster cast, wearing bracelets or watches, use of handcuffs, repetitive supination, pronation and ulnar flexion activities 6, surgical operations such as fracture fixation and arthroscopic procedures, steroid injections, acupuncture, compression of extensor carpi radialis and/or brachioradialis tendons, presence of neuroma, lipoma or ganglion cyst in the wrist as well as exposure to excess cold 7. In addition, the presence of diabetes mellitus was reported to provide basis for development of Wartenberg’s syndrome 8.
Wartenberg syndrome symptoms
Wartenberg syndrome symptoms include burning type pain at proximal forearm and hand dorsoradial, hypoesthesia, numbness and tingling at hand dorsum and thumb radial side are observed. There will be no weakness associated with Wartenberg syndrome. The symptoms of Wartenberg’s syndrome are also aggravated by motion such as repetitive wrist flexion and ulnar deviation.
Physical examination: Tinel’s sign over the area of the superficial radial nerve is the most common finding for Wartenberg’s syndrome. The Finkelstein test may be positive due to traction on the nerve or associated with de Quervain’s tenosynovitis.
Wartenberg syndrome diagnosis
Imaging studies
Radiography
In a suspected entrapment of the radial nerve in the arm, radiography should be performed to detect or rule out a fracture, healing callus, or tumor as the cause of entrapment. In radial tunnel syndrome and posterior interosseous nerve syndrome, radiographs should be obtained to detect or rule out elbow or forearm fractures, dislocations or instabilities, tumors, and arthrosis.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is useful in detecting tumors such as lipomas and ganglions, as well as aneurysms and rheumatoid synovitis.
A study by Jengojan et al 9 found that magnetic resonance neurography based on diffusion tensor imaging was capable of detecting nerve changes during acute entrapment of the radial nerve at the spiral groove. Compression of the nerve resulted in a transient increase in local radial nerve fractional anisotropy values.
Ultrasonography
Toros et al 10 in a study of 26 patients with sensory or motor deficiency of a peripheral nerve from trauma or entrapment, confirmed that high-resolution ultrasonography could show the exact location, extent, and type of lesion, yielding important information that might not be obtained by other modalities. Ultrasonography provided reliable visualization of injured nerves in all 26 patients. Axonal swelling and hypoechogenicity of the nerve was diagnosed in 15 cases, loss of continuity of a nerve bundle in 17, formation of a neuroma of a stump in 6, and partial laceration of a nerve with loss of the normal fascicular pattern in 5. Ultrasonographic findings were confirmed at operation in the 19 patients who underwent surgery 10.
Lo et al 11 compared ultrasonography with electrophysiologic testing in the diagnosis of entrapment neuropathy of the radial nerve at the spiral groove, which is relatively common but technically challenging to localize. The study included 32 normal controls, to obtain ultrasound parameters of the radial nerve, and 10 patients with suspected radial neuropathy, in whom ultrasound and electrophysiologic techniques were used. Ultrasonography correctly identified all six patients with radial neuropathy; the four patients with other diagnoses did not show ultrasound abnormalities. Ultrasonography also required significantly less time than electrophysiologic testing did 11.
Electrodiagnostic testing
Electromyography (EMG) and nerve conduction studies yield abnormal results in radial nerve injuries in the middle and distal third of the humerus. EMG helps locate the site of injury and helps the clinician monitor the nerve recovery over time. EMG may not be positive for 3-6 weeks following injury. By 4 months after the injury, nerve recovery should be demonstrable. EMG may be performed initially to provide a baseline, but unless the nerve is severed, no changes will be observed for 3-6 weeks.
All electrodiagnostic test results are within normal limits in radial tunnel syndrome.
In posterior interosseous nerve syndrome, nerve conduction studies and EMG usually yield abnormal results and help determine the site of compression. These findings may not become abnormal for 3-6 weeks after injury. Serial EMG usually is not necessary once the diagnosis is established but can be used to document improved or worsening nerve function.
If the medial branch of the posterior interosseous nerve is compressed, EMG and conduction studies reveal abnormal function of the extensor carpi ulnaris, the extensor digitorum communis, and the extensor digiti quinti. If only the lateral branch is compressed, then abnormal function of the abductor pollicis longus, the extensor pollicis longus and brevis, and the extensor indicis proprius is revealed. The site of compression is localized by all function proximal to the compression being normal and all function distal to the compression being abnormal.
Diagnostic procedures
In de Quervain disease, injection of cortisone and lidocaine into the tendon sheath of the extensor pollicis brevis and the abductor pollicis longus relieves the symptoms immediately and sometimes permanently. An injection of cortisone and lidocaine into the area of compression of the superficial radial nerve causes the symptoms to subside; however, numbness in the nerve distribution follows, and when the injection wears off, the symptoms return.
A Tinel sign is present in patients with Wartenberg syndrome but usually not in those with de Quervain disease. The two conditions may be related. The inflammation from de Quervain disease causes an inflammation of the nerve. With resolution of one condition, the other may subside or may be adequately treated with an injection 12.
Wartenberg syndrome treatment
As external compression is a common underlying cause of Wartenberg syndrome, removal of the inciting element such as a wristwatch or bracelet is an essential component of nonsurgical management 13. In addition, rest, splinting, and nonsteroidal anti-inflammatory drugs (NSAIDs) are appropriate first-line treatments. The role of corticosteroid injection is less clear.
Wartenberg syndrome surgery
Surgical exploration may be necessary if conservative therapy fails 14. If the superficial sensory branch of the radial nerve is trapped by scar tissue, then release, neurolysis, and coverage with healthy tissue should be performed 14. The presence of a neuroma produces a guarded prognosis for recovery and relief 15. Lanzetta and Foucher 16 reported a 71% success rate in 29 patients who underwent conservative treatment alone, which was defined as removal of a tight watch strap, splinting, and, in 3 cases, a corticosteroid therapy. Surgical decompression had a 74% success rate in 23 patients. They recommended surgical decompression to patients whose symptoms were longstanding and had no distal progression of a Tinel’s sign 16. Surgical decompression may also be indicated in post-traumatic situations in which scar tissue may be the critical compressive factor 13.
- Tagliafico A, Cadoni A, Fisci E, Gennaro S, Molfetta L, Perez MM, et al. Nerves of the hand beyond the carpal tunnel. Semin Musculoskelet Radiol. 2012 Apr;16(2):129-36. doi: 10.1055/s-0032-1311764. Epub 2012 May 30. [↩][↩][↩]
- Braidwood AS. Superficial radial neuropathy. J Bone Joint Surg Br. 1975;57:380–383.[↩]
- De Maeseneer M, Marcelis S, Jager T, Girard C, Gest T, Jamadar D. Spectrum of normal and pathologic findings in the region of the first extensor compartment of the wrist: sonographic findings and correlations with dissections. J Ultrasound Med. 2009;28:779–786.[↩]
- Djurdjevic T, Loizides A, Loscher W, Gruber H, Plaikner M, Peer S. High resolution ultrasound in posterior interosseous nerve syndrome. Muscle Nerve. 2014;49:35–39.[↩]
- Jacobson JA, Fessell DP, Lobo Lda G, Yang LJ. Entrapment neuropathies I: upper limb (carpal tunnel excluded) Semin Musculoskelet Radiol. 2010;14:473–486.[↩]
- Cheiralgia Paresthetica: An Isolated Neuropathy of the Superficial Branch of the Radial Nerve. The Nerve 2015; 1(1): 1-5. https://www.thenerve.net/upload/pdf/nerve-2015-1-1-1.pdf[↩]
- Serçe A, Karaca Umay E, Karaahmet ÖZ, Çakcı FA. An unexpected side effect: Wartenberg syndrome related to the use of splint during carpal tunnel syndrome treatment. Turk J Phys Med Rehabil. 2017;64(1):83–86. Published 2017 Jun 19. doi:10.5606/tftrd.2018.1186 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6709603[↩]
- Demiryürek BE, Emre U, Demirel EA, Taşçılar FN, Atasoy HT, Ortancıl Ö, et al. Radial sinir nöropatilerinin retrospektif değerlendirilmesi. İstanbul Med J. 2015;16:116–118.[↩]
- Jengojan S, Kovar F, Breitenseher J, Weber M, Prayer D, Kasprian G. Acute radial nerve entrapment at the spiral groove: detection by DTI-based neurography. Eur Radiol. 2015 Jun. 25 (6):1678-83.[↩]
- Toros T, Karabay N, Ozaksar K, Sugun TS, Kayalar M, Bal E. Evaluation of peripheral nerves of the upper limb with ultrasonography: a comparison of ultrasonographic examination and the intra-operative findings. J Bone Joint Surg Br. 2009 Jun. 91(6):762-5.[↩][↩]
- Lo YL, Fook-Chong S, Leoh TH, Dan YF, Tan YE, Lee MP, et al. Rapid ultrasonographic diagnosis of radial entrapment neuropathy at the spiral groove. J Neurol Sci. 2008 Aug 15. 271(1-2):75-9.[↩][↩]
- Ilyas A, Ast M, Schaffer AA, Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg. 2007 Dec. 15(12):757-64.[↩]
- Dang AC, Rodner CM: Unusual compression neuropathies of the forearm, Part I: radial nerve. J Hand Surg Am 34A:1906-1914, 2009[↩][↩]
- Pećina MM, Krmpotić-Nemanić J, Markiewitz AD: Tunnel Syndromes: peripheral nerve compression syndromes ed 3. Boca Raton: CRC Press; 2001, pp141-145[↩][↩]
- Dee R: Principles of Orthopaedic Practice ed 2. New York: McGraw-Hill; 1989, pp125-130[↩]
- Lanzetta M, Foucher G: Entrapment of the superficial branch of the radial nerve (Wartenberg’s syndrome): a report of 52 cases. Int Orthop 17:342-345, 1993[↩][↩]