Alcoholism
Alcoholism is also known as alcohol dependence, alcohol addiction, severe alcohol use disorder, severe alcohol abuse or severe alcohol dependence syndrome, is a chronic, relapsing brain disease where a person has lost control of their alcohol use, and they continue to drink despite adverse social, occupational, or health consequences 1, 2. Alcoholism is a chronic disease. That means that it lasts for a long time, or it causes problems again and again. The main treatment for alcoholism is to stop drinking alcohol, which can be difficult. This is because when you use alcohol, parts of your brain make you feel pleasure and intoxication. Most people who are alcoholics still feel a strong desire for alcohol even after they stop drinking.
Alcoholism or ‘alcohol dependence’ is characterized by craving, tolerance, a preoccupation with alcohol and continued drinking in spite of harmful consequences (e.g, liver disease or depression caused by drinking). The International Classification of Diseases volume 10 (ICD-10) defines dependency as: “a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and that typically include a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal state”.
Alcoholism or alcohol dependence, is a disease that causes:
- Craving – a strong need to drink
- Loss of control – not being able to stop drinking once you’ve started
- Physical dependence – withdrawal symptoms
- Tolerance – the need to drink more alcohol to feel the same effect
- Adverse social, occupational or health consequences – the alcohol you are drinking affects your life, your relationships or the lives of others. Alcohol dependence is also associated with increased criminal activity and domestic violence, and an increased rate of significant mental and physical disorders
Griffith Edwards and Gross 3 defined some simple markers of alcoholism. These markers are:
- dependent drinkers have a narrow repertoire of alcohol consumption: alcohol is used to avoid withdrawal symptoms
- drinking overtakes the individual’s activities to the exclusion of everything else, leading to theft, begging and borrowing
- withdrawal symptoms include trembling, fear, insomnia, nightmares, sweating and hallucinations.
- tolerance develops so that the dependent drinker consumes quantities which might make non-drinkers unconscious
- dependent drinkers know that they cannot control their alcohol use
- there is a high tendency to relapse after abstinence
- alcohol withdrawal symptoms occur within 12 hours of the last drink.
The American Psychiatric Association has outlined the criteria used by doctors to diagnose substance use disorders such as alcoholism 4. To receive an alcohol use disorder diagnosis, a person must meet at least 2 of the following criteria within a 12-month period; however, only a qualified mental health professional or a physician can diagnose alcohol use disorder 4:
- Drinking more than you originally intended.
- Being unable to cut down alcohol use even if you want to.
- Spending a lot of time obtaining, using, and recovering from the effects of alcohol.
- Strong desires or cravings to drink alcohol.
- Failing to fulfill obligations at work, home, or school due to alcohol use.
- Continuing to drink despite developing interpersonal/social problems that are the consequence of your alcohol use.
- Giving up activities you once enjoyed because of alcohol use.
- Drinking in situations where it is physically dangerous to do so (like driving or operating machinery).
- Continuing to drink despite a persistent or recurring physical or mental health condition that is likely worsened or caused by your alcohol use.
- Tolerance, meaning you need to drink more to achieve previous effects.
- Withdrawal symptoms (like tremors, sweating, insomnia, or anxiety) when you stop drinking or significantly reduce your drinking (i.e., alcohol dependence).
You may have a drinking problem if you have at least 2 of the following characteristics:
- There are times when you drink more or longer than you planned to.
- You have not been able to cut down or stop drinking on your own, even though you have tried or you want to.
- You spend a lot of time drinking, being sick from drinking, or getting over the effects of drinking.
- Your urge to drink is so strong, you cannot think about anything else.
- As a result of drinking, you do not do what you are expected to do at home, work, or school. Or, you keep getting sick because of drinking.
- You continue to drink, even though alcohol is causing problems with your family or friends.
- You spend less time on or no longer take part in activities that used to be important or that you enjoyed. Instead, you use that time to drink.
- Your drinking has led to situations that you or someone else could have been injured, such as driving while drunk or having unsafe sex.
- Your drinking makes you anxious, depressed, forgetful, or causes other health problems, but you keep drinking.
- You need to drink more than you did to get the same effect from alcohol. Or, the number of drinks you are used to having now have less effect than before.
- When the effects of alcohol wear off, you have symptoms of withdrawal. These include, tremors, sweating, nausea, or insomnia. You may even have had a seizure or hallucinations (sensing things that are not there).
Alcohol use disorder is diagnosed when a person answers “yes” to two or more of the questions below.
In the past year, have you:
- Ended up drinking more or for a longer time than you had planned to?
- Wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of your time drinking, or recovering from drinking?
- Needed a drink first thing in the morning to steady your nerves or get rid of a hangover?
- Felt a strong need to drink?
- Felt annoyed by criticism of your drinking?
- Had guilty feelings about drinking?
- Found that drinking – or being sick from drinking – often interfered with your family life, job, or school?
- Kept drinking even though it was causing trouble with your family or friends?
- Given up or cut back on activities that you enjoyed just so you could drink?
- Gotten into dangerous situations while drinking or after drinking? Some examples are driving drunk and having unsafe sex.
- Kept drinking even though it was making you feel depressed or anxious? Or when it was adding to another health problem?
- Had to drink more and more to feel the effects of the alcohol?
- Had withdrawal symptoms when the alcohol was wearing off? They include trouble sleeping, shakiness, irritability, anxiety, depression, restlessness, nausea, and sweating. In severe cases, you could have a fever, seizures, or hallucinations.
If you have any of these symptoms, your drinking may already be a cause for concern. The more symptoms you have, the more urgent the need for change. A health professional can conduct a formal assessment of your symptoms to see if alcohol use disorder is present.
Like many other diseases, alcoholism affects you physically and mentally. Both your body and your mind have to be treated. In addition to medicine, your doctor may recommend psychosocial treatments. These treatments can help you change your behavior and cope with your problems without using alcohol. Examples of psychosocial treatments include:
- Alcoholics Anonymous or other support group meetings
- Counseling
- Family therapy
- Group therapy
- Addiction treatment program
- Hospital treatment
There may be special centers in your area that offer this kind of treatment. Your doctor can refer you to the psychosocial treatment that is right for you.
Recovering people who attend support groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous (https://www.aa.org)
- Moderation Management (https://moderation.org)
- Secular Organizations for Sobriety (https://www.sossobriety.org)
- SMART Recovery (https://www.smartrecovery.org)
- Women for Sobriety (https://womenforsobriety.org)
- Al-Anon Family Groups (https://al-anon.org)
- Adult Children of Alcoholics (https://adultchildren.org)
- National Council on Alcoholism and Drug Dependence (https://recovered.org)
- National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov)
- National Organization on Fetal Alcohol Syndrome (https://fasdunited.org)
- Substance Abuse and Mental Health Services Administration (https://findtreatment.gov)
If you feel that you sometimes drink too much alcohol, or your drinking is causing problems, or your family is concerned about your drinking, talk with your doctor. Other ways to get help include talking with a mental health professional or seeking help from a support group such as Alcoholics Anonymous or a similar type of self-help group.
Because denial is common, you may not feel like you have a problem with drinking. You might not recognize how much you drink or how many problems in your life are related to alcohol use. Listen to relatives, friends or co-workers when they ask you to examine your drinking habits or to seek help. Consider talking with someone who has had a problem drinking, but has stopped.
If your loved one needs help
Many people with alcohol use disorder hesitate to get treatment because they don’t recognize they have a problem. An intervention from loved ones can help some people recognize and accept that they need professional help. If you’re concerned about someone who drinks too much, ask a professional experienced in alcohol treatment for advice on how to approach that person.
Types of alcohol
Alcohol in the form of ethanol (ethyl alcohol) is found in alcoholic beverages, mouthwash, cooking extracts, some medications and certain household products. Other forms of alcohol — including isopropyl alcohol (found in rubbing alcohol, lotions and some cleaning products) and methanol or ethylene glycol (a common ingredient in antifreeze, paints and solvents) — can cause other types of toxic poisoning that require emergency treatment. Ethanol (alcohol) is a central nervous system depressant that produces euphoria and behavioral excitation at low blood concentrations and acute intoxication (drowsiness, ataxia, slurred speech, stupor, and coma) at higher concentrations. The short-term effects of alcohol result from its actions on ligand-gated and voltage-gated ion channels 5. Prolonged alcohol consumption leads to the development of tolerance and physical dependence, which may result from compensatory functional changes in the same ion channels. Abrupt cessation of prolonged alcohol consumption unmasks these changes, leading to the alcohol withdrawal syndrome, which includes blackouts, tremors, muscular rigidity, delirium tremens, and seizures 6. Alcohol withdrawal seizures typically occur 6 to 48 hours after discontinuation of alcohol consumption and are usually generalized tonic–clonic seizures, although partial seizures also occur 7.
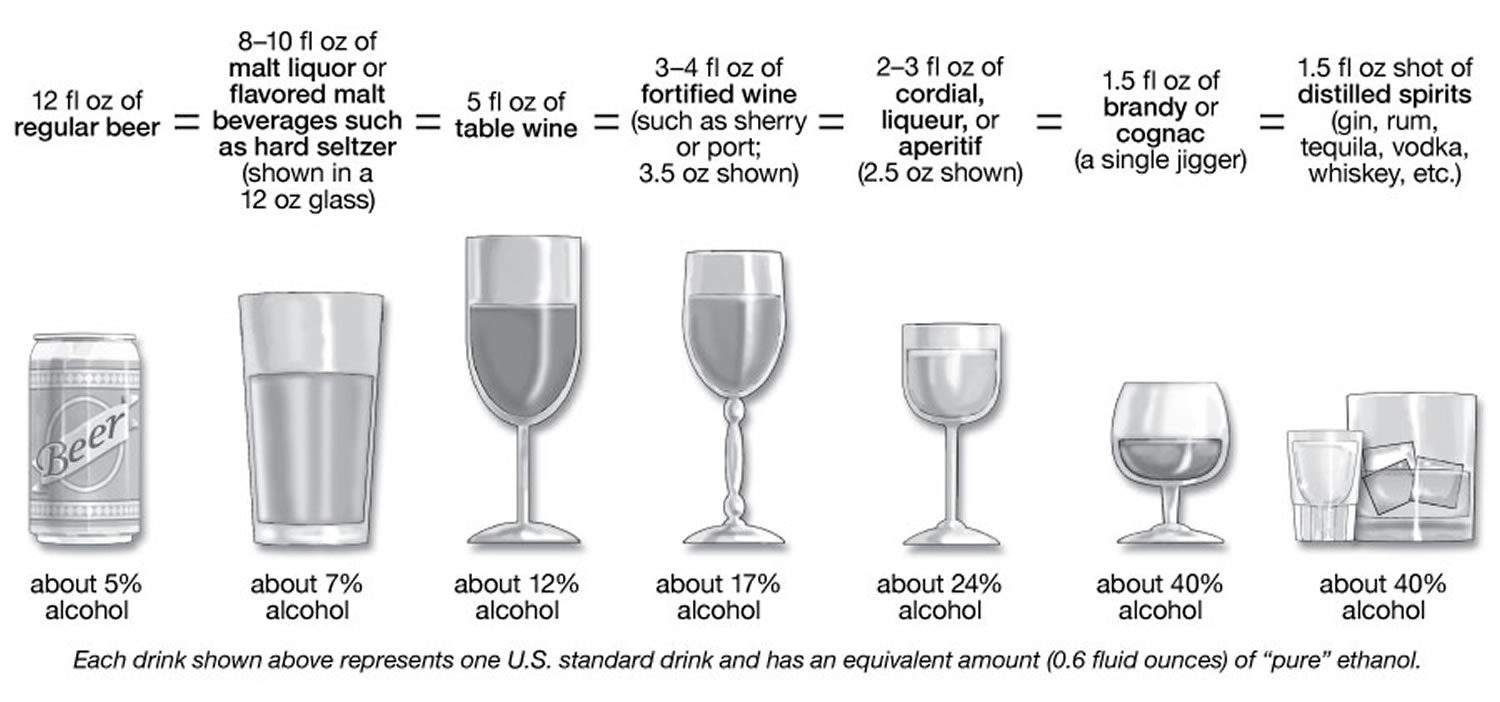
In the United States, a “standard drink” or “alcoholic drink equivalent” is any drink containing 14 grams, or about 0.6 fluid ounces, of “pure” ethanol. One alcoholic drink equals one 12-ounce (oz), or 355 milliliters (mL), can or bottle of beer (with 5% alcohol by volume or alc/vol), a 5-ounce (148 mL) glass of wine (with 12% alc/vol), 1 wine cooler, 1 cocktail, 1 shot of hard liquor; or 1.5 ounces of 80-proof distilled spirits (such as whiskey, rum, or tequila) (with 40% alc/vol) 8. While there is no guaranteed safe amount of alcohol for anyone, the answer from current research is, the less alcohol, the better 9, 10. Alcohol is a carcinogen associated with cancer of the oral cavity, pharynx, larynx, esophagus, colon, rectum, liver, and female breast, with breast cancer risk rising with less than one drink a day. Your whole body is impacted by alcohol use not just your liver, but also your brain, gut, pancreas, lungs, cardiovascular system, immune system, and more and may explain, for example, challenges in managing hypertension, atrial fibrillation, diabetes, and recurrent lung infections.
Alcohol contributes to more than 200 health conditions including liver cirrhosis, cancers, and injuries and causes more than 3 million deaths each year globally (5.3% of all deaths worldwide) 11, 12. In the U.S., about 99,000 people die every year from alcohol-related causes 13, making alcohol one of the leading causes of preventable death 14, 15. More than half of the deaths result from chronic heavy alcohol consumption while the remainder result from acute injuries sustained while intoxicated 16.
The health risks of alcohol tend to be dose-dependent, and the likelihood of certain harms, such as cancer, begin at relatively low amounts 17. Even drinking within the U.S. Dietary Guidelines (see drinking level terms below), for example, increases the risk of breast cancer 18, 19. Additionally, earlier research suggested cardiovascular benefits, but newer, more rigorous studies are finding little or no protective effect of alcohol on cardiovascular or other outcomes 20, 21, 22, 23. In short, current research indicates there is no safe drinking level,11 underscoring the message to patients that “the less, the better” when it comes to alcohol.
The 2020-2025 U.S. Dietary Guidelines states that for adults who choose to drink alcohol, women should have 1 drink or less in a day and men should have 2 drinks or less in a day 24. These amounts are not intended as an average but rather a daily limit.
You are abusing alcohol when:
- You drink 7 drinks per week or more than 3 drinks per occasion (for women).
- You drink more than 14 drinks per week or more than 4 drinks per occasion (for men).
- You have more than 7 drinks per week or more than 3 drinks per occasion (for men and women older than 65).
- Consuming these amounts of alcohol harms your health, relationships, work, and/or causes legal problems.
Figure 1. Standard drink
Footnotes: The sample standard drinks above are just starting points for comparison, because actual alcohol content and customary serving sizes can vary greatly both across and within types of beverages. For example:
- Beer: The most popular type of beer is light beer, which may be light in calories, but not necessarily in alcohol. The mean alc/vol for light beers is 4.3%, almost as much as a regular beer with 5% alc/vol.4 On average, craft beers have more than 5% alc/vol and flavored malt beverages, such as hard seltzers, more than 6% alc/vol.4 Some craft beers and flavored malt beverages have in the range of 8-9% alc/vol. Advise patients to check container labels for the alcohol content and adjust their intake accordingly.
- Wine: The largest category of wine is table wine. On average, table wines contain about 12% alc/vol4 and can range from about 5% to 16%. Larger wine glasses can encourage larger pours. People are often unaware that a 25-ounce (750ml) bottle of table wine with 12% alc/vol contains five standard drinks, and one with 14% alc/vol holds nearly six.
- Cocktails: Recipes for cocktails often exceed one standard drink’s worth of alcohol. The cocktail content calculator on Rethinking Drinking shows the alcohol content in sample cocktails.
What is considered 1 drink?
The National Institute on Alcohol Abuse and Alcoholism defines one standard drink as any one of these:
- 12 ounces (355 milliliters) of regular beer (about 5 percent alcohol)
- 8 to 9 ounces (237 to 266 milliliters) of malt liquor (about 7 percent alcohol)
- 5 ounces (148 milliliters) of unfortified wine (about 12 percent alcohol)
- 1.5 ounces (44 milliliters) of 80-proof hard liquor (about 40 percent alcohol)
Levels of alcohol use
There are four levels of alcohol use:
- Social drinking: There is no guaranteed safe amount of alcohol for anyone. According to the “Dietary Guidelines for Americans 2020-2025” 24, adults of legal drinking age can choose not to drink or to drink in moderation by limiting intake to 2 drinks or less in a day for men (less than 14 drinks per week for men) and 1 drink or less in a day for women (less than 7 drinks per week for women), when alcohol is consumed. Drinking less is better for health than drinking more.
- At risk consumption: the level of drinking begins to pose a health risk. Frequent heavy drinking raises the risk for both acute harms, such as falls and medication interactions, and for chronic consequences, such as alcohol use disorder and dose-dependent increases in liver disease, heart disease and cancers 25, 26, 27.
- For men, consuming more than 5 drinks on any day or more than 15 drinks per week
- For women, consuming more than 4 drinks on any day or more than 8 drinks per week
- Binge drinking on 5 or more days in the past month
- Heavy drinking thresholds for women are lower than men because after consumption, alcohol distributes itself evenly in body water, and pound for pound, women have proportionally less water in their bodies than men do. This means that after a woman and a man of the same weight drink the same amount of alcohol, the woman’s blood alcohol concentration (BAC) will tend to be higher, putting her at greater risk for harm.
- Problem drinking: drinking causes serious problems to you, your family, your work and society in general
- Alcohol dependence and addiction:
- periodic or chronic intoxication
- uncontrollable craving for drink when sober
- tolerance to the effects of alcohol
- psychological and/or physical dependence
What is binge drinking?
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines binge drinking is drinking so much at once that your blood alcohol concentration (BAC) level is 0.08% (0.08 grams of alcohol per deciliter of blood) or more. For a man, this usually happens after having 5 or more drinks within about 2 hours. For a woman, it is after about 4 or more drinks within about 2 hours 28. Not everyone who binge drinks has an alcohol use disorder, but they are at higher risk for getting one.
The Substance Abuse and Mental Health Services Administration (SAMHSA), which conducts the annual National Survey on Drug Use and Health, defines binge drinking as 5 or more alcoholic drinks for males or 4 or more alcoholic drinks for females on the same occasion (i.e., at the same time or within a couple of hours of each other) on at least 1 day in the past month.
Binge drinking occurs in the majority of adolescents who drink 29, in half of adults who drink 29 and in 1 in 10 adults over age 65 30 and is increasing among women 31, 32.
Binge drinking causes more than half of the alcohol-related deaths in the U.S. 29. Binge drinking increases the risk of falls, burns, car crashes, memory blackouts, medication interactions, assaults, drownings, and overdose deaths 29.
What is alcohol poisoning?
Alcohol (ethanol) poisoning also known as alcohol overdose is generally caused by binge drinking at high intensity or from drinking too many alcoholic beverages, especially in a short period of time. Such drinking can exceed the body’s physiologic capacity to process alcohol, causing the blood alcohol concentration to rise. Alcohol exerts its effects by several mechanisms. Alcohol binds directly to gamma-aminobutyric acid (GABA) receptors in the brain, causing sedation. Alcohol also directly affects cardiac, hepatic, and thyroid tissue. Very high levels of alcohol in the body can shutdown critical areas of the brain that control breathing, heart rate, and body temperature, resulting in death. Alcohol poisoning deaths affect people of all ages but are most common among middle-aged adults and men. The clinical signs and symptoms of an overdose of alcohol occurs when a person has a blood alcohol content sufficient to produce impairments that increase the risk of harm.
- Rapid binge drinking (which often happens on a bet or a dare) is especially dangerous because the victim can drink a fatal dose before losing consciousness.
Alcohol overdoses can range in severity, from minimal impairment with balance, decreased judgment and control, slurred speech, reduced muscle coordination, vomiting, and stupor (reduced level of consciousness and cognitive function) to coma and death 33. However, an individual’s response to alcohol is variable depending on many factors, including the amount and rate of alcohol consumption, health status, consumption of other drugs, age, gender, the amount of food eaten, even ethnicity and metabolic and functional tolerance of the drinker 34, 35.
A major cause of alcohol poisoning is binge drinking — a pattern of heavy drinking when a male rapidly consumes five or more alcoholic drinks within two hours, or a female downs at least four drinks within two hours. An alcohol binge can occur over hours or last up to several days.
You can consume a fatal dose before you pass out. Even when you’re unconscious or you’ve stopped drinking, alcohol continues to be released from your stomach and intestines into your bloodstream, and the level of alcohol in your body continues to rise.
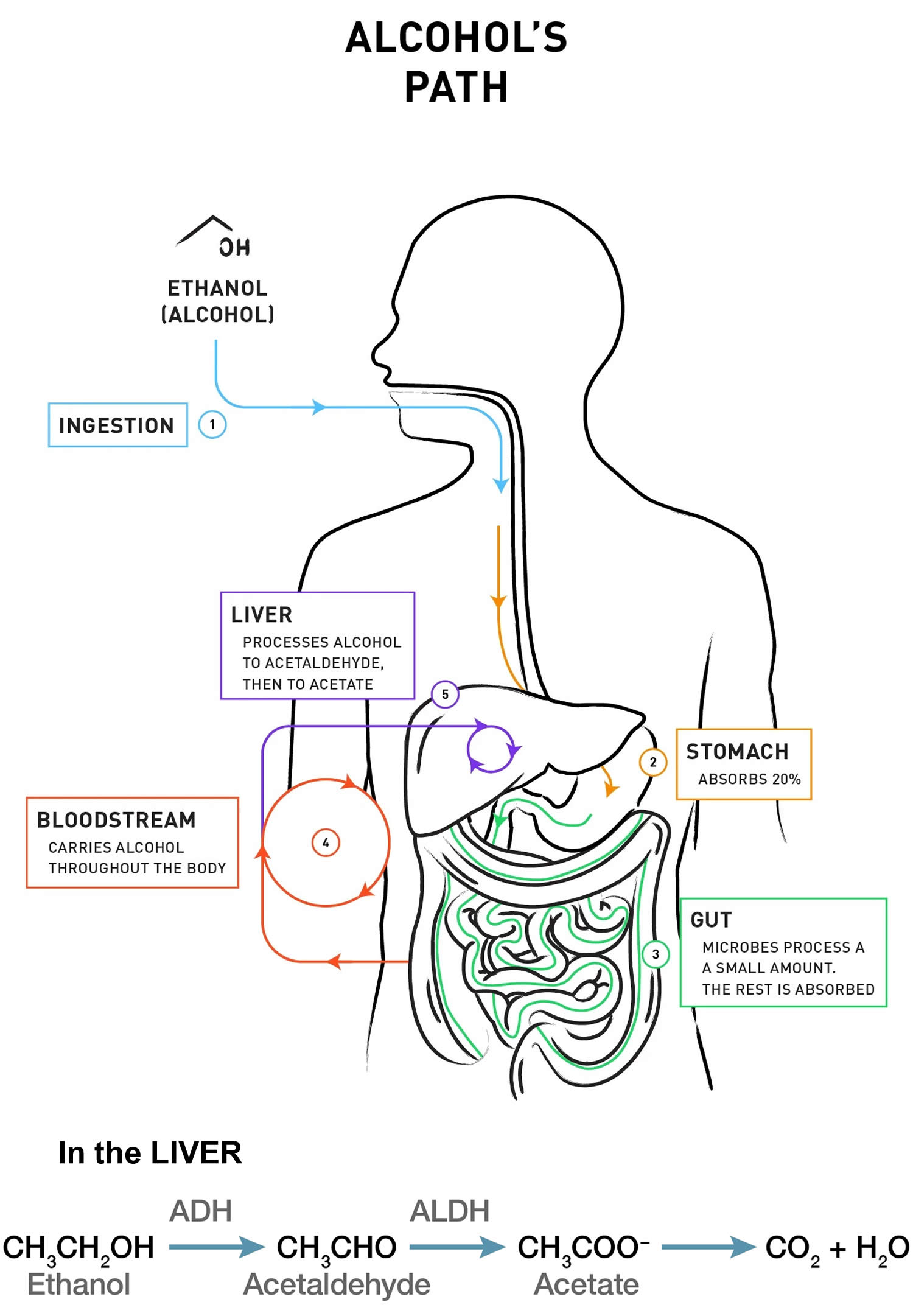
Alcohol is absorbed into the blood mainly from the small bowel, although some is absorbed from the stomach. Alcohol accumulates in blood because absorption is more rapid than oxidation and elimination. The concentration peaks about 30 to 90 min after ingestion if the stomach was previously empty 36.
About 5 to 10% of ingested alcohol is excreted unchanged in urine, sweat, and expired air; the remainder is metabolized mainly by the liver, where alcohol dehydrogenase converts ethanol to acetaldehyde. Acetaldehyde is ultimately oxidized to CO2 and water at a rate of 5 to 10 mL/hour (of absolute alcohol); each milliliter yields about 7 kcal. Alcohol dehydrogenase in the gastric mucosa accounts for some metabolism; much less gastric metabolism occurs in women.
In alcohol-naive people, a blood alcohol level of 300 to 400 mg/dL (BAC 0.3 to 0.4 percent) often causes unconsciousness, and a BAC ≥ 400 mg/dL may be fatal. Sudden death due to respiratory depression or arrhythmias may occur, especially when large quantities are drunk rapidly. This problem is emerging in US colleges but has been known in other countries where it is more common. Other common effects include hypotension and hypoglycemia.
The effect of a particular BAC varies widely; some chronic drinkers seem unaffected and appear to function normally with a BAC in the 300 to 400 mg/dL range, whereas nondrinkers and social drinkers are impaired at a BAC that is inconsequential in chronic drinkers.
- If you suspect someone has alcohol poisoning, get medical help immediately. If you or someone you are with has an exposure, call your local emergency number (such as 911) immediately. Cold showers, hot coffee, or walking will not reverse the effects of alcohol overdose and could actually make things worse.
- When in doubt, call for medical help.
- If you are having difficulty in determining whether an individual is acutely intoxicated, contact a health professional immediately – you cannot afford to guess.
- Hundreds of people die each year from acute alcohol intoxication, more commonly known as alcohol poisoning or alcohol overdose. Caused by drinking too much alcohol too fast, it often occurs on college campuses or wherever heavy drinking takes place.
- At the hospital, medical staff will manage any breathing problems, administer fluids to combat dehydration and low blood sugar, and flush the drinker’s stomach to help clear the body of toxins.
- The best way to avoid an alcohol overdose is to drink responsibly if you choose to drink.
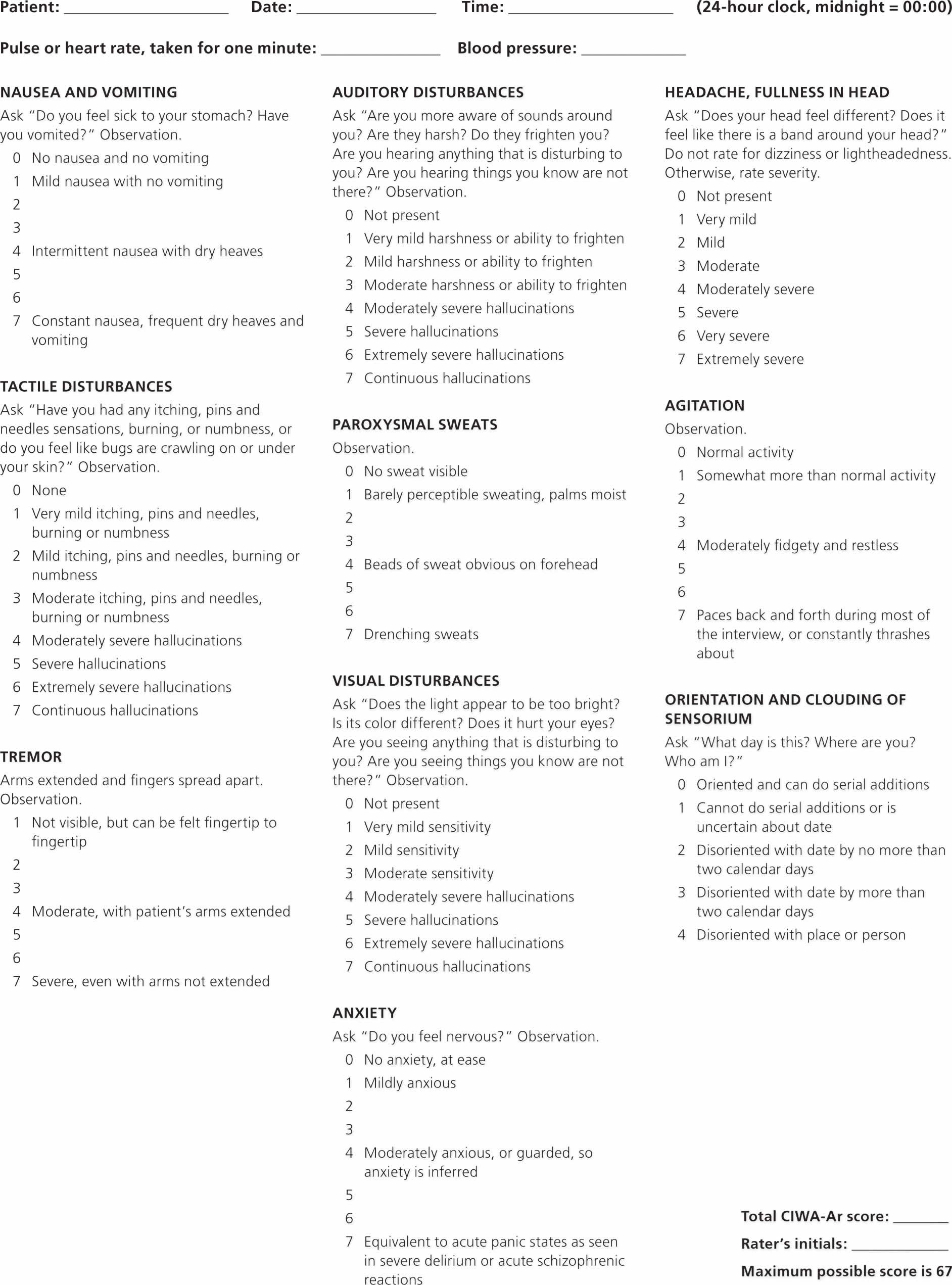
Figure 2. Alcohol Poisoning Scale
[Source 37 ]How does my body process alcohol?
When alcohol is consumed, it passes from your stomach and intestines into your bloodstream, where it distributes itself evenly throughout all the water in your body’s tissues and fluids. Drinking alcohol on an empty stomach increases the rate of absorption, resulting in higher blood alcohol level, compared to drinking on a full stomach. In either case, however, alcohol is still absorbed into the bloodstream at a much faster rate than it is metabolized. Thus, your blood alcohol concentration (BAC) builds when you have additional drinks before prior drinks are metabolized.
Your blood alcohol concentration (BAC) is largely determined by how much and how quickly you drink alcohol as well as by your body’s rates of alcohol absorption, distribution, and metabolism. Binge drinking is defined as reaching a BAC of 0.08% (0.08 grams of alcohol per deciliter of blood) or higher. A typical adult reaches this BAC after consuming 4 or more drinks (women) or 5 or more drinks (men), in about 2 hours.
Your body begins to metabolize alcohol within seconds after ingestion and proceeds at a steady rate, regardless of how much alcohol a person drinks or of attempts to sober up with caffeine or by other means. Most of the alcohol is broken down in your liver by the enzyme alcohol dehydrogenase (ADH). Alcohol dehydrogenase (ADH) transforms ethanol, the type of alcohol in alcohol beverages, into acetaldehyde, a toxic, carcinogenic compound. Generally, acetaldehyde is quickly broken down to a less toxic compound, acetate, by acetaldehyde dehydrogenase (ALDH) (also called aldehyde dehydrogenase). Acetate then is broken down, mainly in tissues other than the liver, into carbon dioxide (CO2) and water (H2O), which are easily eliminated. To a lesser degree, other enzymes (CYP2E1 and catalase) also break down alcohol to acetaldehyde 38.
Although the rate of metabolism is steady in any given person, it varies widely among individuals depending on factors including liver size and body mass, as well as genetics. There are multiple ADH and ALDH enzymes that are encoded by different genes 38. These genetic variants have been shown to influence a person’s drinking levels and, consequently, the risk of developing alcohol abuse or dependence 39. Studies have shown that people carrying certain ADH and ALDH alleles (one of two or more variants of a gene) are at significantly reduced risk of becoming alcohol dependent. In fact, these associations are the strongest and most widely reproduced associations of any gene with the risk of alcoholism. Some people of Asian descent, for example, carry variations of the genes for alcohol dehydrogenase (ADH) or acetaldehyde dehydrogenase (ALDH) that cause acetaldehyde (a toxic carcinogenic compound) to build up when alcohol is consumed, which in turn produces a flushing reaction and increases the risk of cancer risk 40, 41, 42. 20% of Chinese and Japanese cannot drink alcohol because of an inherited deficiency of acetaldehyde dehydrogenase 43.
Figure 3. How the body processes alcohol
Do you have a drinking problem?
While there is no guaranteed safe amount of alcohol for anyone, the answer from current research is, the less alcohol, the better 9, 10. The 2020-2025 U.S. Dietary Guidelines states that for adults who choose to drink alcohol, women should have 1 drink or less in a day and men should have 2 drinks or less in a day 24. These amounts are not intended as an average but rather a daily limit. Many people with alcohol problems cannot tell when their drinking is out of control. It is important to be aware of how much you are drinking. You should also know how your alcohol use may affect your life and those around you.
Many patients may think that heavy drinking is not a concern because they can “hold their liquor.” However, having an innate “low level of response” or “high tolerance” to alcohol is a reason for caution, as people with this trait tend to drink more and thus have an increased risk for alcohol-related problems including alcohol use disorder 44. People who drink within the U.S. Dietary Guidelines, too, may be unaware that even if they don’t feel a “buzz,” driving can be impaired 45.
Doctors consider your drinking medically unsafe when you drink:
- Many times a month, or even many times a week
- 3 to 4 drinks (or more) in 1 day
- 5 or more drinks on one occasion monthly, or even weekly
Twelve questions to ask if you think you may have a drinking problem
- Have you ever decided to stop drinking for a week or so, but only lasted for a couple of days? (Yes or No)
- Do you wish people would mind their own business about your drinking– stop telling you what to do? (Yes or No)
- Have you ever switched from one kind of drink to another in the hope that this would keep you from getting drunk? (Yes or No)
- Have you had to have a drink upon awakening during the past year? (Yes or No)
- Do you envy people who can drink without getting into trouble? (Yes or No)
- Have you had problems connected with drinking during the past year? (Yes or No)
- Has your drinking caused trouble at home? (Yes or No)
- Do you ever try to get “extra” drinks at a party because you do not get enough? (Yes or No)
- Do you tell yourself you can stop drinking any time you want to, even though you keep getting drunk when you don’t mean to? (Yes or No)
- Have you missed days of work or school because of drinking? (Yes or No)
- Do you have “blackouts”? (Yes or No) (Alcohol-related blackouts are gaps in a person’s memory for events that occurred while they were intoxicated. These gaps happen when a person drinks enough alcohol to temporarily block the transfer of memories from short-term to long-term storage, known as memory consolidation, in a brain area called the hippocampus.)
- Have you ever felt that your life would be better if you did not drink? (Yes or No)
If you answer YES 4 or more times – you are probably in trouble with alcohol.
However severe your drinking problem may seem, most people with alcohol use disorder can benefit from treatment. Unfortunately, less than 10 percent of them receive any treatment.
Ultimately, receiving treatment can improve your chances of success in overcoming alcohol use disorder.
Talk with your doctor to determine the best course of action for you.
What are the dangers of too much alcohol?
Too much alcohol is dangerous. Heavy drinking can increase the risk of certain cancers. It may lead to liver diseases, such as fatty liver disease and cirrhosis. It can also cause damage to the brain and other organs. Drinking during pregnancy can harm your baby. Alcohol also increases the risk of death from car crashes, injuries, homicide, and suicide.
How to stop drinking alcohol
There are many ways to help yourself stop drinking. You do not have to drink when other people drink. If someone gives you a drink, it is OK to say no. Stay away from people or places that make you drink. Do not keep alcohol at home.
Handling your urges to drink
Plan ahead to stay in control
As you change your drinking, it’s normal and common to have urges or a craving for alcohol. The words “urge” and “craving” refer to a broad range of thoughts, physical sensations, or emotions that tempt you to drink, even though you have at least some desire not to. You may feel an uncomfortable pull in two directions or sense a loss of control 46.
Fortunately, urges to drink are short-lived, predictable, and controllable. This short strategy offers a recognize-avoid-cope approach commonly used in cognitive behavioral therapy, which helps people to change unhelpful thinking patterns and reactions. It also provides worksheets to help you uncover the nature of your urges to drink and to make a plan for handling them.
With time, and by practicing new responses, you’ll find that your urges to drink will lose strength, and you’ll gain confidence in your ability to deal with urges that may still arise at times. If you are having a very difficult time with urges, or do not make progress with the strategies in this module after a few weeks, then consult a doctor or therapist for support. In addition, some new, non-habit forming medications can reduce the desire to drink or lessen the rewarding effect of drinking so it is easier to stop.
Recognize two types of “triggers”
An urge to drink can be set off by external triggers in the environment and internal ones within yourself.
- External triggers are people, places, things, or times of day that offer drinking opportunities or remind you of drinking. These “high-risk situations” are more obvious, predictable, and avoidable than internal triggers.
- Internal triggers can be puzzling because the urge to drink just seems to “pop up.” But if you pause to think about it when it happens, you’ll find that the urge may have been set off by a fleeting thought, a positive emotion such as excitement, a negative emotion such as frustration, or a physical sensation such as a headache, tension, or nervousness.
Consider tracking and analyzing your urges to drink for a couple of weeks. This will help you become more aware of when and how you experience urges, what triggers them, and ways to avoid or control them. A sample “urge to drink” tracking form is provided below.
Urge To Drink Tracker Form – Record the details as soon after an urge as possible.
| Date/time | Situation (people, place) or trigger (incident, feelings) | What was the urge like? | How I responded | What I’ll do next time | |
|---|---|---|---|---|---|
| Was it a thought? Emotion? Physical sensation? | Rate it from 1 (mild) to 10 (strong) | ||||
Footnote: You can Print a copy of this form and carry it with you from here: https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink-urge-tracker.aspx
[Source: U.S. Department of Health and Human Services. Rethinking Drinking 47]Avoid high-risk situations
In many cases, your best strategy will be to avoid taking the chance that you’ll have an urge, then slip and drink. At home, keep little or no alcohol. Socially, avoid activities involving drinking. If you feel guilty about turning down an invitation, remind yourself that you are not necessarily talking about “forever.” When the urges subside or become more manageable, you may decide to ease gradually into some situations you now choose to avoid. In the meantime, you can stay connected with friends by suggesting alternate activities that don’t involve drinking.
Building your drink refusal skills
- Plan ahead to stay in control
Even if you are committed to changing your drinking, “social pressure” to drink from friends or others can make it hard to cut back or quit. This short module offers a recognize-avoid-cope approach commonly used in cognitive-behavioral therapy, which helps people to change unhelpful thinking patterns and reactions. It also provides links to worksheets to help you get started with your own plan to resist pressure to drink.
Recognize two types of pressure
The first step is to become aware of the two different types of social pressure to drink alcohol—direct and indirect.
- Direct social pressure is when someone offers you a drink or an opportunity to drink.
- Indirect social pressure is when you feel tempted to drink just by being around others who are drinking—even if no one offers you a drink.
Take a moment to think about situations where you feel direct or indirect pressure to drink or to drink too much. You can use the form below to write them down. Then, for each situation, choose some resistance strategies from below,or come up with your own. When you’re done, you can print the form or email it to yourself.
- Avoid pressure when possible
For some situations, your best strategy may be avoiding them altogether. If you feel guilty about avoiding an event or turning down an invitation, remind yourself that you are not necessarily talking about “forever.” When you have confidence in your resistance skills, you may decide to ease gradually into situations you now choose to avoid. In the meantime, you can stay connected with friends by suggesting alternate activities that don’t involve drinking.
Cope with situations you can’t avoid
- Know your “NO”
When you know alcohol will be served, it’s important to have some resistance strategies lined up in advance. If you expect to be offered a drink, you’ll need to be ready to deliver a convincing “no thanks.” Your goal is to be clear and firm, yet friendly and respectful. Avoid long explanations and vague excuses, as they tend to prolong the discussion and provide more of an opportunity to give in. Here are some other points to keep in mind:
- Don’t hesitate, as that will give you the chance to think of reasons to go along
- Look directly at the person and make eye contact
- Keep your response short, clear, and simple
The person offering you a drink may not know you are trying to cut down or stop, and his or her level of insistence may vary. It’s a good idea to plan a series of responses in case the person persists, from a simple refusal to a more assertive reply. Consider a sequence like this:
- No, thank you.
- No, thanks, I don’t want to.
- You know, I’m (cutting back/not drinking) now (to get healthier/to take care of myself/because my doctor said to). I’d really appreciate it if you’d help me out.
You can also try the “broken record” strategy. Each time the person makes a statement, you can simply repeat the same short, clear response. You might want to acknowledge some part of the person’s points (“I hear you…”) and then go back to your broken-record reply (“…but no thanks”). And if words fail, you can walk away.
- Script and practice your “NO”
Many people are surprised at how hard it can be to say no the first few times. You can build confidence by scripting and practicing your lines. First imagine the situation and the person who’s offering the drink. Then write both what the person will say and how you’ll respond, whether it’s a broken record strategy (mentioned above) or your own unique approach. Rehearse it aloud to get comfortable with your phrasing and delivery. Also, consider asking a supportive person to role-play with you, someone who would offer realistic pressure to drink and honest feedback about your responses. Whether you practice through made-up or real-world experiences, you’ll learn as you go. Keep at it, and your skills will grow over time.
- Try other strategies
In addition to being prepared with your “no thanks,” consider these strategies:
- Have non-alcoholic drinks always in hand if you’re quitting, or as “drink spacers” between drinks if you’re cutting back
- Keep track of every drink if you’re cutting back so you stay within your limits
- Ask for support from others to cope with temptation
- Plan an escape if the temptation gets too great
- Ask others to refrain from pressuring you or drinking in your presence (this can be hard)
If you have successfully refused drink offers before, then recall what worked and build on it.
Remember, it’s your choice
How you think about any decision to change can affect your success. Many people who decide to cut back or quit drinking think, “I am not allowed to drink,” as if an external authority were imposing rules on them. Thoughts like this can breed resentment and make it easier to give in. It’s important to challenge this kind of thinking by telling yourself that you are in charge, that you know how you want your life to be, and that you have decided to make a change.
Similarly, you may worry about how others will react or view you if you make a change. Again, challenge these thoughts by remembering that it’s your life and your choice, and that your decision should be respected.
Plan to resist pressure to drink
It’s not possible to avoid all high-risk situations or to block internal triggers, so you’ll need a range of strategies to handle urges to drink. Here are some options:
- Remind yourself of your reasons for making a change. Carry your top reasons on a wallet card or in an electronic message that you can access easily, such as a mobile phone notepad entry or a saved email.
- Talk it through with someone you trust. Have a trusted friend on standby for a phone call, or bring one along to high-risk situations.
- Distract yourself with a healthy, alternative activity. For different situations, come up with engaging short, mid-range, and longer options, like texting or calling someone, watching short online videos, lifting weights to music, showering, meditating, taking a walk, or doing a hobby.
- Challenge the thought that drives the urge. Stop it, analyze the error in it, and replace it. Example: “It couldn’t hurt to have one little drink. WAIT a minute—what am I thinking? One could hurt, as I’ve seen ‘just one’ lead to lots more. I am sticking with my choice not to drink.”
- Ride it out without giving in. Instead of fighting an urge, accept it as normal and temporary. As you ride it out, keep in mind that it will soon crest like an ocean wave and pass.
- Leave high-risk situations quickly and gracefully. It helps to plan your escape in advance.
How to cut down or to quit drinking alcohol
If you’re considering changing your drinking, you’ll need to decide whether to cut down or to quit. It’s a good idea to discuss different options with a doctor, a friend, or someone else you trust.
Quitting is strongly advised if you:
- Try cutting down but cannot stay within the limits you set.
- Have had an alcohol use disorder or now have symptoms.
- Have a physical or mental condition that is caused or worsened by drinking.
- Are taking a medication that interacts with alcohol.
- Are or may become pregnant.
If none of the conditions above apply to you, then talk with your doctor to determine whether you should cut down or quit based on factors such as:
- Family history of alcohol problems
- Your age
- Whether you’ve had drinking-related injuries
- Symptoms such as sleep disorders and sexual dysfunction
Planning for change
Even when you have committed to making a change, you still may have mixed feelings at times. Making a written “My Alcohol Change Plan” will help you to solidify your goals, why you want to reach them, and how you plan to do it.
A sample format is provided below. After filling it in, you can print it or email it to yourself.
- Goal:(select one) I want to drink no more than drink(s) on any day and no more than drink(s) per week OR I want to stop drinking.
- Timing: I will start on this date:
- Reasons: My most important reasons to make these changes are:
- Strategies: I will use these strategies:
- People: The people who can help me are (names and how they can help):
- Signs of success: I will know my plan is working if:
- Possible roadblocks: Some things that might interfere—and how I’ll handle them:
Reminder strategies
Change can be hard, so it helps to have concrete reminders of why and how you’ve decided to do it. Some standard options include carrying a change plan in your wallet or posting sticky notes at home. Also consider these high-tech ideas:
- Fill out a change plan, email it to your personal (non-work) account, store it in a private online folder, and review it weekly.
- Store your goals, reasons, or strategies in your mobile phone as short text messages or notepad entries that you can retrieve when an urge hits.
- Set up automated mobile phone or email calendar alerts that deliver reminders when you choose, such as a few hours before you usually go out. (Email providers such as Gmail and Yahoo mail have online calendars with alert options.)
- Create passwords that are motivating phrases in code, which you’ll reinforce each time you log in, such as 1Day@aTime, 1stThings1st!, or 0Pain=0Gain.
Social support to stop drinking
One potential challenge when people stop drinking is rebuilding a life without alcohol. It may be important to:
- Educate family and friends.
- Develop new interests and social groups.
- Find rewarding ways to spend your time that don’t involve alcohol.
- Ask for help from others.
When asking for support from friends or significant others, be specific. This could include:
- Not offering you alcohol
- Not using alcohol around you
- Giving words of support and withholding criticism
- Not asking you to take on new demands right now
- Going to a group like Alcoholics Anonymous 48
Consider joining Alcoholics Anonymous or another mutual support group (see links below). Recovering people who attend support groups regularly do better than those who do not. Groups can vary widely, so shop around for one that’s comfortable. You’ll get more out of it if you become actively involved by having a sponsor and reaching out to other members for assistance.
- Alcoholics Anonymous (https://www.aa.org)
- Moderation Management (https://moderation.org)
- Secular Organizations for Sobriety (https://www.sossobriety.org)
- SMART Recovery (https://www.smartrecovery.org)
- Women for Sobriety (https://womenforsobriety.org)
- Al-Anon Family Groups (https://al-anon.org)
- Adult Children of Alcoholics (https://adultchildren.org)
- National Council on Alcoholism and Drug Dependence (https://recovered.org)
- National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov)
- National Organization on Fetal Alcohol Syndrome (https://fasdunited.org)
- Substance Abuse and Mental Health Services Administration (https://findtreatment.gov)
Alcoholics anonymous
Alcoholics Anonymous or AA is a fellowship of people who come together to solve their drinking problem 49. Alcoholics Anonymous is FREE and its membership is open to anyone who wants to do something about their drinking problem. It’s FREE to attend AA meetings. There are no age or education requirements to participate. A.A.’s primary purpose is to help alcoholics to achieve sobriety. A.A. does not promise to solve your life’s problems, but AA can show you how to live without drinking “one day at a time.” You stay away from that “first drink.” If there is no first one, there cannot be a tenth one. And when you get rid of alcohol, you’ll find that your life will became much more manageable. To find Alcoholics Anonymous meetings near you please go here: https://www.aa.org/find-aa
Bill W. and Dr. Bob S. (both gentlemen were alcoholics) founded Alcoholics Anonymous in 1935 at Akron, Ohio. They wrote the book Twelve Steps and Twelve Traditions to share their 18 years of collective experience within the Fellowship on how A.A. members recover, and how the society functions. A.A.’s 12 Traditions apply to the life of the Fellowship itself. They outline the means by which A.A. maintains its unity and relates itself to the world about it, the way it lives and grows. The basic principles of A.A., as they are known today, were borrowed mainly from the fields of religion and medicine, though some ideas upon which success finally depended were the result of noting the behavior and needs of the Fellowship itself.
Patients do not need a strong religious background to be successful in AA; they only need the belief in a power higher than themselves. Patients who have tried AA may have had a bad past experience. Patients should try at least 5-10 different meetings before giving up on the AA approach because each meeting is different. For example, women often do better at meetings for women only because the issues for female patients with alcoholism are different from the issues for male patients with alcoholism. A meeting in the suburbs might not be appropriate for someone from the inner city and vice versa. No randomized trials of AA have been performed, but a US Veterans Administration study suggested that patients who attended meetings did much better than those who refused to go.
AA meetings near me
To find Alcoholics Anonymous meetings near you please click here: https://www.aa.org/find-aa
12 steps of AA
A.A.’s 12 Steps are a group of principles, spiritual in their nature, which, if practiced as a way of life, can expel the obsession to drink and enable the sufferer to become happily and usefully whole. The 12 Steps Alcoholics Anonymous can be found in the book Alcoholics Anonymous 50. The AA 12-step approach involves psychosocial techniques used in changing behavior (eg, rewards, social support networks, role models). Each new person is assigned an AA sponsor (a person recovering from alcoholism who supervises and supports the recovery of the new member). The sponsor should be older and should be of the same sex as the patient (opposite sex if the patient is homosexual).
- We admitted we were powerless over alcohol—that our lives had become unmanageable. (https://www.aa.org/sites/default/files/2022-01/en_step1.pdf)
- Came to believe that a Power greater than ourselves could restore us to sanity. (https://www.aa.org/sites/default/files/2022-01/en_step2.pdf)
- Made a decision to turn our will and our lives over to the care of God as we understood Him. (https://www.aa.org/sites/default/files/2022-01/en_step3.pdf)
- Made a searching and fearless moral inventory of ourselves. (https://www.aa.org/sites/default/files/2022-01/en_step4.pdf)
- Admitted to God, to ourselves, and to another human being the exact nature of our wrongs. (https://www.aa.org/sites/default/files/2022-01/en_step5.pdf)
- Were entirely ready to have God remove all these defects of character. (https://www.aa.org/sites/default/files/2022-01/en_step6.pdf)
- Humbly asked Him to remove our shortcomings. (https://www.aa.org/sites/default/files/2022-01/en_step7.pdf)
- Made a list of all persons we had harmed, and became willing to make amends to them all. (https://www.aa.org/sites/default/files/2022-01/en_step8.pdf)
- Made direct amends to such people wherever possible, except when to do so would injure them or others. (https://www.aa.org/sites/default/files/2022-01/en_step9.pdf)
- Continued to take personal inventory and when we were wrong promptly admitted it. (https://www.aa.org/sites/default/files/2022-01/en_step10_0.pdf)
- Sought through prayer and meditation to improve our conscious contact with God as we understood Him, praying only for knowledge of His will for us and the power to carry that out. (https://www.aa.org/sites/default/files/2022-01/en_step11.pdf)
- Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs. (https://www.aa.org/sites/default/files/2022-01/en_step12.pdf)
What cause alcohol use disorder?
The cause of alcohol use disorder is not well understood; however, several factors are thought to contribute to its development. These include the home environment, peer interactions, genetic factors, level of cognitive functioning, and certain existing personality disorders 51.Personality disorders associated with the development of an alcohol use disorder include disinhibition and impulsivity-type disorders, as well as depressive and socialization-related disorders 52.
Almost half of the people with any substance abuse problem, including alcohol use disorder, also had a co-existing mental illness 53, 54. Overall, alcohol use disorder tends to be more common in individuals with less education and low income.
Multiple theories have been suggested as to why some people develop alcohol use disorders. Some of the more evidence-supported theories include positive-effect regulation, negative-effect regulation, pharmacological vulnerability, and deviance proneness. Positive-effect regulation results in drinking for positive rewards (such as feelings of euphoria). Negative-effect regulation is seen when one drinks to cope with feelings of a negative nature, such as depression, anxiety, or feelings of worthlessness. Pharmacological vulnerability makes a note of an individual’s varied response to both acute and chronic effects of alcohol intake and the individual differences in the body’s ability to metabolize the alcohol. Deviance proneness speaks more to an individual’s tendency towards deviant behavior established during childhood, often due to a deficiency in socialization at an early age.
Some of the genes suspected in alcohol use disorder include GABRG2 and GABRA2, COMT Val 158Met, DRD2 Taq1A, and KIAA0040.
Risk factors for alcoholism
There is no single factor that accounts for the variation in individual risk of developing alcohol-use disorders. Alcohol use may begin in the teens, but alcohol use disorder occurs more frequently in the 20s and 30s, though it can start at any age. The evidence suggests that harmful alcohol use and alcohol dependence have a wide range of causal factors
- Family history of alcohol abuse. The risk of alcohol use disorder is higher for people who have a parent or other close relative who has problems with alcohol. This may be influenced by genetic factors.
- offspring of parents with alcohol dependence are four times more likely to develop alcohol dependence
- genetic studies (particularly those in twins) has clearly demonstrated a genetic component to the risk of alcohol dependence
- a meta-analysis of 9,897 twin pairs from Australian and US studies found the heritability of alcohol dependence to be in excess of 50%
- Psychological factors
- psychiatric comorbidity particularly depression, schizophrenia, bipolar disorder (BPD), anxiety, post-traumatic stress disorder (PTSD), psychosis and drug misuse. It’s common for people with a mental health disorder such as anxiety, depression, schizophrenia or bipolar disorder to have problems with alcohol or other substances.
- Stress, adverse life events and abuse
- Sex: men are twice as likely to be problem drinkers
- Occupation:
- publicans and brewers have an increased access to drink and are at a higher risk
- heavy drinking is seen as the norm in some jobs e.g. sailors
- Homelessness:
- a third of homeless people have a drink problem
- Steady drinking over time. Drinking too much on a regular basis for an extended period or binge drinking on a regular basis can lead to alcohol-related problems or alcohol use disorder.
- Started drinking at an early age. People who begin drinking — especially binge drinking — at an early age are at a higher risk of alcohol use disorder.
- History of trauma. People with a history of emotional or other trauma are at increased risk of alcohol use disorder.
- Having bariatric surgery (weight-loss surgery — involves making changes to your digestive system to help you lose weight). Some research studies indicate that having bariatric surgery may increase the risk of developing alcohol use disorder or of relapsing after recovering from alcohol use disorder.
- Social and cultural factors. Having friends or a close partner who drinks regularly could increase your risk of alcohol use disorder. The glamorous way that drinking is sometimes portrayed in the media also may send the message that it’s OK to drink too much. For young people, the influence of parents, peers and other role models can impact risk.
Alcohol addiction prevention
Early intervention can prevent alcohol-related problems in teens. If you have a teenager, be alert to signs and symptoms that may indicate a problem with alcohol:
- Loss of interest in activities and hobbies and in personal appearance
- Red eyes, slurred speech, problems with coordination and memory lapses
- Difficulties or changes in relationships with friends, such as joining a new crowd
- Declining grades and problems in school
- Frequent mood changes and defensive behavior
You can help prevent teenage alcohol use:
- Set a good example with your own alcohol use.
- Talk openly with your child, spend quality time together and become actively involved in your child’s life.
- Let your child know what behavior you expect — and what the consequences will be if he or she doesn’t follow the rules.
Alcoholism signs and symptoms
A few mild symptoms — which you might not see as trouble signs — can signal the start of a drinking problem. It helps to know the signs so you can make a change early. If heavy drinking continues, then over time, the number and severity of symptoms can grow and add up to “alcohol use disorder.” Doctors diagnose alcohol use disorder when a patient’s drinking causes distress or harm. See if you recognize any of these symptoms in yourself. And don’t worry — even if you have symptoms, you can take steps to reduce your risks.
Alcohol use disorder can be mild, moderate or severe, based on the number of symptoms you experience.
Alcohol use disorder signs and symptoms may include:
- Being unable to limit the amount of alcohol you drink
- Wanting to cut down on how much you drink or making unsuccessful attempts to do so
- Spending a lot of time drinking, getting alcohol or recovering from alcohol use
- Feeling a strong craving or urge to drink alcohol
- Failing to fulfill major obligations at work, school or home due to repeated alcohol use
- Continuing to drink alcohol even though you know it’s causing physical, social or interpersonal problems
- Giving up or reducing social and work activities and hobbies
- Using alcohol in situations where it’s not safe, such as when driving or swimming
- Developing a tolerance to alcohol so you need more to feel its effect or you have a reduced effect from the same amount
- Experiencing withdrawal symptoms — such as nausea, sweating and shaking — when you don’t drink, or drinking to avoid these symptoms
Alcohol use disorder can include periods of alcohol intoxication and symptoms of withdrawal.
- Alcohol intoxication results as the amount of alcohol in your bloodstream increases. The higher the blood alcohol concentration is, the more impaired you become. Alcohol intoxication causes behavior problems and mental changes. These may include inappropriate behavior, unstable moods, impaired judgment, slurred speech, impaired attention or memory, and poor coordination. You can also have periods called “blackouts,” where you don’t remember events. Very high blood alcohol levels can lead to coma or even death.
- Alcohol withdrawal can occur when alcohol use has been heavy and prolonged and is then stopped or greatly reduced. It can occur within several hours to four or five days later. Signs and symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping, nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures. Symptoms can be severe enough to impair your ability to function at work or in social situations.
The more symptoms you have, the more serious the problem is. If you think you might have an alcohol use disorder, see your health care provider for an evaluation. Your provider can help make a treatment plan, prescribe medicines, and if needed, give you treatment referrals.
People with alcohol use disorder may also report frequent falls, blackout spells, unsteadiness, or visual disturbances 51. They may report seizures if they went a few days without drinking, or tremors, confusion, emotional disturbances, and frequent job changes. They may also report social issues, such as job termination, separation/divorce, estrangement from family, or loss of home. They may also report sleep disturbances.
People with alcohol use disorder may have hypertension (high blood pressure) or insomnia (trouble falling and staying asleep) initially. In later stages, the patient may complain of nausea or vomiting, hematemesis (vomiting blood), bloated abdomen, epigastric pain, weight loss, jaundice, or other symptoms or signs suggestive of liver dysfunction. They may be asymptomatic early on.
People with alcohol use disorder may exhibit signs of cerebellar dysfunction, such as ataxia (impaired balance or coordination) or difficulty with fine motor skills, on exam. They may exhibit slurred speech, tachycardia (fast heart rate), memory impairment, nystagmus (involuntary eye movement which may cause the eye to rapidly move from side to side, up and down or in a circle), disinhibited behavior, or hypotension (low blood pressure). People with alcohol use disorder may present with tremors, confusion/mental status changes, asterixis, reddsih palms, jaundice, ascites, or other signs of advanced liver disease. There may also be spider angiomata, hepatomegaly/splenomegaly (early; liver becomes cirrhotic and shrunken in advanced disease). They may develop bleeding disorders, anemia, gastritis/ulcers, or pancreatitis as complications of alcohol use. Labs will reveal anemia, thrombocytopenia, coagulopathy, hyponatremia, hyperammonemia, elevated ammonia levels, or decreased B12/folate levels as the advanced liver disease develops.
Alcohol abuse complications
Alcohol depresses your central nervous system. In some people, the initial reaction may be stimulation. But as you continue to drink, you become sedated.
Too much alcohol affects your speech, muscle coordination and vital centers of your brain. A heavy drinking binge may even cause a life-threatening coma or death. This is of particular concern when you’re taking certain medications that also depress the brain’s function.
Alcohol abuse impacting on your safety
Excessive drinking can reduce your judgment skills and lower inhibitions, leading to poor choices and dangerous situations or behaviors, including:
- Motor vehicle accidents and other types of accidental injury, such as drowning
- Relationship problems
- Poor performance at work or school
- Increased likelihood of committing violent crimes or being the victim of a crime
- Legal problems or problems with employment or finances
- Problems with other substance use
- Engaging in risky, unprotected sex, or experiencing sexual abuse or date rape
- Increased risk of attempted or completed suicide
Alcohol abuse impacting on your health
Drinking too much alcohol on a single occasion or over time can cause health problems, including:
- Liver disease. Heavy drinking can cause increased fat in the liver (hepatic steatosis), inflammation of the liver (alcoholic hepatitis), and over time, irreversible destruction and scarring of liver tissue (cirrhosis).
- Digestive problems. Heavy drinking can result in inflammation of the stomach lining (gastritis), as well as stomach and esophageal ulcers. It can also interfere with absorption of B vitamins and other nutrients. Heavy drinking can damage your pancreas or lead to inflammation of the pancreas (pancreatitis).
- Heart problems. Excessive drinking can lead to high blood pressure and increases your risk of an enlarged heart, heart failure or stroke. Even a single binge can cause a serious heart arrhythmia called atrial fibrillation.
- Diabetes complications. Alcohol interferes with the release of glucose from your liver and can increase the risk of low blood sugar (hypoglycemia). This is dangerous if you have diabetes and are already taking insulin to lower your blood sugar level.
- Sexual function and menstruation issues. Excessive drinking can cause erectile dysfunction in men. In women, it can interrupt menstruation.
- Eye problems. Over time, heavy drinking can cause involuntary rapid eye movement (nystagmus) as well as weakness and paralysis of your eye muscles due to a deficiency of vitamin B-1 (thiamin). A thiamin deficiency can also be associated with other brain changes, such as irreversible dementia, if not promptly treated.
- Birth defects. Alcohol use during pregnancy may cause miscarriage. It may also cause fetal alcohol syndrome, resulting in giving birth to a child who has physical and developmental problems that last a lifetime.
- Bone damage. Alcohol may interfere with the production of new bone. This bone loss can lead to thinning bones (osteoporosis) and an increased risk of fractures. Alcohol can also damage bone marrow, which makes blood cells. This can cause a low platelet count, which may result in bruising and bleeding.
- Neurological complications. Excessive drinking can affect your nervous system, causing numbness and pain in your hands and feet, disordered thinking, dementia, and short-term memory loss.
- Wernicke encephalopathy: Wernicke’s encephalopathy is caused by acute thiamine (Vitamin B1) deficiency. Wernicke encephalopathy causes brain damage in the lower parts of the brain called the thalamus and hypothalamus. Symptoms of Wernicke encephalopathy include:
- Confusion and loss of mental activity that can progress to coma and death
- Loss of muscle coordination (ataxia) that can cause leg tremor
- Vision changes such as abnormal eye movements (back and forth movements called nystagmus), double vision, eyelid drooping
- Alcohol withdrawal
- Vitamin B1 (Thiamine) is usually given by injection into a vein or a muscle as soon as possible. This may improve symptoms of:
- Confusion or delirium
- Difficulties with vision and eye movement
- Lack of muscle coordination
- Korsakoff syndrome or Korsakoff psychosis, tends to develop as Wernicke encephalopathy symptoms go away. Korsakoff psychosis results from permanent damage to areas of the brain involved with memory (anterograde and retrograde amnesia), often with confabulation (making up stories) and preceded by Wernicke encephalopathy. Symptoms of Korsakoff syndrome include:
- Inability to form new memories
- Loss of memory, can be severe
- Making up stories (confabulation)
- Seeing or hearing things that are not really there (hallucinations)
- Vitamin B1 (Thiamine) often does not improve loss of memory and intellect that occur with Korsakoff syndrome. Stopping alcohol use can prevent more loss of brain function and damage to nerves.
- Wernicke encephalopathy: Wernicke’s encephalopathy is caused by acute thiamine (Vitamin B1) deficiency. Wernicke encephalopathy causes brain damage in the lower parts of the brain called the thalamus and hypothalamus. Symptoms of Wernicke encephalopathy include:
- Weakened immune system. Excessive alcohol use can make it harder for your body to resist disease, increasing your risk of various illnesses, especially pneumonia.
- Increased risk of cancer. Long-term, excessive alcohol use has been linked to a higher risk of many cancers, including mouth, throat, liver, esophagus, colon and breast cancers. Even moderate drinking can increase the risk of breast cancer.
- Medication and alcohol interactions. Some medications interact with alcohol, increasing its toxic effects. Drinking while taking these medications can either increase or decrease their effectiveness, or make them dangerous.
Alcoholism diagnosis
You’re likely to start by seeing your doctor. If your doctor suspects you have a problem with alcohol, he or she may refer you to a mental health professional.
To assess your problem with alcohol, your doctor will likely:
- Ask you several questions related to your drinking habits. The doctor may ask for permission to speak with family members or friends. However, confidentiality laws prevent your doctor from giving out any information about you without your consent.
- Perform a physical exam. Your doctor may do a physical exam and ask questions about your health. There are many physical signs that indicate complications of alcohol use.
- Lab tests and imaging tests. While there are no specific tests to diagnose alcohol use disorder, certain patterns of lab test abnormalities may strongly suggest it. And you may need tests to identify health problems that may be linked to your alcohol use. Damage to your organs may be seen on tests.
- Complete a psychological evaluation. This evaluation includes questions about your symptoms, thoughts, feelings and behavior patterns. You may be asked to complete a questionnaire to help answer these questions.
- Use the DSM-5 criteria. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published by the American Psychiatric Association, is often used by mental health professionals to diagnose mental health conditions.
DSM-5 alcohol use disorder
DSM-5 Criteria for the Diagnosis of Alcohol Use Disorder 55:
- Criterion A. A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- a. A need for markedly increased amounts of alcohol to achieve intoxication or desired effect.
- b. A markedly diminished effect with continued use of the same amount of alcohol.
- Withdrawal, as manifested by either of the following:
- a. The characteristic withdrawal syndrome for alcohol.
- b. Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
Specify if:
- In early remission: After full criteria for alcohol use disorder were previously met, none of the criteria for alcohol use disorder have been met for at least 3 months but for less than 12 months (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
- In sustained remission: After full criteria for alcohol use disorder were previously met, none of the criteria for alcohol use disorder have been met at any time during a period of 12 months or longer (with the exception that Criterion A4, “Craving, or a strong desire or urge to use alcohol,” may be met).
Specify if:
- In a controlled environment: This additional specifier is used if the individual is in an environment where access to alcohol is restricted.
Alcohol use disorder is defined by a cluster of behavioral and physical symptoms, which can include withdrawal, tolerance, and craving. Alcohol withdrawal is characterized by withdrawal symptoms that develop approximately 4-12 hours after the reduction of intake following prolonged, heavy alcohol ingestion. Because withdrawal from alcohol can be unpleasant and intense, individuals may continue to consume alcohol despite adverse consequences, often to avoid or to relieve withdrawal symptoms. Some withdrawal symptoms (e.g., sleep problems) can persist at lower intensities for months and can contribute to relapse. Once a pattern of repetitive and intense use develops, individuals with alcohol use disorder may devote substantial periods of time to obtaining and consuming alcoholic beverages.
Craving for alcohol is indicated by a strong desire to drink that makes it difficult to think of anything else and that often results in the onset of drinking. School and job performance may also suffer either from the aftereffects of drinking or from actual intoxication at school or on the job; child care or household responsibilities may be neglected; and alcohol-related absences may occur from school or work. The individual may use alcohol in physically hazardous circumstances (e.g., driving an automobile, swimming, operating machinery while intoxicated). Finally, individuals with an alcohol use disorder may continue to consume alcohol despite the knowledge that continued consumption poses significant physical (e.g., blackouts, liver disease), psychological (e.g., depression), social, or interpersonal problems (e.g., violent arguments with spouse while intoxicated, child abuse).
Laboratory studies
Currently, there are no biomarkers that can directly identify alcoholism 56. Alcohol biomarkers are physiological indicators of alcohol exposure or ingestion and may reflect the presence of an alcohol use disorder. These biomarkers are not meant to be a substitute for a comprehensive history and physical examination by an appropriate health professional. Instead, alcohol biomarkers should be a complement to self-reported measures of drinking. Alcohol biomarkers are generally divided into indirect and direct biomarkers 57.
Indirect alcohol biomarkers suggest heavy alcohol use by detecting the toxic effects that alcohol may have had on organ systems or body chemistry 57. Indirect alcohol biomarkers, which suggest heavy alcohol use by detecting the toxic effects of alcohol, include aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma glutamyltransferase (GGT), mean corpuscular volume (MCV), and carbohydrate-deficient transferrin (CDT).
Gamma glutamyltransferase (GGT), aspartate aminotransferase (AST), and mean corpuscular volume (MCV) are the most frequently used indirect biomarkers 58. As a screen for alcohol dependence, the sensitivity/specificity of carbohydrate-deficient transferrin (CDT) is generally higher than AST, ALT, GGT, or MCV 59, 60. Carbohydrate-deficient transferrin (CDT) is less sensitive/specific in women than men 61.
Carbohydrate-deficient transferrin (CDT) is a collection of various isoforms of the iron transport protein transferrin 58. Alcohol consumption above 50-80 g/d for 2-3 weeks appears to increase serum concentrations of CDT 60. CDT tends to distinguish chronic heavy drinkers from light social drinkers 58. A number of different ways are available to measure CDT; some may be better than others, depending on factors such as the type of alcohol consumption and gender 62.
The combination of gamma glutamyltransferase (GGT) and CDT compared with gamma glutamyltransferase (GGT) or CDT alone shows a higher diagnostic sensitivity, a higher diagnostic specificity, and a stronger correlation with the actual amounts of alcohol consumption 59, 60. Combination GGT/CDT values appear to increase after the daily alcohol consumption exceeds a threshold of 40 g 59. This approach is cost-effective, easy to manage in hospital laboratories, and should be suitable for routine clinical care 59.
Other indirect alcohol biomarkers of emerging interest include total serum sialic acid (TSA), 5-hydroxytryptophol (5-HTOL), N-acetyl-beta-hexosaminidase (Beta-Hex), plasma sialic acid index of apolipoprotein J (SIJ), and salsolinol 63.
Direct alcohol biomarkers are analytes of alcohol metabolism 57.
Direct alcohol biomarkers include alcohol itself and ethyl glucuronide (EtG) 57.
A blood alcohol level might be helpful in the office if the patient appears intoxicated but is denying alcohol abuse. Blood alcohol levels that indicate alcoholism with a high degree of reliability are as follows:
- A blood alcohol level in excess of 300 mg/dL in a patient who appears intoxicated but denies alcohol abuse
- A blood alcohol level of greater than 150 mg/dL without gross evidence of intoxication
- A blood alcohol level of greater than 100 mg/dL upon routine examination indicates alcoholism with a high degree of reliability
The short half-life of alcohol limits its use widely as a biomarker 59. As the blood alcohol level detects alcohol intake in the previous few hours, it is not necessarily a good indicator of chronic excessive drinking 58.
Ethyl glucuronide (EtG) is a minor, nonoxidative, water-soluble, stable, and direct metabolite of alcohol that is formed by the conjugation of ethanol with activated glucoronic acid 59. Shortly after alcohol intake, even in small amounts, EtG becomes positive 59. After complete cessation of alcohol intake, EtG can be detected in urine for up to 5 days after heavy binge drinking 59, making EtG an important biomarker of recent alcohol consumption 58. A 2006 report by the Substance Abuse and Mental Health Services Administration states that the use of EtG should be considered as a potential valuable clinical tool, but the use of EtG in forensic settings is premature.
Features of EtG are as follows:
- Becomes positive shortly after intake of alcohol, even in small amounts
- After complete cessation of alcohol intake, EtG can be detected in urine for up to 5 days after heavy binge drinking
Other direct alcohol biomarkers of emerging interest include acetaldehyde, fatty acid ethyl esters (FAEE), Ethyl Sulfate (EtS), and Phosphatidylethanol (PEth) 63.
Alcoholism treatment
Most people with an alcohol use disorder can benefit from some form of treatment. Medical treatments include medicines and behavioral therapies. For many people, using both types gives them the best results. People who are getting treatment for alcohol use disorder may also find it helpful to go to a support group such as Alcoholics Anonymous (AA). If you have an alcohol use disorder and a mental illness, it is important to get treatment for both.
Treatment for alcohol use disorder may include:
- Detox and withdrawal. Treatment may begin with a program of detoxification or detox — withdrawal that’s medically managed — which generally takes two to seven days. You may need to take sedating medications to prevent withdrawal symptoms. Detox is usually done at an inpatient treatment center or a hospital.
- Learning skills and establishing a treatment plan. This usually involves alcohol treatment specialists. It may include goal setting, behavior change techniques, use of self-help manuals, counseling and follow-up care at a treatment center.
- Psychological counseling. Counseling and therapy for groups and individuals help you better understand your problem with alcohol and support recovery from the psychological aspects of alcohol use. You may benefit from couples or family therapy — family support can be an important part of the recovery process.
- Oral medications. A drug called disulfiram (Antabuse) may help prevent you from drinking, although it won’t cure alcohol use disorder or remove the compulsion to drink. If you drink alcohol, the drug produces a physical reaction that may include flushing, nausea, vomiting and headaches. Naltrexone, a drug that blocks the good feelings alcohol causes, may prevent heavy drinking and reduce the urge to drink. Acamprosate may help you combat alcohol cravings once you stop drinking. Unlike disulfiram, naltrexone and acamprosate don’t make you feel sick after taking a drink.
- Injected medication. Vivitrol, a version of the drug naltrexone, is injected once a month by a health care professional. Although similar medication can be taken in pill form, the injectable version of the drug may be easier for people recovering from alcohol use disorder to use consistently.
- Continuing support. Aftercare programs and support groups help people recovering from alcohol use disorder to stop drinking, manage relapses and cope with necessary lifestyle changes. This may include medical or psychological care or attending a support group.
- Treatment for psychological problems. Alcohol use disorder commonly occurs along with other mental health disorders. If you have depression, anxiety or another mental health condition, you may need talk therapy (psychotherapy), medications or other treatment.
- Medical treatment for health conditions. Many alcohol-related health problems improve significantly once you stop drinking. But some health conditions may warrant continued treatment and follow-up.
- Spiritual practice. People who are involved with some type of regular spiritual practice may find it easier to maintain recovery from alcohol use disorder or other addictions. For many people, gaining greater insight into their spiritual side is a key element in recovery.
Some people may need intensive treatment for alcohol use disorder. They may go to a residential treatment center for rehabilitation (rehab). Residential treatment programs typically include licensed alcohol and drug counselors, social workers, nurses, doctors and others with expertise and experience in treating alcohol use disorder. Treatment there is highly structured. It usually includes several different kinds of behavioral therapies. Most residential treatment programs include individual and group therapy, support groups, educational lectures, family involvement and activity therapy. It may also include medicines for detox (medical treatment for alcohol withdrawal) and/or for treating the alcohol use disorder.
Medications for alcohol use disorder
The U.S. Food and Drug Administration (FDA) has approved three medications for treating alcohol dependence, and alcohol use disorder (see Table 1 below) 64. All of these medications are non-addictive, so you don’t have to worry about trading one addiction for another. Your health care provider can help you figure out if one of these medicines is right for you. They are not a cure, but they can help you manage alcohol use disorder. This is just like taking medicines to manage a chronic disease such as asthma or diabetes.
- Naltrexone can help people reduce heavy drinking.
- Acamprosate makes it easier to maintain abstinence.
- Disulfiram blocks the breakdown (metabolism) of alcohol by the body, causing unpleasant symptoms such as nausea and flushing of the skin. Those unpleasant effects can help some people avoid drinking while taking disulfiram.
- Psilocybin (4-phosphoryloxy-N,N-dimethyltryptamine). A 2022 study 65, the largest clinical trial of its kind, found that two doses of psilocybin pills, along with psychotherapy, helped individuals with alcohol use disorder reduce drinking for at least eight months after their first treatments. Trial participants included 93 men and women ages 25 to 65 who were averaging seven alcoholic drinks at a time before the study. More than 80% of those who were given the psychedelic treatment had drastically reduced their drinking eight months after the study started, compared to just over 50% in the antihistamine control group 65.
It is important to remember that not all people will respond to medications, but for a subset of individuals, they can be an important tool in overcoming alcohol dependence.
Of the FDA approved medications, the two newer ones (naltrexone and acamprosate) can make it easier to quit drinking by offsetting changes in the brain caused by alcoholism. They don’t make you sick if you do drink, unlike the older approved medication (disulfiram) 66.
Used in the context of a comprehensive treatment plan, medications for alcohol use disorder can provide an opportunity for behavioral therapies (counseling) to be helpful by reducing craving or helping to maintain abstinence from alcohol. In that way, medications can give people with an alcohol problem some traction in the recovery process.
It’s important to consult a doctor who understands which people are good candidates for alcohol use disorder medications. Some studies suggest that people with a family history of alcohol use disorder may be likely to benefit from naltrexone, for example. But those who have a liver condition or use opioid medications (such as those prescribed for pain) should not take naltrexone. A doctor can assess these and other conditions and match an appropriate medication with the patient.
As with any other medication, patients should communicate with their doctor about how the medication is working, and the doctor may be able to adjust the dose if needed.
Medications for alcohol use disorder can be prescribed not only by specialists in addiction treatment, but also by primary care physicians.
Scientists are working to develop a larger menu of pharmaceutical treatments that could be tailored to individual needs. As more medications become available, people may be able to try multiple medications to find which they respond to best.
Certain medications already approved for other uses have shown promise for treating alcohol dependence and problem drinking:
- The anti-smoking drug varenicline (marketed under the name Chantix) significantly reduced alcohol consumption and craving among people with alcoholism.
- Gabapentin, a medication used to treat pain conditions and epilepsy, was shown to increase abstinence and reduce heavy drinking. Those taking the medication also reported fewer alcohol cravings and improved mood and sleep.
- The anti-epileptic medication topiramate was shown to help people curb problem drinking, particularly among those with a certain genetic makeup that appears to be linked to the treatment’s effectiveness.
Acamprosate
Acamprosate (Campral®) acts on the gamma-aminobutyric acid (GABA) and glutamate neurotransmitter systems and is thought to reduce symptoms of protracted withdrawal, such as insomnia, anxiety, restlessness, and dysphoria 67. Acamprosate has been shown to help dependent drinkers maintain abstinence for several weeks to months, and it may be more effective in patients with severe dependence. Acamprosate is a pill that is taken three times per day.
Acamprosate appears to be most effective at maintaining abstinence in patients who are not currently drinking alcohol 68. Acamprosate seems to interact with glutamate at the N-methyl-d-aspartate receptor, although its exact mechanism is unclear 69. Acamprosate is safe in patients with impaired liver function but should be avoided in patients with severe kidney dysfunction. A systematic review of 27 studies including 7,519 patients using acamprosate showed a number needed to treat (NNT) of 12 to prevent a return to any drinking 70. A Cochrane review of 24 trials including 6,915 patients concluded that acamprosate reduced drinking compared with placebo (NNT = 9) 71. One randomized trial found no difference between acamprosate and placebo, although outcomes improved significantly in both groups. This may be because enrolled patients were highly motivated to decrease alcohol use, increasing the likelihood of success with any treatment 72.
Disulfiram
Disulfiram (Antabuse®) interferes with degradation of alcohol, resulting in the accumulation of acetaldehyde, which, in turn, produces a very unpleasant reaction that includes flushing, nausea, and plapitations whenever you drink alcohol 67. Knowing that drinking will cause these unpleasant effects may help you stay away from alcohol. The utility and effectiveness of disulfiram are considered limited because compliance is generally poor. However, among patients who are highly motivated, disulfiram can be effective, and some patients use it episodically for high-risk situations, such as social occasions where alcohol is present. It can also be administered in a monitored fashion, such as in a clinic or by a spouse, improving its efficacy.
There are limited trials to support the effectiveness of disulfiram. It does not reduce the craving for alcohol, but it causes unpleasant symptoms when alcohol is ingested because it inhibits aldehyde dehydrogenase and alcohol metabolism. Compliance is a major limitation, and disulfiram is more effective when taken under supervision. One trial randomized 243 patients to naltrexone, acamprosate, or disulfiram with supervision over 12 weeks and determined that patients taking disulfiram had fewer heavy drinking days, lower weekly consumption, and a longer period of abstinence compared with the other drugs 73. However, a 2014 meta-analysis of 22 randomized trials found that in open-label studies, disulfiram was more effective than naltrexone, acamprosate, and no disulfiram, but blinded studies did not demonstrate benefit for disulfiram 74. In a systematic review of two studies including 492 patients, disulfiram did not reduce drinking rates 70. A review by the Agency for Healthcare Research and Quality on pharmacotherapy for adults with alcohol-use disorders in outpatient settings found insufficient evidence to support disulfiram’s effectiveness 75.
Naltrexone
Naltrexone blocks opioid receptors that are involved in the rewarding effects of drinking and the craving for alcohol 67. Naltrexone is an opioid antagonist, reduces alcohol consumption in patients with alcohol use disorder and is more successful in those who are abstinent before starting the medication 76. The opioid receptor system mediates the pleasurable effects of alcohol. Alcohol ingestion stimulates endogenous opioid release and increases dopamine transmission. Naltrexone blocks these effects, reducing euphoria and cravings 77. Naltrexone comes either as a pill that is taken daily, or as an injection that can be given once per month. Because naltrexone is metabolized by the liver, liver toxicity is possible, although uncommon. Patients with alcohol use disorder may have liver dysfunction; therefore, caution is warranted. Naltrexone can precipitate severe opioid withdrawal in patients who are opioid-dependent, so these agents should not be used together, and opioids should not be used for at least seven days before starting naltrexone 76. Pain management is challenging for patients taking naltrexone; these patients should carry a medical alert card.
Naltrexone is well tolerated and is not habit-forming. Naltrexone can also reduce your craving for alcohol. This can help you cut back on your drinking.
A Cochrane review that included 50 randomized trials and 7,793 patients found that oral naltrexone decreased heavy drinking (number needed to treat (NNT) = 10) and slightly decreased daily drinking (NNT = 25). The number of heavy drinking days and the amount of alcohol consumed also decreased. Injectable naltrexone did not decrease heavy drinking, but the sample size was small 78. A subsequent systematic review of 53 randomized trials including 9,140 patients found that oral naltrexone increased abstinence rates (NNT = 20) and decreased heavy drinking (NNT = 12). There was no difference between naltrexone and acamprosate. Injectable naltrexone did not demonstrate benefit 70. A randomized trial of 627 veterans with alcohol use disorder who received injectable naltrexone or placebo found that 380 mg of naltrexone given intramuscularly decreased heavy drinking days over six months but did not increase abstinence rates 79. Another meta-analysis found no difference in heavy drinking between acamprosate and naltrexone; however, it favored acamprosate for abstinence and naltrexone for cravings 68. Studies of combination therapy with acamprosate and naltrexone have produced mixed results. The COMBINE study did not show that combined therapy was more effective than either agent alone 80. Another study showed that relapse rates were lower with combined therapy compared with placebo or acamprosate alone, but not compared with naltrexone alone 81. It is unclear if and when combination therapy should be used, although it may be reasonable to consider it if monotherapy fails. Opioid antagonists may also be helpful when used as needed during high-risk situations, such as social events or weekends 82.
Like any medicine, naltrexone can cause side effects. Nausea is the most common one. Other side effects include:
- Headache
- Diarrhea
- Constipation
- Dizziness
- Nervousness
- Insomnia
- Drowsiness
- Anxiety
If you get any of these side effects, tell your doctor. They may change your treatment or suggest ways you can deal with the side effects.
Call your doctor immediately if you experience any of the following symptoms:
- Blurry vision
- Confusion
- Hallucinations (hearing or seeing things that aren’t there)
- Severe vomiting or diarrhea
- Vomiting up blood
- Excessive fatigue
- Bleeding or bruising
- Loss of appetite
- Pain in the upper right part of your stomach that lasts more than a few days
- Light-colored bowel movements
- Dark urine
- Yellowing of the skin or eyes
Talk to your doctor if you have a history of depression. Naltrexone may cause liver damage when taken in large doses. Tell your doctor if you have had hepatitis or liver disease.
Off-label medications
- Anticonvulsants. There are several anticonvulsants that may help patients with alcohol use disorder decrease alcohol consumption, but data are limited. A Cochrane review of 25 trials including 2,641 patients showed that those taking an anticonvulsant (i.e., topiramate, gabapentin [Neurontin], valproate, levetiracetam [Keppra], oxcarbazepine [Trileptal], zonisamide [Zonegran], carbamazepine [Tegretol], pregabalin [Lyrica], or tiagabine [Gabitril]) consumed 1.5 fewer drinks per day than those taking placebo. There was no difference in abstinence rates compared with naltrexone, but anticonvulsants were associated with fewer heavy drinking days and a longer time to relapse; many of the studies were of low quality 83. Topiramate appears to decrease alcohol consumption. The Agency for Healthcare Research and Quality review concluded that there is moderate evidence that topiramate decreases number of drinking days, heavy drinking days, and drinks per day based on two randomized trials 84. An open-label study compared topiramate plus psychotherapy with psychotherapy alone in hospitalized patients after alcohol withdrawal treatment. The topiramate group had lower rates of depression and anxiety and a lower relapse rate after four months 85. However, a randomized trial of 106 patients did not show a difference in alcohol consumption between topiramate therapy and placebo 86. Another randomized trial found that topiramate increased abstinence rates in patients with a specific genetic polymorphism 87. Such targeted medication use for specific populations warrants further study. Three randomized trials suggest a possible benefit from gabapentin. A study of 150 patients found higher abstinence rates in those taking gabapentin compared with placebo (NNT = 8), as well as lower rates of heavy drinking, improved mood, fewer cravings, and improved sleep 88. A study of 60 males with an average alcohol consumption of 17 drinks per day in the previous 90 days who underwent alcohol withdrawal treatment and were treated with gabapentin or placebo found that those in the gabapentin group had fewer heavy drinking days and drank less during the 30-day trial 89. A small study of 21 patients had similar results and also found that gabapentin was more effective at improving sleep over the first six weeks of therapy. Dosages of gabapentin used in the study varied from 300 mg twice per day to 1,800 mg at bedtime 90. Longer studies are needed to evaluate gabapentin for alcohol use disorder. Pregabalin is classified as a controlled substance, and there are limited data regarding its use in alcohol use disorder. A randomized trial comparing pregabalin and naltrexone in 71 patients found no difference in drinking outcomes or cravings, but the pregabalin group had less anxiety, hostility, and psychotic symptomatology 91.
- Antidepressants. Antidepressants are not effective in decreasing alcohol use in persons without coexisting mental health disorders 92. Antidepressants can be helpful in some instances, however, because patients with alcohol use disorder often have coexisting mental health disorders. A trial randomized 170 patients with alcohol dependence and depression to 14 weeks of cognitive behavior therapy plus sertraline (Zoloft; 200 mg per day), naltrexone (100 mg per day), both medications, or double placebo. Those taking a combination of sertraline and naltrexone had higher abstinence rates and a longer delay before relapse to heavy drinking compared with those taking placebo or either agent alone. Neither agent alone was superior to placebo 93. A study of patients with alcohol use disorder and major depression found that 20 to 40 mg per day of fluoxetine (Prozac) reduced drinking, drinking days, and heavy drinking days over 12 weeks 94. There is inconclusive evidence regarding the effectiveness of treating alcohol use disorder with the atypical antipsychotics olanzapine (Zyprexa) and quetiapine (Seroquel).
- Ondansetron. Ondansetron (Zofran) may decrease alcohol consumption in patients with alcohol use disorder. In three studies, ondansetron (4 mcg per kg twice per day) combined with cognitive behavior therapy decreased alcohol consumption and cravings and increased abstinence in young adults with early alcohol use disorder 95. In another trial, a higher dosage of ondansetron (16 mcg per kg twice per day) combined with cognitive behavior therapy decreased depression, anxiety, and hostility 96. This effect may be due to the serotonin-3 antagonist properties of ondansetron. In another randomized trial, men taking ondansetron (8 mg twice per day) had fewer heavy drinking days compared with those taking placebo, although they did not have increased abstinence rates 97. The combination of ondansetron (4 mcg per kg twice per day) and naltrexone (25 mg twice per day) may be effective in treating early alcohol use disorder 97. The dosages commonly studied (4 to 16 mcg per kg twice per day) are much lower than the current available formulations of 4-mg and 8-mg tablets.
Table 1. Medications for the treatment of Alcohol Use Disorder
| Medication | FDA approved for alcohol use disorder | Dosage | Adverse effects | Contraindications* | Comments |
|---|---|---|---|---|---|
| Acamprosate‡ (Campral) | Yes | Two 333-mg enteric-coated tablets three times per day Moderate renal impairment (creatinine clearance of 30 to 50 mL per minute per 1.73 m2 [0.50 to 0.83 mL per second per m2]): initially, one tablet three times per day | Diarrhea, insomnia, anxiety, depression, asthenia, anorexia, pain, flatulence, nausea, dizziness, pruritus, dry mouth, paresthesia, sweating | Severe renal impairment (creatinine clearance < 30 mL per minute per 1.73 m2) | Pregnancy category C, safety unknown in breastfeeding |
| Disulfiram (Antabuse) | Yes | Begin with 250 mg once per day; if not effective, increase to 500 mg once per day | Disulfiram-alcohol interaction: flushing, palpitations, nausea, vomiting, headache Optic neuritis, peripheral neuritis, polyneuritis, peripheral neuropathy, hepatitis, drowsiness, fatigability, impotence, headache, acneiform eruptions, allergic dermatitis, metallic or garlic-like aftertaste | Alcohol, metronidazole (Flagyl), or paraldehyde use; psychosis; cardiovascular disease | Initiate only after patient has abstained from alcohol for at least 12 hours Patient should carry an identification card describing the disulfiram-alcohol interaction; liver function should be monitored for hepatotoxicity Pregnancy category C, safety unknown in breastfeeding |
| Fluoxetine (Prozac) | No | Begin with 20 mg per day; may increase to 60 to 80 mg per day | Ejaculatory dysfunction, nausea, headache, insomnia, nervousness, somnolence, anxiety, diarrhea, anorexia, dry mouth, tremor, asthenia, sweating, dyspepsia, influenza-like illness, serotonin syndrome FDA warning§ | Use of an MAOI such as mesoridazine (Serentil), thioridazine, or linezolid (Zyvox) | Recommended only in patients with comorbid depression Pregnancy category C, safety unknown in breastfeeding |
| Gabapentin (Neurontin) | No | Variable Studies have used 300 mg twice per day or once-daily dosages up to 1,800 mg at bedtime Could begin with 300 mg per day on the first day, then 300 mg twice per day on the second day and 300 mg three times per day on the third day; may increase to maximum dosage of 1,800 mg per day | Dizziness, somnolence, fatigue, peripheral edema, hostility, diarrhea, asthenia, infection, dry mouth, nystagmus, constipation, nausea, vomiting, ataxia, fever, amblyopia | None | Use lower dose if patient has renal impairment (creatinine clearance < 60 mL per minute per 1.73 m2 [1.00 mL per second per m2]) Decreases levels of hydrocodone in a dose-dependent manner Decreased bioavailability with aluminum hydroxide/magnesium hydroxide Opioids may increase levels of gabapentin Pregnancy category C, limited data that it is safe in breastfeeding |
| Naltrexone (Revia [oral], Vivitrol [injectable])‡ | Yes | Oral: 50 to 100 mg per day (alternative dosing: 50 mg every weekday with a 100-mg dose on Saturday, 100 mg every other day, or 150 mg every third day) Injectable: 380 mg once every four weeks | Nausea, vomiting, headache, dizziness, nervousness, fatigue, low energy, insomnia, anxiety, difficulty sleeping, abdominal pain or cramps, joint or muscle pain | Opioid use, acute opioid withdrawal, acute hepatitis, liver failure | Liver function tests should be performed to monitor for hepatotoxicity Pregnancy category C, safety unknown in breastfeeding |
| Ondansetron (Zofran) | No | 4 mcg per kg twice per day (higher dosages may be used); available in 4-mg, 8-mg, 16-mg, and 24-mg oral doses | Malaise, fatigue, headache, dizziness, anxiety, serotonin syndrome; QT interval prolongation and torsades de pointes have been reported | Apomorphine use | Patients with electrolyte abnormalities should be monitored with electrocardiography Should be avoided in patients with congenital long QT syndrome Pregnancy category B, safety unknown in breastfeeding |
| Sertraline (Zoloft) | No | Begin with 50 mg per day; may increase to 200 mg per day | Ejaculatory dysfunction, dry mouth, sweating, somnolence, fatigue, tremor, anorexia, dizziness, headache, diarrhea, dyspepsia, nausea, constipation, agitation, insomnia, serotonin syndrome FDA warning§ | Use of an MAOI such as mesoridazine, thioridazine, or linezolid | May be helpful in patients with comorbid depression when prescribed in conjunction with naltrexone Pregnancy category C, safe in breastfeeding |
| Topiramate (Topamax) | No | Begin with 25-mg dose; increase to a total of 300 mg given twice per day in divided doses Renal impairment (creatinine clearance < 60 mL per minute per 1.73 m2 [1.17 mL per second per m2]): one-half of usual dosage | Hyperchloremic, nonanion gap, metabolic acidosis; acute myopia associated with secondary angle-closure glaucoma has been reported Anorexia, anxiety, diarrhea, fatigue, fever, infection, weight loss, cognitive problems, paresthesia, somnolence, taste perversion, mood problems, nausea, nervousness, confusion | None | Serum bicarbonate and blood ammonia levels should be monitored Pregnancy category D, safety unknown in breastfeeding |
Footnotes:
*—Other than hypersensitivity to the drug, which is a possible contraindication for all medications listed.
‡—Good evidence to support use in patients with alcohol use disorder.
§—Antidepressants increased the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder and other psychiatric disorders.
Abbreviations: FDA = U.S. Food and Drug Administration; MAOI = monoamine oxidase inhibitor.
[Source 98 ]Behavioral therapies
Another name for behavioral therapies for alcohol use disorder is alcohol counseling. It involves working with a health care professional to identify and help change the behaviors that lead to your heavy drinking.
- Cognitive-behavioral therapy (CBT) helps you identify the feelings and situations that can lead to heavy drinking. It teaches you coping skills, including how to manage stress and how to change the thoughts that cause you to want to drink. You may get CBT one-on-one with a therapist or in small groups.
- Motivational enhancement therapy helps you build and strengthen the motivation to change your drinking behavior. It includes about four sessions over a short period of time. The therapy starts with identifying the pros and cons of seeking treatment. Then you and your therapist work on forming a plan for making changes in your drinking. The next sessions focus on building up your confidence and developing the skills you need to be able to stick to the plan.
- Marital and family counseling includes spouses and other family members. It can help to repair and improve your family relationships. Studies show that strong family support through family therapy may help you to stay away from drinking.
- Brief interventions are short, one-on-one or small-group counseling sessions. It includes one to four sessions. The counselor gives you information about your drinking pattern and potential risks. The counselor works with you to set goals and provide ideas that may help you make a change.
Lifestyle choices
As part of your recovery, you’ll need to focus on changing your habits and making different lifestyle choices. These strategies may help.
- Consider your social situation. Make it clear to your friends and family that you’re not drinking alcohol. Develop a support system of friends and family who can support your recovery. You may need to distance yourself from friends and social situations that impair your recovery.
- Develop healthy habits. For example, good sleep, regular physical activity, managing stress more effectively and eating well all can make it easier for you to recover from alcohol use disorder.
- Do things that don’t involve alcohol. You may find that many of your activities involve drinking. Replace them with hobbies or activities that are not centered around alcohol.
Alternative medicine
Avoid replacing conventional medical treatment or psychotherapy with alternative medicine. But if used in addition to your treatment plan when recovering from alcohol use disorder, these techniques may be helpful:
- Yoga. Yoga’s series of postures and controlled breathing exercises may help you relax and manage stress.
- Meditation. During meditation, you focus your attention and eliminate the stream of jumbled thoughts that may be crowding your mind and causing stress.
- Acupuncture. With acupuncture, hair-thin needles are inserted under the skin. Acupuncture may help reduce anxiety and depression.
Alcohol use disorder prognosis
For most people, treatment for an alcohol use disorder is helpful. But overcoming an alcohol use disorder is an ongoing process, and you may relapse (start drinking again). You should look at relapse as a temporary setback, and keep trying. Many people repeatedly try to cut back or quit drinking, have a setback, then try to quit again. Having a relapse does not mean that you cannot recover. If you do relapse, it is important to return to treatment right away, so you can learn more about your relapse triggers and improve your coping skills. This may help you be more successful the next time.
Alcohol withdrawal syndrome
Alcohol withdrawal syndrome is a collection of withdrawal symptoms that may occur when a person who has been drinking too much alcohol on a regular basis suddenly stops or greatly reduced drinking alcohol 99. Approximately 50% of individuals with alcohol use disorder who abruptly stop or reduce their alcohol use will develop signs or symptoms of alcohol withdrawal syndrome 100. Alcohol use disorder is diagnosed in individuals who drink excessively and whose functioning (social, psychological, physical) is at least moderately impacted by their drinking. Alcohol withdrawal syndrome can occur within 6–24 hours to four or five days after the abrupt discontinuation or decrease of alcohol consumption. Alcohol withdrawal syndrome signs and symptoms include sweating, rapid heartbeat, hand tremors, problems sleeping (insomnia), nausea and vomiting, hallucinations, restlessness and agitation, anxiety, and occasionally seizures 101. Alcohol withdrawal syndrome is a potentially life-threatening condition whose severity ranges from mild/moderate forms characterized by tremors, nausea, anxiety, and depression, to severe forms characterized by hallucinations, seizures, delirium tremens and coma 102. If untreated or inadequately treated, alcohol withdrawal can progress to generalized tonic-clonic seizures, delirium tremens, and death 103.
Your alcohol withdrawal symptoms will be at their worst for the first 48 hours. Alcohol withdrawal symptoms can be severe enough to impair your ability to function at work or in social situations. You’ll also find your sleep is disturbed. You may wake up several times during the night or have problems getting to sleep. This is to be expected, and your sleep patterns should return to normal within a month. Your alcohol withdrawal symptoms should gradually start to improve as your body begins to adjust to being without alcohol. This usually takes 3 to 7 days from the time of your last drink. Alcohol withdrawal symptoms are relieved immediately by consuming additional alcohol 104. However, if you’re dependent on alcohol to function, it’s recommended you seek medical advice to manage your alcohol withdrawal syndrome. Furthermore, you’ll need further treatment and support to help you in the long term. People who have gone through alcohol withdrawal syndrome before are more likely to have symptoms each time they quit drinking. You may also have more severe alcohol withdrawal symptoms if you have certain other medical problems.
Alcohol withdrawal syndrome represents a continuous spectrum of symptoms ranging from mild withdrawal symptoms to delirium tremens (DT). Signs and symptoms of alcohol withdrawal syndrome, divided by stage 105, 99:
- Stage 1 – Minor alcohol withdrawal symptoms: Symptoms include anxiety, nausea, and vomiting. It occurs around 8 hours after the last drink of alcohol.
- Stage 2 – Alcoholic hallucinosis: Here there may be hallucinations (visual [zoopsy], auditory [voices] and tactile [paresthesia]) and hypertension 106. Symptoms occur within 12 to 24 hours after the last drink.
- Stage 3 – Alcohol withdrawal with seizures: Generalized tonic-clonic seizures (with short or no postictal period). It usually occurs 24 to 48 hours after the last drink.
- Stage 4 – Delirium tremens: Delirium tremens is an acute episode of sudden confusion (delirium) caused by alcohol withdrawal and is the most severe form of alcohol withdrawal syndrome, potentially leading to intensive care unit (ICU) admission or death 107. Delirium tremens can cause confusion (delirium), panic, hallucinations (seeing, hearing, or feeling things that aren’t real), psychosis, hyperthermia, malignant hypertension, seizures and coma. Some studies estimate that 3% to 5% of hospitalized patients with alcohol withdrawal syndrome progress to delirium tremens 108. Delirium tremens usually occurs 48 to 72 hours after the last drink. Delirium tremens may lead to death in about 5%–10% of the cases, if not managed properly 109.
Common alcohol withdrawal symptoms include:
- Anxiety or nervousness
- Depression
- Fatigue
- Irritability
- Jumpiness or shakiness
- Mood swings
- Nightmares
- Not thinking clearly
Other alcohol withdrawal symptoms may include:
- Sweating, clammy skin
- Enlarged (dilated) pupils
- Headache
- Insomnia (sleeping difficulty)
- Loss of appetite
- Nausea and vomiting
- Pallor
- Rapid heart rate
- Sweating, clammy skin
- Tremor of the hands or other body parts
A severe form of alcohol withdrawal called delirium tremens can cause:
- Agitation
- Fever
- Seeing or feeling things that aren’t there (hallucinations)
- Seizures
- Severe confusion
Alcohol withdrawal syndrome occurs most often in adults. Chronic alcoholism and withdrawal are more common in men than in women 110. But, alcohol withdrawal syndrome may also occur in teenagers or children. The more you drink regularly, the more likely you are to develop alcohol withdrawal syndrome when you stop drinking.
The withdrawal response after discontinuation of a particular drug or alcohol can depend on the duration and quantity of use 111. When people consume alcohol for at least 1 to 3 months or even consume large quantities for at least seven to ten days, the withdrawal response can occur within 6 to 24 hours after cessation of alcohol 112.
About 20% of adults in the emergency room may suffer from alcohol use disorder 110 and about 4-40% of patients admitted to ICU will have alcohol withdrawal syndrome 113. Patients who have alcohol withdrawal syndrome have an increased length of hospital stay and increased mortality than those who do not have alcohol withdrawal syndrome 114.
Talk to your doctor if you think you are going through alcohol withdrawal. It does not matter if your symptoms are mild or severe. The doctor needs to know your problem and if you have had it before. They will treat and manage your alcohol withdrawal symptoms to make sure they don’t lead to other health problems. If you go through alcohol withdrawal more than once and don’t receive treatment, your symptoms can get worse each time.
Treatment for alcohol withdrawal using benzodiazepines and any other medicinal combinations should always be under the supervision of a board-certified physician or psychiatrist. You should never try to withdraw from alcohol using benzodiazepines on your own.
Your doctor will help you manage your alcohol withdrawal symptoms to prevent more serious health problems. Your doctor may prescribe medicine to treat your symptoms. Medicines can help control shakiness, anxiety, and confusion. It can help to take these medicines early on in your withdrawal period. They can keep symptoms from getting worse or lasting as long.
Some people may be prescribed medication to help achieve alcohol abstinence. It’s likely the medication will make you feel drowsy. Only take your medication as directed. Benzodiazepines administration represents the “gold-standard” for the management of any grade of alcohol withdrawal syndrome, including seizures and delirium tremens. In particular, the European Federation of Neurological Societies recommends the use of benzodiazepines for the primary prevention and for the treatment of alcohol withdrawal syndrome-related seizures. The drugs of choice are lorazepam and diazepam. Although lorazepam has some pharmacological advantages to diazepam, the differences are minor and, because i.v. lorazepam is largely unavailable in Europe, diazepam is recommended. Other drugs for detoxification should only be considered as add-on treatments 115. Despite its primary indication as anticonvulsivant drug, phenytoin has been shown to be ineffective in the secondary prevention of alcohol withdrawal seizures in placebo-controlled trials 116. Thus its use should be avoided.
Other medicines used with benzodiazepines or in place of them include 117:
- Acamprosate – Acamprosate is an FDA-approved medication for alcoholism that reduces cravings. Acamprosate can be used with counseling to help readjust the brain to prevent you from drinking.
- Anticonvulsants – Certain anticonvulsants help regulate brain activity during medical detox.
- Opioid antagonists – Opioid antagonists are used to help those detoxing from opioid misuse.
- Barbiturates – Barbiturates work similarly to benzodiazepines and may be used when benzodiazepines are contraindicated.
- Beta-blockers – Beta-blockers are sometimes used for acute anxiety or sleep issues and may be used in place of benzodiazepines.
- GABA agonists – GABA agonists are typically prescribed to assist with sleep issues and seizures.
- Antipsychotics – In low doses, some antipsychotics may be useful in medical detox.
- Naltrexone (two brand names: Revia or Vivitrol) reduces cravings and blocks the alcohol “high.”
- Disulfiram (brand name: Antabuse) creates an unpleasant effect even when you consume only a small amount of alcohol.
- Nutritional therapy may also be part of medical detox and addiction treatment. For example, lack of thiamine, or vitamin B1, leads to cognitive impairments. Because many people with alcohol use disorder are vitamin B1 deficient, replacing it is crucial 118
People who have severe withdrawal often need to go to the hospital. They may need fluids to prevent or treat dehydration. They may need medicines to treat the alcohol withdrawal syndrome symptoms. These often are given through an IV. Your doctor can tell you what level of testing or treatment you need. After the treatment of acute alcohol withdrawal syndrome, some symptoms can persist from weeks to months following the 5–7 days of acute detoxification period, representing the “protracted alcohol withdrawal syndrome” 102.
You must not drive if you’re taking medication to help ease your alcohol withdrawal symptoms. You should also get advice about operating heavy machinery at work. You need to tell the DMV if you have an alcohol problem – failure to do so could result in a fine.
Detox can be a stressful time. Ways you can try to relieve stress include reading, listening to music, going for a walk, and taking a bath. During detox, make sure you drink plenty of fluids (about 3 liters a day). However, avoid drinking large amounts of caffeinated drinks, including tea and coffee, because they can make your sleep problems worse and cause feelings of anxiety. Water, squash or fruit juice are better choices.
Try to eat regular meals, even if you’re not feeling hungry. Your appetite will return gradually.
Your urge to drink again during alcohol withdrawal can be very strong. Support from family and friends can help you resist that urge. It’s important to avoid any triggers or situations that may make you want alcohol. This could mean avoiding certain places or people. You may also choose to attend self-help groups, receive extended counseling or use a talking therapy such as cognitive behavioral therapy (CBT). After withdrawal symptoms go away, you may need more treatment. You can join a support group or sobriety program, such as Alcoholics Anonymous (https://www.aa.org).
If you’re detoxing at home, you’ll regularly see a nurse or another healthcare professional. This might be at home, your family physician or an alcohol withdrawal specialist service. You’ll also be given the relevant contact details for other support group or sobriety program such as National Institute on Alcohol Abuse and Alcoholism (https://www.niaaa.nih.gov) or Al-Anon Family Groups/Al-Anon/Alateen (https://al-anon.org) should you need additional support. These programs can help prevent relapse.
Alcohol withdrawal syndrome symptoms
Alcohol withdrawal syndrome symptoms usually occur within 8 hours after your last drink, but can occur days later. In its mild-to-moderate forms, alcohol withdrawal syndrome symptoms such as increase in blood pressure and pulse rate, tremors, overactive reflexes, irritability, and anxiety usually develop within 6 to 24 hours after your last drink and may subside within few days 119. Alcohol withdrawal syndrome symptoms usually peak by 24 to 72 hours, but may go on for weeks. You’ll also find your sleep is disturbed. You may wake up several times during the night or have problems getting to sleep. This is to be expected, and your sleep patterns should return to normal within a month.
The types of symptoms experienced in alcohol withdrawal syndrome are broken down into three components: autonomic, motor, and psychiatric.
Autonomic symptoms are responses of the nervous system and include 120:
- Rapid heart rate
- Rapid breathing
- Dilated or larger than normal pupils
- Elevated blood pressure
- Elevated body temperature
- Diarrhea
- Nausea/vomiting
Motor symptoms are responses of the body’s nervous and muscular systems and include:
- Hand and body tremors
- Ataxia (impaired speech, balance, or coordination when not intoxicated)
- Changes in a person’s gait
- Hyper responsive reflexes
- Seizures
Psychological symptoms are changes to a person’s mood and perceptual experiences. These symptoms include:
- Paranoia
- Delusions (a fixed, false belief)
- Hallucinations (seeing, hearing, or feeling things that aren’t there)
- Mood instability
- Combativeness
- Agitation
- Disorientation
- Delirium
- Insomnia
Alcohol withdrawal syndrome represents a continuous spectrum of symptoms ranging from mild withdrawal symptoms to delirium tremens (DT). Alcohol withdrawal syndrome can start with mild symptoms and then evolve to more severe forms, or can start with delirium tremens, in particular in those patients with previous history of delirium tremens or with history of repeated alcohol withdrawal syndrome (kindling phenomenon) 100. Usually, 1st degree alcohol withdrawal syndrome symptoms (tremors, diaphoresis, nausea/vomiting, hypertension, tachycardia, hyperthermia, tachypnea) begin 6–12 hours after the last alcohol consumption, lasting until the next drink 121. In co-morbid patients taking other medications such as beta-blockers, significant changes in vital signs (blood pressure and heart rate) can be masked and appear normal. The 2nd degree alcohol withdrawal syndrome symptoms are characterized by visual and tactile disturbances and generally start 24 hours after the last drink. Almost 25% of alcohol withdrawal syndrome patients show transient alterations of perception such as auditory (voices) 122 or less frequently, visual (zooscopies) or tactile disturbances 121. They may be persecutory and cause paranoia, leading to increased patient agitation 123. When these symptoms become persistent, the patient has progressed to alcoholic hallucinosis. However, the patient recognizes the hallucinations as unreal, as dysperceptions, and maintains a clear sensorium 121.
Almost 10% of patients showing withdrawal symptoms develops alcohol withdrawal seizures (3rd degree alcohol withdrawal syndrome), generally starting after 24–48 hours from the last drink and characterized by diffuse, tonic-clonic seizures usually with little or no postictal period 124. Even if self-limiting in the majority of cases, seizures can be difficult to treat and almost in one-third of patients, delirium tremens may represent a clinical worsening of alcohol withdrawal seizures 125.
Delirium tremens represents the most severe manifestation (4th degree) of alcohol withdrawal syndrome, as the result of no treatment or undertreatment of alcohol withdrawal syndrome and occurrs approximately in 5% of patients with alcohol withdrawal syndrome 102. Usually it appears 48–72 hours after the last drink, although it could begin up to 10 days later. Symptoms last normally 5–7 days 126. Delirium tremens is characterized by a rapid fluctuation of consciousness and change in cognition occurring over a short period of time, accompanied by severe autonomic symptoms (sweating, nausea, palpitations and tremor) and psychological symptoms (i.e. anxiety). The typical delirium tremens patient shows agitation, hallucinations and disorientation. The presence of disorientation differentiates delirium from alcoholic hallucinosis 127. Delirium, psychosis, hallucinations, hyperthermia, malignant hypertension, seizures and coma are common manifestations of delirium tremens. Delirium tremens could be responsible of injury to patient or to staff, or of medical complications (aspiration pneumonia, arrhythmia or myocardial infarction), which may lead to death in 1–5% of patients 128.
After the treatment of acute alcohol withdrawal syndrome, some symptoms can persist from weeks to months following the 5–7 days of acute detoxification period, representing the “protracted alcohol withdrawal syndrome” 102.
Alcohol withdrawal syndrome complications
Complications that can accompany alcohol withdrawal syndrome include 129:
- Delirium tremens
- Seizures
- Wernicke-Korsakoff syndrome
- Anxiety
- Depression
- Sleep disturbances
- Hallucinations
- Cardiovascular complications
A variety of clinical conditions could be associated with alcohol withdrawal syndrome both as complication of the disease or of the treatment 102. In particular, infectious (i.e. pneumonia and sepsis) and neurological (Wernicke’s encephalopathy) complications could be associated with immune and nutritional deficits related to alcohol use disorder or can be the direct consequence of the mechanical ventilation and/or ICU stay due to respiratory depression 130. On this connection physicians should be aware of these risks in order to start an adequate treatment.
Moreover, it should be underlined that severe medical illnesses (i.e. pneumonia, coronary heart disease, alcohol liver disease and anaemia) have been reported to precipitate alcohol withdrawal syndrome and to increase the risk of severe alcohol withdrawal syndrome 128. In these patients a prophylactic treatment could be useful, regardless of the clinical institute withdrawal assessment for alcohol (CIWA) score.
Risk factors for severe alcohol withdrawal syndrome
Risk factors for severe alcohol withdrawal syndrome include 131, 105:
- Previous episodes of alcohol withdrawal (detoxification, rehabilitation, seizures, delirium tremens
- Concomitant use of CNS-depressant agents, such as benzodiazepine or barbiturates
- Concomitant use of other illicit substances
- High blood alcohol level (BAL) on admission (i.e. >200 mg/dl)
- Evidence of increased autonomic activity (i.e. systolic blood pressure > 150 mmHg, body temperature > 38°C)
- Older age
- Moderate to severe alcohol withdrawal at diagnosis (Clinical Institute Withdrawal Assessment for Alcohol – revised > 10)
- Medical or surgical illness (i.e. trauma, infection, liver disease, central nervous system (CNS) infection, electrolyte disturbances, hypoglycemia, etc.)
- Severe alcohol dependence
- Abnormal liver function (elevated aspartate aminotransferase [AST])
- Recent alcohol intoxication
- Male sex
Alcohol withdrawal syndrome prevention
Reduce or avoid alcohol. If you have a drinking problem, you should stop alcohol completely. Total and lifelong avoidance of alcohol (abstinence) is the safest approach.
Alcohol withdrawal syndrome diagnosis
When alcohol is consumed in large quantities for a prolonged period (greater than two weeks) and then abruptly discontinued, withdrawal symptoms are likely to occur. Symptoms of alcohol withdrawal syndrome begin six to 24 hours after the last alcohol intake. Alcohol withdrawal affects the central nervous system, autonomic nervous system, and cognitive function 132. Patients have acute alcohol withdrawal syndrome if two of the following symptoms are present after the reduction or discontinuation of alcohol use 133: autonomic hyperactivity (sweating, tachycardia); increased hand tremor; insomnia; nausea or vomiting; transient visual, tactile, auditory hallucinations or illusions; psychomotor agitation; anxiety; or tonic-clonic seizures. If acute alcohol withdrawal syndrome is not treated or is undertreated, delirium tremens can occur. This condition is a severe hyperadrenergic state (i.e., hyperthermia, diaphoresis, tachypnea, tachycardia) characterized by disorientation, impaired attention and consciousness, and visual and/or auditory hallucinations 132.
Alcohol withdrawal syndrome diagnosis depends on the severity of the patient’s condition 134. The severity of acute alcohol withdrawal syndrome can be classified into three stages 135.
- Stage 1 symptoms are mild and not usually associated with abnormal vital signs.
- Stage 2 symptoms are more intense and associated with abnormal vital signs (e.g., elevated blood pressure, respiration, and body temperature).
- Stage 3 includes delirium tremens or seizures. Progression to stage 2 or 3 can occur quickly without treatment.
Your health care provider will perform a physical exam. This may reveal:
- Abnormal eye movements
- Abnormal heart rhythms
- Dehydration (not enough fluids in the body)
- Fever
- Rapid breathing
- Rapid heart rate
- Shaky hands
Blood and urine tests, including a toxicology screen, may be done. Tests to be considered include:
- Glucose – liver disease due to alcoholism may reduce glycogen stores, and ethanol impairs gluconeogenesis. As a consequence, patients in alcohol withdrawal develop anxiety, agitation, tremor, seizures, and diaphoresis, all of which can occur with hypoglycemia.
- Arterial blood gas (ABG) – mixed acid-base disorders are common and often result from alcoholic ketoacidosis, volume-contraction alkalosis, and respiratory alkalosis.
- Complete blood count (CBC) – long-term alcohol ingestion causes myelosuppression (bone marrow suppression resulting in reduced production of red blood cells, white blood cells, and platelets), thrombocytopenia (low blood platelet count) and anemia (lack of red blood cells). Megaloblastic anemia occurs with dietary deficiency of vitamin B-12 and folate; increased mean corpuscular volume (MCV) suggests this condition
- Metabolic panel – look for acidosis, dehydration, concurrent renal disease, and other abnormalities that can occur in chronic alcoholism. Calculate anion and delta gaps, which are helpful in differentiating mixed acid-base disorders. A low blood urea nitrogen (BUN) value is expected in alcoholic liver disease. Expect an elevated lipase level if pancreatitis is suspected. Obtain the blood ammonia level if hepatic encephalopathy is suspected.
- Magnesium, calcium, and liver function tests (LFTs) – may be indicated because patients with chronic alcoholism usually have a dietary magnesium deficiency and concurrent alcoholic hepatitis. Alcoholic pancreatitis may cause hypocalcemia.
- Urinalysis – check for ketones, as patients may have associated alcoholic ketoacidosis. Ketonuria without glycosuria to exclude alcoholic ketoacidosis and the ingestion of isopropyl alcohol. Myoglobinuria from rhabdomyolysis may be suspected when hematuria is noted on urinalysis.
- Cardiac markers – elevated creatine kinase (CK) and cardiac troponin levels may indicate myocardial infarction. Elevated CK level may be from rhabdomyolysis, which may be associated with adrenergic hyperactivity from alcohol withdrawal or myonecrosis if immobile.
- Prothrombin time (PT) – useful index of liver function; patients with cirrhosis are at risk for coagulopathy.
- Toxicology screening – consider measuring serum osmolality and screening for toxic alcohols if severely acidaemic. Other recreational drugs may be present as well.
- Imaging studies – chest radiography to evaluate for aspiration pneumonia, cardiomyopathy, and chronic heart failure.
- Head computed tomography (CT) – risk for intracranial bleeding because of cortical atrophy and coagulopathy.
- Electrocardiography (ECG) – a prolonged QTc interval has been described in patients with an alcohol withdrawal syndrome.
- Lumbar puncture – to rule out meningitis or subarachnoid hemorrhage.
- Blood cultures may also be indicated if sepsis or endocarditis is suspected.
Alcohol withdrawal syndrome DSM-5 diagnostic criteria
According to the American Psychiatric Association Diagnostic and Statistical Manual of mental disorders (DSM-5) criteria, the diagnosis of alcohol withdrawal syndrome is based on the observation of signs and symptoms of withdrawal in those patients who experienced an abrupt reduction or cessation of alcohol consumption 127. DSM-5 requires the observation of at least two of the following symptoms: autonomic hyperactivity (sweating or tachycardia); increased hand tremor; insomnia; nausea or vomiting; transient visual, tactile or auditory hallucinations or illusions; psychomotor agitation; anxiety; and tonic–clonic seizures 127.
DSM-5 Diagnostic Criteria for Alcohol Withdrawal Syndrome 127:
- A. Cessation of (or reduction in) alcohol use that has been heavy and prolonged.
- B. Two (or more) of the following, developing within several hours to a few days after criterion A:
- Autonomic hyperactivity (e.g., sweating or pulse rate greater than 100 beats per minute)
- Increased hand tremor
- Insomnia
- Nausea or vomiting
- Transient visual, tactile, or auditory hallucination s or illusions
- Psychomotor agitation
- Anxiety
- Generalized tonic-clonic seizures
- C. The symptoms in criterion B cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- D. The symptoms are not due to a general medical condition and are not better accounted for by another mental disorder.
- Specify if: With perceptual disturbances: This specifier applies in the rare instance when hallucinations (usually visual or tactile) occur with intact reality testing, or auditory, visual, or tactile illusions occur in the absence of a delirium.
- When hallucinations occur in the absence of delirium (i.e., in a clear sensorium), a diagnosis of substance/medication-induced psychotic disorder should be considered.
Diagnostic features
The essential feature of alcohol withdrawal is the presence of a characteristic withdrawal syndrome that develops within several hours to a few days after the cessation of (or reduction in) heavy and prolonged alcohol use (Criteria A and B). The withdrawal syndrome includes two or more of the symptoms reflecting autonomic hyperactivity and anxiety listed in Criterion B, along with gastrointestinal symptoms.
Withdrawal symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning (Criterion C). The symptoms must not be attributable to another medical condition and are not better explained by another mental disorder (e.g., generalized anxiety disorder), including intoxication or withdrawal from another substance (e.g., sedative, hypnotic, or anxiolytic withdrawal) (Criterion D).
Symptoms can be relieved by administering alcohol or benzodiazepines (e.g., diazepam). The withdrawal symptoms typically begin when blood concentrations of alcohol decline sharply (i.e., within 4-12 hours) after alcohol use has been stopped or reduced. Reflecting the relatively fast metabolism of alcohol, symptoms of alcohol withdrawal usually peak in intensity during the second day of abstinence and are likely to improve markedly by the fourth or fifth day. Following acute withdrawal, however, symptoms of anxiety, insomnia, and autonomic dysfunction may persist for up to 3-6 months at lower levels of intensity.
Fewer than 10% of individuals who develop alcohol withdrawal will ever develop dramatic symptoms (e.g., severe autonomic hyperactivity, tremors, alcohol withdrawal delirium). Tonic-clonic seizures occur in fewer than 3% of individuals.
Associated features supporting diagnosis
Although confusion and changes in consciousness are not core criteria for alcohol withdrawal, alcohol withdrawal delirium may occur in the context of withdrawal. As is true for any agitated, confused state, regardless of the cause, in addition to a disturbance of consciousness and cognition, withdrawal delirium can include visual, tactile, or (rarely) auditory hallucinations (delirium tremens). When alcohol withdrawal delirium develops, it is likely that a clinically relevant medical condition may be present (e.g., liver failure, pneumonia, gastrointestinal bleeding, sequelae of head trauma, hypoglycemia, an electrolyte imbalance, postoperative status).
Alcohol withdrawal syndrome severity assessment
In clinical practice, physicians have the need to predict the probability of a patient to develop severe alcohol withdrawal syndrome. In particular, in those patients in whom a complete medical history is not available (i.e. emergency department, trauma unit, ICU), a high risk of complicated alcohol withdrawal syndrome could orientate the medical decision toward a more aggressive treatment, despite presenting symptoms.
Validated instruments used to assess acute alcohol withdrawal syndrome severity include the Alcohol Withdrawal Scale (Table 1), the revised 10-item form of the Clinical Institute Withdrawal Assessment for Alcohol (Table 2), Luebeck Alcohol withdrawal Risk Scale (LARS) (Table 4) or the recently proposed PAWSS (Prediction of Alcohol Withdrawal Severity Scale) (Table 5) 100. The self-completed, 10-item Short Alcohol Withdrawal Scale (SAWS) (Table 3) has been validated in the outpatient setting 136. Outpatient treatment is appropriate in patients with mild or moderate alcohol withdrawal syndrome, if there are no contraindications. Patients who have not had alcohol in at least five days may also receive outpatient treatment.
The Alcohol Withdrawal Scale (Table 1) and the revised 10-item form of the Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) scale have emerged as a useful tool to assess alcohol withdrawal syndrome severity, even in those patients presenting with severe withdrawal and delirium, without requiring the patient’s participation 137, 138.
The Alcohol Withdrawal Scale (Table 1) was developed in order to provide an assessment of alcohol withdrawal syndrome, even in those patients presenting with severe withdrawal and delirium, without requiring the patient’s participation 139. In this connection, “hallucinations” and “contact” items were included for a better identification of delirium tremens 139. This scale consists of 2 subscales (S subscale: pulse rate, diastolic blood pressure, temperature, breathing rate, sweating, tremor; M subscale: agitation, contact, orientation, hallucination, anxiety) allowing a separate assessment of somatic and mental withdrawal symptoms. Mild alcohol withdrawal syndrome is identified by a total score ≤5; moderate alcohol withdrawal syndrome scores 6–9; severe alcohol withdrawal syndrome results in a score ≥10 (Table 1).
The Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) scale requires limited patient cooperation to evaluate its ten symptoms (Table 2). The Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) Scores of less than 8 indicate mild withdrawal, scores of 8–15 indicate moderate withdrawal (marked autonomic arousal) and scores of greater than 15 points indicate severe withdrawal and are also predictive of the development of seizures and delirium 140. If Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score is <8–10 pharmacological treatment is not necessary, while it may be appropriate in those patients scoring between 8 and 15, to prevent the progression to more severe forms of alcohol withdrawal syndrome (see table 3). Pharmacological treatment is strongly indicated in patients with Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score >15. The evaluation of Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score should be repeated at least every 8 hours. In patients with scores >8–10 or requiring treatment, Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) should be repeated every hour to evaluate the response to treatments. In using the CIWA-Ar, the clinical picture should be considered because medical and psychiatric conditions may mimic alcohol withdrawal symptoms. In addition, certain medications (e.g., beta blockers) may blunt the manifestation of these symptoms.
The initial LARS (Luebeck Alcohol withdrawal Risk Scale) scale (Table 3) applied to the patients consists of 22 items compiled in 4 subscores:
- LARS 1: history of alcohol use (detoxification and withdrawal complications) and abuse of sedatives;
- LARS 2: drinking habits and possible alcohol use complications during the past 4 weeks; in this subscale some items assumed to indicate bad physical condition prior to detoxification (malnutrition, sleep disturbances, etc.) were included;
- LARS 3: clinical symptoms at clinical investigation;
- LARS 4: laboratory values of serum electrolytes at admission.
Table 2. Alcohol-Withdrawal Scale
| Alcohol-withdrawal Scale | ||||||
|---|---|---|---|---|---|---|
| Score | ||||||
| Subscale S – somatic symptoms | 0 | 1 | 2 | 3 | 4 | 5 |
| Pulse rate (per min) | <100 | 101–110 | 111–120 | >120 | ||
| Diastolic blood pressure (mmHg) | <95 | 96–100 | 101–105 | >105 | ||
| Temperature (°C) | <37.0 | 37.0–37.5 | 37.6–38.0 | >38.0 | ||
| Breathing (per min) | <20 | 20–24 | >24 | n.a. | ||
| Sweating | None | Mild (wet hands) | Moderate (forehead) | Severe (profuse) | ||
| Tremor | None | mild (arms raised + fingers spread | moderate (fingers spread) | severe (spontaneous) | ||
| Subscale M – mental symptoms | 0 | 1 | 2 | 3 | 4 | 5 |
| Agitation | none | fastening | rolling in bed | try to leave bed | in rage | |
| Contact | short talk possible | easily distractable (i.e. noise) | drifting contact | dialogue impossible | ||
| Orientation (time, place. person, situation) | fully aware | one kind (i.e. time) | two kinds disturbed | totally confused | ||
| Hallucinations (visual, acoustic and tactile) | none | suggestive | one kind (i.e. visual) | two kinds (visual + tactile) | all kinds | visual hallucinations (as in a film) |
| Anxiety | None | mild (only if asked) | severe (spontaneous complaint) | |||
Table 3. Clinical Institute Withdrawal Assessment for Alcohol – revised (CIWA-Ar) scale
Footnote: Tool to assess the severity of alcohol withdrawal. Absent or very mild ≤ 8 points; mild = 9 to 14 points; moderate = 15 to 20 points; severe > 20 points. Those with a score < 10 do not usually need additional medication.
[Source 141 ]Table 4. Short Alcohol Withdrawal Scale (SAWS)
Footnote: Tool to assess the severity of alcohol withdrawal. Patients indicate how they have felt in the previous 24 hours. Mild withdrawal < 12 points; moderate to severe withdrawal ≥ 12 points.
[Source 142 ]Table 5. Luebeck Alcohol withdrawal Risk Scale (LARS)
| Item |
|---|
| LARS 1 |
| Previous inpatient detoxifications (2–5 = 2; 6–10 = 3, ≥11 = 4) |
| Previous outpatient detoxifications (2–5 = 2; 6–10 = 3, ≥11 = 4) |
| Previous withdrawal delirium (≥3 = 3) |
| Previous withdrawal seizures (≥3 = 3) |
| Use of hypnotics during last 2 weeks |
| LARS 2 |
| Daily consumption of alcoholic beverages during last 4 weeks |
| Pattern of steady drinking |
| Frequent sleep disturbances during the last week |
| Nightmares during the last week |
| Malnutrition during last week |
| Multiple vomiting during last week |
| LARS 3 |
| Blood alcohol content (BAC) ° 1 g/l |
| Tremor (despite of BAC ≥1 g/l) |
| Sweating (despite of BAC ≥1 g/l) |
| Pulse rate ≥100/min (despite of BAC ≥1 g/l) |
| Seizure prior or at admission |
| Polyneuropathy |
| Ataxia |
| LARS 4 |
| Sodium (<136 mmol/l) |
| Potassium ( <3.6 mmol/l) |
| Calcium (<2.2 mmol/l) |
| Chloride (<96 mmol/l) |
Footnote: BAC = blood alcohol content
[Source 143 ]Table 6. Prediction of Alcohol Withdrawal Severity Scale (PAWSS)
Footnote: AWS = alcohol withdrawal syndrome
[Source 144 ]Alcohol withdrawal syndrome treatments
Patients in alcohol withdrawal may have numerous potentially life-threatening medical problems 112. Alcohol withdrawal syndrome is a cause of severe discomfort to patients, symptoms are disabling and patients who experienced withdrawal, often are afraid to stop drinking for fear of developing withdrawal symptoms again.
Alcohol withdrawal syndrome treatment goal includes:
- Reducing withdrawal symptoms
- Prevent seizures, delirium tremens, and death
- Preventing complications of alcohol use
- Therapy to get you to stop drinking (abstinence from alcohol use)
Treatment goals for patients with alcohol withdrawal syndrome are to minimize the severity of symptoms in order to prevent the more severe manifestations such as seizure, delirium and death and to improve the patient’s quality of life 102. Alcohol withdrawal seizures can occur 24 to 72 hours after the last alcohol intake, are typically tonic-clonic, and last less than five minutes. Up to one-third of patients with alcohol withdrawal syndrome who have a related seizure will progress to delirium tremens 145. Moreover an effective treatment of alcohol withdrawal syndrome should be followed by efforts in increasing patient motivation to maintain long-term alcohol abstinence and facilitate the entry into a relapse prevention program 102.
Patients suffering from mild to moderate alcohol withdrawal syndrome can be managed as outpatients while more severe forms should be monitored and treated in an inpatient setting. The availability of an Alcohol Addiction Unit is of help in the clinical evaluation, management, and treatment of alcohol withdrawal syndrome patients, with a reduction in hospitalization costs. Patients can be managed principally as outpatients and transferred to the inpatient unit only when the clinical situation requires 146. Because alcohol withdrawal syndrome symptoms increase with external stimulation, patients should be treated in a quiet environment. Patients with mild alcohol withdrawal syndrome may only require supportive care 147. Psychological treatment does not reduce the risk of seizures or delirium tremens. Most patients with alcohol withdrawal syndrome are prescribed medication, particularly if there is any question about duration of abstinence.
Prophylactic and routine use of thiamine to prevent Wernicke’s encephalopathy:
- Prophylactic thiamine administration is recommended as soon as possible and prior to any carbohydrate load (e.g. intravenous glucose), as glucose intake in the presence of thiamine deficiency can precipitate Wernicke’s encephalopathy. Thiamine should initially be given parentally, as oral thiamine is poorly absorbed through the gastro-intestinal mucosa in people who drink alcohol.
- Administer thiamine 300mg IV per day (diluted in saline over 30 minutes) for 3 days then change to oral 100mg three time per day with meals for at least 5-7 days. Patients with chronic poor nutrition may benefit from extended periods of oral thiamine doses following discharge.
- In the event that the patient presents to hospital but inpatient admission for longer than 2 days is unlikely (e.g. emergency room presentation or 24-48 hour admission), then higher thiamine
doses (e.g. 300mg IV twice a day) may be administered to ensure adequate thiamine dosing. - In the event of poor intravenous access that prevents the recommended regimen, alternative approaches to thiamine dosing should be used. This may include:
- a single intravenous (e.g. 300mg) and high oral doses (e.g. 500mg three time per day) for three days
- once daily intramuscular (e.g. 100mg) dose and high oral doses (e.g. 500mg three time per day) for three days
NOTE: If there is a clinical suspicion of Wernicke’s encephalopathy (e.g. one sign such as confusion, or ataxia or eye signs; or a history of poor nutrition), then consider treating with high dose parenteral thiamine (500mg IV three time per day) as though a diagnosis of Wernicke’s encephalopathy is confirmed.
Figure 3. Alcohol withdrawal syndrome guidelines
Footnote: Richmond Agitation-Sedation Scale (RASS) is a medical scale used to measure the agitation or sedation level of a person 148.
Footnote: The refractory alcohol withdrawal syndrome pathway outlines a suggested strategy for those patients in whom adequate control cannot be obtained despite diazepam 200mg and phenobarbital 390mg. In these patients the overall goal is to avoid intubation unless absolutely necessary. The suggested non-benzodiazepine adjunct in this scenario is ketamine, which is more strongly supported by evidence..
INPATIENT TREATMENT
People with moderate-to-severe symptoms of alcohol withdrawal may need inpatient treatment at a hospital or other facility that treats alcohol withdrawal. You will be watched closely for hallucinations and other signs of delirium tremens.
Treatment may include:
- Monitoring of blood pressure, body temperature, heart rate, and blood levels of different chemicals in the body
- Fluids or medicines given through a vein (by IV)
- Sedation using medicines until withdrawal is complete
Administration of intravenous (IV) glucose to patients with seizures is controversial because this is thought to precipitate acute Wernicke encephalopathy in chronic alcoholism unless thiamine (vitamin B1) is also administered. A benzodiazepine can be administered to control seizures. If the patient has hypoglycemia, dextrose 50% in water (D50W) 25 mL to 50 mL and thiamine (vitamin B1) 100 mg intravenously (IV) is also indicated. Low doses of clonidine can help reverse central adrenergic discharge, relieving tachypnea (rapid breathing), tachycardia (fast heart beat), hypertension (high blood pressure), tremor, and craving for alcohol. In an agitated patient, neuroleptics such as haloperidol 5 mg IV or intramuscularly (IM) may be added to sedative-hypnotic agents as an adjunctive therapy. Caution must be taken because haloperidol may decrease the seizure threshold as well as prolong the QT interval.
OUTPATIENT TREATMENT
Outpatient detoxification is an effective, safe, and low-cost treatment for patients with mild to moderate symptoms of alcohol withdrawal syndrome and may allow for less interruption of work and family life 149, 150. During this process, you will need someone who can stay with and keep an eye on you. It is important that caregivers be comfortable with this responsibility 151. Family support can be critical to the success of outpatient treatment. However, family dysfunction or home triggers for alcohol consumption make success unlikely.
You will likely need to make daily visits to your doctor until you are stable. However, patients with serious psychiatric problems (e.g., suicidal ideation, psychosis) or medical conditions should be treated in an inpatient setting 152. Although routine laboratory tests are unnecessary for patients with mild alcohol withdrawal syndrome, significant laboratory abnormalities (e.g., complete blood count, liver function, glucose, or electrolyte testing) would exclude outpatient treatment. Patients with positive results on a urine drug screen, which signifies concurrent drug abuse, should be treated as inpatients. Outpatient treatment requires that the patient be able to take oral medications; is committed to frequent follow-up visits; and has a relative, friend, or other caregiver who can stay with the patient and administer medication 153.
Treatment usually includes:
- Sedative drugs to help ease withdrawal symptoms
- Blood tests
- Patient and family counseling to discuss the long-term issue of alcoholism
- Testing and treatment for other medical problems linked to alcohol use
It is important to go to a living situation that helps support you in staying sober. Some areas have housing options that provide a supportive environment for those trying to stay sober.
Permanent and life-long abstinence from alcohol is the best treatment for those who have gone through alcohol withdrawal.
Contraindications to outpatient treatment of alcohol withdrawal syndrome
- Coexisting acute or chronic illness requiring inpatient treatment
- Current severe alcohol withdrawal, especially with delirium
- High risk of delirium tremens
- No possibility for follow-up
- No reliable contact person to monitor the patient
- Absence of a support network
- Pregnancy
- Long-term intake of large amounts of alcohol
- Seizure disorder or history of severe alcohol withdrawal seizures
- Suicide risk
- Poorly controlled chronic medical conditions (e.g., diabetes mellitus, chronic obstructive pulmonary disease, congestive heart failure)
Relative contraindications
- Coexisting benzodiazepine dependence
- History of unsuccessful outpatient detoxification
- High risk for severe alcohol withdrawal or delirium tremens 154
- Age > 40 years
- Heavy drinking > 8 years
- Drinking > 100 g of ethanol daily (e.g., about one pint of liquor or eight 12-oz cans of beer)
- Symptoms and signs of withdrawal when not drinking
- Random blood alcohol concentration (BAC) > 200 mg per dL
- Elevated mean corpuscular volume
- Elevated blood urea nitrogen (BUN)
- Cirrhosis
Alcoholic hallucinosis treatment
Alcoholic hallucinosis is a rare complication of chronic alcohol abuse characterized by predominantly auditory hallucinations that occur either during or after a period of heavy alcohol consumption 106. Although this condition had been noted for centuries, its classification status is not yet clear 155. Bleuler (1916) termed the condition as alcohol hallucinosis and differentiated it from delirium tremens 155. International Classification of Diseases-10 (ICD-10) relabeled it as Alcohol induced Psychotic Disorder, Predominantly hallucinatory type 156. Usually alcoholic hallucinosis presents with acoustic verbal hallucinations, delusions and mood disturbances arising in clear consciousness and sometimes may progress to a chronic form mimicking schizophrenia.
The pathophysiology of alcohol-related psychosis is unclear. Several hypotheses exist. Some studies suggest that an increase in central dopaminergic activity and dopamine receptor alterations may be associated with hallucinations in patients with alcohol use disorder 157. However, serotonin may also be involved. Other studies imply that amino acid abnormalities may lead to decreased brain serotonin and increased dopamine activity leading to hallucinations. Elevated levels of beta-carbolines and an impaired auditory system have also been associated with alcohol-related psychosis. Neuro-imaging studies have suggested that perfusion abnormalities to various regions in the brain may be associated with the hallucinations in alcohol dependence 158.
Alcoholic hallucinosis treatment is to stabilize the patient paying close attention to airway, breathing and vital signs. If the patient requires sedation due to alcohol-related psychosis, neuroleptics, such as haloperidol, have been considered the first-line medications for treatment 157. Benzodiazepines, such as lorazepam, are used if there is a concern for alcohol withdrawal and seizures. Certain atypical antipsychotics, such as ziprasidone and olanzpine, have also been used to help sedate patients with acute psychosis. Some patients may require the use of physical restraints to protect the patient as well as the staff. Patients with alcohol-related psychosis must also be evaluated for suicidality since it is associated with higher rates of suicidal behaviors. The prognosis for alcohol-related psychosis is less favorable than earlier studies had speculated. However, if the patient can abstain from alcohol, the prognosis is good. If patients are unable to abstain from alcohol, the risk of recurrence is high 159.
Alcohol withdrawal syndrome supportive therapy
Alcohol withdrawal syndrome supportive therapy is the first-line approach and, sometimes, the only approach required. It includes frequent reassurance, reality orientation, and nursing care 160. A quiet room without dark shadows, noises, and other excessive stimuli (i.e. bright lights) is recommended 161.
Routine examination should include blood (or breath) alcohol concentration, complete blood count, renal function tests, electrolytes, glucose, liver enzymes, urinalysis and urine toxicology screening. General supportive care should correct fluid depletion, hypoglycemia and electrolytes disturbances, and should include hydration and vitamin supplementation. In particular, thiamine supplementation and B-complex vitamins (including folates) are essential for the prevention of Wernicke’s encephalopathy 162. Thiamine can be given routinely in these patients given the absence of significant adverse effects or contraindications 161. Moreover, since the administration of glucose can precipitate or worsen Wernicke’s encephalopathy, thiamine should be administered before any glucose infusion 163. Finally, with the exception of patients with cardiac arrhythmias, electrolytes disturbances or previous history of alcohol withdrawal syndrome-related seizures, there is no evidence to support the routine administration of magnesium during alcohol withdrawal syndrome 164.
Alcohol withdrawal syndrome medication
Because patients with alcohol withdrawal syndrome are often nutritionally depleted, thiamine (100 mg daily) and folic acid (1 mg daily) should be used routinely. Thiamine supplementation lowers the risk of Wernicke encephalopathy, which is characterized by oculomotor dysfunction, abnormal mentation, and ataxia.
The treatment of alcohol withdrawal syndrome requires the use of a long-acting drug as a substitutive agent to be gradually tapered off 165. The ideal drug for alcohol withdrawal syndrome should have a rapid onset and a long duration of action in reducing withdrawal symptoms and a relatively simple metabolism, not depending on liver function. It should not interact with alcohol, should suppress the “drinking behavior” without producing cognitive and/or motor impairment and it should not have a potential for abuse 166.
At present benzodiazepines represent the “gold-standard” in the treatment of alcohol withdrawal syndrome (Table 6 and 7) 167. The choice of benzodiazepine in the management of alcohol withdrawal syndrome may be influenced by rapid onset of action for quick agitation control, longer duration of action to lessen potential wearing off and breakthrough symptoms, or shorter duration of action to lessen prolonged sedation in elderly patients or those with compromised hepatic function 168. When given for alcohol withdrawal syndrome, benzodiazepines may be prescribed as either a fixed or symptom-triggered dosing regimen. Studies have shown that symptom-triggered treatment results in a decreased cumulative dose of benzodiazepines and decreased duration of treatment compared with fixed-dose regimens 169. Alternative medications that have been studied for the treatment of acute alcohol withdrawal include valproic acid, carbamazepine, phenobarbital, gabapentin, clonidine, propofol, antipsychotics, dexmedetomidine, and ketamine 114, 170, 171. In particular, phenobarbital, propofol, dexmedetomidine, and ketamine have been investigated extensively as adjuncts to benzodiazepine therapy for benzodiazepine-refractory alcohol withdrawal syndrome in the ICU setting 172, 173, 170.
In severe cases of alcohol withdrawal syndrome or delirium tremens, barbiturates are sometimes prescribed in addition to benzodiazepines. Barbiturates are stronger than benzodiazepines and carry significant risks of extreme sedation, they are normally delivered in intensive care units with close medical monitoring.
Baclofin and gamma‐hydroxybutyric acid (GHB) and sodium oxylate are also sometimes administered during detoxification from alcohol 174.
Medications like dexmedetomidine may be used only in addition to other medications to reduce symptoms like severe agitation, anxiety, and dangerously high blood pressure 174.
When you have completed medically-supervised detox, other medications may be introduced to reduce cravings for alcohol and prevent relapse. The two most effective and commonly prescribed medications are:
- Acamprosate
- Naltrexone: has the unique benefit of reducing the euphoric feelings that accompany alcohol when consumed. It does this by blocking opioid receptors in the brain which contribute to alcohol’s pleasure-causing effects 175.
Other medications that are sometimes used to treat alcoholism are:
- Disulfiram: Antabuse medication that has been approved to treat alcoholism since 1949 176. It blocks the enzyme responsible for metabolizing a toxic component of alcohol. The result is a cluster of undesirable effects (e.g. nausea, vomiting, flushing) that occur when alcohol is consumed.
- Gabapentin and Topiramate: Anti-seizure medications that are prescribed off-label for alcoholism. Both medications are thought to reduce cravings 175.
Table 7. Oral medications used to treat alcohol withdrawal syndrome
| Medication | Typical single dose | Common adverse effects | Contraindications |
|---|---|---|---|
| Benzodiazepines | |||
| Chlordiazepoxide (Librium) | 25 to 50 mg | Sedation, fatigue, respiratory depression, retrograde amnesia, ataxia, dependence and abuse | Hypersensitivity to drug/class ingredient, severe hepatic impairment, avoid abrupt withdrawal |
| Diazepam (Valium) | 10 mg | ||
| Lorazepam (Ativan) | 2 mg | ||
| Oxazepam | 15 to 30 mg | ||
| Anticonvulsants | |||
| Carbamazepine (Tegretol) | 600 to 800 mg | Dizziness, ataxia, diplopia, nausea, vomiting | Hypersensitivity to drug/class ingredient, hypersensitivity to tricyclic antidepressants, monoamine oxidase inhibitor use within the previous 14 days, hepatic porphyria |
| Gabapentin (Neurontin) | 300 to 600 mg | ||
| Oxcarbazepine (Trileptal) | 450 to 900 mg | ||
| Valproic acid (Depakene) | 1,000 to 1,200 mg | ||
| Beta blocker | |||
| Atenolol (Tenormin) | Pulse 50 to 79 beats per minute: 50 mg | Bradycardia, hypotension, fatigue, dizziness, cold extremities, depression | Hypersensitivity to drug/class ingredient, second- or third-degree atrioventricular block, uncompensated heart failure, cardiogenic shock, sick sinus syndrome without implantable cardioverter-defibrillator, untreated pheochromocytoma |
| Pulse ≥ 80 beats per minute: 100 mg | |||
| Alpha-adrenergic agonist | |||
| Clonidine (Catapres) | 0.2 mg | Hypotension, dry mouth, dizziness, constipation, sedation | Hypersensitivity to drug/class ingredient |
Footnote: These medications should not be stop suddenly.
[Source 177 ]Benzodiazepines
At present benzodiazepines represent the “gold-standard” in the treatment of alcohol withdrawal syndrome (Table 7) 167. Furthermore, benzodiazepines represent the only class of medications with proven efficacy in preventing the development of complicated forms of alcohol withdrawal syndrome, with a reduction in the incidence of seizures (84%), delirium tremens and the associated risk of mortality 178. However, the use of benzodiazepines is associated with increased risk of excessive sedation, motor and memory deficits and respiratory depression, and these effects are more pronounced in patients with liver impairment 167. Moreover the risk of abuse and dependence 179 limits benzodiazepine use in alcohol dependent patients 167.
In the United States, the only benzodiazepines that are approved by the Food and Drug Administration (FDA) for the treatment of alcohol withdrawal syndrome are chlordiazepoxide and diazepam; however, other benzodiazepines are often used because no single agent has proven superior to the others 180. While in Europe, clomethiazole is also widely used 167. The efficacy of benzodiazepines in the treatment of alcohol withdrawal syndrome seems to be mediated by their stimulation of GABAA receptors with alcohol mimicking effects 165.
Certain people make better candidates than others to treat alcohol withdrawal symptoms with benzodiazepines. Those who can benefit the most are those who 181:
- Have a diagnosable anxiety disorder, such as panic disorder or social anxiety, that would interfere with their ability to participate in recovery treatment
- Have trouble falling asleep or staying asleep or not sleeping for long periods
- Have withdrawal symptoms such as agitation, insomnia, tremors, seizures, or convulsions
- Have post-traumatic stress disorder (PTSD) symptoms
No study has shown a clear superiority of any agent over the others. The greater evidence exists for the long-acting agents (chlordiazepoxide and diazepam) 182, given their ability to produce a smoother withdrawal 105. The clinical effect is mediated by the drug (benzodiazepine) per se, and by its active metabolites produced by phase 1 liver oxidation. Subsequently all products of oxidative metabolism are inactivated by phase 2 liver glucuronidation and excreted 183. However, in patients with reduced liver metabolism, such as in the elderly or in those with advanced liver disease, the use of short-acting agents may be preferred in order to prevent excessive sedation and respiratory depression 178. In these cases, oxazepam and lorazepam represent the drugs of choice due to the absence of oxidative metabolism and active metabolites (see Table 7) 184.
The possibility of multiple administration routes (oral, intramuscular [I.M.], or intravenous [I.V.]) represents an advantage of benzodiazepines. The intravenous (IV) route should be preferred for moderate to severe alcohol withdrawal syndrome because of the rapid onset of action, while the oral route can be used in the milder forms. Chlorodiazepoxide and diazepam should not be administered intramuscular (IM) due to their erratic absorption; lorazepam can be administered by all three routes; oxazepam can be administered only orally, while midazolam can be given intravenously as continuous infusion 105.
A “fixed-dose”, rather than a “loading dose” or a “symptoms-triggered” regimen can be adopted for the management of alcohol withdrawal syndrome (Table 7).
- Fixed-Dose Treatment Regimen
- Medical staff breaks the total dose into four smaller amounts with fixed-dose treatments. For example, if a doctor prescribed 40 mg benzodiazepines a day, the doses are given in 10 mg doses four times a day (i.e. diazepam 10 mg four times per day for 1 day, then 5 mg four times per day for 2 days, then tapering off; alternatively chlordiazepoxide 50–100 mg four times per day for 1 day, then 25–50 mg four times per day for 2 days, with subsequent tapering off). With the fixed-dose approach, the chosen drug is given at regular intervals (independently from patient’s symptoms), tapering off the dose by 25% per day from day 4 to day 7. Additional doses can be administered if symptoms are not adequately controlled. This approach is highly effective and could be preferred in those patients at risk for severe alcohol withdrawal syndrome, or in those patients with history of seizures or delirium tremens. However patients should be monitored for the risk of excessive sedation and respiratory depression 182.
- This regimen is helpful in outpatient or inpatient treatment settings 185.
- Loading-Dose Treatment Regimen
- Loading-dose regimens involve doctors administering a moderate-to-high dose of a long-acting benzodiazepine (i.e. diazepam 10–20 mg or chlordiazepoxide 100 mg, every 1–2 hours) in two-hour intervals in order to produce sedation; successively, drug levels will decrease (auto-taper) through metabolism. The risk of benzodiazepine toxicity is high during the early phase of the treatment and the patient requires a strict clinical monitoring to prevent benzodiazepine toxicity. However, this approach seems to produce the shorter treatment course secondary to the progressive auto-tapering of drug levels and to reduce the incidence of severe alcohol withdrawal syndrome promoting recovery from alcohol withdrawal syndrome 182..
- Close monitoring by medical staff includes checking the severity level of withdrawal symptoms. This regimen works best in an inpatient environment.
- Symptom-Triggered Treatment Regimen
- The last scheme, symptom-triggered, is based on the administration of the chosen drug (diazepam 5–20 mg, chlordiazepoxide 50–100 mg or lorazepam 2–4 mg) if the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score is >8–10. Symptom severity is measured hourly. The dose is adjusted (i.e. from 5 to 10 mg of diazepam) according to the severity of the symptoms and can be repeated every hour until the CIWA-Ar score decreases to <8 165. The use of the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score seems to be useful and effective in the dose-adjustment of the drug.
- Monitoring trigger symptoms of alcohol withdrawal should take place in an inpatient medical detox. As triggers occur, medical staff administer benzodiazepines. This method can decrease a person’s time in medical detox.
- However, if someone has a history of seizures or other complications of medical detox, this regimen is considered too high-risk for potential seizure activity 185.
Trials comparing different alcohol withdrawal syndrome treatment strategies did not find clear evidence of the superiority for one of these regimens 186. However, the symptom-triggered regimen has been shown to reduce total benzodiazepine consumption and treatment duration with respect to fixed-dose in patients at low risk for complicated alcohol withdrawal syndrome 187.
From a practical point of view, in an inpatients setting in which an intensive care unit (ICU) is rapidly available the front-loading scheme could be safely chosen. On the contrary, if ICU is not available but a strict clinical observation is possible, symptom-triggered regimen could be preferred in order to reach the clinical effect with the minimum benzodiazepine administration. The fixed-dose treatment represents the recommended regimen in those patients at risk for complicated alcohol withdrawal syndrome, with history of seizures or delirium tremens (in whom drugs should be administered regardless of the symptoms) 105.
Treatment of delirium tremens requires the use of benzodiazepines as primary drugs, with the possible use of neuroleptics to control psychosis and dysperceptions.
Table 8. Benzodiazepines used to treat alcohol withdrawal syndrome
| DRUG | HALF-LIFE | ACTIVE METABOLITES | METABOLISM | EXCRETION |
|---|---|---|---|---|
| Diazepam | 20–80 hours (metabolites 30- 100 hours) | Yes | Hepatic | Hepatic – urinary (metabolites) |
| Chlordiazepoxide | 5–30 hours (metabolites 30- 200 hours) | Yes | Hepatic | Hepatic – urinary (metabolites) |
| Lorazepam | 10–20 hours | No | Hepatic | Urinary, fecal |
| Oxazepam | 10–20 hours | No | Hepatic | Urinary |
| Midazolam | 2–6 hours | Yes | Hepatic, Gut | Urinary |
Table 9. Fixed and Symptom-Triggered Benzodiazepine dosing for oral alcohol withdrawal medications
| Medication | Fixed schedule | Symptom-triggered schedule* |
|---|---|---|
| Day 1 | ||
| Diazepam (Valium) | 10 mg every 6 hours | 10 mg every 4 hours |
| Chlordiazepoxide (Librium) | 25 to 50 mg every 6 hours | 25 to 50 mg every 4 hours |
| Lorazepam (Ativan) | 2 mg every 8 hours | 2 mg every 6 hours |
| Day 2 | ||
| Diazepam | 10 mg every 8 hours | 10 mg every 6 hours |
| Chlordiazepoxide | 25 to 50 mg every 8 hours | 25 to 50 mg every 6 hours |
| Lorazepam | 2 mg every 8 hours | 2 mg every 6 hours |
| Day 3 | ||
| Diazepam | 10 mg every 12 hours | 10 mg every 6 hours |
| Chlordiazepoxide | 25 to 50 mg every 12 hours | 25 to 50 mg every 6 hours |
| Lorazepam | 1 mg every 8 hours | 1 mg every 8 hours |
| Day 4 | ||
| Diazepam | 10 mg at bedtime | 10 mg every 12 hours |
| Chlordiazepoxide | 25 to 50 mg at bedtime | 25 to 50 mg every 12 hours |
| Lorazepam | 1 mg every 12 hours | 1 mg every 12 hours |
| Day 5 | ||
| Diazepam | 10 mg at bedtime | 10 mg every 12 hours |
| Chlordiazepoxide | 25 to 50 mg at bedtime | 25 to 50 mg every 6 hours |
| Lorazepam | 1 mg at bedtime | 1 mg every 12 hours |
Footnote: *For patients with a SAWS (Short Alcohol Withdrawal Scale) score ≥ 12, or CIWA-Ar (Clinical Institute Withdrawal Assessment for Alcohol, Revised) score > 9.
[Source 177 ]Benzodiazepines side effects
All drugs, including benzodiazepines, have the potential for adverse effects. Some who are taking the medication for alcoholism will not have any side effects. Many factors other than the drug play a role in how it reacts with the body. A few examples are allergies, underlying medical conditions, and interactions with other medicines.
Some of the most common side effects of benzodiazepines include 188:
- Breathing issues
- Drowsiness
- Disorientation
- Impaired motor skills
- Drop in blood pressure that may cause a loss of consciousness
- Digestive problems
There are contraindications or times when taking benzodiazepines could result in dangerous or toxic reactions. For example, during pregnancy taking benzodiazepines could lead to congenital malformations 188.
More severe, yet rare, side effects can occur with benzodiazepine toxicity. Complications can lead to 189:
- Food, saliva, liquids, or vomit is breathed into the lungs rather than into the stomach, also called aspiration pneumonia
- Respiratory arrest
- A breakdown of muscle tissue that leaks proteins that can damage kidneys into the blood is also called rhabdomyolysis.
Fortunately, there is a medicine that can reverse the adverse effects of benzodiazepines, flumazenil if toxicity or overdose occurs 189.
Who should not take benzodiazepines for alcohol withdrawal?
Warnings for doctors regarding benzodiazepines as alcohol withdrawal medication include considering other medication for patients who 190:
- Are pregnant or breastfeeding
- Are allergic to any of the ingredients of the medicine
- Are taking other central nervous system depressants, including illicit use
- Have respiratory illness or disease
- Have certain medical problems such as liver or kidney disease
- Have a nervous system disorder
- Have severe depression or suicidal ideation
- Are elderly
Benzodiazepines are also contraindicated for anyone taking them for another condition or taking other medication for alcoholism.
Barbiturates and propofol
The use of barbiturates in the treatment of alcohol withdrawal syndrome has been limited given their narrow therapeutic window, the risk of excessive sedation and the interference with the clearance of many drugs 161. However, in the setting of ICU, in those patients requiring high doses of benzodiazepines to control alcohol withdrawal syndrome symptoms or developing delirium tremens, barbiturates maintain a specific indication. The combination of phenobarbital with benzodiazepines promotes benzodiazepine binding to the GABAA receptor, possibly increasing the efficacy of the benzodiazepine action 191. In patients affected by severe delirium tremens requiring mechanical ventilation, the combination of benzodiazepines and barbiturates produces both a decrease in the need of mechanical ventilation and a trend towards a decrease in ICU length of stay 171.
Propofol enhances the inhibitory effects at the GABAA receptor and decreases excitatory circuits of the NMDA transmitter system. Due to its strong lipophilic properties, it features a rapid onset of action and is easy to titrate because of the short half‐life that allows a rapid evaluation of patient’s mental status after discontinuation 192. Propofol has general anesthetic effects that often require intubation and mechanical ventilation. Its use is therefore restricted to the intensive care unit (ICU) making this agent an adjunct therapy for refractory cases of alcohol withdrawal syndrome 193, 194. These characteristics make propofol a useful therapeutic option in patients with severe delirium tremens, who are poorly controlled with high doses of benzodiazepines 195. However, the use of this drug requires clinical monitoring, endotracheal intubation and mechanical ventilation. In the setting of ICU, in those patients requiring sedation and mechanical ventilation, the Sedation-Agitation Scale (SAS) or the Richmond Agitation-Sedation Scale (RASS) can be used to titrate sedation 171. Its application and experience in alcohol withdrawal syndrome is limited to only a few cases and rebound of withdrawal symptoms soon after stopping propofol infusion has been reported 185.
Alpha2-agonists, beta-blockers and neuroleptics
These classes of medications have been tested and are currently used as adjunctive treatment for alcohol withdrawal syndrome. However, the lack of efficacy in preventing severe alcohol withdrawal syndrome and the risk of masking alcohol withdrawal syndrome symptoms make these drugs not recommended as monotherapy. They should be used only as adjunctive treatment, in patients with co-existing comorbidities, and to control neuro-autonomic manifestations of alcohol withdrawal syndrome when not adequately controlled by benzodiazepines administration.
The administration of these drugs as monotherapy could mask alcohol withdrawal syndrome symptoms and reduce the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) scores with a consequent reduction of the prescription of benzodiazepines and possible risk to develop complicated alcohol withdrawal syndrome.
Beta-blockers (e.g. atenolol) could be used to treat hyperarousal symptoms in patients with coronary artery disease 99. However, given their effect on tremors, tachycardia and hypertension, these drugs could mask alcohol withdrawal syndrome symptoms and should be considered only in conjunction with benzodiazepines in patients with persistent hypertension or tachycardia 167.
The use of alpha2-agonists could have a role in the management of alcohol withdrawal syndrome. Parenteral administration of clonidine may be associated with sedation and other side effects, while low doses of clonidine (oral, transdermal) may have a role in the control of alcohol withdrawal syndrome symptoms via a reduction of autonomic hyperactivity (hypertension and tachycardia) 196. The use of dexmedetomidine, a more selective alfa2-receptor agonist, showed interesting results in controlling sympathetic symptoms with less sedation than clonidine as adjunctive drug to lorazepam for severe alcohol withdrawal syndrome, and with a possible benzodiazepine-sparing effect. However, bradycardia was a commonly observed side-effect. Moreover, these results require further investigations and validation 197.
Neuroleptics (i.e., haloperidol) are generally used for the management of hallucinosis and delirium. However, given their lack of effect in preventing the worsening of alcohol withdrawal syndrome, their facilitating effect on the development of seizures and the risk of QT prolongation, the use of neuroleptic agents as monotherapy is contraindicated. Moreover they are associated with a longer duration of delirium, higher complication rate and higher mortality 168. The use of neuroleptics should be reserved as adjunctive treatment in the case of agitation, perceptual disturbances, or disturbed thinking not adequately controlled by benzodiazepines 167.
Carbamazepine
Carbamazepine is a tricyclic anticonvulsant able to produce a GABAergic effect and to block NMDA receptors 198. It has been shown to be an effective drug in the treatment of alcohol withdrawal syndrome, at least in mild to moderate forms, producing an effect superior to placebo and non-inferior to benzodiazepines 198. The proposed treatment scheme is 600–800 mg/day on day 1, tapered down to 200 mg over 5 days 199. A reduction of alcohol relapse has also been showed in the post-alcohol withdrawal syndrome phase 200. However, side effects associated with long-term administration (i.e. nausea, vomiting, dermatitis, Steven-Johnson syndrome, agranulocitosis) could limit its extensive use. Moreover, given its drug-drug interaction potential, this drug may be difficult to manage in patients with in patients with multiple comorbidities and treated with other medications 201. Oxcarbazepine (900 mg for 3 days, 450 mg for 4th day, 150 mg for 5th day), a metabolite of carbamazepine, due to the only weak induction of Cytochrome P450 and the kidney excretion, could represent a valid alternative to carbamazepine 102. However its role in alcohol withdrawal syndrome remains to be completely demonstrated.
Valproate
Valproic acid (400–500 mg three times per day) is able to produce a dose-dependent improvement of alcohol withdrawal syndrome symptoms 202, with a reduced incidence of seizures and a protection toward the worsening of alcohol withdrawal syndrome severity (anti-kindling effect). These characteristics make valproic acid an interesting and promising drug in the outpatient management of mild-to-moderate forms of alcohol withdrawal syndrome 177. The most commonly observed side-effects were gastrointestinal distress, tremor and sedation 203. The possible increase of liver enzymes (transaminases) could limit its use in alcohol dependent patients with liver impairment.
Sodium oxybate
Sodium oxybate also called gamma-hydroxybutyric acid is a short-chain fatty acid that occurs naturally in mammalian brain, in particular in the thalamus, hypothalamus and basal ganglia. Sodium oxybate is structurally similar to the inhibitory neurotransmitter GABA, binding to sodium oxybate and GABAB receptors with high and low affinity, respectively 204. Given sodium oxybate’s alcohol-mimicking effects on central nervous system (CNS) 205, this drug was tested in preclinical and clinical setting for the treatment of alcohol withdrawal syndrome 206. The efficacy of repeated doses of Sodium Oxybate (50 mg/kg/day in three divided doses) has been shown in comparative studies versus benzodiazepines 207 and versus clomethiazole 208. In almost all studies of sodium oxybate in patients with alcohol withdrawal syndrome in different clinical setting, the primary efficacy endpoint was the decrease of the the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score and/or the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) subscores 141. A meta-analysis performed in 2010 by The Cochrane Collaboration 209 showed that sodium oxybate (50 mg/kg/day) is more effective than placebo in reducing alcohol withdrawal syndrome symptoms score, with an efficacy equivalent to benzodiazepines and clomethiazole. No differences between the groups were observed for side effects and numbers of drop-outs between treatments 209. Recently the GATE 1 study, a phase IV, multicenter, multinational, randomized, active drug-controlled study (double-blind, double dummy), with parallel groups evidenced the efficacy of sodium oxybate and non-inferiority of Sodium Oxybate vs oxazepam in the treatment alcohol withdrawal syndrome 210. The efficacy and the safety of oral Sodium Oxybate in the long-term treatment of alcohol dependence, makes this drug useful in the treatment of both alcohol withdrawal syndrome and long-term treatment for alcohol relapse prevention 209.
Sodium oxybate has been approved in some European countries for the treatment of alcohol withdrawal syndrome and for relapse prevention and maintenance of abstinence. It is not approved for this indication in other countries, as its addictive properties limit its use 211. However, at therapeutic doses for the treatment of alcohol-dependent patients sodium oxybate abuse seems to be a relatively limited phenomenon 212. Future studies are needed to clarify these aspects.
Baclofen
Baclofen is a GABAB receptor agonist, currently used to control spasticity 213. Baclofen is able to reduce alcohol withdrawal syndrome by activating GABAB receptors that might offset alcohol withdrawal syndrome-associated enhanced function of NMDA receptors 214. Moreover baclofen is able to prevent the sensitization of withdrawal anxiety caused by repeated withdrawals 215.
A randomized single-blind study comparing baclofen (10 mg three time per day for 10 days) vs. diazepam (0.5–0.75 mg/kg/day for 6 consecutive days, tapering the dose by 25% daily from day 7 to day 10) in the treatment alcohol withdrawal syndrome did not find any significant differences between the two drugs in the Clinical Institute Withdrawal Assessment for Alcohol Revised (CIWA-Ar) score reductions 216. Moreover, the oral route administration gave the possibility of an outpatient treatment regimen, resulting in a significant reduction in the cost of treatment compared to inpatient alcohol withdrawal syndrome treatment 216.
A more recent double-blind placebo-controlled trial found that the use of baclofen was associated with a significant reduction in the use of ‘as-needed’ lorazepam in the management of alcohol withdrawal syndrome 217. Furthermore some clinical evidence suggests that the use baclofen could have a potential role in the prophylaxis of alcohol withdrawal syndrome in hospitalized patients at risk for alcohol withdrawal syndrome 218.
Baclofen seems to be an easily manageable drug, without significant side effects. At the prescribed doses, there have not been any reports of euphoria or other pleasant effects caused by the drug. Although these data are encouraging, further confirmatory studies are needed to establish the role of baclofen in alcohol withdrawal syndrome. Baclofen showed its efficacy in alcohol relapse prevention 219 suggesting that it could represent a promising drug in the treatment of both alcohol withdrawal syndrome and post-withdrawal 220. The lack of any significant side effect and of liver toxicity 221 makes it possible to use this drug for the treatment of alcohol use disorder patients affected by liver disease 222.
Gabapentin
Gabapentin is a medication structurally similar to GABA, approved for the adjunctive treatment of partial seizures. Its final effect seems to be an amplification of brain GABA synthesis 223. At present, data on the efficacy of gabapentin in the treatment of alcohol withdrawal syndrome are controversial. Preliminary clinical studies suggest the possible efficacy of gabapentin in the treatment of alcohol dependent patients affected by alcohol withdrawal syndrome (400 mg three times per day for 3 days, 400 mg twice per day for 1 day, then 400 mg for 1 day) 224. In a retrospective study analyzing both out- and inpatients treated with gabapentin, the drug seemed to be effective in the treatment of mild-to-moderate alcohol withdrawal syndrome, while it was less effective in severe alcohol withdrawal syndrome 225. In a randomized controlled trial, patients who started taking gabapentin after 3 days of abstinence had fewer heavy drinking days (defined as 5 or more drinks for men and 4 or more drinks for women) and greater rates of abstinence than those who received placebo 103. More recently the safety and effectiveness of gabapentin in the treatment of tonic–clonic seizures associated with alcohol withdrawal syndrome have been demonstrated 226. An open-label study conducted with 27 inpatients compared gabapentin to phenobarbital and demonstrated no difference between the two drugs 227. However, in a double-blind placebo-controlled trial, gabapentin was not more effective than placebo in the management of alcohol withdrawal syndrome 228. A possible explanation of this lack of effect could be the too low entry dose. Moreover, it has been speculated that gabapentin’s effects are at least partially related to its sedative effects, that could be useful in the treatment of the sleep disturbances typically present during alcohol withdrawal syndrome 229. In summary, further confirming data are required on the possible utility of gabapentin in alcohol withdrawal syndrome 230. If confirmed, also gabapentin would be an interesting option in the treatment of alcohol dependent patients, from alcohol withdrawal syndrome to alcohol relapse prevention 231.
Topiramate
Topiramate is an anticonvulsant with several mechanisms of action. In particular, topiramate produces an increase in GABAA receptor-mediated inhibitory activity and antagonizes alpha-amino-3-hydroxy-5-methylisoxazole-4-propionic acid (AMPA) and kainate glutamate receptors with a consequent reduction in dopamine release in the nucleus accumbens. It is able to modulate ionotropic channels, inhibiting L-type calcium channels, limiting the activity of voltage-dependent sodium channels and facilitating potassium conductance. All these effects are at the basis of topiramate’s ability to reduce the hyperactivity and resulting anxiety of alcohol withdrawal syndrome 232.
Open-label studies showed the efficacy of topiramate (50 mg twice per day or once a day) in reducing the incidence of alcohol withdrawal syndrome seizures 233 and symptoms 234. The ability of topiramate to produce an effect on multiple neurotransmitter systems represents the rationale for the use of topiramate in the treatment of alcohol withdrawal syndrome 235. Considering these preliminary data of topiramate in alcohol withdrawal syndrome, and its efficacy in promoting alcohol abstinence 236, topiramate too could represent an interesting pharmacological option for the treatment of alcohol use disorder from alcohol withdrawal syndrome to long-term detoxification 223.
Magnesium
Magnesium is an important cofactor of many enzymes and acts as an inhibitor of neurotransmitter release. Therefore, it may dampen the NMDA‐driven hyperexcitability in alcohol withdrawal syndrome by competing with glutamate in its receptor binding site. Furthermore, magnesium impedes the NO synthase and calcium‐dependent channels, lowering action potential firing 237. As chronic alcohol use is associated with abnormal magnesium metabolism, patients have been given magnesium to treat or prevent alcohol withdrawal syndrome 185. Based on a Cochrane review, there is currently insufficient evidence to support the routine use of magnesium for prophylaxis or treatment of alcohol withdrawal syndrome 164. Nevertheless, as alcohol use and withdrawal are connected with QT interval prolongation and cardiac arrhythmia, laboratory values of magnesium should be determined and deficiencies be balanced 238.
Thiamine
Wernicke’s encephalopathy is afflicted with high morbidity and mortality and presents only in rare cases with the classic triad of confusion, ataxia, and ophthalmoplegia 185. According to the European Federation of the Neurological Societies guideline for diagnosis of Wernicke’s encephalopathy, two of the following four signs are required: (i) dietary deficiencies, (ii) eye signs, (iii) cerebellar dysfunction, and (iv) either an altered mental state or mild memory impairment 239. Particularly in severe alcohol withdrawal syndrome with predominant symptoms of delirium tremens, differentiation from Wernicke’s encephalopathy is sometimes impossible. Because of its easy and uncomplicated treatment, prevention of Wernicke’s encephalopathy with parenteral thiamine should be performed in all patients at risk, including those experiencing alcohol withdrawal syndrome and prior to any parenteral carbohydrate‐containing fluids 240. The earlier thiamine supplementation is started, the faster is recovery, regardless of initial clinical presentation 241.
Alcohol withdrawal syndrome prognosis
How well a person does depends on the amount of organ damage and whether the person can stop drinking completely. Alcohol withdrawal may range from a mild and uncomfortable disorder to a serious, life-threatening condition. Symptoms such as sleep changes, rapid changes in mood, and fatigue may last for months. People who continue to drink a lot may develop health problems such as liver, heart, and nervous system disease.
Most people who go through alcohol withdrawal make a full recovery. But, death is possible, especially if delirium tremens occurs.
- Problem Drinking vs. Alcoholism. https://alcohol.org/alcoholism/or-is-it-just-a-problem[↩]
- Understanding Alcohol Use Disorder. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder[↩]
- Marshall, E. J. (2015), Griffith Edwards’ work on the life course of alcohol dependence. Addiction, 110, 12– 15. doi: 10.1111/add.12908[↩]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington: American Psychiatric Association; 2013[↩][↩]
- Effects of ethanol on ion channels. Crews FT, Morrow AL, Criswell H, Breese G. Int Rev Neurobiol. 1996; 39():283-367. https://www.ncbi.nlm.nih.gov/pubmed/8894851/[↩]
- Management of drug and alcohol withdrawal. Kosten TR, O’Connor PG. N Engl J Med. 2003 May 1; 348(18):1786-95. https://www.ncbi.nlm.nih.gov/pubmed/12724485/[↩]
- Mattson RH. Seizures associated with alcohol use and alcohol withdrawal. In: Feldman B, editor. Epilepsy:Diagnosis and Management. Boston: Little Brown; 1983. pp. 325–332.[↩]
- The Basics: Defining How Much Alcohol is Too Much. https://www.niaaa.nih.gov/health-professionals-communities/core-resource-on-alcohol/basics-defining-how-much-alcohol-too-much#pub-toc1[↩]
- GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018 Dec;5(12):987-1012. doi: 10.1016/S2215-0366(18)30337-7. Epub 2018 Nov 1. Erratum in: Lancet Psychiatry. 2019 Jan;6(1):e2.[↩][↩]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018 Sep 22;392(10152):1015-1035. doi: 10.1016/S0140-6736(18)31310-2. Epub 2018 Aug 23. Erratum in: Lancet. 2018 Sep 29;392(10153):1116. Erratum in: Lancet. 2019 Jun 22;393(10190):e44.[↩][↩]
- Alcohol. https://www.who.int/news-room/fact-sheets/detail/alcohol[↩]
- Global status report on alcohol and health 2018 [Internet]. Geneva: World Health Organization; 2018. https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf[↩]
- White AM, Castle IP, Powell PA, Hingson RW, Koob GF. Alcohol-Related Deaths During the COVID-19 Pandemic. JAMA. 2022;327(17):1704–1706. doi:10.1001/jama.2022.4308[↩]
- Pilar MR, Eyler AA, Moreland-Russell S, Brownson RC. Actual Causes of Death in Relation to Media, Policy, and Funding Attention: Examining Public Health Priorities. Front Public Health. 2020 Jul 7;8:279. doi: 10.3389/fpubh.2020.00279[↩]
- Centers for Disease Control and Prevention (CDC). Alcohol and Public Health: Alcohol-Related Disease Impact (ARDI). Annual Average for United States 2011–2015 Alcohol-Attributable Deaths Due to Excessive Alcohol Use, All Ages. https://nccd.cdc.gov/DPH_ARDI/Default/Default.aspx[↩]
- Esser MB, Sherk A, Liu Y, et al. Deaths and Years of Potential Life Lost From Excessive Alcohol Use — United States, 2011–2015. MMWR Morb Mortal Wkly Rep 2020;69:1428–1433. DOI: http://dx.doi.org/10.15585/mmwr.mm6939a6[↩]
- Rehm J, Gmel GE Sr, Gmel G, Hasan OSM, Imtiaz S, Popova S, Probst C, Roerecke M, Room R, Samokhvalov AV, Shield KD, Shuper PA. The relationship between different dimensions of alcohol use and the burden of disease-an update. Addiction. 2017 Jun;112(6):968-1001. doi: 10.1111/add.13757[↩]
- Cao Y, Willett WC, Rimm EB, Stampfer MJ, Giovannucci EL. Light to moderate intake of alcohol, drinking patterns, and risk of cancer: results from two prospective US cohort studies. BMJ. 2015 Aug 18;351:h4238. doi: 10.1136/bmj.h4238[↩]
- Freudenheim JL. Alcohol’s Effects on Breast Cancer in Women. Alcohol Res. 2020 Jun 18;40(2):11. doi: 10.35946/arcr.v40.2.11[↩]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs. 2016 Mar;77(2):185-98. doi: 10.15288/jsad.2016.77.185[↩]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018 Sep 22;392(10152):1015-1035. doi: 10.1016/S0140-6736(18)31310-2. Epub 2018 Aug 23. Erratum in: Lancet. 2018 Sep 29;392(10153):1116. Erratum in: Lancet. 2019 Jun 22;393(10190):e44[↩]
- Wood AM, Kaptoge S, Butterworth AS, et al. Emerging Risk Factors Collaboration/EPIC-CVD/UK Biobank Alcohol Study Group. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet. 2018 Apr 14;391(10129):1513-1523. doi: 10.1016/S0140-6736(18)30134-X. Erratum in: Lancet. 2018 Jun 2;391(10136):2212.[↩]
- Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, Bennett DA, Chen Y, Dong C, Hu R, Zhou G, Yu B, Jia W, Parish S, Clarke R, Davey Smith G, Collins R, Holmes MV, Li L, Peto R, Chen Z; China Kadoorie Biobank Collaborative Group. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019 May 4;393(10183):1831-1842. doi: 10.1016/S0140-6736(18)31772-0[↩]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf[↩][↩][↩]
- Dawson DA, Li TK, Grant BF. A prospective study of risk drinking: at risk for what? Drug Alcohol Depend. 2008 May 1;95(1-2):62-72. doi: 10.1016/j.drugalcdep.2007.12.007[↩]
- Roerecke M, Rehm J. Chronic heavy drinking and ischaemic heart disease: a systematic review and meta-analysis. Open Heart. 2014 Aug 6;1(1):e000135. doi: 10.1136/openhrt-2014-000135[↩]
- Scoccianti C, Straif K, Romieu I. Recent evidence on alcohol and cancer epidemiology. Future Oncol. 2013 Sep;9(9):1315-22. https://doi.org/10.2217/fon.13.94[↩]
- Drinking Levels Defined. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking[↩]
- White AM, Tapert S, Shukla SD. Binge Drinking. Alcohol Res. 2018;39(1):1-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104965[↩][↩][↩][↩]
- Han BH, Moore AA, Ferris R, Palamar JJ. Binge Drinking Among Older Adults in the United States, 2015 to 2017. J Am Geriatr Soc. 2019 Oct;67(10):2139-2144. doi: 10.1111/jgs.16071[↩]
- Keyes KM, Jager J, Mal-Sarkar T, Patrick ME, Rutherford C, Hasin D. Is There a Recent Epidemic of Women’s Drinking? A Critical Review of National Studies. Alcohol Clin Exp Res. 2019 Jul;43(7):1344-1359. doi: 10.1111/acer.14082. Epub 2019 Jun 5. Erratum in: Alcohol Clin Exp Res. 2020 Feb;44(2):579.[↩]
- Wilsnack RW, Wilsnack SC, Gmel G, Kantor LW. Gender Differences in Binge Drinking. Alcohol Res. 2018;39(1):57-76. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6104960[↩]
- Centers for Disease Control and Prevention. Vital Signs: Alcohol Poisoning Deaths — United States, 2010–2012. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6353a2.htm[↩]
- Caplan YH, Goldberger BA, eds. Garriott’s medicolegal aspects of alcohol, sixth edition. Tucson, AZ: Lawyers and Judges Publication Company; 2015.[↩]
- National Institute of Alcohol Abuse and Alcoholism. Alcohol overdose: the dangers of drinking too much. Bethesda, MD: National Institute of Alcohol Abuse and Alcoholism; 2013. https://pubs.niaaa.nih.gov/publications/AlcoholOverdoseFactsheet/Overdosefact.htm[↩]
- Merck Sharp & Dohme Corp. Alcohol Toxicity and Withdrawal. https://www.merckmanuals.com/professional/special-subjects/recreational-drugs-and-intoxicants/alcohol-toxicity-and-withdrawal[↩]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Overdose: The Dangers of Drinking Too Much. https://pubs.niaaa.nih.gov/publications/AlcoholOverdoseFactsheet/Overdosefact.htm[↩]
- Edenberg HJ. The genetics of alcohol metabolism: role of alcohol dehydrogenase and aldehyde dehydrogenase variants. Alcohol Res Health. 2007;30(1):5-13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860432[↩][↩]
- Hurley TD, Edenberg HJ, Li T-K. Pharmacogenomics: The Search for Individualized Therapies. Weinheim, Germany: Wiley-VCH; 2002. The pharmacogenomics of alcoholism; pp. 417–441.[↩]
- Zaso MJ, Goodhines PA, Wall TL, Park A. Meta-Analysis on Associations of Alcohol Metabolism Genes With Alcohol Use Disorder in East Asians. Alcohol Alcohol. 2019 May 1;54(3):216-224. doi: 10.1093/alcalc/agz011[↩]
- Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nat Rev Genet. 2005 Jul;6(7):521-32. doi: 10.1038/nrg1635[↩]
- Hurley TD, Edenberg HJ. Genes encoding enzymes involved in ethanol metabolism. Alcohol Res. 2012;34(3):339-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3756590[↩]
- National Collaborating Centre for Mental Health (UK). Alcohol-Use Disorders: Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence. Leicester (UK): British Psychological Society (UK); 2011. (NICE Clinical Guidelines, No. 115.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK65487[↩]
- Schuckit MA. A Critical Review of Methods and Results in the Search for Genetic Contributors to Alcohol Sensitivity. Alcohol Clin Exp Res. 2018 May;42(5):822-835. doi: 10.1111/acer.13628[↩]
- Hingson RW, Heeren T, Winter MR. Preventing impaired driving. Alcohol Res Health. 1999;23(1):31-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761696[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Handling urges to drink. https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink.aspx[↩]
- U.S. Department of Health and Human Services. Rethinking Drinking – Handling urges to drink. https://www.rethinkingdrinking.niaaa.nih.gov/Tools/Interactive-worksheets-and-more/Stay-in-control/Coping-With-Urges-To-Drink-urge-tracker.aspx[↩]
- Alcoholics Anonymous. http://www.aa.org/[↩]
- What is A.A.? https://www.aa.org/what-is-aa[↩]
- Twelve Steps and Twelve Traditions Book. https://www.aa.org/the-big-book[↩]
- Nehring SM, Freeman AM. Alcohol Use Disorder. [Updated 2021 Apr 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK436003[↩][↩]
- Pavón, F. J., Serrano, A., Stouffer, D. G., Polis, I., Roberto, M., Cravatt, B. F., Martin-Fardon, R., Rodríguez de Fonseca, F., & Parsons, L. H. (2019). Ethanol-induced alterations in endocannabinoids and relevant neurotransmitters in the nucleus accumbens of fatty acid amide hydrolase knockout mice. Addiction biology, 24(6), 1204–1215. https://doi.org/10.1111/adb.12695[↩]
- Witkiewitz, K., Kranzler, H. R., Hallgren, K. A., O’Malley, S. S., Falk, D. E., Litten, R. Z., Hasin, D. S., Mann, K. F., & Anton, R. F. (2018). Drinking Risk Level Reductions Associated with Improvements in Physical Health and Quality of Life Among Individuals with Alcohol Use Disorder. Alcoholism, clinical and experimental research, 42(12), 2453–2465. https://doi.org/10.1111/acer.13897[↩]
- Degenhardt, L., Bharat, C., Bruno, R., Glantz, M. D., Sampson, N. A., Lago, L., Aguilar-Gaxiola, S., Alonso, J., Andrade, L. H., Bunting, B., Caldas-de-Almeida, J. M., Cia, A. H., Gureje, O., Karam, E. G., Khalaf, M., McGrath, J. J., Moskalewicz, J., Lee, S., Mneimneh, Z., Navarro-Mateu, F., … WHO World Mental Health Survey Collaborators (2019). Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s World Mental Health Surveys. Addiction (Abingdon, England), 114(3), 534–552. https://doi.org/10.1111/add.14482[↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013:490–491.[↩]
- Hashimoto E, Riederer PF, Hesselbrock VM, Hesselbrock MN, Mann K, Ukai W, Sohma H, Thibaut F, Schuckit MA, Saito T. Consensus paper of the WFSBP task force on biological markers: biological markers for alcoholism. World J Biol Psychiatry. 2013 Dec;14(8):549-64. https://doi.org/10.3109/15622975.2013.838302[↩]
- Substance Abuse and Mental Health Services Administration. Center for Substance Abuse Treatment. The Role of Biomarkers in the Treatment of Alcohol Use Disorders. US Department of Health and Human Services. September 2006.[↩][↩][↩][↩]
- Das SK, Dhanya L, Vasudevan DM. Biomarkers of alcoholism: an updated review. Scand J Clin Lab Invest. 2008;68(2):81-92. doi: 10.1080/00365510701532662. Epub 2007 Jun 24. Retraction in: Berg JP. Scand J Clin Lab Invest. 2012 Jul;72(4):343.[↩][↩][↩][↩][↩]
- Niemelä O. Biomarkers in alcoholism. Clin Chim Acta. 2007 Feb;377(1-2):39-49. doi: 10.1016/j.cca.2006.08.035[↩][↩][↩][↩][↩][↩][↩][↩]
- Hannuksela ML, Liisanantti MK, Nissinen AE, Savolainen MJ. Biochemical markers of alcoholism. Clin Chem Lab Med. 2007;45(8):953-61. doi: 10.1515/CCLM.2007.190[↩][↩][↩]
- Sommers MS, Savage C, Wray J, Dyehouse JM. Laboratory measures of alcohol (ethanol) consumption: strategies to assess drinking patterns with biochemical measures. Biol Res Nurs. 2003 Jan;4(3):203-17. doi: 10.1177/1099800402239624[↩]
- Jonas P. Bergström, Anders Helander, Clinical Characteristics of Carbohydrate-Deficient Transferrin (%Disialotransferrin) Measured by HPLC: Sensitivity, Specificity, Gender Effects, and Relationship with other Alcohol Biomarkers, Alcohol and Alcoholism, Volume 43, Issue 4, July-August 2008, Pages 436–441, https://doi.org/10.1093/alcalc/agn017[↩]
- Peterson K. Biomarkers for alcohol use and abuse–a summary. Alcohol Res Health. 2004-2005;28(1):30-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6601655[↩][↩]
- National Institute on Alcohol Abuse and Alcoholism. Treatment for Alcohol Problems: Finding and Getting Help. https://pubs.niaaa.nih.gov/publications/Treatment/treatment.htm[↩]
- Bogenschutz MP, Ross S, Bhatt S, Baron T, Forcehimes AA, Laska E, Mennenga SE, O’Donnell K, Owens LT, Podrebarac S, Rotrosen J, Tonigan JS, Worth L. Percentage of Heavy Drinking Days Following Psilocybin-Assisted Psychotherapy vs Placebo in the Treatment of Adult Patients With Alcohol Use Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2022 Oct 1;79(10):953-962. doi: 10.1001/jamapsychiatry.2022.2096. Erratum in: JAMA Psychiatry. 2022 Sep 14.[↩][↩]
- National Institutes of Health. Rethinking Drinking. Professional help. https://www.rethinkingdrinking.niaaa.nih.gov/Thinking-about-a-change/support-for-quitting/Professional-Help.aspx [↩]
- National Institute on Drug Abuse. Alcohol Addiction: Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition). https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/pharmacotherapi-1[↩][↩][↩]
- Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW. Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful? Addiction. 2013;108(2):275–293.[↩][↩]
- Yahn SL, Watterson LR, Olive MF. Safety and efficacy of acamprosate for the treatment of alcohol dependence. Subst Abuse. 2013;6:1–12.[↩]
- Jonas DE, Amick HR, Feltner C, et al. Pharmacotherapy for adults with alcohol use disorders in outpatient settings: a systematic review and meta-analysis. JAMA. 2014;311(18):1889–1900.[↩][↩][↩]
- Rösner S, Hackl-Herrwerth A, Leucht S, Lehert P, Vecchi S, Soyka M. Acamprosate for alcohol dependence. Cochrane Database Syst Rev. 2010;(9):CD004332.[↩]
- Berger L, Fisher M, Brondino M, et al. Efficacy of acamprosate for alcohol dependence in a family medicine setting in the United States: a randomized, double-blind, placebo-controlled study. Alcohol Clin Exp Res. 2013;37(4):668–674.[↩]
- Laaksonen E, Koski-Jännes A, Salaspuro M, Ahtinen H, Alho H. A randomized, multicentre, open-label, comparative trial of disulfiram, naltrexone and acamprosate in the treatment of alcohol dependence. Alcohol Alcohol. 2008;43(1):53–61.[↩]
- Skinner MD, Lahmek P, Pham H, Aubin HJ. Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis. PLoS One. 2014;9(2):e87366.[↩]
- Agency for Healthcare Research and Quality. Pharmacotherapy for adults with alcohol-use disorders in outpatient settings. Executive summary. https://effectivehealthcare.ahrq.gov/sites/default/files/related_files/alcohol-misuse-drug-therapy-surveillance.pdf[↩]
- Naltrexone. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/naltrexone[↩][↩]
- Niciu MJ, Arias AJ. Targeted opioid receptor antagonists in the treatment of alcohol use disorders. CNS Drugs. 2013;27(10):777–787.[↩]
- Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M. Opioid antagonists for alcohol dependence. Cochrane Database Syst Rev. 2010;(12):CD001867.[↩]
- Garbutt JC, Kranzler HR, O’Malley SS, et al.; Vivitrex Study Group. Efficacy and tolerability of long-acting injectable naltrexone for alcohol dependence: a randomized controlled trial [published corrections appear in JAMA. 2005;293(16):1978, and JAMA. 2005;293(23):2864]. JAMA. 2005;293(13):1617–1625.[↩]
- Anton RF, O’Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–2017.[↩]
- Kiefer F, Jahn H, Tarnaske T, et al. Comparing and combining naltrexone and acamprosate in relapse prevention of alcoholism: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2003;60(1):92–99.[↩]
- van den Brink W, Aubin HJ, Bladström A, Torup L, Gual A, Mann K. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies [published correction appears in Alcohol Alcohol. 2013;48(6):746]. Alcohol Alcohol. 2013;48(5):570–578.[↩]
- Pani PP, Trogu E, Pacini M, Maremmani I. Anticonvulsants for alcohol dependence. Cochrane Database Syst Rev. 2014;(2):CD008544.[↩]
- Johnson BA, Rosenthal N, Capece JA, et al.; Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007;298(14):1641–1651.[↩]
- Paparrigopoulos T, Tzavellas E, Karaiskos D, Kourlaba G, Liappas I. Treatment of alcohol dependence with low-dose topiramate: an open-label controlled study. BMC Psychiatry. 2011;11:41.[↩]
- Likhitsathian S, Uttawichai K, Booncharoen H, Wittayanookulluk A, Angkurawaranon C, Srisurapanont M. Topiramate treatment for alcoholic outpatients recently receiving residential treatment programs: a 12-week, randomized, placebo-controlled trial. Drug Alcohol Depend. 2013;133(2):440–446.[↩]
- Kranzler HR, Covault J, Feinn R, et al. Topiramate treatment for heavy drinkers: moderation by a GRIK1 polymorphism [published correction appears in Am J Psychiatry. 2014;171(5):585]. Am J Psychiatry. 2014;171(4):445–452.[↩]
- Mason BJ, Quello S, Goodell V, Shadan F, Kyle M, Begovic A. Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med. 2014;174(1):70–77.[↩]
- Furieri FA, Nakamura-Palacios EM. Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2007;68(11):1691–1700.[↩]
- Leung JG, Hall-Flavin D, Nelson S, Schmidt KA, Schak KM. The role of gabapentin in the management of alcohol withdrawal and dependence. Ann Pharmacother. 2015;49(8):897–906.[↩]
- Martinotti G, Di Nicola M, Tedeschi D, et al. Pregabalin versus naltrexone in alcohol dependence: a randomised, double-blind, comparison trial. J Psychopharmacol. 2010;24(9):1367–1374.[↩]
- Torrens M, Fonseca F, Mateu G, Farré M. Efficacy of antidepressants in substance use disorders with and without comorbid depression. A systematic review and meta-analysis. Drug Alcohol Depend. 2005;78(1):1–22.[↩]
- Pettinati HM, Oslin DW, Kampman KM, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010;167(6):668–675.[↩]
- Cornelius JR, Salloum IM, Ehler JG, et al. Fluoxetine in depressed alcoholics. A double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1997;54(8):700–705.[↩]
- Kranzler HR, Pierucci-Lagha A, Feinn R, Hernandez-Avila C. Effects of ondansetron in early- versus late-onset alcoholics: a prospective, open-label study. Alcohol Clin Exp Res. 2003;27(7):1150–1155.[↩]
- Johnson BA, Ait-Daoud N, Ma JZ, Wang Y. Ondansetron reduces mood disturbance among biologically predisposed, alcohol-dependent individuals. Alcohol Clin Exp Res. 2003;27(11):1773–1779.[↩]
- Corrêa Filho JM, Baltieri DA. A pilot study of full-dose ondansetron to treat heavy-drinking men withdrawing from alcohol in Brazil. Addict Behav. 2013;38(4):2044–2051.[↩][↩]
- Medications for Alcohol Use Disorder. Am Fam Physician. 2016 Mar 15;93(6):457-465. https://www.aafp.org/afp/2016/0315/afp20160315p457.pdf[↩]
- Alcohol Withdrawal Syndrome. Am Fam Physician. 2004 Mar 15;69(6):1443-1450. https://www.aafp.org/afp/2004/0315/p1443.html[↩][↩][↩]
- Mirijello, A., D’Angelo, C., Ferrulli, A., Vassallo, G., Antonelli, M., Caputo, F., Leggio, L., Gasbarrini, A., & Addolorato, G. (2015). Identification and management of alcohol withdrawal syndrome. Drugs, 75(4), 353–365. https://doi.org/10.1007/s40265-015-0358-1[↩][↩][↩]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, D.C.: American Psychiatric Association; 2013.[↩]
- McKeon A, Frye MA, Delanty N. The alcohol withdrawal syndrome. J Neurol Neurosurg Psychiatry. 2008 Aug;79(8):854-62. doi: 10.1136/jnnp.2007.128322[↩][↩][↩][↩][↩][↩][↩][↩]
- Alcohol Withdrawal Syndrome: Outpatient Management. Am Fam Physician. 2021 Sep ;104(2):253-262. https://www.aafp.org/afp/2021/0900/p253.html[↩][↩]
- Gulati, P., Chavan, B. S., & Sidana, A. (2019). Comparative efficacy of baclofen and lorazepam in the treatment of alcohol withdrawal syndrome. Indian journal of psychiatry, 61(1), 60–64. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_40_17[↩]
- Perry EC. Inpatient management of acute alcohol withdrawal syndrome. CNS Drugs. 2014 May;28(5):401-10. doi: 10.1007/s40263-014-0163-5[↩][↩][↩][↩][↩]
- Perme, B., Vijaysagar, K. J., & Chandrasekharan, R. (2003). Follow-up study of alcoholic hallucinosis. Indian journal of psychiatry, 45(4), 244–246. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2952372/pdf/IJPsy-45-244.pdf[↩][↩]
- Mainerova B, Prasko J, Latalova K, Axmann K, Cerna M, Horacek R, Bradacova R. Alcohol withdrawal delirium – diagnosis, course and treatment. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2015 Mar;159(1):44-52. https://biomed.papers.upol.cz/pdfs/bio/2015/01/07.pdf[↩]
- Schuckit MA. Recognition and management of withdrawal delirium (delirium tremens). N Engl J Med. 2014 Nov 27;371(22):2109-13. doi: 10.1056/NEJMra1407298[↩]
- Lerner WD, Fallon HJ. The alcohol withdrawal syndrome. N Engl J Med. 1985 Oct 10;313(15):951-2. doi: 10.1056/NEJM198510103131509[↩]
- Whiteman, P.J., Hoffman, R.S. and Goldfrank, L.R. (2000), Alcoholism in the Emergency Department: An Epidemiologic Study. Academic Emergency Medicine, 7: 14-20. https://doi.org/10.1111/j.1553-2712.2000.tb01884.x[↩][↩]
- Glasper A, Gossop M, de Wet C, Reed L, Bearn J. Influence of the dose on the severity of opiate withdrawal symptoms during methadone detoxification. Pharmacology. 2008;81(2):92-6. doi: 10.1159/000109982[↩]
- Gupta M, Gokarakonda SB, Attia FN. Withdrawal Syndromes. [Updated 2021 Oct 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459239[↩][↩]
- Awissi DK, Lebrun G, Fagnan M, Skrobik Y; Regroupement de Soins Critiques, Réseau de Soins Respiratoires, Québec. Alcohol, nicotine, and iatrogenic withdrawals in the ICU. Crit Care Med. 2013 Sep;41(9 Suppl 1):S57-68. doi: 10.1097/CCM.0b013e3182a16919[↩]
- Dixit D, Endicott J, Burry L, Ramos L, Yeung SY, Devabhakthuni S, Chan C, Tobia A, Bulloch MN. Management of Acute Alcohol Withdrawal Syndrome in Critically Ill Patients. Pharmacotherapy. 2016 Jul;36(7):797-822. doi: 10.1002/phar.1770[↩][↩]
- Brathen G, Ben-Menachem E, Brodtkorb E, et al. Alcohol-related seizures. In: Gilhus NE, Barnes MP, Brainin M, editors. European Handbook of Neurological Management. 2nd Vol. 1. 2011.[↩]
- Hillbom M, Pieninkeroinen I, Leone M. Seizures in alcohol-dependent patients: epidemiology, pathophysiology and management. CNS Drugs. 2003;17(14):1013-30. doi: 10.2165/00023210-200317140-00002[↩]
- Sachdeva, A., Choudhary, M., & Chandra, M. (2015). Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond. Journal of clinical and diagnostic research : JCDR, 9(9), VE01–VE07. https://doi.org/10.7860/JCDR/2015/13407.6538[↩]
- Zindel, L. R., & Kranzler, H. R. (2014). Pharmacotherapy of alcohol use disorders: seventy-five years of progress. Journal of studies on alcohol and drugs. Supplement, 75 Suppl 17(Suppl 17), 79–88. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4453501[↩]
- David A. Fiellin MD, Patrick G. O’Connor MD, MPH, Eric S. Holmboe MD & Ralph I. Horwitz MD (2002) Risk for delirium tremens in patients with alcohol withdrawal syndrome, Substance Abuse, 23:2, 83-94, DOI: 10.1080/08897070209511478[↩]
- Jesse, S., & Ludolph, A. (2019). Alcohol Withdrawal Syndrome: Clinical Picture and Therapeutic Options. In Neuroscience of Alcohol(pp. 671-680). Academic Press.[↩]
- VICTOR M, ADAMS RD. The effect of alcohol on the nervous system. Res Publ Assoc Res Nerv Ment Dis. 1953;32:526-73.[↩][↩][↩]
- Victor M. Treatment of the neurologic complications of alcoholism. Mod Treat. 1966 May;3(3):491-501.[↩]
- VICTOR M, HOPE JM, ADAMS RD. Auditory hallucinations in the alcoholic patient. Trans Am Neurol Assoc. 1953;3(78th Meeting):273-5.[↩]
- Victor M, Brausch C. The role of abstinence in the genesis of alcoholic epilepsy. Epilepsia. 1967 Mar;8(1):1-20. doi: 10.1111/j.1528-1157.1967.tb03815.x[↩]
- Gold J, Nelson LS. Ethanol withdrawal. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, editors. Goldfrank’s toxicologic emergencies. 9th. New York, NY: McGraw-Hill; 2011. pp. 1134–1142.[↩]
- Wolf KM, Shaughnessy AF, Middleton DB. Prolonged delirium tremens requiring massive doses of medication. J Am Board Fam Pract. 1993 Sep-Oct;6(5):502-4.[↩]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Arlington: American Psychiatric Association; 2013.[↩][↩][↩][↩]
- Schuckit MA, Tipp JE, Reich T, Hesselbrock VM, Bucholz KK. The histories of withdrawal convulsions and delirium tremens in 1648 alcohol dependent subjects. Addiction. 1995 Oct;90(10):1335-47. doi: 10.1046/j.1360-0443.1995.901013355.x[↩][↩]
- Fouarge E, Maquet P. Conséquences neurologiques centrales et périphériques de l’alcoolisme [Neurological consequences of alcoholism]. Rev Med Liege. 2019 May;74(5-6):310-313. French.[↩]
- Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005 Feb 10;352(6):596-607. doi: 10.1056/NEJMcp042262[↩]
- Maldonado JR, Sher Y, Ashouri JF, Hills-Evans K, Swendsen H, Lolak S, Miller AC. The “Prediction of Alcohol Withdrawal Severity Scale” (PAWSS): systematic literature review and pilot study of a new scale for the prediction of complicated alcohol withdrawal syndrome. Alcohol. 2014 Jun;48(4):375-90. doi: 10.1016/j.alcohol.2014.01.004[↩]
- Lemon SJ Jr, Winstead PS, Weant KA. Alcohol withdrawal syndrome. Advanced Emergency Nursing Journal. 2010;32(1):20–27.[↩][↩]
- Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.[↩]
- Campbell EJ, Lawrence AJ, Perry CJ. New steps for treating alcohol use disorder. Psychopharmacology (Berl). 2018 Jun;235(6):1759-1773. doi: 10.1007/s00213-018-4887-7[↩]
- Benzer DG. Management of alcohol intoxication and withdrawal. In: Miller NS, American Society of Addiction Medicine, eds. Principles of Addiction Medicine. Chevy Chase, Md.: The Society; 1994.[↩]
- Elholm B, Larsen K, Hornnes N, et al. A psychometric validation of the Short Alcohol Withdrawal Scale (SAWS). Alcohol Alcohol. 2010;45(4):361–365.[↩]
- Shaw JM, Kolesar GS, Sellers EM, Kaplan HL, Sandor P. Development of optimal treatment tactics for alcohol withdrawal. I. Assessment and effectiveness of supportive care. J Clin Psychopharmacol. 1981 Nov;1(6):382-89. doi: 10.1097/00004714-198111000-00006[↩]
- Sullivan JT, Swift RM, Lewis DC. Benzodiazepine requirements during alcohol withdrawal syndrome: clinical implications of using a standardized withdrawal scale. J Clin Psychopharmacol. 1991 Oct;11(5):291-5.[↩]
- Wetterling T, Kanitz RD, Besters B, Fischer D, Zerfass B, John U, Spranger H, Driessen M. A new rating scale for the assessment of the alcohol-withdrawal syndrome (AWS scale). Alcohol Alcohol. 1997 Nov-Dec;32(6):753-60. https://doi.org/10.1093/oxfordjournals.alcalc.a008326[↩][↩][↩]
- Young GP, Rores C, Murphy C, Dailey RH. Intravenous phenobarbital for alcohol withdrawal and convulsions. Ann Emerg Med. 1987 Aug;16(8):847-50. doi: 10.1016/s0196-0644(87)80520-6[↩]
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989 Nov;84(11):1353-7. doi: 10.1111/j.1360-0443.1989.tb00737.x[↩][↩]
- Elholm B, Larsen K, Hornnes N, Zierau F, Becker U. A psychometric validation of the Short Alcohol Withdrawal Scale (SAWS). Alcohol Alcohol. 2010;45(4):362.[↩]
- TILMAN WETTERLING, BERNHARD WEBER, MARKUS DEPFENHART, BARBARA SCHNEIDER, KLAUS JUNGHANNS, DEVELOPMENT OF A RATING SCALE TO PREDICT THE SEVERITY OF ALCOHOL WITHDRAWAL SYNDROME, Alcohol and Alcoholism, Volume 41, Issue 6, November/December 2006, Pages 611–615, https://doi.org/10.1093/alcalc/agl068[↩]
- Maldonado, Jose & Sher, Yelizaveta & Das, Smita & Hills-Evans, Kelsey & Frenklach, Anna & Lolak, Sermsak & Talley, Rachel & Neri, Eric. (2015). Prospective Validation Study of the Prediction of Alcohol Withdrawal Severity Scale (PAWSS) in Medically Ill Inpatients: A New Scale for the Prediction of Complicated Alcohol Withdrawal Syndrome. Alcohol and alcoholism (Oxford, Oxfordshire). 50. 10.1093/alcalc/agv043. https://www.psychdb.com/_media/addictions/etoh_pawss_score_maldonando_.pdf[↩]
- Neuman JE, Quan D. Alcohol withdrawal syndrome. Emerg Med Rep. 2009;30(16):197–207.[↩]
- Addolorato, G., Mirijello, A., Leggio, L., Ferrulli, A., D’Angelo, C., Vassallo, G., Cossari, A., Gasbarrini, G., Landolfi, R., Agnes, S., Gasbarrini, A., & Gemelli OLT Group (2013). Liver transplantation in alcoholic patients: impact of an alcohol addiction unit within a liver transplant center. Alcoholism, clinical and experimental research, 37(9), 1601–1608. https://doi.org/10.1111/acer.12117[↩]
- Naranjo CA, Sellers EM, Chater K, et al. Nonpharmacologic intervention in acute alcohol withdrawal. Clin Pharmacol Ther. 1983;34(2):214–219.[↩]
- Ely EW, Truman B, Shintani A, Thomason JWW, Wheeler AP, Gordon S et al. Monitoring sedation status over time in ICU patients: the reliability and validity of the Richmond Agitation Sedation Scale (RASS). JAMA 2003; 289:2983-2991.[↩]
- Hayashida M, Alterman AI, McLellan AT, O’Brien CP, Purtill JJ, Volpicelli JR, et al. Comparative effectiveness and costs of inpatient and outpatient detoxification of patients with mild-to-moderate alcohol withdrawal syndrome. N Engl J Med. 1989;320:358-65.[↩]
- Klijnsma MP, Cameron ML, Burns TP, et al. Out-patient alcohol detoxification—outcome after 2 months. Alcohol Alcohol. 1995;30(5):669–673.[↩]
- Stinnett JL. Outpatient detoxification of the alcoholic. Int J Addict. 1982;17(6):1031–1046.[↩]
- Myrick H, Anton RF. Treatment of alcohol withdrawal. Alcohol Health Res World. 1998;22(1):38–43.[↩]
- Blondell RD. Ambulatory detoxification of patients with alcohol dependence. Am Fam Physician. 2005;71(3):495–502.[↩]
- Lukan JK, Reed DN Jr, Looney SW, Spain DA, Blondell RD. Risk factors for delirium tremens in trauma patients. J Trauma. 2002;53:901-6.[↩]
- Bhat, P. S., Ryali, V., Srivastava, K., Kumar, S. R., Prakash, J., & Singal, A. (2012). Alcoholic hallucinosis. Industrial psychiatry journal, 21(2), 155–157. https://doi.org/10.4103/0972-6748.119646[↩][↩]
- Genera, Switzerland: World Health Organization; 2006. The ICD – 10 Classification of Mental and Behavioral Disorders: Clinical Description and Diagnostic Guidelines[↩]
- Stankewicz HA, Richards JR, Salen P. Alcohol Related Psychosis. [Updated 2021 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459134[↩][↩]
- Moggi F. Epidemiologie, Ätiologie und Behandlung von Patienten mit Psychosen und komorbider Suchterkrankung [Epidemiology, etiology and treatment of patients with psychosis and co-morbid substance use disorder]. Ther Umsch. 2018 Jun;75(1):37-43. German. doi: 10.1024/0040-5930/a000964[↩]
- Testino G, Bottaro LC, Patussi V, Scafato E, Addolorato G, Leone S, Renzetti D, Balbinot P, Greco G, Fanucchi T, Schiappacasse G, Cardinale P, Allosio P, Pellicano R, Caputo F; Study Committee of SIA (Società Italiana di Alcologia). Addiction disorders: a need for change. Proposal for a new management. Position paper of SIA, Italian Society on Alcohol. Minerva Med. 2018 Oct;109(5):369-385. doi: 10.23736/S0026-4806.18.05741-5[↩]
- Naranjo CA, Sellers EM, Chater K, Iversen P, Roach C, Sykora K. Nonpharmacologic intervention in acute alcohol withdrawal. Clin Pharmacol Ther. 1983 Aug;34(2):214-9. doi: 10.1038/clpt.1983.155[↩]
- Ambulatory Detoxification of Patients with Alcohol Dependence. Am Fam Physician. 2005 Feb 1;71(3):495-502. https://www.aafp.org/afp/2005/0201/p495.html[↩][↩][↩]
- Cook CC, Thomson AD. B-complex vitamins in the prophylaxis and treatment of Wernicke-Korsakoff syndrome. Br J Hosp Med. 1997 May 7-20;57(9):461-5.[↩]
- Hack JB, Hoffman RS. Thiamine before glucose to prevent Wernicke encephalopathy: examining the conventional wisdom. JAMA. 1998 Feb 25;279(8):583-4. doi: 10.1001/jama.279.8.583[↩]
- Sarai M, Tejani AM, Chan AH, Kuo IF, Li J. Magnesium for alcohol withdrawal. Cochrane Database Syst Rev. 2013 Jun 5;(6):CD008358. doi: 10.1002/14651858.CD008358.pub2[↩][↩]
- Kosten TR, O’Connor PG. Management of drug and alcohol withdrawal. N Engl J Med. 2003 May 1;348(18):1786-95. doi: 10.1056/NEJMra020617[↩][↩][↩]
- Malcolm R, Myrick H, Brady KT, Ballenger JC. Update on anticonvulsants for the treatment of alcohol withdrawal. Am J Addict. 2001;10(s1):s16-s23. doi: 10.1080/10550490150504100[↩]
- Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 1997 Jul 9;278(2):144-51. doi: 10.1001/jama.278.2.144[↩][↩][↩][↩][↩][↩][↩]
- Mayo-Smith MF, Beecher LH, Fischer TL, Gorelick DA, Guillaume JL, Hill A, Jara G, Kasser C, Melbourne J; Working Group on the Management of Alcohol Withdrawal Delirium, Practice Guidelines Committee, American Society of Addiction Medicine. Management of alcohol withdrawal delirium. An evidence-based practice guideline. Arch Intern Med. 2004 Jul 12;164(13):1405-12. doi: 10.1001/archinte.164.13.1405. Erratum in: Arch Intern Med. 2004 Oct 11;164(18):2068. Dosage error in article text.[↩][↩]
- Sen S, Grgurich P, Tulolo A, Smith-Freedman A, Lei Y, Gray A, Dargin J. A Symptom-Triggered Benzodiazepine Protocol Utilizing SAS and CIWA-Ar Scoring for the Treatment of Alcohol Withdrawal Syndrome in the Critically Ill. Ann Pharmacother. 2017 Feb;51(2):101-110. doi: 10.1177/1060028016672036[↩]
- Wong A, Benedict NJ, Armahizer MJ, Kane-Gill SL. Evaluation of adjunctive ketamine to benzodiazepines for management of alcohol withdrawal syndrome. Ann Pharmacother. 2015 Jan;49(1):14-9. doi: 10.1177/1060028014555859[↩][↩]
- Gold, J. A., Rimal, B., Nolan, A., & Nelson, L. S. (2007). A strategy of escalating doses of benzodiazepines and phenobarbital administration reduces the need for mechanical ventilation in delirium tremens. Critical care medicine, 35(3), 724–730. https://doi.org/10.1097/01.CCM.0000256841.28351.80[↩][↩][↩]
- Linn DD, Loeser KC. Dexmedetomidine for Alcohol Withdrawal Syndrome. Ann Pharmacother. 2015 Dec;49(12):1336-42. doi: 10.1177/1060028015607038[↩]
- Sarff M, Gold JA. Alcohol withdrawal syndromes in the intensive care unit. Crit Care Med. 2010 Sep;38(9 Suppl):S494-501. doi: 10.1097/CCM.0b013e3181ec5412[↩]
- Jesse, S., Bråthen, G., Ferrara, M., Keindl, M., Ben-Menachem, E., Tanasescu, R., Brodtkorb, E., Hillbom, M., Leone, M. A. and Ludolph, A. C. (2017), Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurologica Scandinavica, 135: 4– 16. doi: 10.1111/ane.12671[↩][↩]
- The American Psychiatric Association Practice Guideline for the Pharmacological Treatment of Patients With Alcohol Use Disorder. Victor I. Reus, Laura J. Fochtmann, Oscar Bukstein, A. Evan Eyler, Donald M. Hilty, Marcela Horvitz-Lennon, Jane Mahoney, Jagoda Pasic, Michael Weaver, Cheryl D. Wills, Jack McIntyre, Jeremy Kidd, Joel Yager, and Seung-Hee Hong. American Journal of Psychiatry 2018 175:1, 86-90. https://doi.org/10.1176/appi.ajp.2017.1750101[↩][↩]
- Kranzler, H. R., & Soyka, M. (2018). Diagnosis and pharmacotherapy of alcohol use disorder: a review. Jama, 320(8), 815-824.[↩]
- Outpatient Management of Alcohol Withdrawal Syndrome. Am Fam Physician. 2013 Nov 1;88(9):589-595. https://www.aafp.org/afp/2013/1101/p589.html[↩][↩][↩]
- Amato, L., Minozzi, S., & Davoli, M. (2011). Efficacy and safety of pharmacological interventions for the treatment of the Alcohol Withdrawal Syndrome. The Cochrane database of systematic reviews, 2011(6), CD008537. https://doi.org/10.1002/14651858.CD008537.pub2[↩][↩]
- Lugoboni F, Mirijello A, Faccini M, Casari R, Cossari A, Musi G, Bissoli G, Quaglio G, Addolorato G. Quality of life in a cohort of high-dose benzodiazepine dependent patients. Drug Alcohol Depend. 2014 Sep 1;142:105-9. doi: 10.1016/j.drugalcdep.2014.06.020[↩]
- Mayo-Smith MF, Beecher LH, Fischer TL, et al. Management of Alcohol Withdrawal Delirium: An Evidence-Based Practice Guideline. Arch Intern Med. 2004;164(13):1405–1412. doi:10.1001/archinte.164.13.1405 Erratum in: Arch Intern Med. 2004 Oct 11;164(18):2068. Dosage error in article text. [↩]
- Guina J, Merrill B. Benzodiazepines I: Upping the Care on Downers: The Evidence of Risks, Benefits and Alternatives. Journal of Clinical Medicine. 2018; 7(2):17. https://doi.org/10.3390/jcm7020017[↩]
- Muzyk AJ, Leung JG, Nelson S, Embury ER, Jones SR. The role of diazepam loading for the treatment of alcohol withdrawal syndrome in hospitalized patients. Am J Addict. 2013 Mar-Apr;22(2):113-8. doi: 10.1111/j.1521-0391.2013.00307.x[↩][↩][↩]
- Peppers MP. Benzodiazepines for alcohol withdrawal in the elderly and in patients with liver disease. Pharmacotherapy. 1996 Jan-Feb;16(1):49-57.[↩]
- Lejoyeux M, Solomon J, Adès J. Benzodiazepine treatment for alcohol-dependent patients. Alcohol Alcohol. 1998 Nov-Dec;33(6):563-75. doi: 10.1093/alcalc/33.6.563[↩]
- Kattimani, S., & Bharadwaj, B. (2013). Clinical management of alcohol withdrawal: A systematic review. Industrial psychiatry journal, 22(2), 100–108. https://doi.org/10.4103/0972-6748.132914[↩][↩][↩][↩][↩]
- Maldonado JR, Nguyen LH, Schader EM, Brooks JO 3rd. Benzodiazepine loading versus symptom-triggered treatment of alcohol withdrawal: a prospective, randomized clinical trial. Gen Hosp Psychiatry. 2012 Nov-Dec;34(6):611-7. doi: 10.1016/j.genhosppsych.2012.06.016[↩]
- Saitz R, Mayo-Smith MF, Roberts MS, Redmond HA, Bernard DR, Calkins DR. Individualized treatment for alcohol withdrawal. A randomized double-blind controlled trial. JAMA. 1994 Aug 17;272(7):519-23.[↩]
- Bounds CG, Nelson VL. Benzodiazepines. [Updated 2021 Nov 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470159[↩][↩]
- Kang M, Galuska MA, Ghassemzadeh S. Benzodiazepine Toxicity. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482238[↩][↩]
- Pfizer Pharmaceutical. (2021). Xanax XR, Alprazolam Extended-Release. https://labeling.pfizer.com/ShowLabeling.aspx?id=543[↩]
- Mihic SJ, Harris RA. Hypnotics and sedatives. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman and Gilman’s the pharmacological basis of therapeutics. 12th. New York: McGraw-Hill; 2011. pp. 457–480.[↩]
- Irifune M, Takarada T, Shimizu Y, Endo C, Katayama S, Dohi T, Kawahara M. Propofol-induced anesthesia in mice is mediated by gamma-aminobutyric acid-A and excitatory amino acid receptors. Anesth Analg. 2003 Aug;97(2):424-429. doi: 10.1213/01.ANE.0000059742.62646.40[↩]
- Wong A, Benedict NJ, Kane-Gill SL. Multicenter evaluation of pharmacologic management and outcomes associated with severe resistant alcohol withdrawal. J Crit Care. 2015 Apr;30(2):405-9. doi: 10.1016/j.jcrc.2014.10.008[↩]
- Wong A, Benedict NJ, Lohr BR, Pizon AF, Kane-Gill SL. Management of benzodiazepine-resistant alcohol withdrawal across a healthcare system: Benzodiazepine dose-escalation with or without propofol. Drug Alcohol Depend. 2015 Sep 1;154:296-9. doi: 10.1016/j.drugalcdep.2015.07.005[↩]
- McCowan C, Marik P. Refractory delirium tremens treated with propofol: a case series. Crit Care Med. 2000 Jun;28(6):1781-4. doi: 10.1097/00003246-200006000-00014[↩]
- Muzyk AJ, Fowler JA, Norwood DK, Chilipko A. Role of α2-agonists in the treatment of acute alcohol withdrawal. Ann Pharmacother. 2011 May;45(5):649-57. doi: 10.1345/aph.1P575[↩]
- Mueller SW, Preslaski CR, Kiser TH, Fish DN, Lavelle JC, Malkoski SP, MacLaren R. A randomized, double-blind, placebo-controlled dose range study of dexmedetomidine as adjunctive therapy for alcohol withdrawal. Crit Care Med. 2014 May;42(5):1131-9. doi: 10.1097/CCM.0000000000000141[↩]
- Barrons R, Roberts N. The role of carbamazepine and oxcarbazepine in alcohol withdrawal syndrome. J Clin Pharm Ther. 2010 Apr;35(2):153-67. doi: 10.1111/j.1365-2710.2009.01098.x[↩][↩]
- Leggio L, Kenna GA, Swift RM. New developments for the pharmacological treatment of alcohol withdrawal syndrome. A focus on non-benzodiazepine GABAergic medications. Prog Neuropsychopharmacol Biol Psychiatry. 2008 Jul 1;32(5):1106-17. doi: 10.1016/j.pnpbp.2007.09.021[↩]
- Mueller TI, Stout RL, Rudden S, Brown RA, Gordon A, Solomon DA, Recupero PR. A double-blind, placebo-controlled pilot study of carbamazepine for the treatment of alcohol dependence. Alcohol Clin Exp Res. 1997 Feb;21(1):86-92.[↩]
- Pippenger CE. Clinically significant carbamazepine drug interactions: an overview. Epilepsia. 1987;28 Suppl 3:S71-6. doi: 10.1111/j.1528-1157.1987.tb05781.x[↩]
- Reoux JP, Saxon AJ, Shen D. Pharmacokinetic profile of an oral loading dose of divalproex sodium during acute alcohol withdrawal. J Clin Psychopharmacol. 2006 Feb;26(1):105-7. doi: 10.1097/01.jcp.0000196416.06729.fe[↩]
- Reoux JP, Saxon AJ, Malte CA, Baer JS, Sloan KL. Divalproex sodium in alcohol withdrawal: a randomized double-blind placebo-controlled clinical trial. Alcohol Clin Exp Res. 2001 Sep;25(9):1324-9.[↩]
- Snead OC 3rd, Gibson KM. Gamma-hydroxybutyric acid. N Engl J Med. 2005 Jun 30;352(26):2721-32. doi: 10.1056/NEJMra044047. Erratum in: N Engl J Med. 2006 Feb 2;354(5):537[↩]
- Gessa GL, Agabio R, Carai MA, Lobina C, Pani M, Reali R, Colombo G. Mechanism of the antialcohol effect of gamma-hydroxybutyric acid. Alcohol. 2000 Apr;20(3):271-6. doi: 10.1016/s0741-8329(99)00091-9[↩]
- Skala K, Caputo F, Mirijello A, Vassallo G, Antonelli M, Ferrulli A, Walter H, Lesch O, Addolorato G. Sodium oxybate in the treatment of alcohol dependence: from the alcohol withdrawal syndrome to the alcohol relapse prevention. Expert Opin Pharmacother. 2014 Feb;15(2):245-57. doi: 10.1517/14656566.2014.863278[↩]
- Nava F, Premi S, Manzato E, Campagnola W, Lucchini A, Gessa GL. Gamma-hydroxybutyrate reduces both withdrawal syndrome and hypercortisolism in severe abstinent alcoholics: an open study vs. diazepam. Am J Drug Alcohol Abuse. 2007;33(3):379-92. doi: 10.1080/00952990701315046[↩]
- Nimmerrichter AA, Walter H, Gutierrez-Lobos KE, Lesch OM. Double-blind controlled trial of gamma-hydroxybutyrate and clomethiazole in the treatment of alcohol withdrawal. Alcohol Alcohol. 2002 Jan-Feb;37(1):67-73. doi: 10.1093/alcalc/37.1.67[↩]
- Leone MA, Vigna-Taglianti F, Avanzi G, Brambilla R, Faggiano F. Gamma-hydroxybutyrate (GHB) for treatment of alcohol withdrawal and prevention of relapses. Cochrane Database Syst Rev. 2010 Feb 17;(2):CD006266. doi: 10.1002/14651858.CD006266.pub2[↩][↩][↩]
- Caputo F, Skala K, Mirijello A, Ferrulli A, Walter H, Lesch O, Addolorato G. Sodium oxybate in the treatment of alcohol withdrawal syndrome: a randomized double-blind comparative study versus oxazepam. The GATE 1 trial. CNS Drugs. 2014 Aug;28(8):743-52. doi: 10.1007/s40263-014-0183-1[↩]
- Tunnicliff G, Raess BU. Gamma-Hydroxybutyrate (orphan medical). Curr Opin Investig Drugs. 2002 Feb;3(2):278-83[↩]
- Addolorato G, Leggio L, Ferrulli A, Caputo F, Gasbarrini A. The therapeutic potential of gamma-hydroxybutyric acid for alcohol dependence: balancing the risks and benefits. A focus on clinical data. Expert Opin Investig Drugs. 2009 May;18(5):675-86. doi: 10.1517/13543780902905855[↩]
- Addolorato G, Leggio L. Safety and efficacy of baclofen in the treatment of alcohol-dependent patients. Curr Pharm Des. 2010;16(19):2113-7. doi: 10.2174/138161210791516440[↩]
- Colombo G, Agabio R, Carai MA, Lobina C, Pani M, Reali R, Addolorato G, Gessa GL. Ability of baclofen in reducing alcohol intake and withdrawal severity: I–Preclinical evidence. Alcohol Clin Exp Res. 2000 Jan;24(1):58-66.[↩]
- Knapp, D. J., Overstreet, D. H., & Breese, G. R. (2007). Baclofen blocks expression and sensitization of anxiety-like behavior in an animal model of repeated stress and ethanol withdrawal. Alcoholism, clinical and experimental research, 31(4), 582–595. https://doi.org/10.1111/j.1530-0277.2007.00342.x[↩]
- Addolorato G, Leggio L, Abenavoli L, Agabio R, Caputo F, Capristo E, Colombo G, Gessa GL, Gasbarrini G. Baclofen in the treatment of alcohol withdrawal syndrome: a comparative study vs diazepam. Am J Med. 2006 Mar;119(3):276.e13-8. doi: 10.1016/j.amjmed.2005.08.042[↩][↩]
- Lyon JE, Khan RA, Gessert CE, Larson PM, Renier CM. Treating alcohol withdrawal with oral baclofen: a randomized, double-blind, placebo-controlled trial. J Hosp Med. 2011 Oct;6(8):469-74. doi: 10.1002/jhm.928[↩]
- Stallings W, Schrader S. Baclofen as prophylaxis and treatment for alcohol withdrawal: a retrospective chart review. J Okla State Med Assoc. 2007 Sep;100(9):354-60.[↩]
- Flannery BA, Garbutt JC, Cody MW, Renn W, Grace K, Osborne M, Crosby K, Morreale M, Trivette A. Baclofen for alcohol dependence: a preliminary open-label study. Alcohol Clin Exp Res. 2004 Oct;28(10):1517-23. doi: 10.1097/01.alc.0000141640.48924.14[↩]
- Addolorato G, Leggio L, Agabio R, Colombo G, Gasbarrini G. Baclofen: a new drug for the treatment of alcohol dependence. Int J Clin Pract. 2006 Aug;60(8):1003-8. doi: 10.1111/j.1742-1241.2006.01065.x[↩]
- Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, Abenavoli L, D’Angelo C, Caputo F, Zambon A, Haber PS, Gasbarrini G. Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet. 2007 Dec 8;370(9603):1915-22. doi: 10.1016/S0140-6736(07)61814-5[↩]
- Addolorato, G., Mirijello, A., Leggio, L., Ferrulli, A., & Landolfi, R. (2013). Management of alcohol dependence in patients with liver disease. CNS drugs, 27(4), 287–299. https://doi.org/10.1007/s40263-013-0043-4[↩]
- McLean MJ, Morrell MJ, Willmore LJ, Privitera MD, Faught RE, Holmes GL, Magnus-Miller L, Bernstein P, Rose-Legatt A. Safety and tolerability of gabapentin as adjunctive therapy in a large, multicenter study. Epilepsia. 1999 Jul;40(7):965-72. doi: 10.1111/j.1528-1157.1999.tb00804.x[↩][↩]
- Bozikas V, Petrikis P, Gamvrula K, Savvidou I, Karavatos A. Treatment of alcohol withdrawal with gabapentin. Prog Neuropsychopharmacol Biol Psychiatry. 2002 Jan;26(1):197-9. doi: 10.1016/s0278-5846(01)00234-2[↩]
- Voris J, Smith NL, Rao SM, Thorne DL, Flowers QJ. Gabapentin for the treatment of ethanol withdrawal. Subst Abus. 2003 Jun;24(2):129-32. doi: 10.1080/08897070309511541[↩]
- Rustembegovic A, Sofic E, Tahirović I, Kundurović Z. A study of gabapentin in the treatment of tonic-clonic seizures of alcohol withdrawal syndrome. Med Arh. 2004;58(1):5-6.[↩]
- Mariani JJ, Rosenthal RN, Tross S, Singh P, Anand OP. A randomized, open-label, controlled trial of gabapentin and phenobarbital in the treatment of alcohol withdrawal. Am J Addict. 2006 Jan-Feb;15(1):76-84. doi: 10.1080/10550490500419110[↩]
- Bonnet U, Banger M, Leweke FM, Specka M, Müller BW, Hashemi T, Nyhuis PW, Kutscher S, Burtscheidt W, Gastpar M. Treatment of acute alcohol withdrawal with gabapentin: results from a controlled two-center trial. J Clin Psychopharmacol. 2003 Oct;23(5):514-9. doi: 10.1097/01.jcp.0000088905.24613.ad[↩]
- Malcolm R, Myrick LH, Veatch LM, Boyle E, Randall PK. Self-reported sleep, sleepiness, and repeated alcohol withdrawals: a randomized, double blind, controlled comparison of lorazepam vs gabapentin. J Clin Sleep Med. 2007 Feb 15;3(1):24-32.[↩]
- De Sousa A. The role of topiramate and other anticonvulsants in the treatment of alcohol dependence: a clinical review. CNS Neurol Disord Drug Targets. 2010 Mar;9(1):45-9. doi: 10.2174/187152710790966696[↩]
- Müller CA, Geisel O, Banas R, Heinz A. Current pharmacological treatment approaches for alcohol dependence. Expert Opin Pharmacother. 2014 Mar;15(4):471-81. doi: 10.1517/14656566.2014.876008[↩]
- Johnson BA. Recent advances in the development of treatments for alcohol and cocaine dependence: focus on topiramate and other modulators of GABA or glutamate function. CNS Drugs. 2005;19(10):873-96. doi: 10.2165/00023210-200519100-00005[↩]
- Rustembegovic A, Sofic E, Kroyer G. A pilot study of Topiramate (Topamax) in the treatment of tonic-clonic seizures of alcohol withdrawal syndromes. Med Arh. 2002;56(4):211-2.[↩]
- Choi EA, Ki SW, Kim SE, et al. The efficacy and safety of topiramate in the treatment of alcohol withdrawal. J Korean Neuropsychiatr Assoc. 2005;44:328–333.[↩]
- Krupitsky EM, Rudenko AA, Burakov AM, Slavina TY, Grinenko AA, Pittman B, Gueorguieva R, Petrakis IL, Zvartau EE, Krystal JH. Antiglutamatergic strategies for ethanol detoxification: comparison with placebo and diazepam. Alcohol Clin Exp Res. 2007 Apr;31(4):604-11. doi: 10.1111/j.1530-0277.2007.00344.x[↩]
- Johnson BA, Rosenthal N, Capece JA, Wiegand F, Mao L, Beyers K, McKay A, Ait-Daoud N, Anton RF, Ciraulo DA, Kranzler HR, Mann K, O’Malley SS, Swift RM; Topiramate for Alcoholism Advisory Board; Topiramate for Alcoholism Study Group. Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA. 2007 Oct 10;298(14):1641-51. doi: 10.1001/jama.298.14.1641[↩]
- Prior PL, Galduróz JC. Glutamatergic hyperfunctioning during alcohol withdrawal syndrome: therapeutic perspective with zinc and magnesium. Med Hypotheses. 2011 Sep;77(3):368-70. doi: 10.1016/j.mehy.2011.05.017[↩]
- Espay AJ. Neurologic complications of electrolyte disturbances and acid-base balance. Handb Clin Neurol. 2014;119:365-82. doi: 10.1016/B978-0-7020-4086-3.00023-0[↩]
- Galvin R, Bråthen G, Ivashynka A, Hillbom M, Tanasescu R, Leone MA; EFNS. EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. Eur J Neurol. 2010 Dec;17(12):1408-18. doi: 10.1111/j.1468-1331.2010.03153.x[↩]
- LaRoche SM, Shivdat-Nanhoe R. Subacute encephalopathy and seizures in alcoholics (SESA) presenting with non-convulsive status epilepticus. Seizure. 2011 Jul;20(6):505-8. doi: 10.1016/j.seizure.2011.02.008[↩]
- Talbot PA. Timing of efficacy of thiamine in Wernicke’s disease in alcoholics at risk. J Correct Health Care. 2011 Jan;17(1):46-50. doi: 10.1177/1078345810385913[↩]