Adrenalectomy
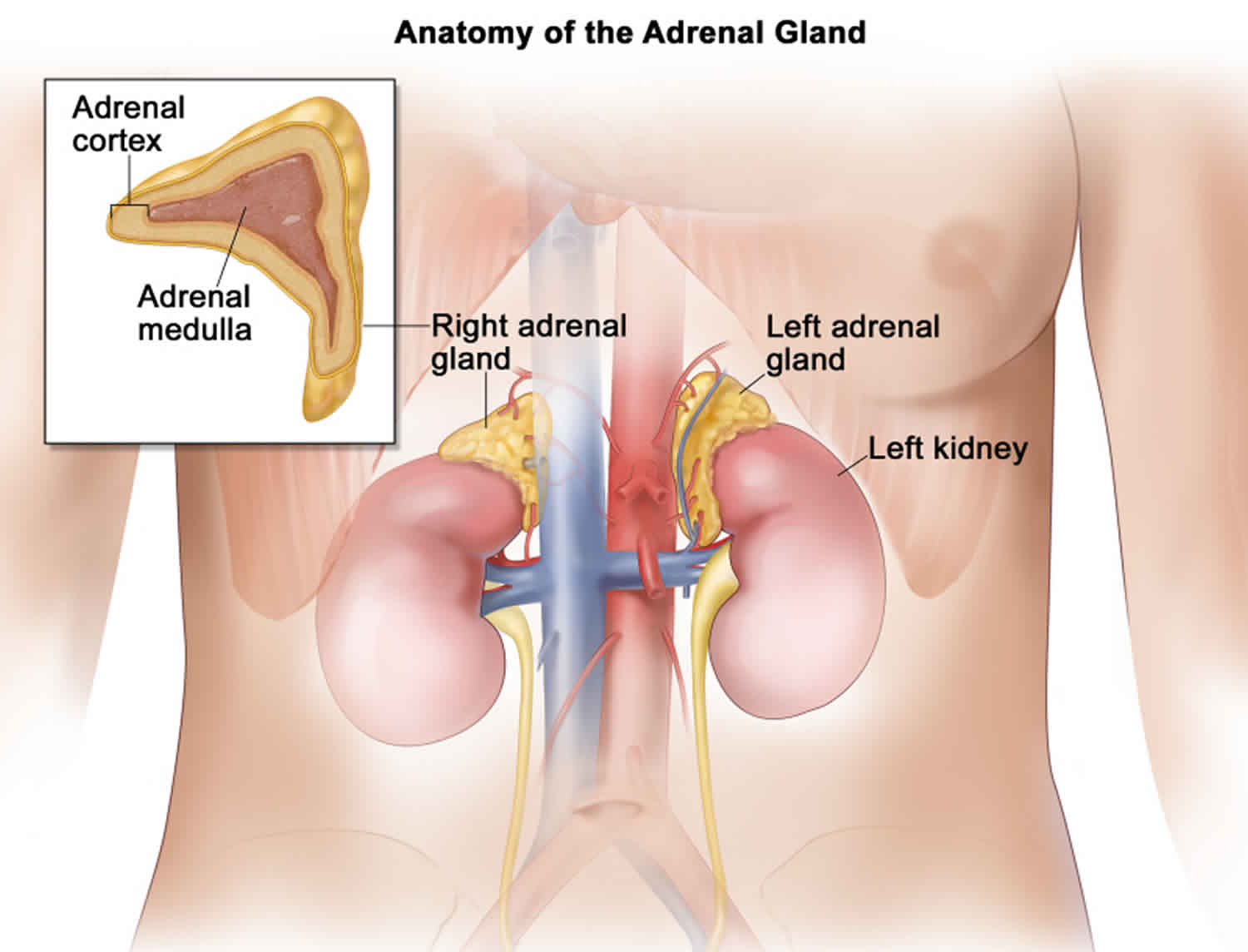
Adrenalectomy is a surgery to remove one or both adrenal glands. The adrenal glands are part of the endocrine system and there are two adrenal glands, one on top of each kidney. The outer part of each gland is the adrenal cortex; the inner part is the adrenal medulla. The adrenal glands make hormones that affect nearly every organ in your body. These hormones include adrenaline and cortisol. They do many things in the body. For example, they help control blood pressure. They help the body deal with stress. And they control the breakdown of fats and proteins in the liver.
Your doctor may took out one or both of your adrenal glands through a cut (incision) in the front, side, or back of your torso (open adrenalectomy). Or the doctor may have made one or more smaller cuts (laparoscopic adrenalectomy). The incisions will leave scars that will fade with time.
The area will feel sore after the surgery. This usually lasts about 1 to 2 weeks. Your doctor will give you pain medicine.
Your body can work fine with one healthy adrenal gland. If both adrenal glands were removed or your remaining adrenal gland isn’t healthy, you can take medicine every day to replace the hormones they were making.
The adrenal cortex makes important hormones that:
- Balance the water and salt in the body.
- Help keep blood pressure normal.
- Help control the body’s use of protein, fat, and carbohydrates.
- Cause the body to have masculine or feminine characteristics.
Sometimes, a mass in the adrenal gland is removed because it releases a hormone that can cause harmful side effects.
- One of the most common tumors is a pheochromocytoma, which can cause very high blood pressure
- Other disorders include Cushing syndrome, Conn syndrome, and an adrenal mass of unknown cause
Adrenal surgery may be done to remove a tumor that may be cancer or a growth (mass) that not be cancer. Adrenalectomy also may be done for people with Cushing’s syndrome, a problem that causes too much cortisol in the body. It may be done to remove a tumor that makes too much adrenaline.
You will receive general anesthesia that allows you to be asleep and pain free during adrenal surgery.
Adrenal gland removal can be performed in two ways. The surgery may be done through a single cut (incision). This is called open surgery. Or you may have laparoscopic surgery. The type of surgery you have depends on the problem being treated.
- With open surgery, the surgeon makes one large surgical cut (incision) to remove the gland.
- With the laparoscopic technique, several small cuts are made. Your doctor puts a lighted tube, or scope, and other tools through several small cuts.
If you have laparoscopic surgery, you may be able to leave the hospital the next day. With open surgery, you may stay in the hospital for a few days or longer.
The surgeon will discuss which approach is better for you.
After the adrenal gland is removed, it is sent to a pathologist for examination under a microscope.
Adrenocortical carcinoma is also called cancer of the adrenal cortex. A tumor of the adrenal cortex may be functioning (makes more hormones than normal) or nonfunctioning (does not make more hormones than normal). Most adrenocortical tumors are functioning. The hormones made by functioning tumors may cause certain signs or symptoms of disease.
The adrenal medulla makes hormones that help the body react to stress. Cancer that forms in the adrenal medulla is called pheochromocytoma.
Adrenocortical carcinoma and pheochromocytoma can occur in both adults and children.
Adrenalectomy risks
Risks for anesthesia and surgery in general include:
- Reaction to medicines
- Breathing problems
- Bleeding, blood clots, or infection
Risks for adrenal surgery include:
- Damage to nearby organs in the body
- Wound that breaks open or bulging tissue through the incision (incisional hernia)
- Acute adrenal crisis in which there is not enough cortisol, a hormone produced by the adrenal glands
Laparoscopic adrenalectomy
Laparoscopic adrenalectomy is a minimally invasive technique, which provides patients with less discomfort and equivalent results when compared to the larger incision required with traditional open adrenalectomy surgery. When compared to conventional open surgery, laparoscopic adrenalectomy has resulted in significantly less post-operative pain, a shorter hospital stay, earlier return to work and daily activities, a more favorable cosmetic result and outcomes identical to that of open surgery.
The laparoscopic transabdominal lateral adrenalectomy is currently the most widely used approach, since it allows an optimal comprehensive view of the adrenal lodge and surrounding structures, and provides adequate working space 1. An additional advantage of the transabdominal approach is the possibility to explore the abdominal cavity allowing the treatment of eventually associated abdominal pathologies during the same procedure. Moreover, this approach allows a quick conversion to hand-assisted or open surgery in the case of difficult dissection or intraoperative hemorrhage.
Laparoscopic adrenalectomy is performed under a general anesthetic. The typical length of the operation is 3-4 hours. The surgery is performed through 3 small (1cm) incisions made in the abdomen. A telescope and small instruments are inserted into the abdomen through these keyhole incisions, which allow the surgeon to completely free and dissect the diseased adrenal gland without having to place his hands into the abdomen. The adrenal gland is then placed within a plastic sack and removed intact through an extension of one of the existing incision sites.
Laparoscopic adrenalectomy indications
Endoscopic adrenalectomy is the gold standard treatment for small to medium-sized (≤6 cm) benign adrenal tumours, both functioning and non-functioning 2.
However, the increasing experience with the endoscopic adrenalectomy produced the broadening of the indications to this approach, proposing it also for large and potentially malignant adrenal tumors 3.
Despite tumor size is usually considered a parameter predicting the malignancy of the adrenal lesion, it remains relatively insensitive and nonspecific 4. The role of tumor size as a limiting factor for the choice of the surgical approach for adrenalectomy, seems unimportant for some surgeons 5. Conversely, other surgeons consider the tumors size as a key factor for the laparoscopic approach to adrenalectomy, assessing the adrenal lesion size threshold for endoscopic adrenalectomy between 6 and 10 cm 5. From a theoretical point of view, about 75% of adrenal tumors >6 cm will be benign at the final pathological report 6. Thus, if a tumor size >6 cm is recognized as a contraindication to laparoscopic adrenalectomy, the advantages of minimally invasive approach will be denied to patients having a most likely benign disease 5.
Moreover, the early experience on laparoscopic adrenalectomy reported that in experienced hands the endoscopic removal of large adrenal lesions (up to 10 cm in maximum diameter), in absence of suspicious radiological findings, was feasible and safe 7.
However, in the case of invasive adrenocortical carcinoma open adrenalectomy remains the procedure of choice 5.
The large diffusion of minimally invasive adrenalectomy led to an increased referral to surgery in the case of adrenal incidentaloma 8, with a consequent increased risk of unexpected pathological diagnosis of adrenocortical carcinoma after endoscopic adrenalectomy 9. The reported frequency of adrenocortical carcinoma in patients operated for adrenal incidentaloma reaches 10% in some series 10.
However, in absence of radiological suspicious findings (invasion of surrounding structures, lymph node or distant metastases, intravenous thrombus), it may difficult to predict malignancy pre-and even intra-operatively 10.
A complete surgical resection is the mainstay treatment of localized adrenocortical carcinoma [European Network for Study of Adrenal Tumors stage I–III] 11, since a R0 resection is the only means to achieve long-term disease control in adrenocortical carcinoma patients 12. Some reports reported an increased risk of R1-R2 resection or tumour spill 9, peritoneal carcinomatosis 13 and earlier recurrence 9 in patients undergoing endoscopic adrenalectomy for localized adrenocortical carcinoma. Therefore, based on these findings, an international consensus conference on adrenocortical carcinoma strongly discouraged endoscopic adrenalectomy for the treatment of known or suspicious adrenocortical carcinoma 14.
On the contrary, recently published comparative studies based on single center 15 or multi-institutional series 16 demonstrated that the oncologic outcomes of localized adrenocortical carcinoma following endoscopic adrenalectomy and open adrenalectomy could be similar. Therefore, the role of endoscopic adrenalectomy in the treatment of localized adrenocortical carcinoma is one of the most controversial and debated topics in adrenal surgery.
Due to the low incidence of adrenocortical carcinoma, there are no randomized trials comparing endoscopic and open adrenalectomy 17. Indeed, the discussion on this subject should be on the basis of the retrospective study of single center series and multi-institutional surveys.
During the last years, several papers further supported the debate. Several series from the USA persist to discourage endoscopic adrenalectomy in patients with known or suspected adrenocortical carcinoma 18, while some reports from Europe showed that endoscopic adrenalectomy does not jeopardize the oncologic outcome of selected cases of adrenocortical carcinoma 19.
Therefore, nowadays, there are not definitive conclusion regarding the oncologic outcome of endoscopic adrenalectomy vs. open adrenalectomy in patients with adrenocortical carcinoma.
However, it could be argued that in referral centers the oncologic outcome of adrenocortical carcinoma treated with endoscopic approach is not inferior to that achieved whit open adrenalectomy, when strict selection criteria and the principles of oncologic surgery are observed. On the other hand, if performed by non-experienced surgeons, endoscopic adrenalectomy for adrenocortical carcinoma can involve a higher risk of R1/R2 resection and tumour bed and/or intraperitoneal recurrence, mostly if strict selection criteria and the rule of conversion to open approach in case of challenging dissection are not followed.
However, if an endoscopic approach is considered for an adrenal tumour at increased risk of malignancy (a mass with radiological intratumoral signs of suspicion and without clear locoregional involvement), the transabdominal lateral adrenalectomy might be preferred approach because it might allow intraoperative evaluation of the presence of distant metastasis and larger en bloc resection of the tumour 17.
Laparoscopic adrenalectomy risks and complications
Although laparoscopic adrenalectomy has proven to be very safe, as in any surgical procedure there are risks and potential complications. The safety and complication rates are similar when compared to the open surgery. Potential risks include:
- Bleeding: Blood loss during this procedure is typically minor (less than 100 cc) and a blood transfusion is needed in less than 5% of patients. If you are interested in autologous blood transfusion (donating your own blood) prior to your surgery, you must make your surgeon aware. When the packet of information is mailed or given to you regarding your surgery, you will receive an authorization form for you to take to the Red Cross in your area.
- Infection: All patients are treated with intravenous antibiotics, prior to starting surgery to decrease the chance of infection from occurring after surgery. If you develop any signs or symptoms of infection after the surgery (fever, drainage from your incisions, urinary frequency/discomfort, pain or anything that you may be concerned about) please contact us at once.
- Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, spleen, liver, pancreas, kidney and gallbladder could require further surgery. Injury could occur to nerves or muscles related to positioning.
- Hernia: Hernias at incision sites rarely occur since all keyhole incisions are closed carefully at the completion of your surgery.
- Conversion to Open Surgery: The surgical procedure may require conversion to the standard open operation if difficulty is encountered during the laparoscopic procedure. This could result in a larger standard open incision and possibly a longer recuperation period.
Robotic adrenalectomy
With the increased use of robotics in the operating theater, robotic adrenalectomy has been adopted by many high-volume tertiary centers as an alternative treatment to conventional laparoscopic adrenalectomy 20. In adrenal gland surgery, minimally invasive surgery has been proven being effective, compared to open adrenalectomy. It is accepted as the standard surgical method for the majority of adrenal masses. Robotic adrenalectomy is a safe, feasible and effective method, which is positioned as an option, since it is accepted as associated with a three-dimensional perception, a tremor-free surgery, improved moving capacity of the robotic arms with multi-articulation and precise camera control, increasing the ergonomics of this type of surgery 21. These advantages are useful, especially when meticulous dissection is warranted in a deep and narrow field. Overall, robotic technology allows surgeons to carry out complex tasks in a minimally invasive manner, with an expected faster learning curve than conventional laparoscopy. In adrenal surgery, the application of robotics has not gained that much popularity among surgeons.
The benefit of robotic adrenalectomy compared to conventional laparoscopic adrenalectomy is still a matter of debate.
A controversy to be taken into consideration in minimal invasive adrenal gland surgery is whether the technique of posterior retroperitoneal approach or lateral transabdominal approach is a more appropriate method. Although the results of both techniques are similar, in 2013, the minimal surgical approach protocol of the American Society for Gastrointestinal and Endoscopic Surgery has provided recommendations regarding the surgical technique for adrenal gland pathologies for specific clinical conditions 22. These recommendations are:
- Retroperitoneal approach may result in shorter operative time and less complications in the presence of previous abdominal surgery;
- In patients undergoing bilateral adrenalectomy, the posterior retroperitoneal approach may be a more appropriate option because of the advantages of not having to re-position the patient during the operation;
- The lateral transabdominal approach in morbid obese patients (body mass index >35 kg/m²) and for large tumors (>6 cm) is more advantageous in terms of applicability compared to other surgical methods.
Although these recommendations help the surgeons in the surgical procedure, it is important to note that the most appropriate surgical technique is the surgeon’s most experienced technique. Regarding robotic surgery, Kahramangil and Berber 23 showed that both robotic approaches, retroperitoneal and transabdominal are equally safe and efficacious, based on their experience in 200 robotic adrenalectomies.
In the literature, there are many studies comparing robotic and conventional laparoscopic adrenalectomy. There have been numbers of systematic reviews and meta-analysis 24. Brunaud et al. 25 defined the learning curve for transabdominal robotic adrenalectomy as 20 cases and found that the previous clinical experience and duration of first assistance are effective factors.
Robotic adrenalectomy is performed under general anesthesia. Preoperative preparation and positioning of the patient is the same as for laparoscopic adrenalectomy. The transperitoneal approach provides greater working space, facilitates orientation by providing readily identifiable anatomical landmarks and better visualization of surrounding anatomical structures. The patient is placed in the left or right lateral decubitus position according the tumor location (left decubitus for right side adrenal tumor and right decubitus for left side tumor) and positioned in a slight Trendelenburg position. Extreme care is taken with pressure points and correctly padding them with pillows and foams. Four trocars are used for left adrenalectomy and one additional port used for right adrenalectomy to aid in liver retraction.
Currently, robotic surgery is performed with the DaVinci Si or Xi robotic surgical systems (Intuitive Surgical Sarl, Aubonne, Switzerland). These systems consist of three-arm robotic manipulator and remote-control surgical console. After positioning the patient, four or five trocars are used for the procedure. After entering the abdomen with open technique, following insufflation, one camera port (12 mm), two ports for the robotic arms (8 mm) and one port for manual assistance (12 mm) (and one additional port for right sided to aid in liver retraction) are placed. First the camera port (12 mm) is inserted above and lateral to the umbilicus, at the lateral border of the abdominal rectus muscle across from the 12th rib. After the first port insertion, the endoscope is inserted and the abdomen is carefully inspected to rule out any accidental injuries or in terms of other intra-abdominal masses.
After exploration, other ports are inserted under direct vision. To avoid clashing between the robotic arms, the ports must be placed about 8–10 cm in distance from each other. The role of the assistant on the surgical table is to change the robotic instruments when necessary, to assist in dissection through the assistant’s port, to attach the clip to the adrenal vein or to seal with the vessel sealing device and to perform the wash & aspiration process. A 30-degree endoscope is used for surgery.
Left-sided robotic adrenalectomy
Left-sided robotic transabdominal adrenalectomy is performed with the patient in the right lateral decubitus position. For the perfect gland exposure, a complete medial colonic mobilization may be needed. After dividing the lateral adhesions of the spleen and splenorenal ligaments, the spleen, colon, and the pancreas are mobilized medially until the adrenal gland is clearly visualized. During this mobilization, attention should be paid to the tail of the pancreas. Dissection continues into the periadrenal fat in order to identify the following landmarks: inferiorly the left renal vein, laterally the superior pole of the kidney, medially the tail of the pancreas and splenic vessels and posteriorly the psoas muscle. Then the adrenal vein is carefully dissected and clipped by using the robotic clip applier or standard laparoscopic clips placed by the bedside assistant. A vessel sealer also can be used. For hemostasis control, before the mass is removed from the abdomen, it is advised to wait 3–4 minutes after the intra-abdominal gas is evacuated and re-check the operation site. After the adrenalectomy is complete, the robot is undocked, and the gland is removed using a specimen retrieval bag and delivered through the auxiliary port site. After the operative site is irrigated and suctioned, trocars are removed.
Right-sided robotic adrenalectomy
Right-sided robotic transabdominal adrenalectomy is performed with the patient placed in the left lateral decubitus position. On this, different than the left side, five trocars are used (one additional port to aid in liver retraction). The triangular ligament is divided via a robotic monopolar hook and the liver retracted with a laparoscopic retractor superiorly by the assistant to provide wide exposure of the inferior vena cava. Gerota’s fascia is incised at the level of the upper pole of the kidney. After the precise dissection of the vena cava and identify the major landmarks (laterally the superior pole of the right kidney, posteriorly the psoas muscle), the right adrenal vein is identified and divided after a clip or vessel sealer has been applied by the assistant. After completion of the dissection of the adrenal space with robotic hook, bipolar forceps and/or vessel sealer, hemostasis is controlled as in left adrenalectomy, and the gland is removed using a specimen retrieval bag.
Bilateral robotic adrenalectomy
Surgery of both adrenal glands as a single operation is possible, also for minimally invasive adrenalectomy. This can be carried out either retroperitoneally or peritoneally with the robotic surgical system. Repositioning is warranted in the peritoneal approached cases that will undergo a lateral decubitus positioning. For these cases, two ports (the assistant and most medial ports) can be used in common to avoid redundant trocar insertion. Details regarding trocar positioning and surgical technique for robot-assisted laparoscopic bilateral adrenalectomy have been described by us previously 26.
Robotic adrenalectomy complications
Complications associated with robotic adrenalectomy are hemorrhage, hematoma, wound infection, urinary tract infection, adjacent organ injuries, ileus, complications due to the laparoscopic procedure and atelectasis. The complication rate between the robotic and laparoscopic groups was similar in many studies. Besides, postoperative morbidity and mortality have been shown to be comparable to conventional laparoscopy 21. A recent comprehensive meta-analysis, pooling 1,162 (747 robotic and 415 conventional laparoscopic) cases out of 27 studies, revealed that there was no significant difference between the robotic and the laparoscopic groups for intraoperative complications, postoperative complications, mortality, conversion to laparotomy and conversion to laparotomy or laparoscopy 24. Data regarding complications was also supported by another detailed recent systematic review 27. In a paper carried out by Greilsamer et al. 28, based on an experience of more than 300 robotic cases, independent risk factors for perioperative complications after robotic-assisted unilateral adrenalectomy were described as conversion to laparotomy and patient age. Tumor size >5 cm was the only predictive factor for conversion to laparotomy in that series 28.
Robotic adrenalectomy postoperative care
After surgery, the patient is kept in the intensive care unit (ICU) for a few hours. Antibiotics and prophylaxis for deep vein thrombosis are given according to hospital protocol to all patients. Pain control is performed using intravenous non-opioid and intramuscular opioid analgesics. The vital signs and fluid balances of the patients are closely monitored for the first 24 hours. Oral intake of the patients will be started on the first day of surgery with clear liquids and gradually advanced to a normal diet. All patients are mobilized at 8 hours postoperatively. The urethral catheter is generally removed on the first day and—if used—the drain is removed on the first or second day. Patients who do not develop additional complications are discharged on the 2nd or 3rd day after surgery.
Adrenalectomy recovery
Adrenalectomy is surgery to remove all or part of one or both adrenal glands. Adrenal glands are located above the kidneys. They make hormones that affect nearly every organ in the body. These hormones include adrenaline and cortisol.
While in the hospital, you may:
- Be asked to sit on the side of the bed and walk on the same day of your surgery
- Have a tube, or catheter, that comes from your bladder
- Have a drain that comes out through your surgical cut
- Not be able to eat the first 1 to 3 days, and then you will begin with liquids
- Be encouraged to do breathing exercises
- Wear special stockings to prevent blood clots
- Receive shots under your skin to prevent blood clots
- Receive pain medicine
- Have your blood pressure monitored and continue to receive blood pressure medicine
You will be discharged in 1 or 2 days after the surgery.
People who undergo the laparoscopic surgery mostly have faster recovery than with open surgery. How well you do after surgery depends on the reason for the surgery:
- If you had surgery for Conn syndrome, you may have to stay on blood pressure medicines.
- If you had surgery for Cushing syndrome, you are at risk for complications that will need to be treated. Your provider can tell you more about this.
- If you had surgery for pheochromocytoma, the outcome is usually good.
How to care for yourself at home
- Follow instructions on how to care for yourself as you recover.
- You can remove the dressing and shower the day after the surgery, unless your surgeon tells you otherwise.
- You may have some pain and may need to take medicine for pain.
- You can start doing some light activities.
Recovering from open surgery may be painful because of where the surgical cut is located. Recovery after a laparoscopic procedure is most often quicker
Incision care
- You will have a dressing over the cut (incision). A dressing helps the incision heal and protects it. Your doctor will tell you how to take care of this.
- If you have strips of tape on the incision, leave the tape on for a week or until it falls off.
- If you had stitches, your doctor will tell you when to come back to have them removed.
- Wash the area daily with warm water, and pat it dry. Don’t use hydrogen peroxide or alcohol. They can slow healing.
Activity
- Allow the area to heal. Don’t move quickly or lift anything heavy until you are feeling better.
- Rest when you feel tired.
- You can do your normal activities when it feels okay to do so.
- Be active. Walking is a good choice.
- You will probably need to take 2 to 4 weeks off from work. It depends on the type of work you do and how you feel.
- Hold a pillow over your incisions when you cough or take deep breaths. This will support your belly and may help to decrease your pain.
Diet
- You can eat your normal diet. If your stomach is upset, try bland, low-fat foods like plain rice, broiled chicken, toast, and yogurt.
- If your bowel movements are not regular right after surgery, try to avoid constipation and straining. Drink plenty of water. Your doctor may suggest fibre, a stool softener, or a mild laxative.
Medicines
- Be safe with medicines. Read and follow all instructions on the label.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, ask your doctor if you can take an over-the-counter medicine.
- If you take aspirin or some other blood thinner, be sure to talk to your doctor. He or she will tell you if and when to start taking this medicine again. Make sure that you understand exactly what your doctor wants you to do.
- Your doctor will tell you if and when you can restart your medicines. He or she will also give you instructions about taking any new medicines.
Hygiene
You may shower 24 to 48 hours after surgery, if your doctor okays it. Pat the incision dry. Do not take a bath for the first 2 weeks, or until your doctor tells you it is okay.
Call your local emergency number anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have severe trouble breathing.
- You have chest pain, are short of breath, or cough up blood.
Call your doctor now or seek immediate medical care if:
- You have pain that does not get better after you take pain medicine.
- You have loose stitches, or your incision comes open.
- You are bleeding from the incision.
- You have symptoms of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the incision.
- Pus draining from the incision.
- A fever.
Watch closely for changes in your health, and be sure to contact your doctor if:
- You do not have a bowel movement after taking a laxative.
- Raffaelli M, De Crea C, Bellantone R. Laparoscopic adrenalectomy. Gland Surg. 2019;8(Suppl 1):S41–S52. doi:10.21037/gs.2019.06.07 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6646817[↩]
- Assalia A, Gagner M. Laparoscopic adrenalectomy. Br J Surg 2004;91:1259-74. 10.1002/bjs.4738[↩]
- Lombardi CP, Raffaelli M, De Crea C, et al. Role of laparoscopy in the management of adrenal malignancies. J Surg Oncol 2006;94:128-31. 10.1002/jso.20599[↩]
- Henry JF, Sebag F, Iacobone M, et al. Results of laparoscopic adrenalectomy for large and potentially malignant tumors. World J Surg 2002;26:1043-7. 10.1007/s00268-002-6666-0[↩]
- Carnaille B. Adrenocortical carcinoma: which surgical approach? Langenbecks Arch Surg 2012;397:195-9. 10.1007/s00423-011-0852-1[↩][↩][↩][↩]
- MacGillivray DC, Whalen GF, Malchoff CD, et al. Laparoscopic resection of large adrenal tumors. Ann Surg Oncol 2002;9:480-5. 10.1007/BF02557272[↩]
- Brunt LM, Moley JF. Adrenal incidentaloma. World J Surg 2001;25:905-13. 10.1007/s00268-001-0029-0[↩]
- Miccoli P, Raffaelli M, Berti P, et al. Adrenal surgery before and after the introduction of laparoscopic adrenalectomy. Br J Surg 2002;89:779-82. 10.1046/j.1365-2168.2002.02110.x[↩]
- Miller BS, Ammori JB, Gauger PG, et al. Laparoscopic resection is inappropriate in patients with known or suspected adrenocortical carcinoma. World J Surg 2010;34:1380-5. 10.1007/s00268-010-0532-2[↩][↩][↩]
- O’Neill CJ, Spence A, Logan B, et al. Adrenal incidentalomas: risk of adrenocortical carcinoma and clinical outcomes. J Surg Oncol 2010;102:450-3. 10.1002/jso.21553[↩][↩]
- Fassnacht M, Johanssen S, Quinkler M, et al. Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: proposal for a Revised TNM Classification. Cancer 2009;115:243-50. 10.1002/cncr.24030[↩]
- Else T, Kim AC, Sabolch A, et al. Adrenocortical carcinoma. Endocr Rev 2014;35:282-326. 10.1210/er.2013-1029[↩]
- Leboulleux S, Deandreis D, Al Ghuzlan A, et al. Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur J Endocrinol 2010;162:1147-53. 10.1530/EJE-09-1096[↩]
- Schteingart DE, Doherty GM, Gauger PG, et al. Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr Relat Cancer 2005;12:667-80. 10.1677/erc.1.01029[↩]
- Porpiglia F, Fiori C, Daffara F, et al. Retrospective evaluation of the outcome of open versus laparoscopic adrenalectomy for stage I and II adrenocortical cancer. Eur Urol 2010;57:873-8. 10.1016/j.eururo.2010.01.036[↩]
- Brix D, Allolio B, Fenske W, et al. Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur Urol 2010;58:609-15. 10.1016/j.eururo.2010.06.024[↩]
- Gaujoux S, Mihai R;joint working group of ESES and ENSAT. European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg 2017;104:358-76. 10.1002/bjs.10414[↩][↩]
- Else T, Williams AR, Sabolch A, et al. Adjuvant therapies and patient and tumor characteristics associated with survival of adult patients with adrenocortical carcinoma. J Clin Endocrinol Metab 2014;99:455-61. 10.1210/jc.2013-2856[↩]
- Donatini G, Caiazzo R, Do Cao C, et al. Long-term survival after adrenalectomy for stage I/II adrenocortical carcinoma (ACC): a retrospective comparative cohort study of laparoscopic versus open approach. Ann Surg Oncol 2014;21:284-91. 10.1245/s10434-013-3164-6[↩]
- Makay O, Erol V, Ozdemir M. Robotic adrenalectomy. Gland Surg. 2019;8(Suppl 1):S10–S16. doi:10.21037/gs.2019.01.09 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6646813[↩]
- Teo XL, Lim SK. Robotic assisted adrenalectomy: Is it ready for prime time? Investig Clin Urol 2016;57:S130-46. 10.4111/icu.2016.57.S2.S130[↩][↩]
- Stefanidis D, Goldfarb M, Kercher KW, et al. SAGES Guidelines for minimally invasive treatment of adrenal pathology. Surg Endosc 2013;27:3960-80. 10.1007/s00464-013-3169-z[↩]
- Kahramangil B, Berber E. Comparison of posterior retroperitoneal and transabdominal lateral approaches in robotic adrenalectomy: an analysis of 200 cases. Surg Endosc 2018;32:1984-9. 10.1007/s00464-017-5894-1[↩]
- Economopoulos KP, Mylonas KS, Stamou AA, et al. Laparoscopic versus robotic adrenalectomy: A comprehensive meta-analysis. Int J Surg 2017;38:95-104. 10.1016/j.ijsu.2016.12.118[↩][↩]
- Brunaud L, Ayav A, Zarnegar R, et al. Prospective evaluation of 100 robotic-assisted unilateral adrenalectomies. Surgery 2008;144:995-1001. 10.1016/j.surg.2008.08.032[↩]
- Makay Ö, Uǧuz A, Uǧuz I, et al. Robot-assisted laparoscopic bilateral adrenalectomy: A case report. Turk J Surg 2012;28:225-8. 10.5152/UCD.2012.26[↩]
- Heger P, Probst P, Hüttner FJ, et al. Evaluation of open and minimally invasive adrenalectomy: a systematic review and network meta-analysis. World J Surg 2017;41:2746-57. 10.1007/s00268-017-4095-3[↩]
- Greilsamer T, Nomine-Criqui C, Thy M, et al. Robotic-assisted unilateral adrenalectomy: risk factors for perioperative complications in 303 consecutive patients. Surg Endosc 2019;33:802-10. 10.1007/s00464-018-6346-2[↩][↩]