What is benign prostatic hypertrophy
Benign prostatic hypertrophy (BPH) also called benign prostatic hyperplasia or prostate gland enlargement. Most men will get BPH as they get older. An enlarged prostate gland can cause uncomfortable urinary symptoms, such as blocking the flow of urine out of the bladder. Benign prostatic hypertrophy symptoms often start after age 50. Benign prostatic hypertrophy can also cause bladder, urinary tract or kidney problems.
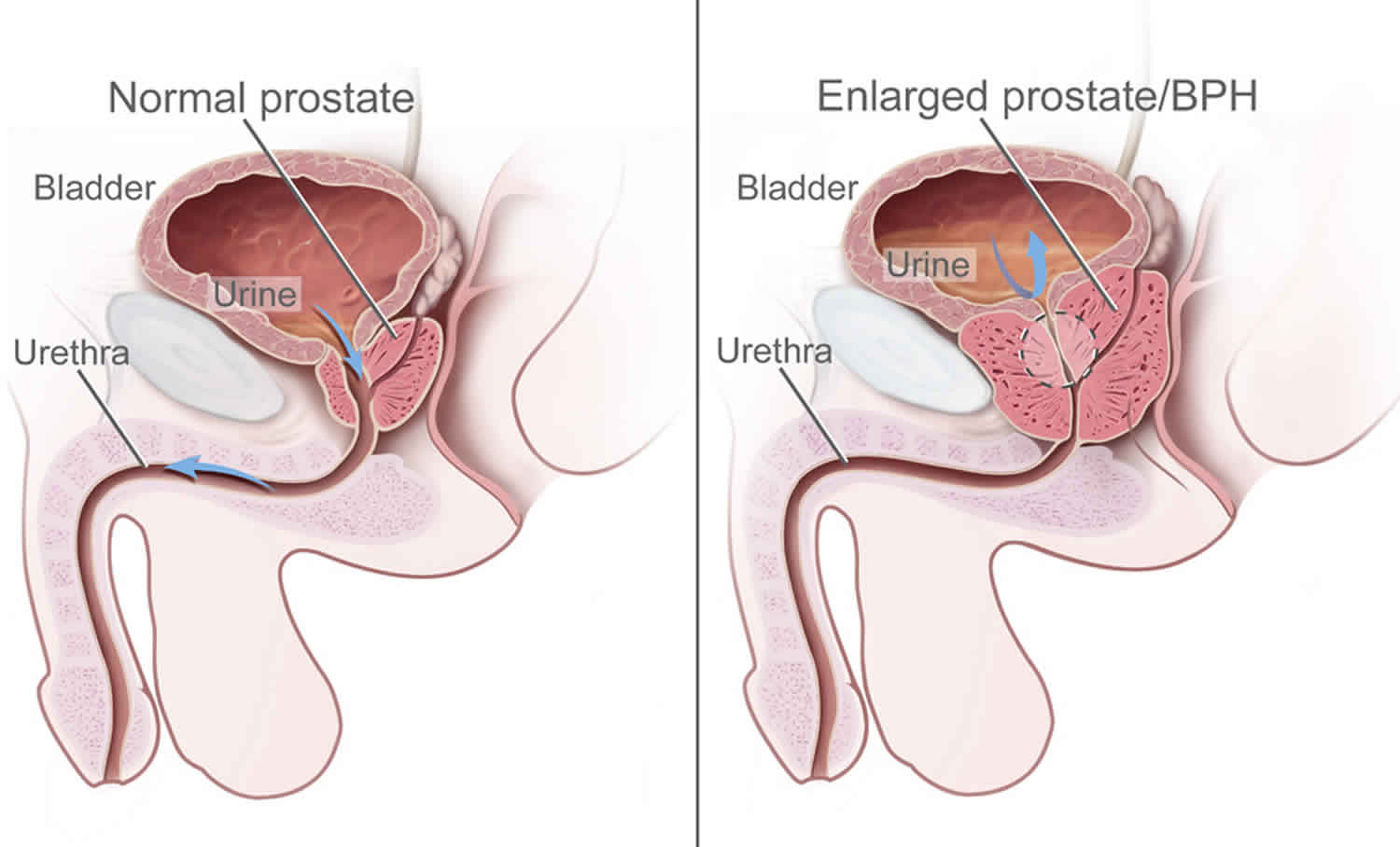
The prostate is a gland in men. It helps make semen, the fluid that contains sperm. The prostate gland is located beneath your bladder. The tube that transports urine from the bladder out of your penis (urethra) passes through the center of the prostate. As men age, their prostate grows bigger. If it gets too large, it begins to block urine flow.
Benign prostatic hypertrophy is the most common prostate problem for men older than age 50. In 2010, as many as 14 million men in the United States had lower urinary tract symptoms suggestive of benign prostatic hypertrophy 1. Although benign prostatic hypertrophy rarely causes symptoms before age 40, the occurrence and symptoms increase with age. Benign prostatic hypertrophy affects about 50 percent of men between the ages of 51 and 60 and up to 90 percent of men older than 80 2.
Benign prostatic hypertrophy is not cancer and it does not seem to increase your chance of getting prostate cancer. But the early symptoms are the same. Check with your doctor if you have:
- A frequent and urgent need to urinate, especially at night
- Trouble starting a urine stream or making more than a dribble
- A urine stream that is weak, slow, or stops and starts several times
- The feeling that you still have to go, even just after urinating
- Small amounts of blood in your urine
Benign prostatic hypertrophy means the prostate gland has grown bigger. As the prostate gland grows, it can block the urethra and cause problems, such as:
- Not being able to fully empty your bladder
- Needing to urinate two or more times per night
- Slowed or delayed start of the urinary stream and dribbling at the end
- Straining to urinate and weak urine stream
- Strong and sudden urge to urinate or a loss of urinary control
Severe benign prostatic hypertrophy can cause serious problems over time, such as urinary tract infections (UTIs) and bladder or kidney damage. If it is found early, you are less likely to develop these problems.
Tests for benign prostatic hypertrophy include a digital rectal exam, blood and imaging tests, a urine flow study, and examination with a scope called a cystoscope.
There are several effective treatments for benign prostatic hypertrophy, including medications, minimally invasive therapies and surgery. To choose the best option, you and your doctor will consider your symptoms, the size of your prostate, other health conditions you might have and your preferences.
A person may have urinary symptoms unrelated to benign prostatic hypertrophy that are caused by bladder problems, UTIs, or prostatitis—inflammation of the prostate. Symptoms of benign prostatic hypertrophy also can signal more serious conditions, including prostate cancer.
Men with symptoms of benign prostatic hypertrophy should see a health care provider.
See your doctor right away if you have:
- Complete inability to urinate
- Painful, frequent, and urgent need to urinate, with fever and chills
- Blood or pus in your urine
- Great discomfort or pain in the lower abdomen, back, side, and urinary tract
- Less urine than usual
- Fever or chills
Also see your doctor if:
- Your bladder does not feel completely empty after you urinate.
- You take medicines that may cause urinary problems. These may include diuretics, antihistamines, antidepressants, or sedatives. DO NOT stop or change your medicines without first talking to your doctor.
- You have taken tried self-care steps and your symptoms have not gotten better.
Benign prostatic hypertrophy causes
The cause of benign prostatic hypertrophy is not well understood; however, it occurs mainly in older men. Benign prostatic hypertrophy does not develop in men whose testicles were removed before puberty. For this reason, some researchers believe factors related to aging and the testicles may cause benign prostatic hypertrophy.
Throughout their lives, men produce testosterone, a male hormone, and small amounts of estrogen, a female hormone. As men age, the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen. Scientific studies have suggested that benign prostatic hypertrophy may occur because the higher proportion of estrogen within the prostate increases the activity of substances that promote prostate cell growth.
Another theory focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of dihydrotestosterone in the prostate. This accumulation of dihydrotestosterone may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce dihydrotestosterone do not develop benign prostatic hypertrophy.
Risk factors for benign prostatic hypertrophy
Risk factors for prostate gland enlargement include:
- Aging. Prostate gland enlargement rarely causes signs and symptoms in men younger than age 40. About one-third of men experience moderate to severe symptoms by age 60, and about half do so by age 80.
- Family history. Having a blood relative, such as a father or a brother, with prostate problems means you’re more likely to have problems.
- Diabetes and heart disease. Studies show that diabetes, as well as heart disease and use of beta blockers, might increase the risk of benign prostatic hypertrophy.
- Lifestyle. Obesity increases the risk of benign prostatic hypertrophy, while exercise can lower your risk.
Benign prostatic hypertrophy symptoms
The severity of symptoms in people who have benign prostatic hypertrophy varies, but symptoms tend to gradually worsen over time. Common signs and symptoms of BPH include:
- Frequent or urgent need to urinate
- Increased frequency of urination at night (nocturia)
- Difficulty starting urination
- Weak urine stream or a stream that stops and starts
- Dribbling at the end of urination
- Inability to completely empty the bladder
Less common signs and symptoms include:
- Urinary tract infection
- Inability to urinate
- Blood in the urine
The size of your prostate doesn’t necessarily determine the severity of your symptoms. Some men with only slightly enlarged prostates can have significant symptoms, while other men with very enlarged prostates can have only minor urinary symptoms.
In some men, symptoms eventually stabilize and might even improve over time.
Other possible causes of urinary symptoms
Conditions that can lead to symptoms similar to those caused by benign prostatic hypertrophy include:
- Urinary tract infection
- Inflammation of the prostate (prostatitis)
- Narrowing of the urethra (urethral stricture)
- Scarring in the bladder neck as a result of previous surgery
- Bladder or kidney stones
- Problems with nerves that control the bladder
- Cancer of the prostate or bladder
If you’re having urinary problems, discuss them with your doctor. Even if you don’t find urinary symptoms bothersome, it’s important to identify or rule out any underlying causes. Untreated, urinary problems might lead to obstruction of the urinary tract.
If you’re unable to pass any urine, seek immediate medical attention.
Benign prostatic hypertrophy complications
Complications of an enlarged prostate can include:
- Sudden inability to urinate (urinary retention). You might need to have a tube (catheter) inserted into your bladder to drain the urine. Some men with an enlarged prostate need surgery to relieve urinary retention.
- Urinary tract infections (UTIs). Inability to fully empty the bladder can increase the risk of infection in your urinary tract. If UTIs occur frequently, you might need surgery to remove part of the prostate.
- Bladder stones. These are generally caused by an inability to completely empty the bladder. Bladder stones can cause infection, bladder irritation, blood in the urine and obstruction of urine flow.
- Bladder damage. A bladder that hasn’t emptied completely can stretch and weaken over time. As a result, the muscular wall of the bladder no longer contracts properly, making it harder to fully empty your bladder.
- Kidney damage. Pressure in the bladder from urinary retention can directly damage the kidneys or allow bladder infections to reach the kidneys.
Most men with an enlarged prostate don’t develop these complications. However, acute urinary retention and kidney damage can be serious health threats.
Having an enlarged prostate is not believed to increase your risk of developing prostate cancer.
Benign prostatic hypertrophy diagnosis
Your doctor will start by asking detailed questions about your symptoms and doing a physical exam. This initial exam is likely to include:
- Digital rectal exam. The doctor inserts a finger into the rectum to check your prostate for enlargement.
- Urine test. Analyzing a sample of your urine can help rule out an infection or other conditions that can cause similar symptoms.
- Blood test. The results can indicate kidney problems.
- Prostate-specific antigen (PSA) blood test. PSA is a substance produced in your prostate. PSA levels increase when you have an enlarged prostate. However, elevated PSA levels can also be due to recent procedures, infection, surgery or prostate cancer.
After that, your doctor might recommend additional tests to help confirm an enlarged prostate and to rule out other conditions. These tests include:
- Urinary flow test. You urinate into a receptacle attached to a machine that measures the strength and amount of your urine flow. Test results help determine over time if your condition is getting better or worse.
- Postvoid residual volume test. This test measures whether you can empty your bladder completely. The test can be done using ultrasound or by inserting a catheter into your bladder after you urinate to measure how much urine is left in your bladder.
- 24-hour voiding diary. Recording the frequency and amount of urine might be especially helpful if more than one-third of your daily urinary output occurs at night.
If your condition is more complex, your doctor may recommend:
- Transrectal ultrasound. An ultrasound probe is inserted into your rectum to measure and evaluate your prostate.
- Prostate biopsy. Transrectal ultrasound guides needles used to take tissue samples (biopsies) of the prostate. Examining the tissue can help your doctor diagnose or rule out prostate cancer.
- Urodynamic and pressure flow studies. A catheter is threaded through your urethra into your bladder. Water — or, less commonly, air — is slowly injected into your bladder. Your doctor can then measure bladder pressure and determine how well your bladder muscles are working. These studies are usually used only in men with suspected neurological problems and in men who have had a previous prostate procedure and still have symptoms.
- Cystoscopy. A lighted, flexible instrument (cystoscope) is inserted into your urethra, allowing your doctor to see inside your urethra and bladder. You will be given a local anesthetic before this test.
Benign prostatic hypertrophy treatment
A wide variety of treatments are available for enlarged prostate, including medication, minimally invasive therapies and surgery. The best treatment choice for you depends on several factors, including:
- The size of your prostate
- Your age
- Your overall health
- The amount of discomfort or bother you are experiencing
If your symptoms are tolerable, you might decide to postpone treatment and simply monitor your symptoms. For some men, symptoms can ease without treatment.
Treatment options for benign prostatic hypertrophy may include:
- Lifestyle changes
- Medications
- Minimally invasive procedures
- Surgery
A health care provider treats benign prostatic hypertrophy based on the severity of symptoms, how much the symptoms affect a man’s daily life, and a man’s preferences.
Men may not need treatment for a mildly enlarged prostate unless their symptoms are bothersome and affecting their quality of life. In these cases, instead of treatment, a urologist may recommend regular checkups. If benign prostatic hypertrophy symptoms become bothersome or present a health risk, a urologist most often recommends treatment.
Lifestyle and home remedies
To help control the symptoms of an enlarged prostate, try to:
- Limit beverages in the evening. Don’t drink anything for an hour or two before bedtime to avoid middle-of-the-night trips to the toilet.
- Limit caffeine and alcohol. They can increase urine production, irritate the bladder and worsen symptoms.
- Limit decongestants or antihistamines. These drugs tighten the band of muscles around the urethra that control urine flow, making it harder to urinate.
- Go when you first feel the urge. Waiting too long might overstretch the bladder muscle and cause damage.
- Schedule bathroom visits. Try to urinate at regular times — such as every four to six hours during the day — to “retrain” the bladder. This can be especially useful if you have severe frequency and urgency.
- Follow a healthy diet. Obesity is associated with enlarged prostate.
- Stay active. Inactivity contributes to urine retention. Even a small amount of exercise can help reduce urinary problems caused by an enlarged prostate.
- Urinate — and then urinate again a few moments later. This practice is known as double voiding.
- Keep warm. Colder temperatures can cause urine retention and increase the urgency to urinate.
- Reduce stress. Nervousness and tension can lead to more frequent urination.
Learn about exercises (Kegel exercises) that strengthen the pelvic floor muscles. Doing these exercise may help with leaking or losing control of your urine. Once you have learned how to do these, you should perform them 3 times a day.
Medication
Medication is the most common treatment for mild to moderate symptoms of prostate enlargement. The options include:
- Alpha blockers. These medications relax bladder neck muscles and muscle fibers in the prostate, making urination easier. Alpha blockers — which include alfuzosin (Uroxatral), doxazosin (Cardura), tamsulosin (Flomax) and silodosin (Rapaflo) — usually work quickly in men with relatively small prostates. Most people find that these drugs help their symptoms. Symptoms often get better soon after starting on the medicine. You must take this medicine every day. Side effects might include dizziness and a harmless condition in which semen goes back into the bladder instead of out the tip of the penis (retrograde ejaculation). Ask your doctor before taking Sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis) with alpha- blockers because there can sometimes be an interaction.
- 5-alpha reductase inhibitors. These medications shrink your prostate by blocking the production of dihydrotestosterone, which accumulates in the prostate and may cause prostate growth. These medications — which include finasteride (Proscar) and dutasteride (Avodart) — might take up to six months to be effective. Finasteride and dutasteride act more slowly than alpha blockers and are useful for only moderately enlarged prostates. Side effects include retrograde ejaculation.
- Phosphodiesterase-5 inhibitors. Urologists prescribe these medications mainly for erectile dysfunction. Tadalafil (Cialis) belongs to this class of medications and can reduce lower urinary tract symptoms by relaxing smooth muscles in the lower urinary tract. Studies suggest this medication, which is often used to treat erectile dysfunction, can also treat prostate enlargement. Researchers are working to determine the role of erectile dysfunction drugs in the long-term treatment of benign prostatic hypertrophy.
- Combination drug therapy. Your doctor might recommend taking an alpha blocker and a 5-alpha reductase inhibitor at the same time if either medication alone isn’t effective. Several studies, such as the Medical Therapy of Prostatic Symptoms (MTOPS) study, have shown that combining two classes of medications, instead of using just one, can more effectively improve symptoms, urinary flow, and quality of life. The combinations include:
- finasteride and doxazosin
- dutasteride and tamsulosin (Jalyn), a combination of both medications that is available in a single tablet
- alpha blockers and antimuscarinics
- A urologist may prescribe a combination of alpha blockers and antimuscarinics for patients with overactive bladder symptoms. Overactive bladder is a condition in which the bladder muscles contract uncontrollably and cause urinary frequency, urinary urgency, and urinary incontinence. Antimuscarinics are a class of medications that relax the bladder muscles.
Minimally invasive or surgical therapy
Minimally invasive or surgical therapy might be recommended if:
- Your symptoms are moderate to severe
- Medication hasn’t relieved your symptoms
- You have a urinary tract obstruction, bladder stones, blood in your urine or kidney problems
- You prefer definitive treatment
Minimally invasive or surgical therapy might not be an option if you have:
- An untreated urinary tract infection
- Urethral stricture disease
- A history of prostate radiation therapy or urinary tract surgery
- A neurological disorder, such as Parkinson’s disease or multiple sclerosis
Any type of prostate procedure can cause side effects. Depending on the procedure you choose, complications might include:
- Semen flowing backward into the bladder instead of out through the penis during ejaculation (retrograde ejaculation)
- Temporary difficulty with urination
- Urinary tract infection
- Bleeding
- Erectile dysfunction
- Very rarely, loss of bladder control (incontinence)
There are several types of minimally invasive or surgical therapies.
Transurethral resection of the prostate (TURP)
A lighted scope is inserted into your urethra, and the surgeon removes all but the outer part of the prostate. TURP generally relieves symptoms quickly, and most men have a stronger urine flow soon after the procedure. After TURP you might temporarily need a catheter to drain your bladder.
Transurethral incision of the prostate (TUIP)
A lighted scope is inserted into your urethra, and the surgeon makes one or two small cuts in the prostate gland — making it easier for urine to pass through the urethra. This surgery might be an option if you have a small or moderately enlarged prostate gland, especially if you have health problems that make other surgeries too risky.
Transurethral microwave thermotherapy (TUMT)
Your doctor inserts a special electrode through your urethra into your prostate area. Microwave energy from the electrode destroys the inner portion of the enlarged prostate gland, shrinking it and easing urine flow. TUMT might only partially relieve your symptoms, and it might take some time before you notice results. This surgery is generally used only on small prostates in special circumstances because re-treatment might be necessary.
Transurethral needle ablation (TUNA)
In this procedure, a scope is passed into your urethra, allowing your doctor to place needles into your prostate gland. Radio waves pass through the needles, heating and destroying excess prostate tissue that’s blocking urine flow. TUNA may be an option in select cases, but the procedure is rarely used any longer.
Transurethral needle ablation
This procedure uses heat generated by radiofrequency energy to destroy prostate tissue. A urologist inserts a cystoscope through the urethra to the prostate. A urologist then inserts small needles through the end of the cystoscope into the prostate. The needles send radiofrequency energy that heats and destroys selected portions of prostate tissue. Shields protect the urethra from heat damage.
High-intensity focused ultrasound. For this procedure, a urologist inserts a special ultrasound probe into the rectum, near the prostate. Ultrasound waves from the probe heat and destroy enlarged prostate tissue.
Transurethral electrovaporization
For this procedure, a urologist inserts a tubelike instrument called a resectoscope through the urethra to reach the prostate. An electrode attached to the resectoscope moves across the surface of the prostate and transmits an electric current that vaporizes prostate tissue. The vaporizing effect penetrates below the surface area being treated and seals blood vessels, which reduces the risk of bleeding.
Water-induced thermotherapy
This procedure uses heated water to destroy prostate tissue. A urologist inserts a catheter into the urethra so that a treatment balloon rests in the middle of the prostate. Heated water flows through the catheter into the treatment balloon, which heats and destroys the surrounding prostate tissue. The treatment balloon can target a specific region of the prostate, while surrounding tissues in the urethra and bladder remain protected.
Prostatic stent insertion
This procedure involves a urologist inserting a small device called a prostatic stent through the urethra to the area narrowed by the enlarged prostate. Once in place, the stent expands like a spring, and it pushes back the prostate tissue, widening the urethra. Prostatic stents may be temporary or permanent. Urologists generally use prostatic stents in men who may not tolerate or be suitable for other procedures.
Laser therapy
A high-energy laser destroys or removes overgrown prostate tissue. Laser therapy generally relieves symptoms right away and has a lower risk of side effects than does nonlaser surgery. Laser therapy might be used in men who shouldn’t have other prostate procedures because they take blood-thinning medications.
The options for laser therapy include:
- Ablative procedures. These procedures vaporize obstructive prostate tissue to increase urine flow. Examples include photoselective vaporization of the prostate (PVP) and holmium laser ablation of the prostate (HoLAP). Ablative procedures can cause irritating urinary symptoms after surgery, so in rare situations another resection procedure might be needed at some point.
- Enucleative procedures. Enucleative procedures, such as holmium laser enucleation of the prostate (HoLEP), generally remove all the prostate tissue blocking urine flow and prevent regrowth of tissue. The removed tissue can be examined for prostate cancer and other conditions. These procedures are similar to open prostatectomy.
Prostatic urethral lift (PUL)
Special tags are used to compress the sides of the prostate to increase the flow of urine. The procedure might be recommended if you have lower urinary tract symptoms. Prostatic urethral lift also might be offered to some men concerned about treatment impact on erectile dysfunction and ejaculatory problems, since the effect on ejaculation and sexual function is much lower with prostatic urethral lift that it is with TURP.
Embolization
In this experimental procedure, the blood supply to or from the prostate is selectively blocked, causing the prostate to decrease in size. Long-term data on the effectiveness of this procedure aren’t available.
Open or robot-assisted prostatectomy
The surgeon makes an incision in your lower abdomen to reach the prostate and remove tissue. Open prostatectomy is generally done if you have a very large prostate, bladder damage or other complicating factors. The surgery usually requires a short hospital stay and is associated with a higher risk of needing a blood transfusion.
Follow-up care
Your follow-up care will depend on the specific technique used to treat your enlarged prostate.
Your doctor might recommend limiting heavy lifting and excessive exercise for seven days if you have laser ablation, transurethral needle ablation or transurethral microwave therapy. If you have open or robot-assisted prostatectomy, you might need to restrict activity for six weeks.
What are the complications of benign prostatic hypertrophy treatment?
The complications of benign prostatic hypertrophy treatment depend on the type of treatment.
Medications
Medications used to treat benign prostatic hypertrophy may have side effects that sometimes can be serious. Men who are prescribed medications to treat benign prostatic hypertrophy should discuss possible side effects with a health care provider before taking the medications. Men who experience the following side effects should contact a health care provider right away or get emergency medical care:
- hives
- rash
- itching
- shortness of breath
- rapid, pounding, or irregular heartbeat
- painful erection of the penis that lasts for hours
- swelling of the eyes, face, tongue, lips, throat, arms, hands, feet, ankles, or lower legs
- difficulty breathing or swallowing
- chest pain
- dizziness or fainting when standing up suddenly
- sudden decrease or loss of vision
- blurred vision
- sudden decrease or loss of hearing
- chest pain, dizziness, or nausea during sexual activity
These side effects are mostly related to phosphodiesterase-5 inhibitors. Side effects related to alpha blockers include:
- dizziness or fainting when standing up suddenly
- decreased sexual drive
- problems with ejaculation
Minimally Invasive Procedures
Complications after minimally invasive procedures may include
- UTIs
- painful urination
- difficulty urinating
- an urgent or a frequent need to urinate
- urinary incontinence
- blood in the urine for several days after the procedure
- sexual dysfunction
- chronic prostatitis—long-lasting inflammation of the prostate
- recurring problems such as urinary retention and UTIs
Most of the complications of minimally invasive procedures go away within a few days or weeks. Minimally invasive procedures are less likely to have complications than surgery.
Surgery
Complications after surgery may include
- problems urinating
- urinary incontinence
- bleeding and blood clots
- infection
- scar tissue
- sexual dysfunction
- recurring problems such as urinary retention and UTIs
Problems urinating. Men may initially have painful urination or difficulty urinating. They may experience urinary frequency, urgency, or retention. These problems will gradually lessen and, after a couple of months, urination will be easier and less frequent.
Urinary incontinence. As the bladder returns to normal, men may have some temporary problems controlling urination. However, long-term urinary incontinence rarely occurs. The longer urinary problems existed before surgery, the longer it takes for the bladder to regain its full function after surgery.
Bleeding and blood clots. After benign prostatic hypertrophy surgery, the prostate or tissues around it may bleed. Blood or blood clots may appear in urine. Some bleeding is normal and should clear up within several days. However, men should contact a health care provider right away if:
- they experience pain or discomfort
- their urine contains large clots
- their urine is so red it is difficult to see through
Blood clots from benign prostatic hypertrophy surgery can pass into the bloodstream and lodge in other parts of the body—most often the legs. Men should contact a health care provider right away if they experience swelling or discomfort in their legs.
Infection. Use of a Foley catheter after benign prostatic hypertrophy surgery may increase the risk of a UTI. Anesthesia during surgery may cause urinary retention and also increase the risk of a UTI. In addition, the incision site of an open prostatectomy may become infected. A health care provider will prescribe antibiotics to treat infections.
Scar tissue. In the year after the original surgery, scar tissue sometimes forms and requires surgical treatment. Scar tissue may form in the urethra and cause it to narrow. A urologist can solve this problem during an office visit by stretching the urethra. Rarely, the opening of the bladder becomes scarred and shrinks, causing blockage. This problem may require a surgical procedure similar to transurethral incision of the prostate (TUIP).
Sexual dysfunction. Some men may experience temporary problems with sexual function after benign prostatic hypertrophy surgery. The length of time for restored sexual function depends on the type of benign prostatic hypertrophy surgery performed and how long symptoms were present before surgery. Many men have found that concerns about sexual function can interfere with sex as much as the benign prostatic hypertrophy surgery itself. Understanding the surgical procedure and talking about concerns with a health care provider before surgery often help men regain sexual function earlier. Many men find it helpful to talk with a counselor during the adjustment period after surgery. Even though it can take a while for sexual function to fully return, with time, most men can enjoy sex again.
Most health care providers agree that if men with benign prostatic hypertrophy were able to maintain an erection before surgery, they will probably be able to have erections afterward. Surgery rarely causes a loss of erectile function. However, benign prostatic hypertrophy surgery most often cannot restore function that was lost before the procedure. Some men find a slight difference in the quality of orgasm after surgery. However, most report no difference.
Prostate surgery may make men sterile, or unable to father children, by causing retrograde ejaculation—the backward flow of semen into the bladder. Men flush the semen out of the bladder when they urinate. In some cases, medications such as pseudoephedrine, found in many cold medications, or imipramine can treat retrograde ejaculation. These medications improve muscle tone at the bladder neck and keep semen from entering the bladder.
Recurring problems. Men may require further treatment if prostate problems, including benign prostatic hypertrophy, return. Problems may arise when treatments for benign prostatic hypertrophy leave a good part of the prostate intact. About 10 percent of men treated with transurethral resection of the prostate (TURP) or transurethral incision of the prostate (TUIP) require additional surgery within 5 years. About 2 percent of men who have an open prostatectomy require additional surgery within 5 years.
In the years after benign prostatic hypertrophy surgery or treatment, men should continue having a digital rectal exam once a year and have any symptoms checked by a health care provider. In some cases, the health care provider may recommend a digital rectal exam and checkup more than once a year.
References