Bence Jones protein
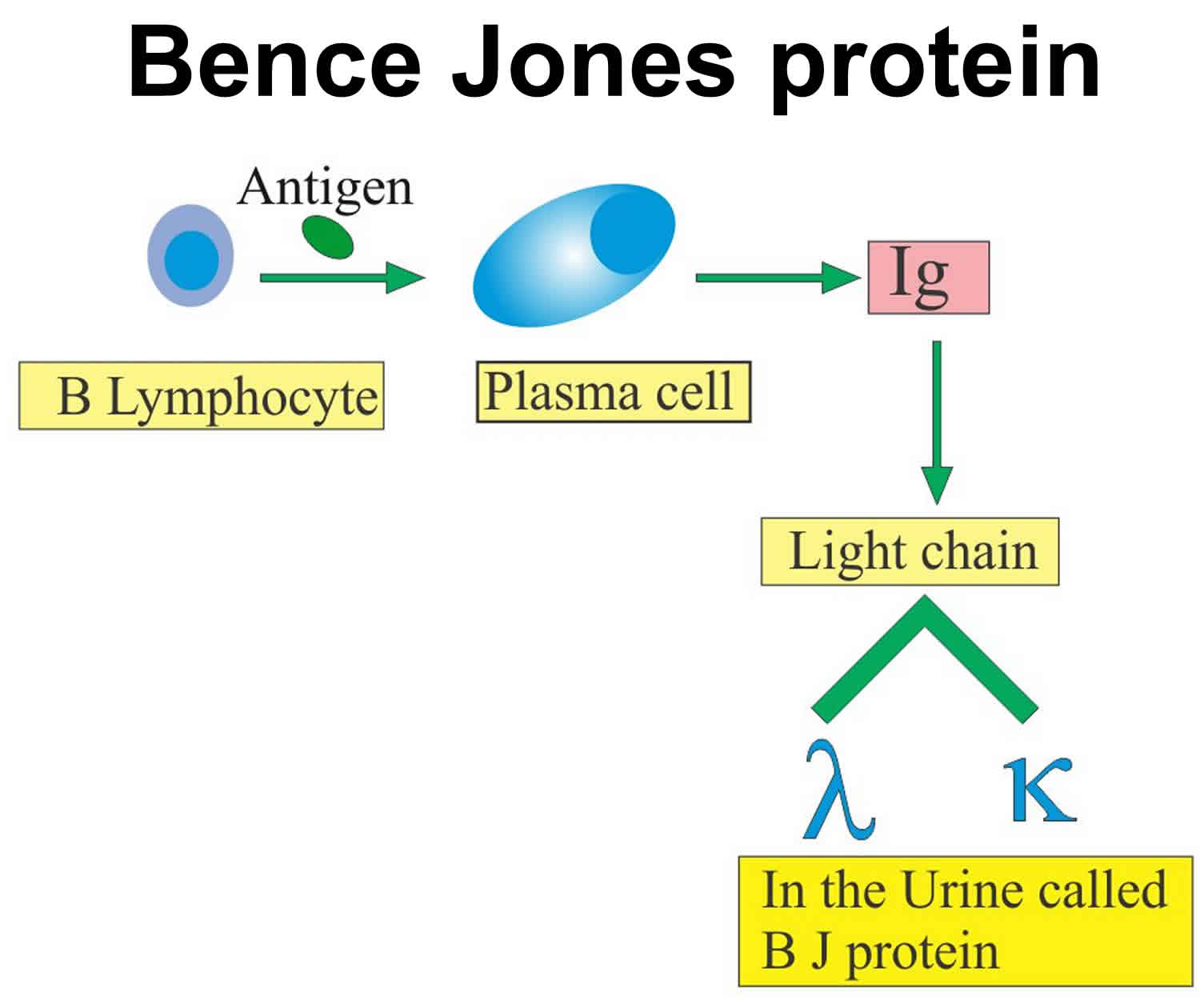
Bence Jones protein is known as the light chain of monoclonal immunoglobulin protein (also called paraprotein or myeloma components) without the accompanying heavy chain and can be accurately quantified by electrophoretic techniques including immunofixation electrophoresis 1. The other crucial point is that Bence Jones protein is undetectable by dipsticks used to detect proteinuria since they detect albumin and not Bence Jones protein. Bence Jones protein may be found in the urine of people with certain forms of protein disorders, such as amyloidosis and multiple myeloma. In most cases of multiple myeloma, a single type of intact (whole) immunoglobulin is produced in excess. In a minority of cases, only one section of an immunoglobulin called a “free light chain” (paraproteins) is produced in large amounts. These excess free light chains proteins are released into the bloodstream and since they are relatively small molecules, they are filtered by the kidneys and released into the urine. Another term for these excess free light chains of immunoglobulins (kappa κ or lambda λ) in the urine of multiple myeloma patient which is called Bence-Jones protein. Bence Jones protein are single peptide chain with a molecular weight of 20,000 and the kidney metabolizes Bence Jones protein through the processes of glomerular filtration, proximal renal tubular absorption, and renal catabolism. Bence Jones proteins spill into the urine once capacity for tubular absorption becomes saturated 2. Normally Bence Jones proteins are not found in the urine.
Bence Jones protein may be seen in tumor metastasis to bone, multiple myeloma, chronic lymphocytic leukemia, lymphoma, macroglobulinemia, and amyloidosis.
Bence Jones proteins are very small in size so easily filtered from the kidney glomeruli and can be detected in urine and difficult to find in the blood. Bence Jones proteins are present in the serum as tetramers. Bence Jones protein or free light chains, are found in the urine as low molecular weight monomers, dimers, or high molecular weight polymers. So urine sample is used.
Testing for Bence Jones protein in urine is indicated when plasma cell disorders such as multiple myeloma are suspected. Patient signs and symptoms that may prompt testing include anemia, hypercalcemia, and renal impairment. Bone manifestations such as painful lytic lesions and vertebral crush and long bone fractures are also indications. Increased suspicion for disorders such as multiple myeloma may also be prompted by symptoms of hyperviscosity like blurred vision, headaches, and epistaxis, as well as increased susceptibility to infection. Unfortunately, patients will initially present with nonspecific symptoms such as fatigue and back pain, which can often delay diagnostic testing such as assessing urine for Bence Jones proteinuria 3.
At least 60% of patients with classical myeloma have Bence Jones protein in their urine. More importantly, 20% of patients with multiple myeloma produce Bence Jones Proteins (light chains) only in the serum and urine without any heavy chains. Excessive secretion of Bence Jones Proteins causes acute kidney injury from tubular obstruction and tubulointerstitial inflammation, termed tubular nephropathy. Tubular damage results in the Fanconi syndrome with glycosuria, aminoaciduria, phosphaturia, and renal tubular acidosis type 2 3.
Presence of Bence Jones proteinuria significantly raises suspicion for multiple myeloma and warrants referral to a hematology clinic. Bone marrow aspiration for plasma cells and investigation for Bence Jones protein are also significant markers for prognostic progression regarding the treatment of multiple myeloma. Plasma cells in multiple myeloma can present in various forms, including as a mature, normal plasma cell, demonstrating features of immaturity such as a low cytoplasmic-nuclear ratio or loose chromatin, or present as bizarre “flame cells” with red cytoplasm. Bone marrow in patients with multiple myeloma generally is hypercellular and infiltrated diffusely by plasma cells 4. Clonal bone marrow plasma cells equal to or greater than 10% or biopsy-proven or extramedullary plasmacytoma are criteria for the diagnosis of multiple myeloma 5. More specifically, changes in the level of urinary light chain excretion can assess response to therapy. Direct positive effects on the treatment of multiple myeloma are defined as a reduction to 50% or less of the pretreatment value of urinary M-protein 3. In patients with Waldenstrom macroglobulinemia and amyloidosis, Bence Jones protein can also be present and crucial in the diagnosis. In amyloidosis, immunofixation electrophoresis is superior to the serum free light chain assay for detecting light chains 6.
Testing for Bence Jones protein and interpreting its clinical implications is best accomplsihed by an interprofessional team that includes multiple health care professionals including physicians, nursing (particularly onconolgy specialy nurses), and laboratory persoinnel.
Bence Jones proteins are presented in two forms:
- Monoclonal gammopathy.
- In free light chain disease.
Bence Jones protein in urine test uses:
- Bence Jones protein in urine test will help in the diagnosis of multiple myeloma.
- Bence Jones protein in urine test may be used to monitor the treatment of multiple myelomas.
- This may be seen in Waldenstrom’s Macroglobulinemia.
Bence Jones protein present in serum or urine or both depends upon the kidney function like:
- Filtration.
- Reabsorption.
- Catabolism.
Bence Jones protein in urine causes
Bence Jones protein may be found in:
- Bence Jones protein are present in 75% of multiple myeloma patients.
- Chronic lymphocytic leukemia.
- Lymphoma.
- Amyloidosis.
- Waldenstrom macroglobulinemia.
- Monoclonal gammopathy of unknown significance.
- Tumor metastasis to the bone.
False urine test
- Bence Jones protein may be seen in connective tissue diseases, renal diseases, and some malignancies.
- Dilute urine may give a false negative result.
Polyclonal light chains, usually kappa, tend to produce a characteristic banding pattern after electrophoresis and immunofixation electrophoresis. These light chain ladders are not Bence Jones proteins but commonly appear in urine samples of elderly populations suffering from tubular proteinuria due to inflammatory disease. Moreover, Bence Jones Proteins can sometimes co-migrate with the bands in these ladders. These ladders must be carefully examined to ensure that there are no concomitant Bence Jones proteins. However, the clinical presentation and other investigative findings help confirm the presence of Bence Jones protein 2.
Bence Jones protein in urine significance
Bence Jones protein is a monoclonal globulin protein found in the blood or urine. The isolated finding of a Bence Jones protein is known as monoclonal gammopathy of uncertain significance (MGUS). Finding this protein in the context of end-organ manifestations such as renal failure, lytic bone disease, or anemia, or large numbers of plasma cells in the bone marrow of patients can be diagnostic of multiple myeloma.
The proteins are antibody immunoglobulin free light chains (paraproteins) and are produced by neoplastic plasma cells. The light chains can be detected by heating or electrophoresis of concentrated urine. Light chains precipitate when heated to 50 – 60 degrees Celsius and redisolve at 90 -100 degrees Celsius. These tests are essential in patients suspected of having Bence Jones proteins in their urine as these proteins don’t react with the reagents normally utilized in urinalysis dipsticks. This leads to false negative results in people with Bence Jones proteins in their urine undergoing standard urinalysis. There are various rarer conditions which can produce Bence Jones proteins, such as Waldenström’s macroglobulinemia and other malignanices.
Bence Jones protein test procedure
A clean catch early morning urine sample is needed to screen for Bence Jones proteins by urine protein electrophoresis and immunofixation electrophoresis. A 24-hour urine catch is desirable to accurately quantify the amount of Bence Jones protein excreted since it aids in the diagnosis of multiple myeloma. This specimen requires no preservative and can be kept at room temperature 7.
- Bence Jones protein test is done on the urine of the patient.
- First-morning sample around 50 mL, uncontaminated urine in the container.
- To know the amount, 24 hours urine sample may be collected.
- Morning sample may be advised.
- If there is a delay then refrigerate the sample.
Precautions
- Avoid dilute urine.
- If there is a delay for the test then refrigerate the sample.
- Avoid heat because heat-coagulable protein can decompose, will cause a positive result.
Urine tests for Bence Jones light chains protein:
- To perform the heat test:
- The urine must first be acidified by adding 1 ml of 2 molar acetate buffer to 4 ml of filtered urine.
- These proteins (light chains immunoglobulins) soluble at room temperature.
- Precipitate at 60 °C 8.
- Again disappear (redissolve) at boiling temperature or at 80°C.
- Protein precipitation test: The sulphosalicylic acid positive test used for the quantitation of protein excreted in 24 hours of urine.
- Urine immunofixation electrophoresis (preferable) or immunoelectrophoresis is the definitive test that allows differentiation between Kappa and Lambda chains in the urine.
- This test may negative with the urine routine test strips.
Methods for detection of Bence Jone proteins include conventional high-resolution electrophoresis or capillary zone electrophoresis followed by confirmation through immunofixation electrophoresis (preferable) or immunoelectrophoresis.
The various electrophoretic methods are conducted on a medium of agarose and cellulose acetate. Differences between these methods arise regarding the volume of sample loaded and sensitivity of protein stain utilized. Depending on these characteristics, patient urine must be concentrated before analysis to ensure appropriate sensitivity. Coomassie Blue and Colloidal Gold serve as the stains used to detect Bence Jones proteinuria. Colloidal Gold is the most sensitive stain but has drawbacks such as demanding technique and lack of stoichiometry between uptake by Bence Jones protein and by other proteins 2.
After gel electrophoresis, follow-up immunofixation electrophoresis serves as immunologic confirmation of potential Bence Jones proteinuria type ( kappa or lambda) and is the most sensitive measure of Bence Jones protein. Immunofixation electrophoresis follows with antisera to IgG, IgA, IgM, total kappa, and total lambda. In the instances of a monoclonal protein visualized without a corresponding heavy chain, additional immunofixation gel with antisera to delta and epsilon heavy chains can be performed but is not cost effective. The issue of antigen excess with immunofixation electrophoresis can be minimized through decreased initial loading of antigen. Immunoblotting is an alternative to immunofixation electrophoresis but is more cumbersome and is not common practice in clinical laboratories 6.
An advance in the field is the ability to accurately measure free light chains by immunoassay and express them as a ratio. This test, the free light chain assay, is now used routinely to diagnose and monitor patients with plasma cell dyscrasias. The International Myeloma Working Group now suggests using serum free light chain assay instead of urine protein electrophoresis and immunofixation electrophoresis if multiple myeloma is suspected. Quantitative free light chain assays utilize antisera directed against epitopes that are exposed only when light chains are free. Kappa and lambda free light chain concentrations are quantified, and the ratio of kappa to lambda is used to determine unbalanced light chain synthesis. The free light chain assay is a significant addition to the clinical management of plasma cell dyscrasias due to its increased sensitivity for the determination of serum free light chains compared to previous methods. It also is a better marker of early remission and early relapse of multiple myeloma and prognostic marker for identification of risk of progression of monoclonal gammopathy of undetermined significance and smoldering myeloma. Its short physiologic half-life allows the free light chain assay to be a useful tool for real-time monitoring for response to treatment and disease progression 9. However the free light chain assay has pitfalls including the prozone phenomena of antigen excess, excess variability, and non-linearity and hence immunofixation electrophoresis of urine is a valuable test for light chains 10.
Overall, in light of the discussion of these various procedures, utilization of serum protein electrophoresis and free light chain assay will diagnose 100% of cases of multiple myeloma. This combination of testing poses as a cost-effective and accurate modality for many laboratories worldwide 9. However, the immunofixation electrophoresis detection of Bence Jones protein, commonly lambda light chains, is still required to detect amyloidosis 6.
- Ramakrishnan N, Jialal I. Bence-Jones Protein. [Updated 2019 Apr 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541035[↩]
- Beetham R. Detection of Bence-Jones protein in practice. Ann. Clin. Biochem. 2000 Sep;37 ( Pt 5):563-70.[↩][↩][↩]
- Smith D, Yong K. Multiple myeloma. BMJ. 2013 Jun 26;346:f3863.[↩][↩][↩]
- Albagoush SA, Azevedo AM. Cancer, Multiple Myeloma. [Updated 2019 Mar 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534764[↩]
- Rajkumar SV. Multiple myeloma: 2016 update on diagnosis, risk-stratification, and management. Am. J. Hematol. 2016 Jul;91(7):719-34.[↩]
- Willrich MA, Katzmann JA. Laboratory testing requirements for diagnosis and follow-up of multiple myeloma and related plasma cell dyscrasias. Clin. Chem. Lab. Med. 2016 Jun 01;54(6):907-19.[↩][↩][↩]
- Kaplan JS, Horowitz GL. Twenty-four-hour Bence-Jones protein determinations: can we ensure accuracy? Arch. Pathol. Lab. Med. 2011 Aug;135(8):1048-51.[↩]
- Ribatti D. A historical perspective on milestones in multiple myeloma research. Eur. J. Haematol. 2018 Mar;100(3):221-228.[↩]
- Bhole MV, Sadler R, Ramasamy K. Serum-free light-chain assay: clinical utility and limitations. Ann. Clin. Biochem. 2014 Sep;51(Pt 5):528-42.[↩][↩]
- Jialal I, Pahwa R, Beck RC, Schmotzer CL. Therapeutic Monoclonal Antibodies and the Value of the Free Light Chain Assay in Myeloma. Am. J. Clin. Pathol. 2018 Oct 01;150(5):468-469.[↩]