Atonic seizure
Atonic seizure also known as “drop attacks” or “drop seizures”, where the person’s muscles suddenly relax and they become floppy 1. If they are standing they often fall, usually forwards, and may injure the front of their head or face. People may get injured when they fall. Head protection, such as a helmet or other protective gear, may be needed. Like tonic seizures, atonic seizures tend to be brief and happen without warning. Atonic seizures typically last less than 15 seconds. With both tonic and atonic seizures people usually recover quickly, apart from possible injuries. Atonic seizure was first described as a postepileptic paralytic phenomenon and is now well known as Todd’s paralysis 2. Atonic seizures usually begin in childhood and may last into adult years 3. Often atonic seizures may be seen in syndromes like Lennox-Gastaut or Dravet syndrome. Other types of seizures may occur in the same person too.
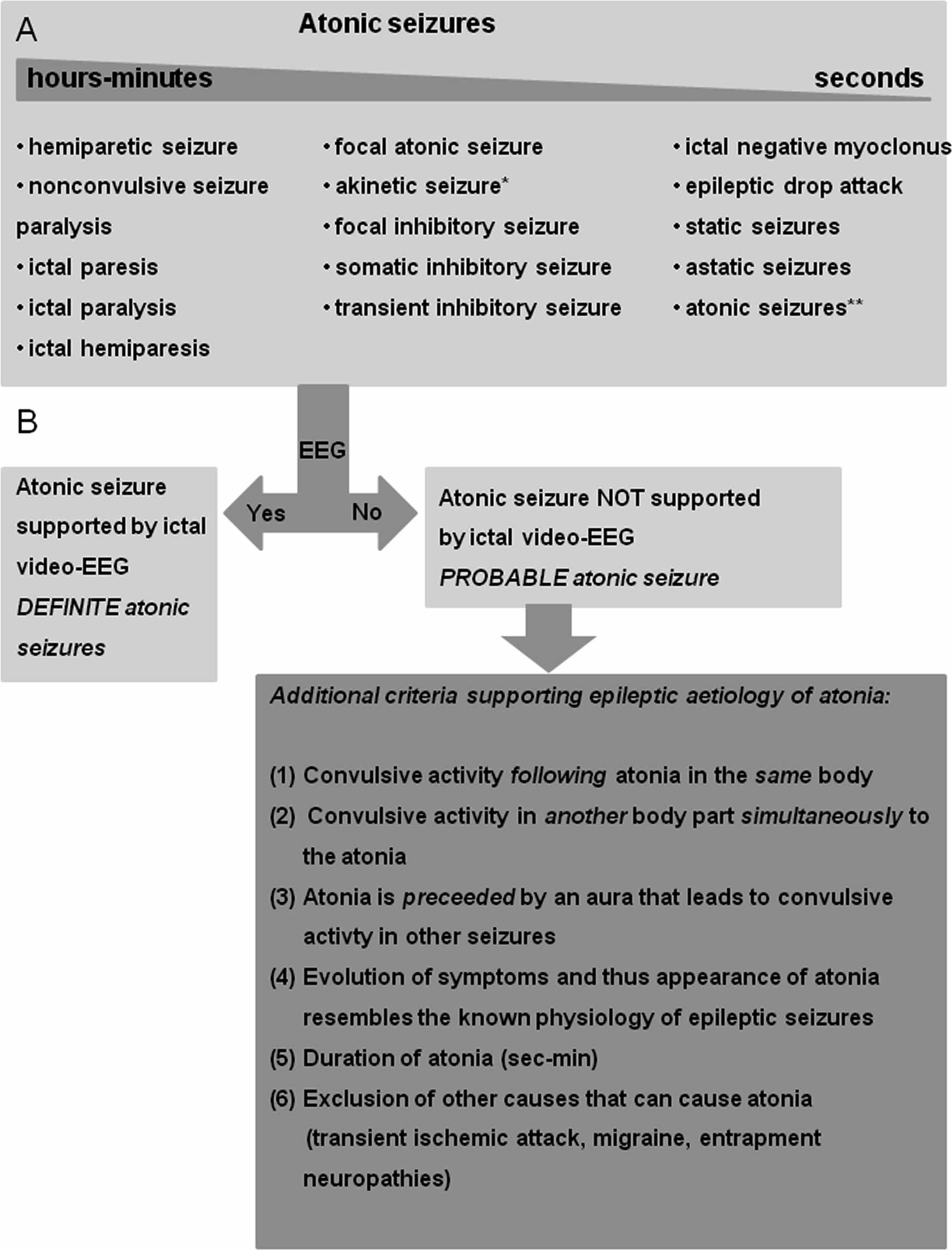
Atonic seizures are often seen in patients with generalized epilepsies and have been traditionally thought of as a clinical manifestation of generalized seizures, classified under the subheadings of generalized epilepsies 4. In these generalized epilepsies, as in myoclonic astatic epilepsy of childhood, atonia is mainly involving trunk muscles leading to seizure induced falls 5. However, atonia has also been observed in patients with focal epilepsy, mainly manifesting as limb atonia 6. Recognition of atonia as a manifestation of focal seizures is important in order to not mislabel these events as part of generalized epilepsy or even as non-epileptic. Moreover, a large proportion of patients with focal epilepsy, in some cases presenting with atonia, are referred for presurgical evaluation of intractable seizures. Currently, such an episode of atonia during an epileptic seizure is increasingly recognized as an ictal event. Focal atonic seizures are partial seizures in which the ictal manifestation consists of paresis or paralysis of one or more parts of the body 7.
If you think your loved one or you may be having atonic seizures, it is important to talk to your health care provider right away. These seizures have the potential to cause serious injury due to falls. Seek help to get an accurate diagnosis and treatment plan.
In the video below a man has an atonic seizure while out walking with his girlfriend.
Figure 1. Atonic seizures definition
[Source 8 ]Atonic seizure causes
The cause of atonic seizures is currently unknown. Precise pathophysiological and anatomical insight into the neuronal activity underlying the clinical manifestation of atonia can be gained by intracranial recording of spontaneous atonic seizures or from cortical stimulations, either intra- or extracranial, eliciting atonia. Atonic seizures are best defined with simultaneous electroencephalogram (EEG) recordings and the semiology of focal atonic seizures includes both limb atonia and trunk atonia. The different concepts on the pathophysiology underlying atonic seizures involve negative motor and primary motor area activation and activation of corticoreticulospinal pathways; however, the exact mechanisms are not fully understood 8. Further clinical and experimental characterization of this enigmatic semiology will improve the understanding of atonic seizures and therefore might aid in correctly localizing this seizure semiology in patients with pharmacoresistant epilepsy 8.
When atonic seizure starts in one area of the brain:
- Atonic seizures can start in one part of the brain with a loss of tone in one part of the body. This is called a focal motor atonic seizure.
When atonic seizure starts on both sides of the brain:
- Usually, atonic seizures affect both sides of the brain. These are called generalized onset atonic seizures. These seizures would begin with a sudden drop or loss of tone affecting the head, trunk, or whole body. Usually a person having a generalized atonic seizure is not fully aware during the event.
Atonic seizure symptoms
In an atonic seizure, the person’s body will suddenly become limp.
- If sitting, their head or upper body may slump over.
- If standing, the person many fall limply to the ground. Since the muscles are weak or limp, the person falls like a rag doll.
- When a person’s muscles are stiff or rigid, they will fall like a tree trunk. These are usually called tonic seizures.
After an atonic seizure, the person may or may not be confused. Often a person can return to their usual activity fairly quickly. Some may need to rest for a while after a seizure.
If the person fell, they may have been injured and need first aid for bruises, cuts, or other injuries. For serious injuries (like a broken bone or head injury), the person will need to go to an emergency room.
How often do atonic seizures occur?
It depends. People can have just one atonic seizure or several in a row. When an atonic seizure happens, try your best to make sure the person is in a safe place to prevent injuries and falls.
In some types of epilepsy like Lennox-Gastaut or Dravet syndrome, seizures can happen in clusters with two or more at one time or in one day. If a person is at risk for seizure clusters, they should talk to their doctor or nurse about ways to treat clusters.
Atonic seizure diagnosis
A number of tests are used to determine whether a person has a form of epilepsy and, if so, what kind of seizures the person has.
Imaging and monitoring
An electroencephalogram or EEG, can assess whether there are any detectable abnormalities in the person’s brain waves and may help to determine if antiseizure drugs would be of benefit. This most common diagnostic test for epilepsy records electrical activity detected by electrodes placed on the scalp. Some people who are diagnosed with a specific syndrome may have abnormalities in brain activity, even when they are not experiencing a seizure. However, some people continue to show normal electrical activity patterns even after they have experienced a seizure. These occur if the abnormal activity is generated deep in the brain where the EEG is unable to detect it. Many people who do not have epilepsy also show some unusual brain activity on an EEG. Whenever possible, an EEG should be performed within 24 hours of an individual’s first seizure. Ideally, EEGs should be performed while the person is drowsy as well as when he or she is awake because brain activity during sleep and drowsiness is often more revealing of activity resembling epilepsy. Video monitoring may be used in conjunction with EEG to determine the nature of a person’s seizures and to rule out other disorders such as psychogenic non-epileptic seizures, cardiac arrhythmia, or narcolepsy that may look like epilepsy.
A magnetoencephalogram (MEG) detects the magnetic signals generated by neurons to help detect surface abnormalities in brain activity. Magnetoencephalogram can be used in planning a surgical strategy to remove focal areas involved in seizures while minimizing interference with brain function.
The most commonly used brain scans include CT (computed tomography), PET (positron emission tomography) and MRI (magnetic resonance imaging). CT and MRI scans reveal structural abnormalities of the brain such as tumors and cysts, which may cause seizures. A type of MRI called functional MRI (fMRI) can be used to localize normal brain activity and detect abnormalities in functioning. SPECT (single photon emission computed tomography) is sometimes used to locate seizure foci in the brain. A modification of SPECT, called ictal SPECT, can be very helpful in localizing the brain area generating seizures. In a person admitted to the hospital for epilepsy monitoring, the SPECT blood flow tracer is injected within 30 seconds of a seizure, then the images of brain blood flow at the time of the seizure are compared with blood flow images taken in between seizures. The seizure onset area shows a high blood flow region on the scan. PET scans can be used to identify brain regions with lower than normal metabolism, a feature of the epileptic focus after the seizure has stopped.
Medical history
Taking a detailed medical history, including symptoms and duration of the seizures, is still one of the best methods available to determine what kind of seizures a person has had and to determine any form of epilepsy. The medical history should include details about any past illnesses or other symptoms a person may have had, as well as any family history of seizures. Since people who have suffered a seizure often do not remember what happened, caregiver or other accounts of seizures are vital to this evaluation. The person who experienced the seizure is asked about any warning experiences. The observers will be asked to provide a detailed description of events in the timeline they occurred.
Blood tests
Blood samples may be taken to screen for metabolic or genetic disorders that may be associated with the seizures. They also may be used to check for underlying health conditions such as infections, lead poisoning, anemia, and diabetes that may be causing or triggering the seizures. In the emergency department it is standard procedure to screen for exposure to recreational drugs in anyone with a first seizure.
Developmental, neurological, and behavioral tests
Tests devised to measure motor abilities, behavior, and intellectual ability are often used as a way to determine how epilepsy is affecting an individual. These tests also can provide clues about what kind of epilepsy the person has.
Atonic seizures treatment
A variety of seizure medicines can be used to treat atonic seizures, including valproic acid, topiramate, zonisamide, levetiracetam, lamotrigine, clonazepam, chlorazepate, lorazepam, clobazam, rufinamide, felbamate, and sometimes others. However, medicines often have limited effectiveness against atonic seizures. Since atonic seizures are common in people with Lennox-Gastaut syndrome, some new seizure medicines specific for this syndrome may help. When medicines don’t work, dietary therapies (ketogenic, low glycemic, or modified Atkins diet), vagus nerve stimulation, or the split-brain operation (callosotomy) may help. Which therapy to try depends in part on whether seizures start in one area or both sides of the brain.
People who have frequent atonic seizures without warning may need protective headgear or helmet. If they fall forward and injure the face frequently, a face mask or helmet to prevent facial injury should be considered.
Think of other ways to prevent injury. For example:
- Use a gaitbelt when walking with someone (the other person can hold onto the person with seizures by holding the back of the belt)
- Use a wheelchair instead of walking long distances, on hard surfaces, or when at high risk for falls
- Use other protective padding (elbow or knee pads)
- Blume W.T., Lüders H.O., Mizrahi E., Tassinari C., van Emde Boas W., Engel J. Glossary of descriptive terminology for ictal semiology: report of the ILAE Task Force on Classification and Terminology. Epilepsia. 2001;42:1212–1218.[↩]
- Kang MJ, Choi JY, An YS, et al. A patient with atonic seizures mimicking transient ischemic attacks. Epilepsy Behav Case Rep. 2015;3:30–32. Published 2015 Apr 2. doi:10.1016/j.ebcr.2015.03.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4389206[↩]
- Atonic seizures. https://www.epilepsy.com/learn/types-seizures/atonic-seizures[↩]
- Proposal for revised clinical electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia. 1981; 22: 489–501[↩]
- Doose, H. Myoclonic astatic epilepsy of early childhood. in: J. Roger, C. Dravet, M. Bureau, F.E. Dreifuss, P. Wolf (Eds.) Epileptic syndromes in infancy, childhood and adolescence. John Libbey Eurotext, London; 1985: 78–88[↩]
- Noachtar, Soheyl, Luders, and Hans, O. Akinetic seizures. The epileptic seizures: pathophysiology and clinical semiology. Churchill Livingstone, New York; 2000[↩]
- Kovac S., Diehl B. Atonic phenomena in focal seizures: nomenclature, clinical findings and pathophysiological concepts. Seizure. 2012;21:561–567. https://doi.org/10.1016/j.seizure.2012.06.004[↩]
- Atonic phenomena in focal seizures: Nomenclature, clinical findings and pathophysiological concepts. Kovac, Stjepana et al. Seizure – European Journal of Epilepsy, Volume 21, Issue 8, 561 – 567 https://doi.org/10.1016/j.seizure.2012.06.004[↩][↩][↩]