The American Diabetes Association Diet
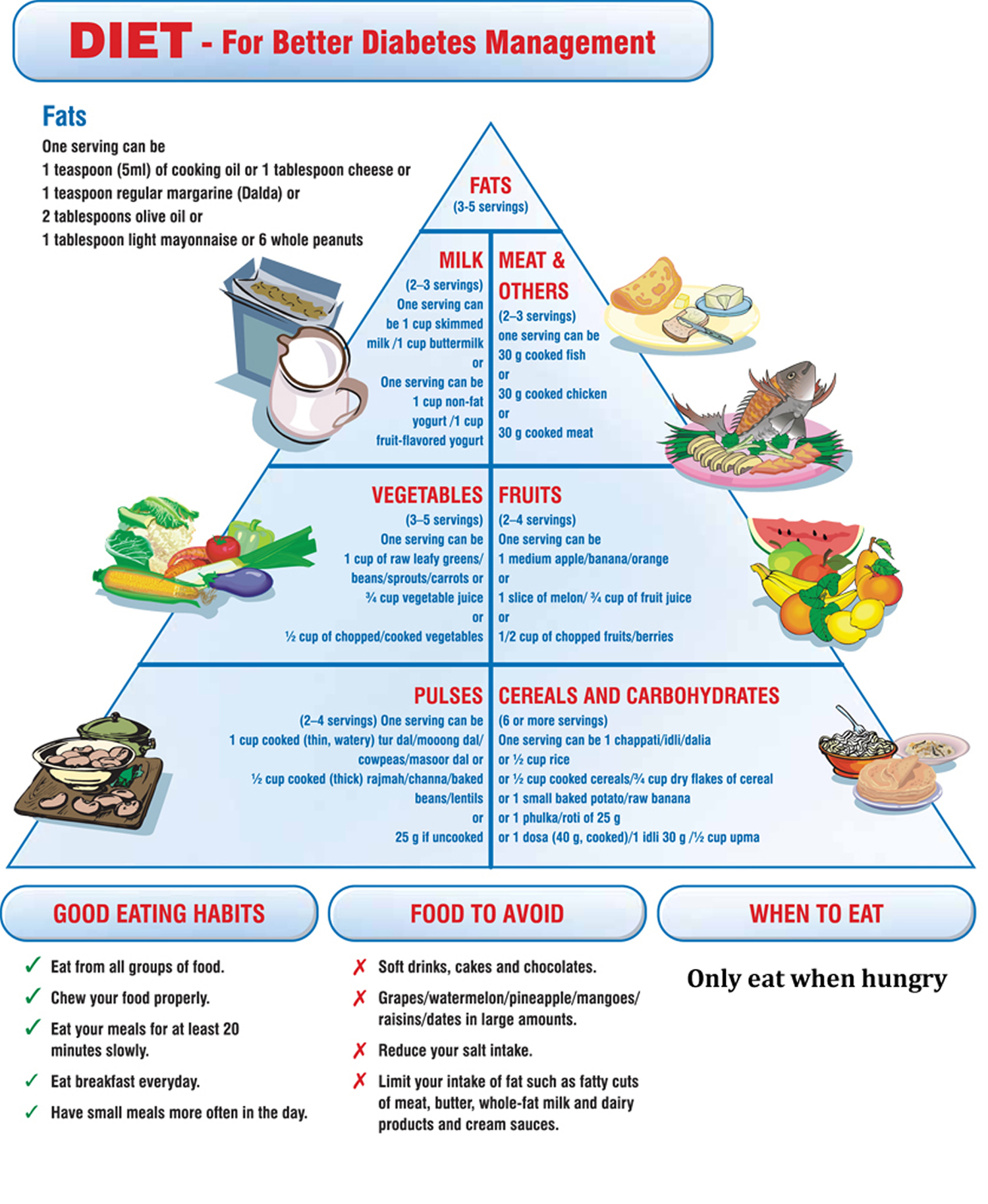
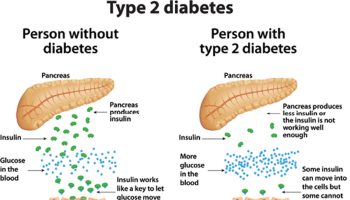
The diabetes diet is simply a healthy-eating plan that will help you control your blood sugar. Diabetic diet usually contains low-glycaemic index food, with similar amount of protein, complex carbohydrates, fibres, and unsaturated fatty acids as in food for general public 1. If you have diabetes, your body cannot make or properly use insulin. This leads to high blood glucose, or blood sugar, levels. What you eat is closely connected to the amount of sugar in your blood. The right food choices will help you control your blood sugar level and controlling your blood sugar can prevent the complications of diabetes 2.
General Dietary Goals for Diabetes
The nutrition therapy goals 3 for the individual with diabetes have evolved in the past few years and have become more flexible and user-friendly.
These goals include the following:
- To promote and support healthful eating patterns, emphasizing a variety of nutrient dense foods in appropriate portion sizes in order to improve overall health and specifically to:
- Attain individualized glycemic, blood pressure, and lipid goals. General recommended goals from the ADA for these markers are as follows:*
- A1C <7%
- Blood pressure,<140/80mmHg
- LDL cholesterol ,<100 mg/dL
- Triglycerides <150 mg/dL
- HDL cholesterol >40 mg/dL for men
- HDL cholesterol >50 mg/dL for women
- Achieve and maintain body weight goals
- Delay or prevent complications of diabetes
- To address individual nutrition needs based on personal and cultural preferences, health literacy and numeracy, access to healthful food choices, willingness and ability to make behavioral changes, as well as barriers to change
- To maintain the pleasure of eating by providing positive messages about food choices while limiting food choices only when indicated by scientific evidence
- To provide the individual with diabetes with practical tools for day-to-day meal planning rather than focusing on individual macronutrients, micronutrients
*A1C, blood pressure, and cholesterol goals may need to be adjusted for the individual based on age, duration of diabetes, health history, and other present health conditions. Further recommendations for individualization of goals can be found in the ADA Standards of Medical Care in Diabetes 4.
If you go to the American Diabetes Association website, there is no such thing as the American Diabetes Association (ADA) diet per se. In other word, there is no one diet or meal plan that works for everyone with diabetes. Instead the American Diabetes Association promotes healthy diabetes meal plan. A diabetes meal plan is a guide that tells you how much and what kinds of food you can choose to eat at meals and snack times. A good meal plan should fit in with your schedule and eating habits. The important thing is to follow a meal plan that is tailored to personal preferences and lifestyle and helps achieve goals for blood glucose, cholesterol and triglycerides levels, blood pressure, and weight management.
Research shows that both the amount and the type of carbohydrate in food affect blood glucose levels. Studies also show that the total amount of carbohydrate in food, in general, is a stronger predictor of blood glucose response than the Glycemic Index (GI). Based on the research, for most people with diabetes, the first tool for managing blood glucose is some type of carbohydrate counting.
Because the type of carbohydrate can affect blood glucose, using the Glycemic Index may be helpful in “fine-tuning” blood glucose management. In other words, combined with carbohydrate counting, it may provide an additional benefit for achieving blood glucose goals for individuals who can and want to put extra effort into monitoring their food choices.
People with diabetes can eat the same foods the family enjoys and people with diabetes have to take extra care to make sure that their food is balanced with insulin and oral medications (if they take them), and exercise to help manage their blood glucose levels.
This might sound like a lot of work, but your doctor and/or dietitian can help you create a meal plan that is best for you. When you make healthy food choices, you will improve your overall health and you can even prevent complications such as heart disease and some cancers.
The right meal plan will help you improve your blood glucose, blood pressure, and cholesterol numbers and also help keep your weight on track. Whether you need to lose weight or stay where you are, your meal plan can help.
There is no one perfect food, so including a variety of different foods and watching portion sizes is key to a healthy diet. Also, make sure your choices from each food group provide the highest quality nutrients you can find. In other words, pick foods rich in vitamins, minerals and fiber over those that are processed.
Everyone benefits from healthy eating so the whole family can take part in healthy eating. It takes some planning but you can fit your favorite foods into your meal plan and still manage your blood glucose, blood pressure and cholesterol.
- Avoid foods labelled ‘diabetic’ or ‘suitable for diabetics’. These foods contain similar amounts of calories and fat, and they can affect your blood glucose levels. They are usually more expensive and can have a laxative effect. Stick to your usual foods. If you want to have an occasional treat, go for your normal treats and keep an eye on your portions.
There isn’t one specific “diabetes diet.” Healthy eating helps keep your blood sugar in your target range. It is a critical part of managing your diabetes, because controlling your blood sugar can prevent the complications of diabetes.
- The Centers for Disease Control and Prevention has a free recipes ebook for people and their families with diabetes, you download a free copy here 5.
A registered dietitian can also help you make an eating plan just for you. It should take into account your weight, medicines, lifestyle, and other health problems you have.
- To find out about your body mass index (BMI), you can use a FREE online BMI calculators from the Centers for Disease Control and Prevention (CDC) – for Adults 6 and for Children 7
- To find out What and How Much To Eat, you can use a FREE, award-winning, state-of-the-art, online diet and activity tracking tool called SuperTracker 8 from the United States Department of Agriculture Center for Nutrition Policy and Promotion 8. This free application empowers you to build a healthier diet, manage weight, and reduce your risk of chronic diet-related diseases. You can use SuperTracker 8 to determine what and how much to eat; track foods, physical activities, and weight; and personalize with goal setting, virtual coaching, and journaling.
SuperTracker website 8
- To find out about how many calories you should eat to lose weight according to your weight, age, sex, height and physical activity, you can use a FREE online app Body Weight Planner 9
- To find out about the 5 Food Groups you should have on your plate for a meal, you can use a FREE online app ChooseMyPlate 10
Energy balance
Matching the amount of food you eat with the amount of energy you burn through activity and exercise is important. Putting too much fuel in your body can lead to weight gain. Being overweight or obese can make it difficult to manage your diabetes and can increase the risk of heart disease, stroke and cancer.
Limit foods high in energy such as take away foods, sweet biscuits, cakes, sugar sweetened drinks and fruit juice, lollies, chocolate and savoury snacks. Some people have a healthy diet but eat too much. Reducing your portion size is one way to decrease the amount of energy you eat. Being active has many benefits. Along with healthy eating, regular physical activity can help you to manage your blood glucose levels, reduce your blood fats (cholesterol and triglycerides) and maintain a healthy weight.
Learn more about exercise and maintaining a healthy weight.
Carbohydrate
Carbohydrate foods play an important role in your diet. They are the best energy source for your body, especially your brain. When carbohydrates are digested they break down to form glucose in the bloodstream. Insulin takes the glucose out of the blood and puts it into the muscles, liver and other cells in the body where it is used to provide energy. Most carbohydrate containing foods are also very good sources of fibre, vitamins and minerals which keep our body and bowels healthy.
Of the three key nutrients in your food – fat, protein and carbohydrate, carbohydrate is the nutrient that will have the biggest impact on your blood glucose levels. The effect of carbohydrate will depend on i) the amount of carbohydrate you eat and ii) the type of carbohydrate you eat.
Everyone’s carbohydrate needs are different depending on your gender, how active you are, your age and your body weight. Anyone with diabetes should see an Accredited Practising Dietitian to work out the amount of carbohydrate to eat at each meal and snack.
All carbohydrate foods are digested to produce glucose but they do so at different rates – some slow, some fast. The glycemic index or GI is a way of describing how quickly a carbohydrate food is digested and enters the blood stream.
Low GI carbohydrate foods enter the blood stream slowly and have less of an impact on blood glucose levels. Examples of low GI foods include traditional rolled oats, dense wholegrain breads, lentils and legumes, sweet potato, milk, yoghurt, pasta and most types of fresh fruit. The type of carbohydrate you eat is very important as some can cause higher blood glucose after eating. The best combination is to eat moderate amounts of high fibre low GI carbohydrates.
For some people, a lower carbohydrate diet may help with diabetes management. If you are considering reducing the carbohydrate content of your diet, consult your healthcare team for individualised advice.
Sugar
A healthy eating plan for diabetes can include some sugar. It is ok to have a sprinkle of sugar on porridge or a scrape of jam on some low GI high fibre bread. However, foods that are high in added sugars and poor sources of other nutrients should be consumed sparingly. In particular, limit high energy foods such as sweets, lollies and standard soft drinks. Some sugar may also be used in cooking and many recipes can be modified to use less than the amount stated or substituted with an alternative sweetener. Select recipes that are low in fat (particularly saturated fat) and contain some fibre.
Alternative sweeteners
As mentioned above small amounts of sugar as part of a balanced meal plan shouldn’t have a large effect on blood glucose levels. However sweeteners such as Equal, Stevia, Sugarine and Splenda can be used in place of sugar especially if they are replacing large amounts of sugar. Foods and drinks that have been sweetened with an alternative sweetener, such as diet soft drinks and cordials, sugar-free lollies etc., are also best enjoyed occasionally, as they do not have any nutritional benefit and may often take the place of more nutritious foods and drinks, such as fruits, vegetables, dairy, nuts and water.
Protein
Protein foods are needed by the body for growth and repair. Protein does not break down into glucose, so it does not directly raise blood glucose levels.
The main protein foods are:
- Meats, chicken, fish, & tofu
- Eggs
- Nuts & seeds
- Cheese
There are some protein foods which also contain carbohydrate such as milk, yoghurt, lentils and legumes which will have an effect on blood glucose levels but these should still be included as part of a healthy diet.
Drink water
Water is needed for most of the body’s functions and the body needs to be kept hydrated every day. Water is the best drink to have because it contains no extra kilojoules and won’t have an effect on your blood glucose levels. Other good choices are:
- Tea, coffee, herbal tea, water, soda water, plain mineral water
- If you want a sweet drink occasionally products labelled ‘diet’ or ‘low joule’
- If you choose to drink alcohol limit your intake to no more than 2 standard drinks per day with some alcohol free days each week.
To successfully manage diabetes, you need to understand how foods and nutrition affect your body. Food portions and food choices are important. Carbohydrates, fat and protein need to be balanced to ensure blood sugar levels stay as stable as possible. (This is particularly important for people with Type 1 diabetes.)
The key to eating with diabetes is to eat a variety of healthy foods from all food groups, in the amounts your meal plan outlines. For that reason the American Diabetes Association has created:
- The Diabetic Diet Meal Plans 11 and
- A online tool called Create Your Plate 12. With Create Your Plate method, you fill your plate with more non-starchy veggies and smaller portions of starchy foods and protein—no special tools or counting required. You can practice with this interactive tool 12.
The American Diabetes Association’s Create Your Plate online interactive meal planning tool
The American Diabetes Association’s Create Your Plate online interactive meal planning tool divides your daily food requirements according to the percentage daily requirement for each major food groups: 25 percent Protein, 25 percent Grains and Starchy Foods and 50 percent Non-starchy Vegetables 12. Creating your plate lets you still choose the foods you want, but changes the portion sizes so you are getting larger portions of non-starchy vegetables and a smaller portion of starchy foods. The healthy meal combinations are endless.
Using the 7 simple steps to Create Your Plate 12 you can simply and effectively manage your diabetes and lose weight at the same time. When you are ready, you can try new foods within each food category.
Try these seven steps to get started:
- Using your dinner plate, put a line down the middle of the plate. Then on one side, cut it again so you will have three sections on your plate.
- Fill the largest section with non-starchy vegetables.
- Now in one of the small sections, put grains and starchy foods.
- And then in the other small section, put your protein.
- Add a serving of fruit, a serving of dairy or both as your meal plan allows.
- Choose healthy fats in small amounts. For cooking, use oils. For salads, some healthy additions are nuts, seeds, avocado and vinaigrettes.
- To complete your meal, add a low-calorie drink like water, unsweetened tea or coffee.
The food groups are :
Vegetables
- Non-starchy Vegetables 13
The following is a list of common non-starchy vegetables:
- Amaranth or Chinese spinach
- Artichoke
- Artichoke hearts
- Asparagus
- Baby corn
- Bamboo shoots
- Beans (green, wax, Italian)
- Bean sprouts
- Beets
- Brussels sprouts
- Broccoli
- Cabbage (green, bok choy, Chinese)
- Carrots
- Cauliflower
- Celery
- Chayote
- Coleslaw (packaged, no dressing)
- Cucumber
- Daikon
- Eggplant
- Greens (collard, kale, mustard, turnip)
- Hearts of palm
- Jicama
- Kohlrabi
- Leeks
- Mushrooms
- Okra
- Onions
- Pea pods
- Peppers
- Radishes
- Rutabaga
- Salad greens (chicory, endive, escarole, lettuce, romaine, spinach, arugula, radicchio, watercress)
- Sprouts
- Squash (cushaw, summer, crookneck, spaghetti, zucchini)
- Sugar snap peas
- Swiss chard
- Tomato
- Turnips
- Water chestnuts
- Yard-long beans
Generally, non-starchy vegetables have about 5 grams of carbohydrate in ½ cup cooked or 1 cup raw. Most of the carbohydrate is fiber so unless you eat more than 1 cup of cooked or 2 cups of raw at a time, you may not need to count the carbohydrates from the non-starchy vegetables.
The best choices are fresh, frozen and canned vegetables and vegetable juices without added sodium, fat or sugar.
If using canned or frozen vegetables, look for ones that say low sodium or no salt added on the label.
As a general rule, frozen or canned vegetables in sauces are higher in both fat and sodium.
If using canned vegetables with sodium, drain the vegetables and rinse with water. Then cook the rinsed vegetables in fresh water. This will cut back on how much sodium is left on the vegetables.
For good health, try to eat at least 3-5 servings of vegetables a day. This is a minimum and more is better! A serving of vegetables is:
- ½ cup of cooked vegetables or vegetable juice
- 1 cup of raw vegetables
- Starchy Starchy Vegetables and Grains 14
Grains
- At least half of your grains for the day should be whole grains. A whole grain is the entire grain—which includes the bran, germ and endosperm (starchy part).
The most popular grain in the US is wheat so that will be our example. To make 100% whole wheat flour, the entire wheat grain is ground up. “Refined” flours like white and enriched wheat flour include only part of the grain – the starchy part, and are not whole grain. They are missing many of the nutrients found in whole wheat flour.
Examples of whole grain wheat products include 100% whole wheat bread, pasta, tortillas, and crackers. But don’t stop there! There are many whole grains to choose from.
Finding whole grain foods can be a challenge. Some foods only contain a small amount of whole grain but will say it contains whole grain on the front of the package. For all cereals and grains, read the ingredient list and look for the following sources of whole grains as the first ingredient:
Best Choices
- Bulgur (cracked wheat)
- Whole wheat flour/
- Whole oats/oatmeal
- Whole grain corn/corn meal
- Popcorn
- Brown rice
- Whole rye
- Whole grain barley
- Whole farro
- Wild rice
- Buckwheat
- Buckwheat flour
- Triticale
- Millet
- Quinoa
- Sorghum
If you suffer from Celiac disease or gluten intolerance :
- Celiac disease is a digestive disorder. When someone with celiac disease eats food containing gluten, their body reacts by damaging the small intestine. Uncomfortable symptoms such as abdominal pain often occur. The damage to the small intestine also interferes with the body’s ability to make use of the nutrients in food. About 1% of the total population has celiac disease. It is more common in people with type 1 diabetes. An estimated 10% of people with type 1 also have celiac. The only way to manage celiac disease is to completely avoid all foods that have gluten. Following a gluten-free diet will prevent permanent damage to your body and will help you feel better.
- Gluten Intolerance : There are also many people who are said to have a gluten intolerance. When these people eat foods that contain gluten, they also experience uncomfortable symptoms. However, they test negative for celiac disease and actual damage to their small intestine does not occur. More research about gluten intolerance is needed, but avoiding foods with gluten should help to relieve these symptoms.
Gluten is a protein found in wheat, rye, barley and all foods that are made with these grains.
Starchy Vegetables
Starchy vegetables are great sources of vitamins, minerals and fiber . The best choices do not have added fats, sugar or sodium.
Try a variety such as:
- Parsnip
- Plantain
- Potato
- Pumpkin
- Acorn squash
- Butternut squash
- Green Peas
- Corn
Best Choices of Dried Beans, Legumes, Peas and Lentils
Try to include dried beans into several meals per week. They are a great source of protein and are loaded with fiber, vitamins and minerals.
- Dried beans such as black, lima, and pinto
- Lentils
- Dried peas such as black-eyed and split
- Fat-free refried beans
- Vegetarian baked beans
Fruits 15
Wondering if you can eat fruit ? Yes !
Fruits are loaded with vitamins, minerals and fiber just like vegetables.
Fruit contains carbohydrate so you need to count it as part of your meal plan. Having a piece of fresh fruit or fruit salad for dessert is a great way to satisfy your sweet tooth and get the extra nutrition you’re looking for.
The best choices of fruit are any that are fresh, frozen or canned without added sugars.
- Choose canned fruits in juice or light syrup
- Dried fruit and 100% fruit juice are also nutritious choices, but the portion sizes are small so they may not be as filling as other choices. Only 2 tablespoons of dried fruit like raisins or dried cherries contains 15 grams of carbohydrate so be cautious with your portion sizes!
- Includes oranges, melon, berries, apples, bananas, and grapes
For Carbohydrate Counters
- A small piece of whole fruit or about ½ cup of frozen or canned fruit has about 15 grams of carbohydrate. Servings for most fresh berries and melons are from ¾ – 1 cup.
- Fruit juice can range from 1/3 -1/2 cup for 15 grams of carbohydrate.
Fruit can be eaten in exchange for other sources of carbohydrate in your meal plan such as starches, grains, or dairy.
Protein 16
The biggest difference among foods in this group is how much fat they contain, and for the vegetarian proteins, whether they have carbohydrate.
Meats do not contain carbohydrate so they do not raise blood glucose levels. A balanced meal plan usually has about 2-5 ounces of meat.
Most plant-based protein foods, like beans and soy products, and any breaded meats contain carbohydrate. It’s best to read food labels carefully for these foods.
In general there is about 15 grams of carbohydrate in ½ cup beans, and between 5 to 15 grams in soy-based products like veggie burgers and “chicken” nuggets.
The best choices are:
- Plant-based proteins
- Fish and seafood
- Chicken and other poultry
- Cheese and eggs
Fish and Seafood
Try to include fish at least 2 times per week.
- Fish high in omega-3 fatty acids like Albacore tuna, herring, mackerel, rainbow trout, sardines, and salmon
- Other fish including catfish, cod, flounder, haddock, halibut, orange roughy, and tilapia
- Shellfish including clams, crab, imitation shellfish, lobster, scallops, shrimp, oysters.
Poultry
Choose poultry without the skin for less saturated fat and cholesterol.
- Chicken, turkey, cornish hen
Game
- Buffalo, ostrich, rabbit, venison
- Dove, duck, goose, or pheasant (no skin)
Beef, Pork, Veal, Lamb
If you decide to have these, choose the leanest options, which are:
- Select or Choice grades of beef trimmed of fat including: chuck, rib, rump roast, round, sirloin, cubed, flank, porterhouse, T-bone steak, tenderloin
- Beef jerky
- Lamb: chop, leg, or roast
- Organ meats: heart, kidney, liver
- Veal: loin chop or roast
- Pork: Canadian bacon, center loin chop, ham, tenderloin
Cheese and Eggs
- Reduced-fat cheese
- Cottage cheese
- Egg whites and egg substitutes
Dairy 17
Including sources of dairy in your diet is an easy way to get calcium and high-quality protein.
The best choices of dairy products are:
- Fat-free or low-fat (1% milk)
- Plain non-fat yogurt (regular or Greek yogurt)
- non-fat light yogurt (regular or Greek yogurt)
- unflavored fortified soy milk
If you are lactose intolerant or don’t like milk, you may want to try fortified soy milk, rice milk, or almond milk as a source of calcium and vitamin D.
Tips for Carb Counters
- 1 cup of milk or yogurt is equal to 1 small piece of fruit or 1 slice of bread
- Each 1 cup serving of milk or 6 ounce serving of yogurt has about 12 grams of carbohydrate and 8 grams of protein. Greek yogurt is higher in protein than regular yogurt, with about 12 grams per 6 ounce serving.
- If you are trying to switch to lower fat dairy products, take the time to get used to the taste and texture difference. For example, first change from whole milk to 2%. Then to 1% or non-fat milk.
- Switching from whole to 1% milk will save you 70 calories and 4 grams of saturated fat in every serving!
Eat more fiber by eating more whole-grain foods 18. Whole grains can be found in:
- Breakfast cereals made with 100% whole grains.
- Oatmeal.
- Whole grain rice.
- Whole-wheat bread, bagels, pita bread, and tortillas.
What Can you Drink ?
Food often takes center stage when it comes to diabetes. But don’t forget that the beverages you drink can also have an effect on your weight and blood glucose!
The American Diabetes Association recommends choosing zero-calorie or very low-calorie drinks 19. This includes:
- Water
- Unsweetened teas
- Coffee no added sugar
- Diet soda
- Other low-calorie drinks and drink mixes
You can also try flavoring your water with a squeeze of lemon or lime juice for a light, refreshing drink with some flavor. All of these drinks provide minimal calories and carbohydrate. If you choose to drink juice, be sure the label says it is 100% juice with no sugar added. Juice provides a lot of carbohydrates in a small portion, so be sure to count it in your meal plan. Usually about 4 ounces or less of juice contains 15 grams of carbohydrate and 50 or more calories.
What to Avoid
Avoid sugary drinks like regular soda, fruit punch, fruit drinks, energy drinks, sweet tea, and other sugary drinks. These will raise blood glucose and can provide several hundred calories in just one serving! See for yourself:
- One 12-ounce can of regular soda has about 150 calories and 40 grams of carbohydrate. This is the same amount of carbohydrate in 10 teaspoons of sugar!
- One cup of fruit punch and other sugary fruit drinks have about 100 calories (or more) and 30 grams of carbohydrate.
Make your calories count with these nutritious foods:
- Healthy carbohydrates. During digestion, sugars (simple carbohydrates) and starches (complex carbohydrates) break down into blood glucose. Focus on the healthiest carbohydrates, such as fruits, vegetables, whole grains, legumes (beans, peas and lentils) and low-fat dairy products.
- Fiber-rich foods. Dietary fiber includes all parts of plant foods that your body can’t digest or absorb. Fiber moderates how your body digests and helps control blood sugar levels. Foods high in fiber include vegetables, fruits, nuts, legumes (beans, peas and lentils), whole-wheat flour and wheat bran.
- Heart-healthy fish. Eat heart-healthy fish at least twice a week. Fish can be a good alternative to high-fat meats. For example, cod, tuna and halibut have less total fat, saturated fat and cholesterol than do meat and poultry. Fish such as salmon, mackerel, tuna, sardines and bluefish are rich in omega-3 fatty acids, which promote heart health by lowering blood fats called triglycerides. Avoid fried fish and fish with high levels of mercury, such as tilefish, swordfish and king mackerel.
- “Good” fats. Foods containing monounsaturated and polyunsaturated fats can help lower your cholesterol levels. These include avocados, almonds, pecans, walnuts, olives, and canola, olive and peanut oils. But don’t overdo it, as all fats are high in calories.
The glycemic index, or GI, measures how a carbohydrate-containing food raises blood glucose. Foods are ranked based on how they compare to a reference food — either glucose or white bread.
A food with a high GI raises blood glucose more than a food with a medium or low GI.
Meal planning with the GI involves choosing foods that have a low or medium GI. If eating a food with a high GI, you can combine it with low GI foods to help balance the meal.
Examples of carbohydrate-containing foods with a low GI include dried beans and legumes (like kidney beans and lentils), all non-starchy vegetables, some starchy vegetables like sweet potatoes, most fruit, and many whole grain breads and cereals (like barley, whole wheat bread, rye bread, and all-bran cereal).
Meats and fats don’t have a GI because they do not contain carbohydrate.
Low GI Foods (55 or less)
- 100% stone-ground whole wheat or pumpernickel bread
- Oatmeal (rolled or steel-cut), oat bran, muesli
- Pasta, converted rice, barley, bulgar
- Sweet potato, corn, yam, lima/butter beans, peas, legumes and lentils
- Most fruits, non-starchy vegetables and carrots
Medium GI (56-69)
- Whole wheat, rye and pita bread
- Quick oats
- Brown, wild or basmati rice, couscous
High GI (70 or more)
- White bread or bagel
- Corn flakes, puffed rice, bran flakes, instant oatmeal
- Shortgrain white rice, rice pasta, macaroni and cheese from mix
- Russet potato, pumpkin
- Pretzels, rice cakes, popcorn, saltine crackers
- melons and pineapple
What Affects the GI of a Food ?
Fat and fiber tend to lower the GI of a food. As a general rule, the more cooked or processed a food, the higher the GI; however, this is not always true.
Below are a few specific examples of other factors that can affect the GI of a food:
- Ripeness and storage time — the more ripe a fruit or vegetable is, the higher the GI.
- Processing — juice has a higher GI than whole fruit; mashed potato has a higher GI than a whole baked potato, stone ground whole wheat bread has a lower GI than whole wheat bread.
- Cooking methods — how long a food is cooked (al dente pasta has a lower GI than soft-cooked pasta), frying, boiling and baking.
- Fibre: wholegrains and high-fibre foods act as a physical barrier that slows down the absorption of carbohydrate. This is not the same as ‘wholemeal’, where, even though the whole of the grain is included, it has been ground up instead of left whole. For example, some mixed grain breads that include wholegrains have a lower GI than wholemeal or white bread.
- Fat lowers the GI of a food. For example, chocolate has a medium GI because of it’s fat content, and crisps will actually have a lower GI than potatoes cooked without fat.
- Protein lowers the GI of food. Milk and other diary products have a low GI because they are high in protein and contain fat.
- Variety — converted long-grain white rice has a lower GI than brown rice but short-grain white rice has a higher GI than brown rice.
Your food choices matter a lot when you’ve got diabetes. Some are better than others.
Nothing is completely off limits. Even items that you might think of as “the worst” could be occasional treats — in tiny amounts. But they won’t help you nutrition-wise, and it’s easiest to manage your diabetes if you mainly stick to the “best” options.
What is the difference between Glycemic Index (GI) and Glycemic Load (GL) ?
Your blood glucose rises and falls when you eat a meal containing carbs. How high it rises and how long it remains high depends on the quality of the carbohydrates (the GI) and the quantity (the serve size). Glycemic load or GL combines both the quality and quantity of carbohydrate in one ‘number’. It’s the best way to predict blood glucose values of different types and amounts of food.
The formula is:
GL = (GI x available carbohydrate in a 100g serving) divided by 100.
Let’s take a single apple as an example.
It has a GI of 40 and it contains 15 grams of carbohydrate.
GL = 40 x 15/100 = 6 g
What about a small baked potato?
Its GI is 80 and it contains 15 g of carbohydrate.
GL = 80 x 15/100 = 12 g
You can think of GL as the amount of carbohydrate in a food “adjusted” for its glycemic potency.
- Low GL = <10
- Medium GL = 11-19
- High GL = >20
Therefore the Glycemic Load takes into account the amount of carbohydrate consumed and is a more accurate measure of the impact of a food on blood sugars. As a general rule foods that have a low GL usually have a low GI and those with a medium to high GL value almost always have a very high GI value.
Here is an abbreviated chart of the glycemic index and glycemic load, per serving, for more than 100 common foods.
| FOOD | Glycemic index (glucose = 100) | Serving size (grams) | Glycemic load per serving |
| BAKERY PRODUCTS AND BREADS | |||
| Banana cake, made with sugar | 47 | 60 | 14 |
| Banana cake, made without sugar | 55 | 60 | 12 |
| Sponge cake, plain | 46 | 63 | 17 |
| Vanilla cake made from packet mix with vanilla frosting (Betty Crocker) | 42 | 111 | 24 |
| Apple muffin, made with rolled oats and sugar | 44 | 60 | 13 |
| Apple muffin, made with rolled oats and without sugar | 48 | 60 | 9 |
| Waffles, Aunt Jemima® | 76 | 35 | 10 |
| Bagel, white, frozen | 72 | 70 | 25 |
| Baguette, white, plain | 95 | 30 | 14 |
| Coarse barley bread, 80% kernels | 34 | 30 | 7 |
| Hamburger bun | 61 | 30 | 9 |
| Kaiser roll | 73 | 30 | 12 |
| Pumpernickel bread | 56 | 30 | 7 |
| 50% cracked wheat kernel bread | 58 | 30 | 12 |
| White wheat flour bread, average | 75 | 30 | 11 |
| Wonder® bread, average | 73 | 30 | 10 |
| Whole wheat bread, average | 69 | 30 | 9 |
| 100% Whole Grain® bread (Natural Ovens) | 51 | 30 | 7 |
| Pita bread, white | 68 | 30 | 10 |
| Corn tortilla | 52 | 50 | 12 |
| Wheat tortilla | 30 | 50 | 8 |
| BEVERAGES | |||
| Coca Cola® (US formula) | 63 | 250 mL | 16 |
| Fanta®, orange soft drink | 68 | 250 mL | 23 |
| Lucozade®, original (sparkling glucose drink) | 95 | 250 mL | 40 |
| Apple juice, unsweetened | 41 | 250 mL | 12 |
| Cranberry juice cocktail (Ocean Spray®) | 68 | 250 mL | 24 |
| Gatorade, orange flavor (US formula) | 89 | 250 mL | 13 |
| Orange juice, unsweetened, average | 50 | 250 mL | 12 |
| Tomato juice, canned, no sugar added | 38 | 250 mL | 4 |
| BREAKFAST CEREALS AND RELATED PRODUCTS | |||
| All-Bran®, average | 44 | 30 | 9 |
| Coco Pops®, average | 77 | 30 | 20 |
| Cornflakes®, average | 81 | 30 | 20 |
| Cream of Wheat® | 66 | 250 | 17 |
| Cream of Wheat®, Instant | 74 | 250 | 22 |
| Grape-Nuts® | 75 | 30 | 16 |
| Muesli, average | 56 | 30 | 10 |
| Oatmeal, average | 55 | 250 | 13 |
| Instant oatmeal, average | 79 | 250 | 21 |
| Puffed wheat cereal | 80 | 30 | 17 |
| Raisin Bran® | 61 | 30 | 12 |
| Special K® (US formula) | 69 | 30 | 14 |
| GRAINS | |||
| Pearled barley, average | 25 | 150 | 11 |
| Sweet corn on the cob | 48 | 60 | 14 |
| Couscous | 65 | 150 | 9 |
| Quinoa | 53 | 150 | 13 |
| White rice, boiled, type non-specified | 72 | 150 | 29 |
| Quick cooking white basmati | 63 | 150 | 26 |
| Brown rice, steamed | 50 | 150 | 16 |
| Parboiled Converted white rice (Uncle Ben’s®) | 38 | 150 | 14 |
| Whole wheat kernels, average | 45 | 50 | 15 |
| Bulgur, average | 47 | 150 | 12 |
| COOKIES AND CRACKERS | |||
| Graham crackers | 74 | 25 | 13 |
| Vanilla wafers | 77 | 25 | 14 |
| Shortbread | 64 | 25 | 10 |
| Rice cakes, average | 82 | 25 | 17 |
| Rye crisps, average | 64 | 25 | 11 |
| Soda crackers | 74 | 25 | 12 |
| DAIRY PRODUCTS AND ALTERNATIVES | |||
| Ice cream, regular, average | 62 | 50 | 8 |
| Ice cream, premium (Sara Lee®) | 38 | 50 | 3 |
| Milk, full-fat, average | 31 | 250 mL | 4 |
| Milk, skim, average | 31 | 250 mL | 4 |
| Reduced-fat yogurt with fruit, average | 33 | 200 | 11 |
| FRUITS | |||
| Apple, average | 36 | 120 | 5 |
| Banana, raw, average | 48 | 120 | 11 |
| Dates, dried, average | 42 | 60 | 18 |
| Grapefruit | 25 | 120 | 3 |
| Grapes, black | 59 | 120 | 11 |
| Oranges, raw, average | 45 | 120 | 5 |
| Peach, average | 42 | 120 | 5 |
| Peach, canned in light syrup | 52 | 120 | 9 |
| Pear, raw, average | 38 | 120 | 4 |
| Pear, canned in pear juice | 44 | 120 | 5 |
| Prunes, pitted | 29 | 60 | 10 |
| Raisins | 64 | 60 | 28 |
| Watermelon | 72 | 120 | 4 |
| BEANS AND NUTS | |||
| Baked beans | 40 | 150 | 6 |
| Black-eyed peas | 50 | 150 | 15 |
| Black beans | 30 | 150 | 7 |
| Chickpeas | 10 | 150 | 3 |
| Chickpeas, canned in brine | 42 | 150 | 9 |
| Navy beans, average | 39 | 150 | 12 |
| Kidney beans, average | 34 | 150 | 9 |
| Lentils | 28 | 150 | 5 |
| Soy beans, average | 15 | 150 | 1 |
| Cashews, salted | 22 | 50 | 3 |
| Peanuts | 13 | 50 | 1 |
| PASTA and NOODLES | |||
| Fettucini | 32 | 180 | 15 |
| Macaroni, average | 50 | 180 | 24 |
| Macaroni and Cheese (Kraft®) | 64 | 180 | 33 |
| Spaghetti, white, boiled, average | 46 | 180 | 22 |
| Spaghetti, white, boiled 20 min | 58 | 180 | 26 |
| Spaghetti, whole-grain, boiled | 42 | 180 | 17 |
| SNACK FOODS | |||
| Corn chips, plain, salted | 42 | 50 | 11 |
| Fruit Roll-Ups® | 99 | 30 | 24 |
| M & M’s®, peanut | 33 | 30 | 6 |
| Microwave popcorn, plain, average | 65 | 20 | 7 |
| Potato chips, average | 56 | 50 | 12 |
| Pretzels, oven-baked | 83 | 30 | 16 |
| Snickers Bar®, average | 51 | 60 | 18 |
| VEGETABLES | |||
| Green peas | 54 | 80 | 4 |
| Carrots, average | 39 | 80 | 2 |
| Parsnips | 52 | 80 | 4 |
| Baked russet potato | 111 | 150 | 33 |
| Boiled white potato, average | 82 | 150 | 21 |
| Instant mashed potato, average | 87 | 150 | 17 |
| Sweet potato, average | 70 | 150 | 22 |
| Yam, average | 54 | 150 | 20 |
| MISCELLANEOUS | |||
| Hummus (chickpea salad dip) | 6 | 30 | 0 |
| Chicken nuggets, frozen, reheated in microwave oven 5 min | 46 | 100 | 7 |
| Pizza, plain baked dough, served with parmesan cheese and tomato sauce | 80 | 100 | 22 |
| Pizza, Super Supreme (Pizza Hut®) | 36 | 100 | 9 |
| Honey, average | 61 | 25 | 12 |
The complete list of the glycemic index and glycemic load for more than 1,000 foods can be found in the article “International tables of glycemic index and glycemic load values: 2008” by Fiona S. Atkinson, Kaye Foster-Powell, and Jennie C. Brand-Miller in the December 2008 issue of Diabetes Care, Vol. 31, number 12, pages 2281-2283. (Source 20).
Benefits of Low Glycaemic Index or Low Glycaemic Load Diets for Diabetes Mellitus
To assess the effects of low glycaemic index or low glycaemic load, diets on glycaemic control in people with diabetes, eleven relevant randomised controlled trials, lasting 1 to 12 months, involving 402 participants were analysed 21.
There was a significant decrease in the glycated haemoglobin A1c (HbA1c) -0.5%. Episodes of hypoglycaemia were significantly fewer with low glycaemic index or low glycaemic load compared to high GI diet in one trial (difference of -0.8 episodes per patient per month), and proportion of participants reporting more than 15 hyperglycaemic episodes per month was lower for low-GI diet compared to measured carbohydrate exchange diet in another study (35% versus 66%). No study reported on mortality, morbidity or costs. The review authors concluded a low-GI diet can improve glycaemic control in diabetes without compromising hypoglycaemic events 21. This result is consistent with another smaller trial involving eight type 2 diabetes mellitus patients who were given carbohydrate foods with either a high or low glycemic index over a 2 weeks period 22.
I) Starches
Your body needs carbs. But you want to choose wisely. Use this list as a guide.
Best Choices
- Whole grains, such as brown rice, oatmeal, quinoa, millet, or amaranth
- Baked sweet potato
- Items made with whole grains and no (or very little) added sugar
Worst Choices
- Processed grains, such as white rice or white flour
- Cereals with little whole grains and lots of sugar
- White bread
- French fries
- Fried white-flour tortillas
II) Vegetables
Load up! You’ll get fiber and very little fat or salt (unless you add them). Remember, potatoes and corn count as carbs.
Best Choices
- Fresh veggies, eaten raw or lightly steamed, roasted, or grilled
- Plain frozen vegetables, lightly steamed
- Greens such as kale, spinach, and arugula. Iceberg lettuce is not as great, because it’s low in nutrients.
- Low sodium or unsalted canned vegetables
- Go for a variety of colors: dark greens, red or orange (think of carrots or red peppers), whites (onions) and even purple (eggplants). The 2015 U.S. guidelines recommend 2.5 cups of veggies per day.
Worst Choices
- Canned vegetables with lots of added sodium
- Veggies cooked with lots of added butter, cheese, or sauce
- Pickles, if you need to limit sodium — otherwise, pickles are okay.
- Sauerkraut, for the same reason as pickles — so, limit them if you have high blood pressure
III) Fruits
They give you carbohydrates, vitamins, minerals, and fiber. Most are naturally low in fat and sodium. But they tend to have more carbs than vegetables do.
Best Choices
- Fresh fruit
- Plain frozen fruit or fruit canned without added sugar
- Sugar-free or low-sugar jam or preserves
- No-sugar-added apple sauce
Worst Choices
- Canned fruit with heavy sugar syrup
- Chewy fruit rolls
- Regular jam, jelly, and preserves (unless you have a very small portion)
- Sweetened apple sauce
- Fruit punch, fruit drinks, fruit juice drinks
IV) Protein
You have lots of choices, including beef, chicken, fish, pork, turkey, seafood, beans, cheese, eggs, nuts, and tofu.
Best Choices
The American Diabetes Association lists these as the top options:
- Plant-based proteins, such as beans, nuts, seeds, or tofu
- Fish and seafood
- Chicken and other poultry (Choose the breast meat if possible.)
- Eggs and low-fat dairy
If you eat meat, keep it low in fat. Trim the skin off poultry.
Try to include some plant-based protein from beans, nuts, or tofu, even if you’re not a vegetarian or vegan. You’ll get nutrients and fiber that aren’t in animal products.
Worst Choices
- Fried meats
- Higher-fat cuts of meat, such as ribs
- Pork bacon
- Regular cheeses
- Poultry with skin
- Deep-fried fish
- Deep-fried tofu
- Beans prepared with lard
V) Dairy
Keep it low in fat. If you want to splurge, keep your portion small.
Best Choices
- 1% or skim milk
- Low-fat yogurt
- Low-fat cottage cheese
- Low-fat or nonfat sour cream
Worst Choices
- Regular yogurt
- Regular cottage cheese
- Regular sour cream
- Regular ice cream
- Regular half-and-half
VI) Fats, Oils, and Sweets
They’re tough to resist. But it’s easy to get too much and gain weight, which makes it harder to manage your diabetes.
Best Choices
- Natural sources of vegetable fats, such as nuts, seeds, or avocados (high in calories, so keep portions small)
- Foods that give you omega-3 fatty acids, such as salmon, tuna, or mackerel
- Plant-based oils, such as canola, grapeseed, or olive oils
Worst Choices
- Anything with artificial trans fat in it. It’s bad for your heart. Check the ingredient list for anything that’s “partially hydrogenated,” even if the label says it has 0 grams of trans fat.
VII) Drinks
When you down a favorite drink, you may get more calories, sugar, salt, or fat than you bargained for. Read the labels so you know what’s in a serving.
Best Choices
- Water, unflavored or flavored sparkling water
- Unsweetened tea (add a slice of lemon)
- Coffee, black or with added low-fat milk and sugar substitute
Worst Choices
- Light beer, small amounts of wine, or non-fruity mixed drinks
- Regular sodas
- Regular beer, fruity mixed drinks, dessert wines
- Sweetened tea
- Coffee with sugar and cream
- Flavored coffees and chocolate drinks
- Energy drinks
Summary
Healthy eating and an active lifestyle are important for everyone, including people with diabetes. To achieve and maintain a healthy weight, be physically active and choose amounts of nutritious foods and drinks to meet your energy needs. Having a healthy diet and being active is an important part of managing diabetes because it will help manage your blood glucose levels and your body weight.
- Meals that are recommended for people with diabetes are the same as for those without diabetes.
- There is no need to prepare separate meals or buy special foods.
- Everyone including family and friends can enjoy the same healthy and tasty meals together.
- As a guide, we recommend people with diabetes follow the American Dietary Guidelines Healthy Eating for Adults and Healthy Eating for Children.
- Everyone’s needs are different so we recommend everyone with diabetes visit a dietitian for personal advice.
- Enjoy a wide variety of nutritious from these five food groups every day:
a) Plenty of vegetables and different types and colors and legumes/beans.
b) Fruits
c) Grain (cereal) foods, mostly wholegrain and/or high cereal fiber varieties, such as breads, cereals, rice, pasta, noodles, polenta, couscous, quinoa, oats, and barley.
d) Lean meats and poultry, fish, eggs, tofu, nuts and seeds, and legumes/beans.
e) Milk, yogurt, cheese and/or their alternatives, mostly reduced fat.
And drink plenty of water. Limit intake of foods and drinks containing added salt, sugar and saturated and trans fats.

Low Calorie Diet on Weight Loss and the Metabolic Profile of Obese Patients with Type 2 Diabetes Mellitus
A small study 23 with 60 patients (23 males and 37 postmenopausal females) who have type 2 diabetes and are obese, to compare the effects of low calorie diet (1800 kcal/day) plus intensive insulin therapy (4 insulin injections/day) versus low calorie diet (1800 kcal/day) plus conventional insulin therapy (2/3 insulin injections/day). At 6 months post-interventions, there were significant reductions were observed in the body weight, body mass index (BMI), HbA1c for all participants and cholesterol. At 1 year, median body weight reduction was 4.5 kg for patients on low calorie diet (1800 kcal/day) plus intensive insulin therapy and 4.8 kg for those on low calorie diet (1800 kcal/day) plus conventional insulin therapy. The conclusion was a 12-month 1800-kcal low calorie dietary intervention achieved significant body weight loss and HbA1c reductions irrespectively of insulin regimen. The low calorie diet (1800 kcal/day) plus conventional insulin therapy was associated with body weight loss greater than 8.0%, whereas low calorie diet (1800 kcal/day) plus intensive insulin therapy was associated with higher rates of normoglycemia 23.
Very Low Calorie Diet in Obese Type 2 Diabetes
A small study was conducted with fifty-one obese subjects (24 with diabetes and 27 obese without diabetes) to compare weight loss and change in body composition in obese subjects with and without type 2 diabetes mellitus during a very-low-calorie diet (VLCD) program 24. After 24 weeks of intervention, there was no difference in weight loss between the 2 groups. Both groups completing the study per protocol had near-identical weight change during the program, with similar weight loss at 24 weeks (diabetes: 8.5 ± 1.3 kg vs control: 9.4 ± 1.2 kg). Change in fat mass index correlated with change in body mass index (BMI) in both groups, but change in fat mass index per unit change in BMI was less in the diabetic group compared with controls, which persisted after adjusting for age, sex, and baseline BMI. Insulin concentrations remained higher and peak β-hydroxybutyrate concentrations were lower in the diabetic compared with the control group. The conclusion was while following a 24-week very-low-calorie diet program, obese subjects with and without diabetes achieved comparable weight loss; but the decrease in body fat per unit weight loss was less in diabetic subjects. Hyperinsulinemia may have inhibited lipolysis in the diabetic group; however, further investigation into other factors is needed 24.
Low Carbohydrate Low Calorie Diet in type 2 Diabetes
In a very small study 25 comparing the effects of low carbohydrate low calorie diet (1800 kcal for men and 1600 kcal for women, distributed as 20 % carbohydrates, 30 % protein and 50 % fat) and high carbohydrate low calorie diet (1600-1800 kcal for men and 1400-1600 kcal for women, consisted of approximately 60 % carbohydrates, 15 % protein and 25 % fat) in two groups of obese patients with type 2 diabetes. The diets were tested with regard to glycaemic control and bodyweight. A group of 16 obese patients with type 2 diabetes was advised on a low-carbohydrate diet, Fifteen obese diabetes patients on a high-carbohydrate diet were control group. Positive effects on the glucose levels were seen very soon. After 6 months a marked reduction in bodyweight of patients in the low-carbohydrate diet group was observed, and this remained one year later. After 6 months the mean changes in the low-carbohydrate group and the control (high carbohydrate low calorie diet) group respectively were fasting blood glucose: -3.4 and -0.6 mmol/l; HBA1c: -1.4 % and -0.6 %; Body Weight: -11.4 kg and -1.8 kg; BMI: -4.1 kg/m2 and -0.7 kg/m2. In conclusion, a low-carbohydrate diet is an effective tool in the treatment of obese patients with type 2 diabetes 25.
- J Health Popul Nutr. 2012 Dec; 30(4): 447–455. Factors Associated with Consumption of Diabetic Diet among Type 2 Diabetic Subjects from Ahmedabad, Western India. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3763616/[↩]
- U.S. National Library of Medicine, Medline Plus. Diabetic Diet. https://medlineplus.gov/diabeticdiet.html[↩]
- Evert, A.B. and Boucher, J.L. et al; Nutrition Therapy Recommendations For the Management of Adults with Diabetes,:Position Statement by the ADA, Diabetes Care 2013, 363821-42.[↩]
- Standards of Medical Care in Diabetes-2013 Diabetes Care 2013;36(Suppl. 1):S11–S66[↩]
- https://www.cdc.gov/diabetes/ndep/cdcinfo/ndep_pdf/tasty-recipes-508.pdf[↩]
- BMI Calculator Adults. https://www.cdc.gov/healthyweight/assessing/bmi/adult_BMI/english_bmi_calculator/bmi_calculator.html[↩]
- BMI Calculator Children. https://nccd.cdc.gov/dnpabmi/Calculator.aspx[↩]
- https://supertracker.usda.gov/[↩][↩][↩][↩]
- Body Weight Planner. https://www.supertracker.usda.gov/bwp/index.html[↩]
- ChooseMyPlate. https://www.choosemyplate.gov/[↩]
- American Diabetes Association. All of Our Meal Plans. http://www.diabetes.org/mfa-recipes/meal-plans/meal-plans.html[↩]
- American Diabetes Association. Create Your Plate. http://www.diabetes.org/food-and-fitness/food/planning-meals/create-your-plate/[↩][↩][↩][↩]
- American Diabetes Association. Non-starchy Vegetables. http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/non-starchy-vegetables.html[↩]
- American Diabetes Association. Grains and Starchy Vegetables. http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/grains-and-starchy-vegetables.html[↩]
- American Diabetes Association. Fruits. http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/fruits.html[↩]
- American Diabetes Association. Protein Foods. http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/meat-and-plant-based-protein.html[↩]
- American Diabetes Association. Dairy. http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/dairy.html[↩]
- Centers for Disease Control and Prevention. Managing Diabetes: Eat Right ! https://www.cdc.gov/diabetes/managing/eatright.html[↩]
- American Diabetes Association. What Can I Drink ? http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/making-healthy-food-choices/what-can-i-drink.html[↩]
- Diabetes Care 2008 Dec; 31(12): 2281-2283. https://doi.org/10.2337/dc08-1239. International Tables of Glycemic Index and Glycemic Load Values: 2008. http://care.diabetesjournals.org/content/31/12/2281.full[↩]
- Cochrane Review 21 January 2009. Low glycaemic index, or low glycaemic load, diets for diabetes mellitus. http://www.cochrane.org/CD006296/ENDOC_low-glycaemic-index-or-low-glycaemic-load-diets-for-diabetes-mellitus[↩][↩]
- Am J Clin Nutr. 1988 Aug;48(2):248-54. Low-glycemic-index starchy foods in the diabetic diet. https://www.ncbi.nlm.nih.gov/pubmed/3407604[↩]
- Adv Ther. 2016 Mar;33(3):447-59. doi: 10.1007/s12325-016-0300-2. Epub 2016 Feb 17. Obese Patients with Type 2 Diabetes on Conventional Versus Intensive Insulin Therapy: Efficacy of Low-Calorie Dietary Intervention. https://www.ncbi.nlm.nih.gov/pubmed/26886777[↩][↩]
- Metabolism. 2012 Jun;61(6):873-82. doi: 10.1016/j.metabol.2011.10.017. Epub 2011 Dec 5. Less fat reduction per unit weight loss in type 2 diabetic compared with nondiabetic obese individuals completing a very-low-calorie diet program. https://www.ncbi.nlm.nih.gov/pubmed/22146094?dopt=Abstract[↩][↩]
- Ups J Med Sci. 2005;110(1):69-73. Lasting improvement of hyperglycaemia and bodyweight: low-carbohydrate diet in type 2 diabetes–a brief report. https://www.ncbi.nlm.nih.gov/pubmed/15801687?dopt=Abstract[↩][↩]