Beriberi
Beriberi is a condition that occurs in people who are deficient in thiamin (vitamin B1). There are two major types of beriberi: wet beriberi which affects the cardiovascular system and dry beriberi which affects the nervous system 1. People with wet beriberi may experience increased heart rate, shortness of breath, and swelling of the lower legs 2. Signs and symptoms of dry beriberi include difficulty walking; loss of feeling in the hands and/or feet; paralysis of the lower legs; mental confusion; speech difficulty; pain; and/or vomiting.
There are two major types of beriberi:
- Wet beriberi: Affects the cardiovascular system.
- Dry beriberi and Wernicke-Korsakoff syndrome: Affects the nervous system.
Beriberi can occur in infants when they are:
- Breastfed and the mother’s body is lacking in thiamine
- Fed unusual formulas that don’t have enough thiamine
Some medical treatments that can raise your risk of beriberi are:
- Getting dialysis
- Taking high doses of diuretics (water pills)
Beriberi is rare in the United States since many foods are now vitamin enriched; however, alcohol abuse, dialysis and taking high doses of diuretics increases the risk of developing the condition 3. In most cases, beriberi occurs sporadically in people with no family history of the condition. A rare condition known as genetic beriberi is inherited (passed down through families) and is associated with an inability to absorb thiamine from foods. Beriberi treatment generally includes thiamine supplementation, given by injection or taken by mouth. With treatment, symptoms usually improve quickly.
Untreated, beriberi can be fatal. Heart damage is usually reversible. A full recovery is expected in these cases. However, if acute heart failure has already occurred, the outlook is poor. Nervous system damage is also reversible, if caught early. If it is not caught early, some symptoms such as memory loss may remain even with treatment.
If a person with Wernicke encephalopathy receives thiamine replacement, language problems, unusual eye movements, and walking difficulties may go away. However, Korsakoff syndrome (or Korsakoff psychosis) tends to develop as Wernicke symptoms go away.
Beriberi causes
Beriberi is caused by thiamine (vitamin B1) deficiency or the lack of thiamine pyrophosphate, the active form of thiamine (also spelled thiamin). Thiamine pyrophosphate, the biologically active form of thiamine, acts as a coenzyme in carbohydrate metabolism through the decarboxylation of alpha ketoacids. It also takes part in the formation of glucose by acting as a coenzyme for the transketolase in the pentose monophosphate pathway. Thiamine is important for the growth, development, and function of the cells in your body.
Beriberi is rare in the United States. This is because most foods are now vitamin enriched. If you eat a normal, healthy diet, you should get enough thiamine. Today, beriberi occurs mostly in people who abuse alcohol. Drinking heavily can lead to poor nutrition. Excess alcohol makes it harder for the body to absorb and store vitamin B1 (thiamine).
Worldwide, thiamine deficiency is primarily due to inadequate dietary intake, specifically in diets comprised mainly of polished rice and grains 4. In Western countries, thiamine deficiency most commonly presents in patients suffering from alcoholism or chronic illness. Special populations of individuals also at risk for thiamine deficiency include pregnant women, those requiring parental feeding, individuals who have undergone bariatric surgery, those with overall poor nutritional status, and patients on chronic diuretic therapy as it increases urinary losses 4. Thiamine deficiency in women can cause infantile beriberi 5.
In rare cases, beriberi can be genetic. This condition is passed down through families. People with this condition lose the ability to absorb thiamine from foods. This can happen slowly over time. The symptoms occur when the person is an adult. However, this diagnosis is often missed. This is because health care providers may not consider beriberi in nonalcoholics.
Deficiency of thiamine can be related to 6:
- Poor intake
- Diets primarily high in polished rice/processed grains
- Chronic alcoholism
- Parenteral nutrition without adequate thiamine supplementation
- Gastric bypass surgery
- Poor absorption
- Malnutrition
- Gastric bypass surgery
- Malabsorption syndrome
- Increased loss
- Diarrhea
- Hyperemesis gravidarum
- Diuretic use
- Renal replacement therapy
- Increased thiamine utilization
- Pregnancy
- Lactation
- Hyperthyroidism
- Refeeding syndrome
- Drugs such as diuretics (water pills) can lead to thiamine deficiency
Beriberi signs and symptoms
Beriberi is a disease in which the body does not have enough thiamine or vitamin B1.
There are two major types of beriberi:
- Wet beriberi: Thiamine deficiency with cardiovascular system involvement is termed wet beriberi. The chronic form of wet beriberi consists of 3 stages. In the first stage, peripheral vasodilation occurs, leading to a high cardiac output state. This leads to salt and water retention mediated through the renin-angiotensin-aldosterone system in the kidneys. As the vasodilation progresses, the kidneys detect a relative loss of volume and respond by conserving salt. With the salt retention, fluid is also absorbed into the circulatory system. The resulting fluid overload leads to edema of the dependent extremities.
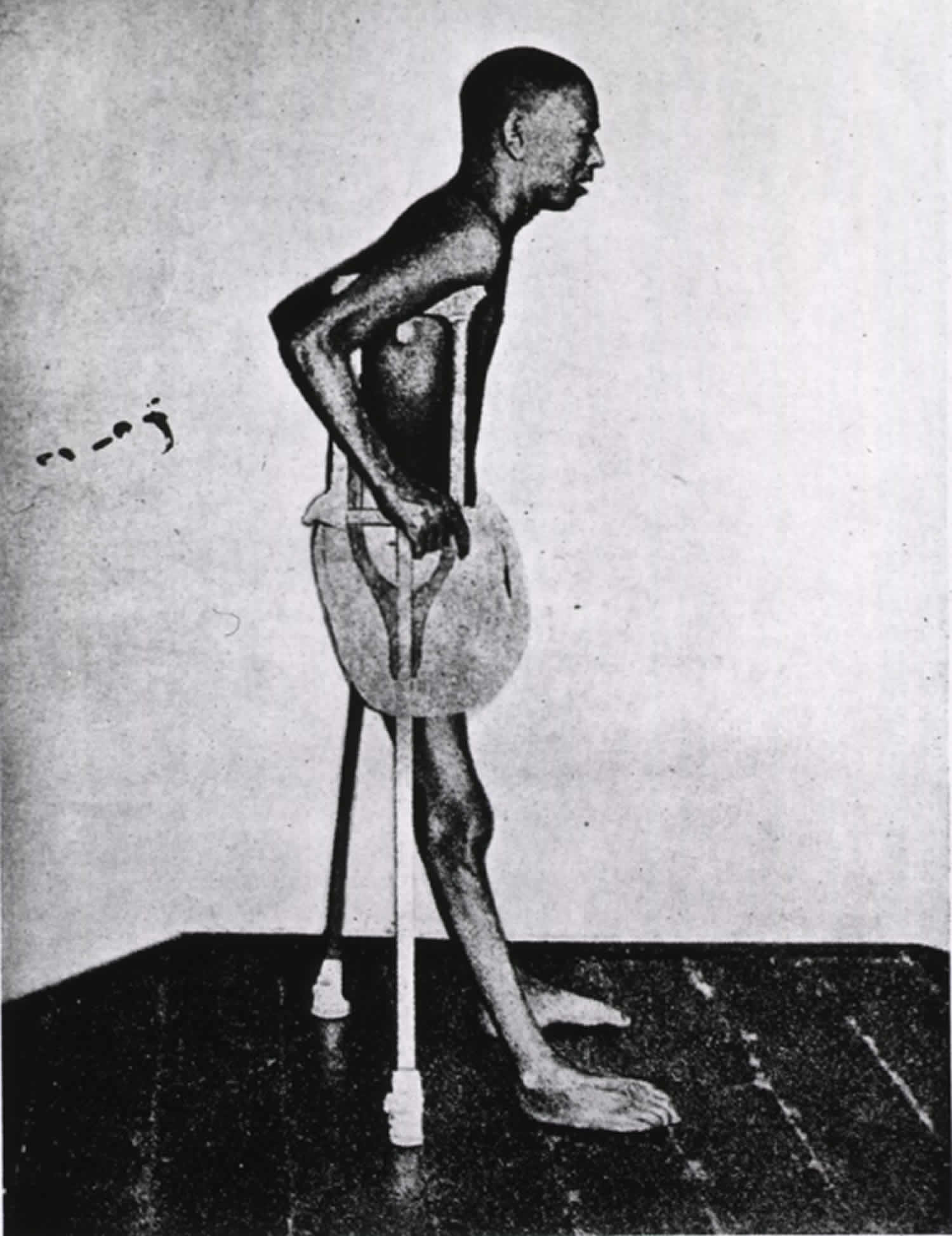
- Dry beriberi: Thiamine deficiency with nervous system involvement is termed dry beriberi. This presentation usually occurs when poor caloric intake and relative physical inactivity are present. The neurologic findings can be peripheral neuropathy characterized by symmetrical impairment of sensory, motor, and reflex functions of the extremities, especially in the distal lower limbs. Histologic analysis has shown that the lesions arise from a degeneration of the myelin in the muscular sheaths without inflammation 7.
- Cerebral beriberi also known as Wernicke-Korsakoff syndrome that affects the nervous system 8.
Symptoms of “dry beriberi” include:
- Difficulty walking
- Loss of feeling (sensation) in hands and feet
- Loss of muscle function or paralysis of the lower legs
- Mental confusion
- Pain
- Speech difficulties
- Strange eye movements (nystagmus)
- Tingling
- Vomiting
Symptoms of “wet beriberi” include:
- Awakening at night short of breath
- Increased heart rate
- Shortness of breath with activity
- Swelling of the lower legs
Wernicke-Korsakoff syndrome
Wernicke encephalopathy and Korsakoff syndrome are often thought to be on a spectrum with one another as they are both due to thiamine or vitamin B1 deficiency. Wernicke’s encephalopathy causes brain damage in lower parts of the brain called the thalamus and hypothalamus 9. Korsakoff’s psychosis results from permanent damage to areas of the brain involved with memory 9. Therefore, clinicians should screen for them together. Wernicke encephalopathy classically presents with the triad of altered mental status, ophthalmoplegia, and ataxia. In reality, less than 20% of patients will present with all three of these findings 10. Korsakoff syndrome or Korsakoff’s psychosis is a neuropsychiatric disorder associated with memory disturbances in which there are significant deficits in anterograde and retrograde memory. Immediate memory is maintained, but short-term memory is diminished with intact sensorium. The disorder is associated with patients fabricating stories in the setting of clear consciousness. Confabulations can be spontaneous or provoked with provoked confabulation commonly seen in chronic Korsakoff syndrome and spontaneous confabulation usually noted in the acute Wernicke’s encephalopathy 11, 12.
The following signs and symptoms should cause suspicion for Wernicke-Korsakoff syndrome 10:
- Altered mental status (up to 82% of patients) – amnesia, disorientation, confabulations
- Oculomotor findings – most often horizontal nystagmus, retinal hemorrhage, ophthalmoplegia, cranial nerve IV palsy, conjugate gaze
- Loss of muscular coordination (ataxia) – wide-based gait. Ataxia is likely to be a combination of polyneuropathy, cerebellar damage, and vestibular paresis. Vestibular dysfunction, usually without hearing loss, is universally impaired in the acute stages of Wernicke encephalopathy.
The cognitive impairments specific to Korsakoff syndrome vs. Wernicke encephalopathy include anterograde amnesia, profoundly limiting one’s learning capacity, retrograde amnesia, as well as executive deficits, resulting in decreased inhibition and difficulties with judgment, planning and problem-solving 13. Anterograde amnesia can result in the classic symptom of confabulations, replacing one’s gap in memory with untrue information 14.
Symptoms of Wernicke encephalopathy include:
- Confusion and loss of mental activity that can progress to coma and death
- Loss of muscle coordination (ataxia) that can cause leg tremor
- Vision changes such as abnormal eye movements (back and forth movements called nystagmus), double vision, eyelid drooping
- Alcohol withdrawal
Symptoms of Korsakoff syndrome include:
- Inability to form new memories
- Loss of memory, can be severe
- Making up stories (confabulation)
- Seeing or hearing things that are not really there (hallucinations)
Beriberi complications
Beriberi complications may include:
- Coma
- Congestive heart failure
- Death
- Psychosis
Beriberi diagnosis
A physical examination may show signs of congestive heart failure, including:
- Difficulty breathing, with neck veins that stick out
- Enlarged heart
- Fluid in the lungs
- Rapid heartbeat
- Swelling in both lower legs
A person with late-stage beriberi may be confused or have memory loss and delusions. The person may be less able to sense vibrations. The person may appear poorly nourished.
A physical examination of the nervous and muscular system may show signs of damage to many nerve systems:
- Changes in walking
- Coordination problems
- Abnormal eye movement
- Drooping of the eyelids
- Decreased or abnormal reflexes
- Fast pulse (heart rate)
- Low blood pressure
- Low body temperature
- Muscle weakness and atrophy (loss of tissue mass)
- Problems with walk (gait) and coordination.
For practical reasons, replacing thiamine as an initial test may be most feasible 15. If the patient responds to thiamine administration, it is safe to assume that a measure of thiamine deficiency was responsible for the signs and symptoms 15. Thiamine is not toxic in high levels, which means that this route carries little risk. In addition, time is saved in treating the patient and money is saved in testing. However, although observation of a patient’s clinical response to thiamine administration remains the easiest, least expensive form of testing, clinicians usually miss the subclinical forms of thiamine deficiency 15.
The diagnosis of Wernicke’s encephalopathy is a histopathological diagnosis, made after a postmortem examination of the brain 16, 17, 18.
The Caine criteria have been described to have a sensitivity or 85% and specificity of 100% for Wernicke encephalopathy, in the alcoholic population 19, 10. Because of the strong overlap, the Caine criteria can be used to help screen for Korsakoff syndrome as well.
Caine criteria for the diagnosis of Wernicke encephalopathy in chronic alcoholics 19. When 2 out of these 4 criteria apply, the clinical diagnosis of Wernicke encephalopathy is made 10, 19:
- Dietary deficiencies
- Undernutrition (body mass index <2 SD below normal)
- A history of grossly impaired dietary intake
- An abnormal thiamine status
- Oculomotor abnormalities
- Ophthalmoplegia
- Nystagmus
- Gaze palsy
- Cerebellar dysfunction
- Unsteadiness or ataxia
- Abnormalities of past pointing
- Dysdiadokokinesia
- Impaired heel-shin testing
- Either an altered mental state OR mild memory impairment
- Altered mental status
- Disorientation in two of three fields
- Confused
- An abnormal digit span
- Comatose
- Mild memory impairment
- Failure to remember two or more words in the four-item memory test
- Impairment on more elaborate neuropsychological tests of memory function
- Altered mental status
The following tests are used to check a person’s nutrition level:
- Serum albumin (relates to person’s general nutrition)
- Transketolase activity in red blood cells (reduced in people with thiamine deficiency). The serum level of thiamin is not a reliable indicator of thiamin status. However, thiamin function can be measured by red blood cells transketolase activity (erythrocytes transketolase activity or ETKA). Red blood cells transketolase activity (EKTA) of 0 to 15% is considered adequate, 15 to 25% is considered a moderate risk, and 25% or higher is considered high risk for thiamin deficiency 20, 21.
- Serum vitamin B1 or thiamine levels. Direct measurement of erythrocyte thiamin pyrophosphate (TPP) can be done using whole-blood testing and has more sensitivity, specificity, precision, and robustness 20. The concentration of TPP in the whole blood ranges from 70 to 180 nmol/L 22.
- Urine tests to see if thiamine is passing through the urine. Urinary thiamine excretion can be used to measure adequate dietary intake. However, it does not reflect the thiamine stores in the body. In adults, urinary thiamine excretion of <100 mcg/day suggests inadequate intake, and less than 40 mcg/day suggests thiamin deficiency 23.
- Liver enzymes may be high in people with a history of long-term alcohol abuse.
A brain MRI may show changes in the tissue of the brain. But if Wernicke-Korsakoff syndrome is suspected, treatment should start immediately. Usually a brain MRI exam is not needed.
Beriberi treatment
In suspected cases of thiamine deficiency, prompt administration of parenteral (intravenously or intramuscularly) thiamine is indicated.
To treat mild thiamine deficiency, the World Health Organization (WHO) recommends daily oral doses of 10 mg thiamine for a week, followed by 3–5 mg/daily for at least 6 weeks 24. For patients at risk of thiamine deficiency or with confirmed thiamine deficiency, parenteral (intravenously or intramuscularly) thiamine of 100 mg 3 times a day or 200 mg 3 times a day has been used, respectively, in clinical practice 25. The recommended treatment for severe thiamine deficiency consists of 25–30 mg intravenously in infants and 50–100 mg in adults, then 10 mg daily administered intramuscularly for approximately one week, followed by 3–5 mg/day oral thiamine for at least 6 weeks 26.
The preferred dose of thiamine treatment for Wernicke encephalopathy may be as high as 500 mg given one to three times daily parenterally 8. All malnourished patient may need higher doses of thiamine 8. Thiamine is generally administered before or together with glucose solutions because the glucose oxidation can decrease thiamine levels thereby exacerbating the neurological symptoms of Wernicke encephalopathy 8. Patients with magnesium deficiency should also be treated as this can result in reduced recovery from Wernicke encephalopathy especially in patients with alcoholism 27, 14, 28. Following a review of 19 papers, it has been recommended not to delay in correcting hypoglycemia 29. There are suggestions that prolonged and not acute replacement of glucose without thiamine supplementation increased the risk of Wernicke encephalopathy.
For Korsakoff syndrome high dose thiamine at 500 mg to 1500 mg, IV, three times daily for at least 3 days 10. Electrolyte abnormalities should be corrected and fluids replaced. In particular, magnesium requires replacement, as thiamine-dependent enzymes cannot operate in a magnesium-deficient state. Many patients will present needing glucose replacement as well, and traditionally it was thought that replacing glucose before thiamine could exacerbate the patient’s symptoms 30.
Thiamine, even at high concentrations, is not toxic in a person with normal kidney function 31. No cases of thiamine toxicity have been reported from the use of thiamine at the dosages indicated, even in patients in critical condition 31.
Once clinical symptoms improve, thiamine supplementation can switch to the oral route with a dose range of 50 to 100 mg per day 32. It is equally important in individuals with thiamine deficiency to require other nutrient supplementation such as magnesium, vitamin B2 (riboflavin), vitamin B3 (nicotinamide), vitamin B6 (pyridoxine), vitamin B12, vitamin C, potassium, and phosphate 26.
Support for cardiac function is necessary in cases of wet beriberi, because lack of cardiac support leads to low-output cardiac failure when the thiamine deficiency is corrected 31.
Follow-up care until delivery of current pregnancy, intensive care for advanced cardiomyopathy, definitive care for hyperthyroidism, or further workup of intestinal derangement may be warranted in patients with thiamine deficiency 31.
Blood tests may be repeated after the treatment is started. These tests will show how well you are responding to the medicine.
After the acute phase of vitamin and electrolyte replacement, there is mounting evidence that memory rehabilitation is beneficial in Korsakoff syndrome. Declarative memory (“knowing what”) seems to be most affected in Korsakoff syndrome, leading to many patients requiring lifelong care. Because procedural learning (“knowing how”) seems to remain somewhat maintained in Korsakoff syndrome, memory rehabilitation focussed in this area has shown promising outcomes. There has been some success in small Korsakoff syndrome patient populations in learning procedures and improving their autonomy 13.
Thiamine deficiency recovery time
Beriberi can be quickly fatal or can slowly rob an individual of almost all energy for even the simplest of daily activities. However, beriberi is one of the most easily treatable thiamine deficiency, with a remarkable recovery being possible even in severe cases 33. Therefore, the patient prognosis for beriberi is usually good, unless patients have established Korsakoff syndrome. While thiamine can induce partial improvement, the neuropsychological deficits persist in many cases. The confusional state usually improves when IV thiamine is administered but the learning and memory deficits only improve partially. A small number of patients fail to have any improvement and may develop Korsakoff psychosis or Korsakoff syndrome, which often requires institutionalization. Very few individuals recover at this point.
In cases of wet beriberi, clinical improvement can be observed within 12 hours of treatment, with normalization of heart function and size occurring in 1 or 2 days 33. The recovery is so dramatic that treatment with thiamine is a diagnostic test, which can be used in cases of acute heart failure and insidious peripheral neuropathy 33.
A retrospective study by Harel et al 34 indicated that thiamine deficiency in infancy can lead to long-term motor function problems. The study looked at children aged 5-6 years who, during the first 2 years of life, had been fed a faulty milk substitute that was deficient in thiamine, comparing them with age-matched controls. The Movement Assessment Battery for Children and the Zuk Assessment indicated that motor function difficulties existed in 56% and 59%, respectively, of the thiamine-deficient formula group, compared with 10% and 3%, respectively, of the control group. The results suggested that infantile thiamine deficiency affects gross and fine motor function, as well as balance skills 34.
Beriberi prognosis
The overall prognosis for patients with thiamine deficiency is good as it is easily treatable, and most signs and symptoms of the deficiency fully resolve with thiamine supplementation. Cardiac dysfunction seen in wet beriberi can be expected to improve within 24 hours of initiation of treatment 4. Symptoms of dry beriberi may improve or resolve 4. Unfortunately, once thiamine deficiency has progressed to Korsakoff syndrome, the patient may show minimal improvement during initial treatment, and the remaining symptoms may be permanent 35.
What is Thiamine?
Thiamine also known as vitamin B1 or thiamin, is one of the water-soluble B vitamins. Vitamin B1 or thiamine is naturally present in some foods, added to some food products, and available as a dietary supplement. Vitamin B1 or thiamine plays a critical role in energy metabolism and, therefore, in the growth, development, and function of cells 36. Foods rich in vitamin B1 or thiamine include whole grains, brown rice, lean pork, poultry, eggs, fish, soybean, nuts, dried beans, peas, and fortified or enriched grain products such as cereals, infant formulas, and bread 37, 38, 5. Multivitamins will provide an additional 1.5 mg of thiamine on top of a diet rich in thiamine 39.
Ingested vitamin B1 or thiamine from food and dietary supplements is absorbed by the small intestine through active transport at nutritional doses and by passive diffusion at pharmacologic doses 32, 36. Most dietary vitamin B1 or thiamine is in phosphorylated forms, and intestinal enzyme phosphatase hydrolyzes them to free thiamin before the vitamin is absorbed by the small intestine 36. The remaining dietary vitamin B1 or thiamine is in free (absorbable) form 36, 40. Thiamine, a water-soluble vitamin, cannot be stored in appreciable amounts 41. Humans store vitamin B1 or thiamine primarily in the liver, but in very small amounts (approximately 30 mg) 42. Vitamin B1 or thiamine has a short half‐life of 14 to 18 days and body stores are limited, so people require a continuous supply of thiamine from the diet 43, 32, 44.
Vitamin B1 or thiamine is present in the body as free thiamine, as well as in several phosphorylated forms: thiamine monophosphate (TMP), thiamine diphosphate (TDP also known as thiamin pyrophosphate (TPP)), and thiamine triphosphate (TTP) 45, 46, 47. About 80% of the approximately 25–30 mg of vitamin B1 or thiamine in the adult human body is in the form of thiamin pyrophosphate (TPP) also known as thiamin diphosphate (TDP), the main metabolically active form of vitamin B1 or thiamine. Bacteria in the large intestine also synthesize free thiamin and thiamin pyrophosphate (TPP), but their contribution, if any, to thiamin nutrition is currently unknown 48. Thiamin pyrophosphate (TPP) serves as an essential cofactor for five enzymes involved in glucose, amino acid (proteins), and fatty acids (lipids) metabolism (Figure 1) 49, 36, 42.
Levels of vitamin B1 or thiamine in the blood are not reliable indicators of thiamin status. Thiamine status is often measured indirectly by assaying the activity of the transketolase enzyme, which depends on thiamin pyrophosphate (TPP), in red blood cell hemolysates in the presence and absence of added thiamin pyrophosphate (TPP) 42. The result, known as the “TPP effect,” reflects the extent of unsaturation of transketolase with TPP. The result is typically 0%–15% in healthy people, 15%–25% in those with marginal deficiency, and higher than 25% in people with thiamine deficiency. Another commonly used measure of vitamin B1 or thiamine status is urinary thiamine excretion, which provides data on dietary intakes but not tissue stores 26. For adults, excretion of less than 100 mcg/day vitamin B1 or thiamine in urine suggests insufficient thiamine intake, and less than 40 mcg/day indicates an extremely low intake 23.
Figure 1. Vitamin B1 (thiamine) function
Footnote: Major biochemical reactions requiring vitamin B1 or thiamine as a cofactor (a compound that is essential for the activity of an enzyme).
[Source 50 ]How much Thiamine do I need?
The amount of vitamin B1 or thiamine you need depends on your age and sex 51. Average daily recommended amounts are listed in Table 1 below in milligrams (mg). The Recommended Dietary Allowance (RDA) is average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals 52. Table 1 lists the current Recommended Dietary Allowance (RDA) for vitamin B1 or thiamine 52. For infants from birth to 12 months, the Food and Nutrition Board at the Institute of Medicine of the National Academies established an adequate intake (intake at this level is assumed to ensure nutritional adequacy; adequate intake is established when evidence is insufficient to develop an RDA). for vitamin B1 or thiamine that is equivalent to the mean intake of vitamin B1 or thiamine in healthy, breastfed infants 26.
Most people in the United States consume the recommended amounts of vitamin B1 or thiamine 26. An analysis of data from the 2003-2006 National Health and Nutrition Examination Survey showed that only 6% of the U.S. population has a usual intake below the estimated average requirement (average daily level of intake estimated to meet the requirements of 50% of healthy individuals. It is usually used to assess the adequacy of nutrient intakes in populations but not individuals) 38.
Among children and teens, the average daily vitamin B1 or thiamine intake from foods is 1.27 mg for ages 2–5 years, 1.54 mg for ages 6–11 years, and 1.68 mg for ages 12–19 years 53. In adults aged 20 and older, the average daily vitamin B1 or thiamine intake from foods is 1.95 mg in men and 1.39 mg in women. The average daily vitamin B1 or thiamine intake from foods and supplements in children and teens is 1.51 mg for ages 2–5 years, 1.76 mg for ages 6–11 years, and 1.95 mg for ages 12–19 years. In adults aged 20 and older, the average daily vitamin B1 or thiamine intake from foods and supplements is 4.89 mg in men and 4.90 mg in women 26.
No current data on rates of thiamine deficiency in the U.S. population are available 26.
Most people in the United States get enough vitamin B1 or thiamine from the foods they eat. Thiamine deficiency is rare in this country. However, certain groups of people are more likely than others to have trouble getting enough vitamin B1 or thiamine:
- People with alcohol dependence
- Older individuals
- People with HIV/AIDS
- People with diabetes
- People who have had weight loss surgery
Table 1. Recommended Dietary Allowances (RDAs) for vitamin B1 or thiamine
| Life Stage | Recommended Amount |
|---|---|
| Birth to 6 months | 0.2 mg |
| Infants 7–12 months | 0.3 mg |
| Children 1–3 years | 0.5 mg |
| Children 4–8 years | 0.6 mg |
| Children 9–13 years | 0.9 mg |
| Teen boys 14–18 years | 1.2 mg |
| Teen girls 14–18 years | 1.0 mg |
| Men | 1.2 mg |
| Women | 1.1 mg |
| Pregnant teens and women | 1.4 mg |
| Breastfeeding teens and women | 1.4 mg |
What foods provide Thiamine or vitamin B1?
Vitamin B1 or thiamine is found naturally in many foods and is added to some fortified foods. You can get recommended amounts of vitamin B1 or thiamine by eating a variety of foods, including the following 40:
- Whole grains and fortified bread, cereal, pasta, and rice
- Meat (especially pork) and fish
- Legumes (such as black beans and soybeans), seeds, and nuts
Breads, cereals, and infant formulas in the United States and many other countries are fortified with thiamine 40. The most common sources of vitamin B1 or thiamine in the U.S. diet are cereals and bread 37. Pork is another major source of the vitamin. Dairy products and most fruits contain little vitamin B1 or thiamine 42. About half of the vitamin B1 or thiamine in the U.S. diet comes from foods that naturally contain thiamin; the remainder comes from foods to which thiamine has been added 38.
The U.S. Department of Agriculture’s (USDA’s) FoodData Central website (https://fdc.nal.usda.gov) lists the nutrient content of many foods and provides a comprehensive list of foods containing vitamin B1 or thiamine arranged by nutrient content (https://ods.od.nih.gov/pubs/usdandb/Thiamin-Content.pdf) and by food name (https://ods.od.nih.gov/pubs/usdandb/Thiamin-Food.pdf).
Heating foods containing vitamin B1 or thiamine can reduce their thiamin content. For example, bread has 20%–30% less vitamin B1 or thiamine than its raw ingredients, and milk pasteurization reduces thiamin content (which is very small to begin with) in milk by up to 20% 42. Because vitamin B1 or thiamine dissolves in water, a significant amount of the vitamin is lost when cooking water is thrown out 42. Processing also alters vitamin B1 or thiamine levels in foods; for example, unless white rice is enriched with thiamin, it has one tenth the amount of thiamin in unenriched brown rice 54.
Data on the bioavailability of vitamin B1 or thiamine from food are very limited 55. Some studies do show, however, that thiamin absorption increases when intakes are low 36.
Several food sources of thiamine are listed in Table 2.
Table 2. Vitamin B1 (thiamine) food sources
| Food | Milligrams (mg) per serving | Percent Daily Value (DV*) |
|---|---|---|
| Breakfast cereals, fortified with 100% of the Daily Value (DV) for thiamine, 1 serving | 1.2 | 100 |
| Egg noodles, enriched, cooked, 1 cup | 0.5 | 42 |
| Pork chop, bone-in, broiled, 3 ounces | 0.4 | 33 |
| Trout, cooked, dry heat, 3 ounces | 0.4 | 33 |
| Black beans, boiled, ½ cup | 0.4 | 33 |
| English muffin, plain, enriched, 1 muffin | 0.3 | 25 |
| Mussels, blue, cooked, moist heat, 3 ounces | 0.3 | 25 |
| Tuna, Bluefin, cooked, dry heat, 3 ounces | 0.2 | 17 |
| Macaroni, whole wheat, cooked, 1 cup | 0.2 | 17 |
| Acorn squash, cubed, baked, ½ cup | 0.2 | 17 |
| Rice, brown, long grain, not enriched, cooked, ½ cup | 0.2 | 17 |
| Rice, white, long grain, enriched, cooked, ½ cup | 0.1 | 8 |
| Bread, whole wheat, 1 slice | 0.1 | 8 |
| Orange juice, prepared from concentrate, 1 cup | 0.1 | 8 |
| Sunflower seeds, toasted, 1 ounce | 0.1 | 8 |
| Beef steak, bottom round, trimmed of fat, braised, 3 ounces | 0.1 | 8 |
| Yogurt, plain, low fat, 1 cup | 0.1 | 8 |
| Oatmeal, regular and quick, unenriched, cooked with water, ½ cup | 0.1 | 8 |
| Corn, yellow, boiled, 1 medium ear | 0.1 | 8 |
| Milk, 2%, 1 cup | 0.1 | 8 |
| Barley, pearled, cooked, 1 cup | 0.1 | 8 |
| Cheddar cheese, 1½ ounces | 0 | 0 |
| Chicken, meat and skin, roasted, 3 ounces | 0 | 0 |
| Apple, sliced, 1 cup | 0 | 0 |
Footnote: *DV = Daily Value. Daily Values were developed by the U.S. Food and Drug Administration (FDA) to help consumers compare the nutrient contents of products within the context of a total diet. The DV for thiamine is 1.5 mg for adults and children age 4 and older. Foods providing 20% or more of the Daily Value are considered to be high sources of a nutrient.
[Source 56 ]Thiamine Deficiency
Thiamine deficiency, also called vitamin B1 deficiency, is a rare disorder that occurs if the recommended daily intake of vitamin B1 or thiamine is not maintained 57, 58. Populations and cultures that rely heavily upon rice based diets are at increased risk of thiamine deficiency 59. Thiamine deficiency may also occur due to impaired intestinal absorption or high excretion rates, such as in people with alcohol dependency, acquired immunodeficiency syndrome (AIDS), and malnutrition 60, 61. Individuals with certain medical and non-medical conditions are more susceptible to vitamin B1 deficiency, e.g., alcohol dependency, older age, diabetes, post-weight loss surgery, cancers that have spread throughout the body, cancer chemotherapy with poor dietary intake, gastrointestinal disease, pregnancy with hyperemesis gravidarum (severe nausea and vomiting during pregnancy), lactation, fasting, starvation, use of unbalanced diets, malnourished patients with intestinal obstruction or malabsorption syndromes, hyperthyroidism (overactive thyroid), kidney failure on hemodialysis, and systemic infections 62, 22, 59.
Thiamine is important for the growth, development, and function of the cells in your body. In the human body, thiamine or vitamin B1 exists mainly in the form of thiamin pyrophosphate (TPP). This is the main active form of thiamine and serves as a cofactor for many enzymes during the metabolism of glucose, branched-chain amino acids (protein), and fatty acids (lipids) (see Figure 1 below) 49. Thiamine or vitamin B1 deficiency can lead to severe (or even fatal) cardiovascular, muscular, gastrointestinal, and central and peripheral nervous systems complications, including heart failure, neuropathy leading to ataxia and paralysis, confusion, or delirium 63, 64.
Most people have no symptoms and signs of thiamine deficiency or vitamin B1 deficiency; therefore, it must be suspected in the appropriate clinical setting 65. Thiamine deficiency or vitamin B1 deficiency early symptoms and signs are often nonspecific and vague, such as fatigue. However, early symptoms mainly arise from neurological, heart and gastrointestinal systems, where patients may experience weight loss, anorexia, confusion, short-term amnesia, malaise, muscle weakness, and heart symptoms due to heart failure 66.
Generally, heart effects are referred to as “wet beriberi”, the peripheral neurological signs and symptoms are called “dry beriberi”, and delirium, mental confusion and abnormal eye movements (due to ophthalmoplegia, which is paralysis or weakness of the eye muscles), stance and gait ataxia are termed “cerebral beriberi” or Wernicke’s encephalopathy 67, 68, 50. “Gastrointestinal beriberi” is caused by lactic acidosis, a condition resulting from the accumulation of lactate and is often associated with nausea, vomiting, and severe abdominal pain 69.
Beriberi is the classic diet related thiamine deficiency which can present as wet or dry types. “Wet beriberi” presents as a right sided high-output heart failure with signs of peripheral swelling (edema), an enlarged heart, warm extremities, rapid heart rate (tachycardia), and respiratory distress 66. “Dry beriberi” is predominantly a neurological complication involving the peripheral nervous system and presents with painful peripheral neuropathy, malaise, muscle weakness, seizures, or brisk tendon reflexes 22. Infants and children are susceptible to vitamin B1 deficiency too, presenting as infantile or childhood beriberi. Usually, infants present with swelling (edema), ill-looking appearance, pallor, anorexia, coffee ground vomiting, and diarrhea 66. Neurological signs include a hoarse cry due to vocal cord paralysis, head lag, seizures, coma, and sudden infant death syndrome. “Juvenile beriberi” is uncommon and often misdiagnosed due to overlapping symptoms of meningitis 49.
If thiamine deficiency or vitamin B1 deficiency is prolonged or left untreated, an individual is at risk of advanced-stage symptoms due to irreversible neurological damage called Wernicke-Korsakoff syndrome 10, 70. Wernicke-Korsakoff syndrome is more common in the United States and 8 to 10 times more common among people with chronic alcohol consumption/misuse, severe gastrointestinal disorders, cancers, drug use, and AIDS 66. Wernicke-Korsakoff syndrome presents in two phases. Wernicke’s encephalopathy occurs early and presents with polyneuropathy, ataxia, abnormal eye movements due to ophthalmoplegia (paralysis or weakness of the eye muscles), and gait abnormalities. Korsakoff’s syndrome also called Korsakoff psychosis, Korsakoff’s dementia, Korsakoff’s amnesia, or amnestic confabulatory syndrome, is a residual syndrome in patients who suffered from a Wernicke encephalopathy, but did not receive immediate and adequate treatment with thiamine or vitamin B1 replacement therapy 70, 71, 72, 73. The most conspicuous symptom of Korsakoff’s syndrome is global short-term amnesia, which can be very profound. In combination with other cognitive and behavioral deficits such as disorientation, confabulation, and hallucinations, which may have far-reaching effects on daily life 74, 75, 76. Wernicke encephalopathy is acute and often reversible while Korsakoff syndrome is chronic and may be irreversible 77. The most common cause of Korsakoff syndrome is chronic alcohol abuse 30. Alcohol interferes with gastrointestinal tract absorption of thiamine as well as interfering with the liver’s ability to store thiamine. Additionally, accompanying malnutrition often compounds the effects of alcoholism leading to further thiamine deficiency. Other causes of Korsakoff syndrome include eating disorders, chronic vomiting (including hyperemesis gravidarum), psychiatric disorders, chemotherapy, and cancer 78, 79. As Korsakoff syndrome is advanced-stage symptoms of thiamine deficiency, parenteral thiamine treatment does not lead to recovery in about one-quarter of patients 76.
Thiamine deficiency causes
Thiamine deficiency or vitamin B1 deficiency may result from inadequate dietary thiamine intake, administration of total parenteral nutrition without adequate thiamine replacement, increased physiological requirements for thiamine, excessive loss of thiamine from the body, impaired intestinal absorption, small intestinal bacterial overgrowth (SIBO), consumption of anti-thiamine factors (ATF) in food, antacids, sulfites, or sodium bicarbonate food preservatives or a combination of these factors 80, 81, 82, 50.
The maximum body store of thiamine is 30 mg, which is rapidly depleted within 2 weeks of beginning a thiamine-deficient diet 41. Risk factors for decreased thiamine intake include protracted vomiting, weight loss surgery or gastrointestinal surgery, malnutrition, extreme nausea and vomiting during pregnancy (hyperemesis gravidarum), anorexia, and alcoholism 83.
Other conditions that may cause thiamine deficiency or vitamin B1 deficiency include:
- HIV/AIDS
- Cancers that have spread throughout the body
- Extreme nausea and vomiting during pregnancy (hyperemesis gravidarum)
- Heart failure (when treated with long-term diuretic therapy)
- Long periods of intravenous (IV) nutrition without receiving thiamine supplements
- Long-term dialysis
- Taking high doses of diuretics (water pills)
- Very high thyroid hormone levels (thyrotoxicosis)
- Breastfed infants whose mother is lacking in thiamine
- Infants fed unusual formulas that don’t have enough thiamine.
In rare cases, thiamine deficiency or vitamin B1 deficiency can be a genetic metabolic disease 84, 85. This condition is passed down through families. People with this condition lose the ability to absorb thiamine from foods. This can happen slowly over time. The symptoms occur when the person is an adult. However, this diagnosis is often missed. This is because health care providers may not consider thiamine deficiency in nonalcoholics 85.
Inadequate dietary thiamine or vitamin B1 intake
Inadequate consumption of thiamine or vitamin B1 is the main cause of thiamine deficiency in developing countries 86. Thiamine deficiency is common in low-income populations whose diets are high in carbohydrate and low in thiamine. Examples of foods that can lead to inadequate thiamine intake upon prolonged consumption include sago, cassava flour, unfortified white bread, or highly refined cereals such as polished white rice 41. The consumption of a diet composed mainly of refined carbohydrates or one that includes high alcohol intake also reduces body thiamine stores 41.
To attain maximal erythrocyte transketolase activity, at least 0.6 mg of thiamine per 1000 kcal of carbohydrate is required 41. Most humans will develop symptoms of thiamine deficiency when intake is below 0.2 mg of thiamine per 1000 kcal. Whole wheat flour contains 0.55 mg of thiamine per 100 g, brown rice 0.33 mg per 100 g, and highly milled white rice only 0.08 mg per 100 g 41. Adding baking powder (sodium bicarbonate) to wholemeal flour when baking bread reduces the thiamine content 41. Washing white rice in water prior to cooking reduces the thiamine content by half. Thiamine is heat labile, chlorine sensitive, and water soluble, so discarding the rice water after cooking or using chlorinated water for cooking or washing rice contributes to thiamine loss from the diet 80. Parboiling (partly cook food by boiling) of rice was originally developed in India but is not practiced in Southeast Asia or Japan, where milled white rice is preferred. Rice parboiling distributes the thiamine content from the bran and aluerone layer to the endosperm prior to milling. This is why beriberi is rare in India, where parboiled rice is the primary form of rice consumed 80.
After 1878, mechanical roller milling of wheat and polishing of rice became widespread 87. Consumption of mass-produced, polished white rice as the staple diet in East Asian countries led to epidemics of thiamine deficiency (beriberi) in the 1800s and 1900s 88, 87. Polished rice and milled wheat were also popular because removal of the oil-rich bran layer from rice or the wheat bran from wheat grains prolonged storage times, minimized rancidity, and reduced the susceptibility to weevils. Mandatory fortification of wheat flour with the thiamine mononitrate vitamer was introduced in Australia in 1991. Since then, Wernicke-Korsakoff syndrome has become very uncommon in Australia. The thiamine mononitrate vitamer is used because it is non-hygroscopic and more stable than thiamine hydrochloride 89. Mandatory fortification of bread with iodine and folate was commenced in Australia in 2009. Folate deficiency may indirectly contribute to thiamine deficiency, as folate is required for the regeneration of reduced nicotinamide adenine dinucleotide (NADH) by dihydrofolate reductase. NADH is necessary for the regeneration of TPP 90. Vitamin C may protect against the development of symptoms of thiamine deficiency 80.
Breast-fed infants whose mothers are thiamine deficient are vulnerable to developing infantile beriberi. Alcoholism, which is associated with low intake of thiamine among other nutrients, is the primary cause of thiamine deficiency in industrialized countries. Some of the non-alcoholic conditions associated with Wernicke-Korsakoff syndrome include anorexia nervosa, bariatric surgery (weight-loss surgery), gastrointestinal malignancies, and malabsorption syndromes 91, 92, 93, 94. Obese individuals may also be at heightened risk of thiamine deficiency 95, 96. Moreover, cases of Wernicke’s encephalopathy have been linked with hyperemesis gravidarum (severe nausea and vomiting during pregnancy) 97, 98, and with parenteral nutrition lacking vitamin supplementation 99, 100.
Increased thiamine or vitamin B1 requirement
Conditions resulting in an increased requirement for thiamine or vitamin B1 include strenuous physical exertion, fever, severe infection or sepsis, hyperthyroidism, pregnancy, breast-feeding, adolescent growth, major surgery, refeeding syndrome, or rapid growth of cancers 32, 101, 102, 103, 104, 105, 106, 107, 108. Such conditions place individuals with marginal thiamine intake at risk for developing symptomatic thiamine deficiency.
Fever can critically increase the requirement for thiamine, as a rise in core body temperature of 1°C will increase the basal metabolic rate by 10% 109. Consumption of a high-fat or a high-carbohydrate diet results in increased metabolic consumption of thiamine 90. This is particularly relevant in individuals with preexisting thiamine deficiency, such as refugees, prisoners of war, persons with alcoholism, oncology patients, and postoperative bariatric surgery or gastrectomy patients. Administering oral, enteral, or parenteral nutrition to these patients without concomitant thiamine supplementation can result in fulminant beriberi or acute refeeding syndrome 80, 110, 111, 112, 113.
Malaria patients in Southeast Asia were found to be thiamine deficient more frequently than non-infected individuals 114, 115. Malarial infection leads to a large increase in the metabolic demand for glucose. Because thiamine is required for enzymes involved in glucose metabolism, the stresses induced by malarial infection could exacerbate thiamin deficiency in predisposed individuals. HIV-infected individuals, whether or not they had developed AIDS, were also found to be at increased risk for thiamine deficiency 116. Furthermore, chronic alcohol abuse impairs intestinal absorption and utilization of thiamine 68; therefore, alcoholics have increased requirements for thiamine or vitamin B1. Thiamine deficiency is also observed as a complication of the refeeding syndrome: the introduction of carbohydrates in severely starved individuals leads to an increased demand for thiamine in glycolysis and the citric acid cycle that precipitates thiamine deficiency 117.
Anti-thiamin factors
The presence of anti-thiamin factors (ATF) in foods contributes to the risk of thiamin deficiency. Certain plants contain anti-thiamin factors (ATF), which react with thiamine to form an oxidized, inactive product. Consuming very large amounts of tea or coffee (including decaffeinated), as well as chewing tea leaves and betel nuts, might lower thiamin status due to the presence of anti-thiamin factors (ATF) 118, 119. Anti-thiamin factors (ATF) include mycotoxins (molds), thiaminases that break down thiamin in food, thiamine antagonists, and hemin 41. Individuals who habitually eat certain raw fresh-water fish, raw shellfish, or ferns are at higher risk of thiamine deficiency because these foods contain thiaminase that normally is inactivated by heat in cooking 68, 120, 121, 122, 123. In Nigeria, an acute, neurologic syndrome (seasonal ataxia) has been associated with thiamine deficiency precipitated by a thiaminase in African silkworms (Anaphe species), a traditional, high-protein food for some Nigerians 124.
Thiamine antagonists are found in tea and betel nuts (tannic acid), coffee (chlorogenic acid, caffeic acid), bracken fern (caffeic acid), and pigmented polyphenol-containing foods such as red cabbage, blueberries, red currants, and red beets 41. These cause oxidation of the thiazole ring of thiamine, forming nonabsorbable thiamine disulfide 80. For example, consumption of 1 g of dry tea leaves boiled in 100 mL of water for 5 minutes caused thiamine loss of 0.21 mg per hour 125. Vitamin C and cysteine can protect thiamine from degradation caused by organic acids and polyphenols 126. Outbreaks of beriberi in the wet season in some countries may be related to low availability of food, importation of poor-quality rice or milled white rice, seasonal variations in plant tannin levels, or the mycotoxin citreoviridin, produced by rice mold 127, 102, 128.
Food additives and thiamine
Thiamine is unstable under alkaline conditions produced by food additives such as preservatives and antacids (eg, sodium bicarbonate), which cause disruption of the thiamine methylene bridge 41. Sulfite-type food preservatives include sulfur dioxide, sodium sulfite, sodium and potassium bisulfite, and sodium and potassium metabisulfite 41. These are used extensively in the production and preservation of foods and beverages, including dried fruit, ready-to-eat salad vegetables, frozen fried potatoes, wine, beer, soft drinks, packaged fruit juices, shellfish, and pickled and pureed foods. Sulfites possess antioxidant and antimicrobial activities, which inhibit the enzymatic and nonenzymatic (browning) spoiling of food. This preserves the color, freshness, flavor, and crispness of food but substantially reduces the available thiamine. For example, respective thiamine loss from cabbage blanched with sulfite-treated water versus untreated water was 45% vs 15% 80. The use of sulfiting agents in foods recognized as important sources of thiamine is prohibited by the US Food and Drug Administration 129, 130, 131, 132.
Excessive loss of thiamine caused by thiamine-drug interactions
Excessive loss of thiamine may precipitate thiamine deficiency. Increased losses of ingested thiamine can be caused by drug-related polyuria or diarrhea, drug interactions, or chronic excessive alcohol consumption 41. Thiamine is a polar, water-soluble vitamin and is not protein bound, which allows it to be easily dialyzed or filtered in the glomerulus. Increased urine flow, loop diuretics, or dialysis can all cause thiamine deficiency. Thiamine deficiency is associated with drugs such as omeprazole, phenytoin, 5-fluorouracil, metformin, alcohol, antibiotics, furosemide, and thiazide diuretics 83. By increasing urinary flow, diuretics may prevent reabsorption of thiamine by the kidneys and increase its excretion in the urine 133, 134. The risk of thiamine deficiency is increased in diuretic-treated patients with marginal thiamine intake 135 and in individuals receiving long-term, diuretic therapy 136. Patients with congestive heart failure who receive chronic therapy with furosemide or thiazide diuretics can also develop thiamine deficiency. The prevalence of thiamine deficiency in this patient population varies from 21% to 98% 41. Supplementation with thiamine has been shown to improve left ventricular ejection fraction by 22%, New York Heart Association Functional Classification, and TPP effect (from 11.7% to 5.4%) in these patients 137. Mechanisms for exacerbation of heart failure by diuretics include increased thiamine loss in urine, furosemide-related inhibition of cardiac myocyte thiamine uptake, furosemide-induced anorexia, furosemide inhibition of intestinal absorption or cellular uptake of thiamine, and hypomagnesemia 83. Unrecognized thiamine deficiency in heart failure patients treated with long-term diuretic therapy may result in Shoshin beriberi 138.
Individuals with kidney failure requiring hemodialysis lose thiamine at an increased rate and are at risk for thiamine deficiency 139. Alcoholics who maintain a high fluid intake and high urine flow rate may also experience increased loss of thiamine, exacerbating the effects of low thiamine intake 140.
Omeprazole a proton pump inhibitor because of its azole analogue molecular structure may cause inactivation of pyruvate decarboxylase and human erythrocyte transketolase, resulting in antagonism of thiamine 141. Omeprazole may inhibit gastric proton pumps by competing with thiamine for binding to hydrogen/potassium adenosine triphosphatase 84, 141. Proton pump inhibitor drugs or Roux-en-Y gastric bypass surgery may also worsen subclinical thiamine deficiency by promoting small intestinal bacterial overgrowth, which alters luminal thiamine levels 142, 82. Hypomagnesemia induced by proton pump inhibitors can contribute to functional thiamine deficiency, as magnesium is a required cofactor for the formation of TPP and acetyl coenzyme A 142. 5-Fluorouracil decreases hepatic thiamine levels and thiamine-dependent transketolase activity. This is associated with an increase in the TPP effect in vitro and in whole blood 143. 5-Fluorouracil is catabolized to fluoroacetate, which blocks the Krebs cycle and ATP production, leading to neurotoxicity, ammonia formation, and encephalopathy 144, 145, 146. Metformin, a substrate and inhibitor of the human thiamine transporter 2, reduces both intestinal absorption of thiamine and levels of thiamine in tissues and liver 147, 148, 149. Alcohol decreases carrier-mediated thiamine transport in the brush border and basolateral membrane of enterocytes in the jejunum (thiamine transporter 1) and potentially decreases thiamine production by intestinal flora in the lumen 150
Small intestinal bacterial overgrowth can be treated specifically with certain oral antibiotics such as rifaximin, neomycin, and metronidazole, which can improve postoperative thiamine deficiency in Roux-en-y gastric bypass patients 151, 81, 82. The use of broad-spectrum antibiotics (penicillins, cephalosporins, aminoglycosides, tetracyclines, fluoroquinolones, sulfonamides, trimethoprim), however, can potentially cause thiamine deficit in some patients by reducing counts of normal intestinal bacteria that produce thiamine (eg, Escherichia coli, bifidobacteria, Lactobacillus spp) and by promoting the growth of pathogenic flora such as Clostridium spp, which produce thiaminases 152, 83. Metronidazole, a thiazole, has been shown to be a substrate for thiaminase 1. Formation of thiamine antimetabolites from metronidazole, which can occur particularly with high cumulative doses or prolonged use of metronidazole, can inhibit thiamine pyrophosphokinase, leading to irreversible, painful, peripheral neuropathy 126.
Table 3. Effects of drugs and antithiamine agents on thiamine
| Drug family/antithiamine agent | Drug | Effect on thiamine |
|---|---|---|
| Alcohol | Ethanol | Decreased intestinal thiamine transport |
| Antibiotic | Metronidazole | Production of thiamine antimetabolites |
| Antibiotics | β-lactams, aminoglycosides, trimethoprim, quinolones | Decreased production of thiamine by intestinal microbiota |
| Chemotherapy | 5-fluorouracil | Decreased production of hepatic thiamine, decreased TKT activity |
| Polyphenols (coffee, tea) | Caffeic acid, tannic acid | Oxidation of thiazole ring |
| Diuretics | Furosemide, thiazides | Increased renal excretion, decreased intestinal absorption |
| Flavonoids | Quercetin, rutin | Oxidation to thiamine disulfide |
| Food preservatives | Sulfites | Disruption of thiamine methylene bridge |
| Oral hypoglycemics (biguanide) | Metformin | THTR2 inhibitor, prevents active transport of thiamine |
| Proton pump inhibitors | Omeprazole | Inactivation of PDH, erythrocyte transketolase, and H/K ATPase |
Abbreviations: H/K ATPase = hydrogen/potassium adenosine triphosphatase; PDH = pyruvate dehydrogenase; TKT = transketolase; THTR2 = thiamine transporter 2.
[Source 41 ]Groups at risk of thiamine deficiency
The following groups are among those most likely to have inadequate thiamine status 26.
People with alcohol dependence
In highly industrialized countries, chronic alcohol use disorders appear to be the most common cause of thiamine deficiency 36. Up to 80% of people with chronic alcoholism develop thiamine deficiency because ethanol reduces gastrointestinal absorption of thiamine, thiamine stores in the liver, and thiamine phosphorylation 42, 72. Also, people with alcoholism tend to have inadequate intakes of essential nutrients, including thiamine.
Older adults
Up to 20%–30% of older adults have laboratory indicators that suggest some degree of thiamine deficiency 40, 55. Possible reasons include low dietary intakes, a combination of chronic diseases, concomitant use of multiple medications, and low absorption of thiamin as a natural result of aging 153, 154. Some small studies have found that the risk of deficiency is particularly high in elderly people who reside in an institution 155, 156.
People with HIV/AIDS
People with HIV infection have an increased risk of thiamin deficiency and its sequelae, including beriberi and Wernicke-Korsakoff syndrome 36, 157. Autopsies of 380 people with AIDS found that almost 10% had Wernicke’s encephalopathy 158, and some experts believe that thiamin deficiency is underdiagnosed in this population 159. The association between thiamin deficiency and HIV/AIDS is probably due to malnutrition as a result of the catabolic state associated with AIDS 26.
People with diabetes
Some small studies have found that thiamine levels in plasma are up to 76% lower in people with type 1 diabetes than in healthy volunteers and 50%–75% lower in people with type 2 diabetes 160, 161. Other studies have shown a higher risk of thiamine deficiency in people with type 1 and/or type 2 diabetes based on tests of erythrocyte transketolase activity 162, 163. These lower thiamine levels might be due to increases in clearance of thiamin by the kidneys. The relevance of these effects to clinical prognosis or outcomes is not known.
People who have undergone weight loss surgery
Weight loss surgery also called bariatric surgery for weight loss is associated with some risks, including severe thiamine deficiency due to malabsorption that can lead to beriberi or Wernicke’s encephalopathy 26. A 2008 literature review identified 84 cases of Wernicke’s encephalopathy after bariatric surgery (primarily gastric bypass surgery) between 1991 and 2008 164. About half of these patients experienced long-lasting neurologic impairments. Micronutrient supplements that include thiamine are almost always recommended for patients following weight loss surgery to avoid deficiencies 165.
Thiamine deficiency prevention
Eating a proper diet that is rich in vitamins will prevent thiamine deficiency. Nursing mothers should make sure that their diet contains all vitamins. If your infant is not breastfed, make sure that the infant formula contains thiamine.
If you drink alcohol, try to cut down or quit. Also, take B vitamins to make sure your body is properly absorbing and storing thiamine.
Thiamine deficiency symptoms
Most people have no symptoms and signs of thiamine deficiency or vitamin B1 deficiency; therefore, it must be suspected in the appropriate clinical setting 65. Thiamine deficiency or vitamin B1 deficiency early symptoms and signs are often nonspecific and vague, such as fatigue. However, early symptoms mainly arise from neurological, heart and gastrointestinal systems, where patients may experience weight loss, anorexia, confusion, short-term amnesia, malaise, muscle weakness, and heart symptoms due to heart failure 66.
Generally, heart effects of thiamine deficiency are referred to as “wet beriberi”, the peripheral neurological signs and symptoms of thiamine deficiency are called “dry beriberi”, and delirium, mental confusion and abnormal eye movements (due to ophthalmoplegia, which is paralysis or weakness of the eye muscles), stance and gait ataxia are termed “cerebral beriberi” or Wernicke’s encephalopathy 67, 68, 50. “Gastrointestinal beriberi” is caused by lactic acidosis, a condition resulting from the accumulation of lactate and is often associated with nausea, vomiting, and severe abdominal pain 69.
Thiamine deficiency cardiovascular signs and symptoms are as follows:
- Fast heart rate (tachycardia)
- Chest pain
- Wide pulse pressure
- Heart failure (orthopnea with or without edema, warm skin due to vasodilation) 166
- Hypotension, shock
Thiamine deficiency gastroenterologic signs and symptoms are as follows:
- Anorexia
- Abdominal discomfort
- Constipation
- Difficulty swallowing (dysphagia) 167
Thiamine deficiency neurologic signs and symptoms of thiamine deficiency are as follows 168:
- Poor memory, irritability, sleep disturbance
- Wernicke encephalopathy and/or Korsakoff syndrome 169
- Bilateral, symmetrical lower extremity paresthesias, burning pain
- Muscle cramps
- Decreased vibratory position sensation
- Absent knee and ankle jerk
- Muscle atrophy
- Foot drop (late stage)
- Abnormal eye movement (back and forth movements called nystagmus) – most common (early sign) 170
Thiamine deficiency infantile beriberi signs and symptoms are as follows 171:
- Congestive heart failure
- Loss of voice (aphonia)
- Absent deep tendon reflex.
A study by Mifsud et al 170 described the characteristics of 56 cases of thiamine deficiency that were seen at a French tertiary hospital. A history of alcohol abuse was found in 45 patients (80%), and while neurologic symptoms were the basis for diagnosis in the majority of individuals, there were frequent instances of nonspecific and digestive symptoms. Moreover, the criteria for malnutrition were fulfilled in 34% of patients. Of the 54% of patients in whom brain magnetic resonance imaging (MRI) scans were performed, abnormal scans were found in 63% of cases 170.
A study by Isenberg-Grzeda et al 172 indicated that thiamine deficiency may be a frequent occurrence among inpatients with cancer, even in those who are of normal weight or overweight, lack other vitamin deficiencies, and are receiving multivitamin supplements. The single-center study found thiamine deficiency in 55.3% of 217 patients, with risk factors for the deficiency including active cancer treatment and fluorouracil-based chemotherapy 172.
A literature review by Jain et al 173 comparing the incidence of thiamine deficiency in patients with heart failure to that in controls reported an odds ratio of 2.53, with possible reasons for the deficiency in heart failure including diuretic use, dietary changes, and alterations in the absorption and metabolism of thiamine. The literature also indicated that thiamine supplementation may improve symptoms and ejection fraction in patients with heart failure 173.
Wernicke-Korsakoff syndrome signs and symptoms
Wernicke encephalopathy and Korsakoff syndrome are often thought to be on a spectrum with one another as they are both due to thiamine or vitamin B1 deficiency. Wernicke’s encephalopathy causes brain damage in lower parts of the brain called the thalamus and hypothalamus 9. Korsakoff’s psychosis results from permanent damage to areas of the brain involved with memory 9. Therefore, clinicians should screen for them together. Wernicke encephalopathy classically presents with the triad of altered mental status, ophthalmoplegia, and ataxia. In reality, less than 20% of patients will present with all three of these findings 10. Korsakoff syndrome or Korsakoff’s psychosis is a neuropsychiatric disorder associated with memory disturbances in which there are significant deficits in anterograde and retrograde memory. Immediate memory is maintained, but short-term memory is diminished with intact sensorium. The disorder is associated with patients fabricating stories in the setting of clear consciousness. Confabulations can be spontaneous or provoked with provoked confabulation commonly seen in chronic Korsakoff syndrome and spontaneous confabulation usually noted in the acute Wernicke’s encephalopathy 11, 12.
The following signs and symptoms should cause suspicion for Wernicke-Korsakoff syndrome 10:
- Altered mental status (up to 82% of patients) – amnesia, disorientation, confabulations
- Oculomotor findings – most often horizontal nystagmus, retinal hemorrhage, ophthalmoplegia, cranial nerve IV palsy, conjugate gaze
- Loss of muscular coordination (ataxia) – wide-based gait. Ataxia is likely to be a combination of polyneuropathy, cerebellar damage, and vestibular paresis. Vestibular dysfunction, usually without hearing loss, is universally impaired in the acute stages of Wernicke encephalopathy.
The cognitive impairments specific to Korsakoff syndrome vs. Wernicke encephalopathy include anterograde amnesia, profoundly limiting one’s learning capacity, retrograde amnesia, as well as executive deficits, resulting in decreased inhibition and difficulties with judgment, planning and problem-solving 13. Anterograde amnesia can result in the classic symptom of confabulations, replacing one’s gap in memory with untrue information 14.
Symptoms of Wernicke encephalopathy include:
- Confusion and loss of mental activity that can progress to coma and death
- Loss of muscle coordination (ataxia) that can cause leg tremor
- Vision changes such as abnormal eye movements (back and forth movements called nystagmus), double vision, eyelid drooping
- Alcohol withdrawal
Symptoms of Korsakoff syndrome include:
- Inability to form new memories
- Loss of memory, can be severe
- Making up stories (confabulation)
- Seeing or hearing things that are not really there (hallucinations)
Thiamine deficiency complications
Thiamine deficiency complications may include:
- Coma
- Congestive heart failure
- Death
- Psychosis
Thiamine deficiency diagnosis
A physical examination may show signs of congestive heart failure, including:
- Difficulty breathing, with neck veins that stick out
- Enlarged heart
- Fluid in the lungs
- Rapid heartbeat
- Swelling in both lower legs
A person with late-stage beriberi may be confused or have memory loss and delusions. The person may be less able to sense vibrations. The person may appear poorly nourished.
A physical examination of the nervous and muscular system may show signs of damage to many nerve systems:
- Changes in walking
- Coordination problems
- Abnormal eye movement
- Drooping of the eyelids
- Decreased or abnormal reflexes
- Fast pulse (heart rate)
- Low blood pressure
- Low body temperature
- Muscle weakness and atrophy (loss of tissue mass)
- Problems with walk (gait) and coordination.
For practical reasons, replacing thiamine as an initial test may be most feasible 15. If the patient responds to thiamine administration, it is safe to assume that a measure of thiamine deficiency was responsible for the signs and symptoms 15. Thiamine is not toxic in high levels, which means that this route carries little risk. In addition, time is saved in treating the patient and money is saved in testing. However, although observation of a patient’s clinical response to thiamine administration remains the easiest, least expensive form of testing, clinicians usually miss the subclinical forms of thiamine deficiency 15.
The diagnosis of Wernicke’s encephalopathy is a histopathological diagnosis, made after a postmortem examination of the brain 16, 17, 18.
The Caine criteria have been described to have a sensitivity or 85% and specificity of 100% for Wernicke encephalopathy, in the alcoholic population 19, 10. Because of the strong overlap, the Caine criteria can be used to help screen for Korsakoff syndrome as well.
Caine criteria for the diagnosis of Wernicke encephalopathy in chronic alcoholics 19. When 2 out of these 4 criteria apply, the clinical diagnosis of Wernicke encephalopathy is made 10, 19:
- Dietary deficiencies
- Undernutrition (body mass index <2 SD below normal)
- A history of grossly impaired dietary intake
- An abnormal thiamine status
- Oculomotor abnormalities
- Ophthalmoplegia
- Nystagmus
- Gaze palsy
- Cerebellar dysfunction
- Unsteadiness or ataxia
- Abnormalities of past pointing
- Dysdiadokokinesia
- Impaired heel-shin testing
- Either an altered mental state OR mild memory impairment
- Altered mental status
- Disorientation in two of three fields
- Confused
- An abnormal digit span
- Comatose
- Mild memory impairment
- Failure to remember two or more words in the four-item memory test
- Impairment on more elaborate neuropsychological tests of memory function
- Altered mental status
The following tests are used to check a person’s nutrition level:
- Serum albumin (relates to person’s general nutrition)
- Transketolase activity in red blood cells (reduced in people with thiamine deficiency). The serum level of thiamin is not a reliable indicator of thiamin status. However, thiamin function can be measured by red blood cells transketolase activity (erythrocytes transketolase activity or ETKA). Red blood cells transketolase activity (EKTA) of 0 to 15% is considered adequate, 15 to 25% is considered a moderate risk, and 25% or higher is considered high risk for thiamin deficiency 20, 21.
- Serum vitamin B1 or thiamine levels. Direct measurement of erythrocyte thiamin pyrophosphate (TPP) can be done using whole-blood testing and has more sensitivity, specificity, precision, and robustness 20. The concentration of TPP in the whole blood ranges from 70 to 180 nmol/L 22.
- Urine tests to see if thiamine is passing through the urine. Urinary thiamine excretion can be used to measure adequate dietary intake. However, it does not reflect the thiamine stores in the body. In adults, urinary thiamine excretion of <100 mcg/day suggests inadequate intake, and less than 40 mcg/day suggests thiamin deficiency 23.
- Liver enzymes may be high in people with a history of long-term alcohol abuse.
A brain MRI may show changes in the tissue of the brain. But if Wernicke-Korsakoff syndrome is suspected, treatment should start immediately. Usually a brain MRI exam is not needed.
Thiamine deficiency treatment
In suspected cases of thiamine deficiency, prompt administration of parenteral (intravenously or intramuscularly) thiamine is indicated.
To treat mild thiamine deficiency, the World Health Organization (WHO) recommends daily oral doses of 10 mg thiamine for a week, followed by 3–5 mg/daily for at least 6 weeks 24. For patients at risk of thiamine deficiency or with confirmed thiamine deficiency, parenteral (intravenously or intramuscularly) thiamine of 100 mg and 200 mg 3 times a day has been used, respectively, in clinical practice 25. The recommended treatment for severe thiamine deficiency consists of 25–30 mg intravenously in infants and 50–100 mg in adults, then 10 mg daily administered intramuscularly for approximately one week, followed by 3–5 mg/day oral thiamine for at least 6 weeks 26.
The preferred dose of thiamine treatment for Wernicke encephalopathy may be as high as 500 mg intravenous thiamine given three times daily for 3 to 5 days, followed by intravenous thiamine, 250 mg/day for 3 to 5 days or until the symptoms disappear, and then further treatment with oral thiamine, 100 mg/day 174, 8. The rationale for using three times daily dosing of intravenous thiamine in acute presentations is based on the short half-life of intravenous thiamine (96 minutes) and the slow, carrier mediated process of thiamine transport across the blood–brain barrier 41. A single intravenous dose of thiamine is less likely to achieve sufficient brain tissue levels, and the bioavailability of oral thiamine hydrochloride is only 3.7% to 5.3% 174.
All malnourished patient may need higher doses of thiamine 8. Thiamine is generally administered before or together with glucose solutions because the glucose oxidation can decrease thiamine levels thereby exacerbating the neurological symptoms of Wernicke encephalopathy 8. Patients with magnesium deficiency should also be treated as this can result in reduced recovery from Wernicke encephalopathy especially in patients with alcoholism 27, 14, 28. Following a review of 19 papers, it has been recommended not to delay in correcting hypoglycemia 29. There are suggestions that prolonged and not acute replacement of glucose without thiamine supplementation increased the risk of Wernicke encephalopathy.
For Korsakoff syndrome high dose thiamine at 500 mg to 1500 mg, IV, three times daily for at least 3 days 10. Electrolyte abnormalities should be corrected and fluids replaced. In particular, magnesium requires replacement, as thiamine-dependent enzymes cannot operate in a magnesium-deficient state. Many patients will present needing glucose replacement as well, and traditionally it was thought that replacing glucose before thiamine could exacerbate the patient’s symptoms 30.
Thiamine, even at high concentrations, is not toxic in a person with normal kidney function 31. No cases of thiamine toxicity have been reported from the use of thiamine at the dosages indicated, even in patients in critical condition 31.
Once clinical symptoms improve, thiamine supplementation can switch to the oral route with a dose range of 50 to 100 mg per day 32. It is equally important in individuals with thiamine deficiency to require other nutrient supplementation such as magnesium, vitamin B2 (riboflavin), vitamin B3 (nicotinamide), vitamin B6 (pyridoxine), vitamin B12, vitamin C, potassium, and phosphate 26.
Support for cardiac function is necessary in cases of wet beriberi, because lack of cardiac support leads to low-output cardiac failure when the thiamine deficiency is corrected 31.
Follow-up care until delivery of current pregnancy, intensive care for advanced cardiomyopathy, definitive care for hyperthyroidism, or further workup of intestinal derangement may be warranted in patients with thiamine deficiency 31.
Blood tests may be repeated after the treatment is started. These tests will show how well you are responding to the medicine.
After the acute phase of vitamin and electrolyte replacement, there is mounting evidence that memory rehabilitation is beneficial in Korsakoff syndrome. Declarative memory (“knowing what”) seems to be most affected in Korsakoff syndrome, leading to many patients requiring lifelong care. Because procedural learning (“knowing how”) seems to remain somewhat maintained in Korsakoff syndrome, memory rehabilitation focussed in this area has shown promising outcomes. There has been some success in small Korsakoff syndrome patient populations in learning procedures and improving their autonomy 13.
Thiamine deficiency recovery time
Beriberi can be quickly fatal or can slowly rob an individual of almost all energy for even the simplest of daily activities. However, beriberi is one of the most easily treatable thiamine deficiency, with a remarkable recovery being possible even in severe cases 33. Therefore, the patient prognosis for beriberi is usually good, unless patients have established Korsakoff syndrome. While thiamine can induce partial improvement, the neuropsychological deficits persist in many cases. The confusional state usually improves when IV thiamine is administered but the learning and memory deficits only improve partially. A small number of patients fail to have any improvement and may develop Korsakoff psychosis or Korsakoff syndrome, which often requires institutionalization. Very few individuals recover at this point.
In cases of wet beriberi, clinical improvement can be observed within 12 hours of treatment, with normalization of heart function and size occurring in 1 or 2 days 33. The recovery is so dramatic that treatment with thiamine is a diagnostic test, which can be used in cases of acute heart failure and insidious peripheral neuropathy 33.
A retrospective study by Harel et al 34 indicated that thiamine deficiency in infancy can lead to long-term motor function problems. The study looked at children aged 5-6 years who, during the first 2 years of life, had been fed a faulty milk substitute that was deficient in thiamine, comparing them with age-matched controls. The Movement Assessment Battery for Children and the Zuk Assessment indicated that motor function difficulties existed in 56% and 59%, respectively, of the thiamine-deficient formula group, compared with 10% and 3%, respectively, of the control group. The results suggested that infantile thiamine deficiency affects gross and fine motor function, as well as balance skills 34.
Thiamine deficiency prognosis
Untreated, beriberi can be fatal. With treatment, symptoms usually improve quickly. Heart damage is usually reversible. A full recovery is expected in these cases. However, if acute heart failure has already occurred, the outlook is poor.
Nervous system damage is also reversible, if caught early. High suspicion for Wernicke’s encephalopathy is key to improving patient prognosis. Classically, the thinking was that once Korsakoff syndrome has set in, memory loss (amnesia) was generally irreversible, even with treatment 175, 176, 30. Several case studies and eight double-blind trials have been published, where Korsakoff syndrome patients were treated with clonidine, fluvoxamine, reboxetine, or rivastigmine. Together, these studies did not produce any consistent evidence for the efficacy of any of these interventions 177. Therefore, until this date, no effective pharmacological treatment for Korsakoff syndrome is available 70. More recent research has shown promise in memory rehabilitation including memory compensation techniques and error-less learning strategies 70. If a person with Wernicke encephalopathy receives thiamine replacement, language problems, unusual eye movements, and walking difficulties may go away. However, Korsakoff syndrome or Korsakoff psychosis tends to develop as Wernicke symptoms go away.
Regarding neuroimaging, associations with cortical lesions have shown to correlate with a worse prognosis 10.
- Dabar G, Harmouche C, Habr B, Riachi M, Jaber B. Shoshin Beriberi in Critically-Ill patients: case series. Nutrition Journal. 2015;14:51. doi:10.1186/s12937-015-0039-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4443551/[↩]
- Hemodynamic studies in beriberi heart disease. Akbarian M, Yankopoulos NA, Abelmann WH. Am J Med. 1966 Aug; 41(2):197-212. https://www.ncbi.nlm.nih.gov/pubmed/5912298/[↩]
- Thiamine supplementation in the critically ill. Manzanares W, Hardy G. Curr Opin Clin Nutr Metab Care. 2011 Nov; 14(6):610-7. https://www.ncbi.nlm.nih.gov/pubmed/21912244/[↩]
- Wiley KD, Gupta M. Vitamin B1 Thiamine Deficiency. [Updated 2022 Jul 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537204[↩][↩][↩][↩]
- Wooley, J.A. (2008), Characteristics of Thiamin and Its Relevance to the Management of Heart Failure. Nutr Clin Pract, 23: 487-493. https://doi.org/10.1177/0884533608323430[↩][↩]
- Attaluri P, Castillo A, Edriss H, Nugent K. Thiamine Deficiency: An Important Consideration in Critically Ill Patients. Am J Med Sci. 2018 Oct;356(4):382-390. doi: 10.1016/j.amjms.2018.06.015[↩]
- Karuppagounder SS, Xu H, Pechman D, Chen LH, DeGiorgio LA, Gibson GE. Translocation of amyloid precursor protein C-terminal fragment(s) to the nucleus precedes neuronal death due to thiamine deficiency-induced mild impairment of oxidative metabolism. Neurochem Res. 2008 Jul;33(7):1365-72. doi: 10.1007/s11064-008-9594-z[↩]
- Vasan S, Kumar A. Wernicke Encephalopathy. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470344[↩][↩][↩][↩][↩][↩][↩]
- Wernicke-Korsakoff syndrome. https://medlineplus.gov/ency/article/000771.htm[↩][↩][↩][↩]
- Sharp CS, Wilson MP, Nordstrom K. Psychiatric Emergencies for Clinicians: Emergency Department Management of Wernicke-Korsakoff Syndrome. J Emerg Med. 2016 Oct;51(4):401-404. doi: 10.1016/j.jemermed.2016.05.044[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Karakonstantis S, Galani D, Korela D, Maragou S, Arna D, Basta M. Missing the early signs of thiamine deficiency. A case associated with a liquid-only diet. Nutr Neurosci. 2020 May;23(5):384-386. doi: 10.1080/1028415X.2018.1507964[↩][↩]
- Oudman, E., Wijnia, J.W., Oey, M.J., van Dam, M.J. and Postma, A. (2018), Preventing Wernicke’s encephalopathy in anorexia nervosa: A systematic review. Psychiatry Clin. Neurosci., 72: 774-779. https://doi.org/10.1111/pcn.12735[↩][↩]
- Oudman E, Nijboer TC, Postma A, Wijnia JW, Van der Stigchel S. Procedural Learning and Memory Rehabilitation in Korsakoff’s Syndrome – a Review of the Literature. Neuropsychol Rev. 2015 Jun;25(2):134-48. doi: 10.1007/s11065-015-9288-7[↩][↩][↩][↩]
- Johnson JM, Fox V. Beyond Thiamine: Treatment for Cognitive Impairment in Korsakoff’s Syndrome. Psychosomatics. 2018 Jul-Aug;59(4):311-317. doi: 10.1016/j.psym.2018.03.011[↩][↩][↩][↩]
- Beriberi (Thiamine Deficiency) Workup. https://emedicine.medscape.com/article/116930-workup[↩][↩][↩][↩][↩][↩]
- Colmant H. Enzephalopathien Bei Chronischem Alkoholismus. Stuttgart: Enke; 1965.[↩][↩]
- Harper CG, Giles M, Finlay-Jones R. Clinical signs in the Wernicke-Korsakoff complex: a retrospective analysis of 131 cases diagnosed at necropsy. J Neurol Neurosurg Psychiatry. 1986 Apr;49(4):341-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1028756/pdf/jnnpsyc00096-0001.pdf[↩][↩]
- Torvik A. Wernicke’s encephalopathy–prevalence and clinical spectrum. Alcohol Alcohol Suppl. 1991;1:381-4.[↩][↩]
- Caine D, Halliday GM, Kril JJ, Harper CG. Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol Neurosurg Psychiatry. 1997 Jan;62(1):51-60. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486695/pdf/jnnpsyc00001-0059.pdf[↩][↩][↩][↩][↩][↩]
- Talwar D, Davidson H, Cooney J, St JO’Reilly D. Vitamin B(1) status assessed by direct measurement of thiamin pyrophosphate in erythrocytes or whole blood by HPLC: comparison with erythrocyte transketolase activation assay. Clin Chem. 2000 May;46(5):704-10.[↩][↩][↩][↩]
- Bates CJ. Vitamin analysis. Ann Clin Biochem. 1997 Nov;34 ( Pt 6):599-626. doi: 10.1177/000456329703400604[↩][↩]
- Frank, L.L. (2015), Thiamin in Clinical Practice. Journal of Parenteral and Enteral Nutrition, 39: 503-520. https://doi.org/10.1177/0148607114565245[↩][↩][↩][↩]
- Gibson GE, Blass JP. Thiamine-dependent processes and treatment strategies in neurodegeneration. Antioxid Redox Signal. 2007 Oct;9(10):1605-19. doi: 10.1089/ars.2007.1766[↩][↩][↩]
- Thiamine deficiency and its prevention and control in major emergencies. 23 February 1999. https://www.who.int/publications/i/item/WHO-NHD-99.13[↩][↩]
- Galvin, R., Bråthen, G., Ivashynka, A., Hillbom, M., Tanasescu, R. and Leone, M.A. (2010), EFNS guidelines for diagnosis, therapy and prevention of Wernicke encephalopathy. European Journal of Neurology, 17: 1408-1418. https://doi.org/10.1111/j.1468-1331.2010.03153.x[↩][↩]
- Thiamin. https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Onishi H, Ishida M, Uchida N, Shintani D, Nishikawa T, Hasegawa K, Fujiwara K, Akechi T. Subclinical thiamine deficiency identified by preoperative evaluation in an ovarian cancer patient: Diagnosis and the need for preoperative thiamine measurement. Palliat Support Care. 2019 Oct;17(5):609-610. doi: 10.1017/S1478951518000615[↩][↩]
- Oudman E, Wijnia JW, van Dam M, Biter LU, Postma A. Preventing Wernicke Encephalopathy After Bariatric Surgery. Obes Surg. 2018 Jul;28(7):2060-2068. doi: 10.1007/s11695-018-3262-4[↩][↩]
- Schabelman E, Kuo D. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012 Apr;42(4):488-94. doi: 10.1016/j.jemermed.2011.05.076[↩][↩]
- Covell T, Siddiqui W. Korsakoff Syndrome. [Updated 2023 Jan 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539854[↩][↩][↩][↩]
- Beriberi (Thiamine Deficiency) Treatment & Management. https://emedicine.medscape.com/article/116930-treatment[↩][↩][↩][↩][↩][↩][↩][↩]
- Sriram, K., Manzanares, W. and Joseph, K. (2012), Thiamine in Nutrition Therapy. Nutrition in Clinical Practice, 27: 41-50. https://doi.org/10.1177/0884533611426149[↩][↩][↩][↩][↩]
- Beriberi (Thiamine Deficiency). https://emedicine.medscape.com/article/116930-overview#a7[↩][↩][↩][↩][↩][↩]
- Harel Y, Zuk L, Guindy M, Nakar O, Lotan D, Fattal-Valevski A. The effect of subclinical infantile thiamine deficiency on motor function in preschool children. Matern Child Nutr. 2017 Oct;13(4):e12397. doi: 10.1111/mcn.12397[↩][↩][↩][↩]
- Okafor C, Nimmagadda M, Soin S, Lanka L. Non-alcoholic Wernicke encephalopathy: great masquerader. BMJ Case Rep. 2018 Dec 27;11(1):e227731. doi: 10.1136/bcr-2018-227731[↩]
- Said HM. Thiamin. In: Coates PM, Betz JM, Blackman MR, et al., eds. Encyclopedia of Dietary Supplements. 2nd ed. London and New York: Informa Healthcare; 2010:748-53.[↩][↩][↩][↩][↩][↩][↩][↩]
- Sharma S, Sheehy T, Kolonel LN. Ethnic differences in grains consumption and their contribution to intake of B-vitamins: results of the Multiethnic Cohort Study. Nutr J. 2013 May 20;12:65. doi: 10.1186/1475-2891-12-65[↩][↩]
- Fulgoni VL 3rd, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J Nutr. 2011 Oct;141(10):1847-54. doi: 10.3945/jn.111.142257[↩][↩][↩]
- Saldanha LG, Dwyer JT, Bailen RA. Modernization of the National Institutes of Health Dietary Supplement Label Database. J Food Compost Anal. 2021 Sep;102:104058. doi: 10.1016/j.jfca.2021.104058[↩]
- Bettendorff L. Thiamin. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:261-79.[↩][↩][↩][↩]
- Wilson RB. Pathophysiology, prevention, and treatment of beriberi after gastric surgery. Nutr Rev. 2020 Dec 1;78(12):1015-1029. doi: 10.1093/nutrit/nuaa004[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Bemeur C, Butterworth RF. Thiamin. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:317-24.[↩][↩][↩][↩][↩][↩][↩]
- Thiamine. Monograph. Altern Med Rev. 2003 Feb;8(1):59-62.[↩]
- Tallaksen CM, Sande A, Bøhmer T, Bell H, Karlsen J. Kinetics of thiamin and thiamin phosphate esters in human blood, plasma and urine after 50 mg intravenously or orally. Eur J Clin Pharmacol. 1993;44(1):73-8. doi: 10.1007/BF00315284[↩]
- Lonsdale D. A review of the biochemistry, metabolism and clinical benefits of thiamin(e) and its derivatives. Evid Based Complement Alternat Med. 2006 Mar;3(1):49-59. doi: 10.1093/ecam/nek009[↩]
- Bettendorff, L. and Wins, P. (2009), Thiamin diphosphate in biological chemistry: new aspects of thiamin metabolism, especially triphosphate derivatives acting other than as cofactors. The FEBS Journal, 276: 2917-2925. https://doi.org/10.1111/j.1742-4658.2009.07019.x[↩]
- Manzetti S, Zhang J, van der Spoel D. Thiamin function, metabolism, uptake, and transport. Biochemistry. 2014 Feb 11;53(5):821-35. doi: 10.1021/bi401618y[↩]
- Nabokina SM, Said HM. A high-affinity and specific carrier-mediated mechanism for uptake of thiamine pyrophosphate by human colonic epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2012 Aug 1;303(3):G389-95. doi: 10.1152/ajpgi.00151.2012[↩]
- Lonsdale D. Thiamin. Adv Food Nutr Res. 2018;83:1-56. doi: 10.1016/bs.afnr.2017.11.001[↩][↩][↩]
- Thiamin. https://lpi.oregonstate.edu/mic/vitamins/thiamin[↩][↩][↩][↩]
- Thiamin. https://ods.od.nih.gov/factsheets/Thiamin-Consumer[↩][↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998[↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. What We Eat in America, 2013-2014. 2012. https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweia-data-tables/[↩]
- The USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/[↩]
- Institute of Medicine. Food and Nutrition Board. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: National Academy Press; 1998.[↩][↩]
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 27. Nutrient Data Laboratory home page, 2014. https://ndb.nal.usda.gov/ndb/[↩]
- World Health Organization. Geneva: Department of Nutrition for Health and Development, WHO; 1999. Thiamine deficiency and its prevention and control in major emergencies. Report no: WHO/NHD/99.13.[↩]
- Fattal-Valevski A, Kesler A, Sela BA, Nitzan-Kaluski D, Rotstein M, Mesterman R, Toledano-Alhadef H, Stolovitch C, Hoffmann C, Globus O, Eshel G. Outbreak of life-threatening thiamine deficiency in infants in Israel caused by a defective soy-based formula. Pediatrics. 2005 Feb;115(2):e233-8. https://doi.org/10.1542/peds.2004-1255[↩]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Vitamin B. [Updated 2021 May 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548710[↩][↩]
- Thomson AD, Baker H, Leevy CM. Patterns of 35S-thiamine hydrochloride absorption in the malnourished alcoholic patient. J Lab Clin Med. 1970 Jul;76(1):34-45.[↩]
- Thomson AD, Jeyasingham MD, Pratt OE, Shaw GK. Nutrition and alcoholic encephalopathies. Acta Med Scand Suppl. 1987;717:55-65. doi: 10.1111/j.0954-6820.1987.tb13042.x[↩]
- Kumar N. Neurologic presentations of nutritional deficiencies. Neurol Clin. 2010 Feb;28(1):107-70. doi: 10.1016/j.ncl.2009.09.006[↩]
- Kerns JC, Arundel C, Chawla LS. Thiamin deficiency in people with obesity. Adv Nutr. 2015 Mar 13;6(2):147-53. doi: 10.3945/an.114.007526[↩]
- Hutson SM, Sweatt AJ, Lanoue KF. Branched-chain [corrected] amino acid metabolism: implications for establishing safe intakes. J Nutr. 2005 Jun;135(6 Suppl):1557S-64S. doi: 10.1093/jn/135.6.1557S. Erratum in: J Nutr. 2005 Aug;135(8):2009.[↩]
- Beriberi (Thiamine Deficiency) Clinical Presentation. https://emedicine.medscape.com/article/116930-clinical[↩][↩]
- Martel JL, Kerndt CC, Doshi H, et al. Vitamin B1 (Thiamine) [Updated 2022 Aug 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482360[↩][↩][↩][↩][↩]
- Yamasaki H, Tada H, Kawano S, Aonuma K. Reversible pulmonary hypertension, lactic acidosis, and rapidly evolving multiple organ failure as manifestations of shoshin beriberi. Circ J. 2010 Sep;74(9):1983-5. doi: 10.1253/circj.cj-10-0202[↩][↩]
- Tanphaichitr V. Thiamin. In: Shils M, ed. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins; 1999:381-389.[↩][↩][↩][↩]
- Donnino M. Gastrointestinal beriberi: a previously unrecognized syndrome. Ann Intern Med. 2004 Dec 7;141(11):898-9. doi: 10.7326/0003-4819-141-11-200412070-00035[↩][↩]
- Arts NJ, Walvoort SJ, Kessels RP. Korsakoff’s syndrome: a critical review. Neuropsychiatr Dis Treat. 2017 Nov 27;13:2875-2890. doi: 10.2147/NDT.S130078[↩][↩][↩][↩]
- Thomson AD, Guerrini I, Marshall EJ. The evolution and treatment of Korsakoff’s syndrome: out of sight, out of mind? Neuropsychol Rev. 2012 Jun;22(2):81-92. doi: 10.1007/s11065-012-9196-z[↩]
- ROBERTA AGABIO, THIAMINE ADMINISTRATION IN ALCOHOL-DEPENDENT PATIENTS, Alcohol and Alcoholism, Volume 40, Issue 2, March/April 2005, Pages 155–156, https://doi.org/10.1093/alcalc/agh106[↩][↩]
- ALLAN D. THOMSON, E. JANE MARSHALL, THE NATURAL HISTORY AND PATHOPHYSIOLOGY OF WERNICKE’S ENCEPHALOPATHY AND KORSAKOFF’S PSYCHOSIS, Alcohol and Alcoholism, Volume 41, Issue 2, March/April 2006, Pages 151–158, https://doi.org/10.1093/alcalc/agh249[↩]
- Talland G. Deranged Memory: A Psychonomic Study of the Amnesic Syndrome. New York: Academic Press; 1965.[↩]
- Kopelman MD. The Korsakoff syndrome. Br J Psychiatry. 1995 Feb;166(2):154-73. doi: 10.1192/bjp.166.2.154[↩]
- Michael D. Kopelman, Allan D. Thomson, Irene Guerrini, E. Jane Marshall, The Korsakoff Syndrome: Clinical Aspects, Psychology and Treatment, Alcohol and Alcoholism, Volume 44, Issue 2, March-April 2009, Pages 148–154, https://doi.org/10.1093/alcalc/agn118[↩][↩]
- Segal JB, Bouffard MA, Schlaug G. Characteristic Neuroimaging Abnormalities of Korsakoff Syndrome. JAMA Neurol. 2016;73(10):1248–1249. doi:10.1001/jamaneurol.2016.1843[↩]
- Nikolakaros G, Ilonen T, Kurki T, Paju J, Papageorgiou SG, Vataja R. Non-alcoholic Korsakoff syndrome in psychiatric patients with a history of undiagnosed Wernicke’s encephalopathy. J Neurol Sci. 2016 Nov 15;370:296-302. doi: 10.1016/j.jns.2016.09.025[↩]
- Isenberg-Grzeda E, Rahane S, DeRosa AP, Ellis J, Nicolson SE. Wernicke-Korsakoff syndrome in patients with cancer: a systematic review. Lancet Oncol. 2016 Apr;17(4):e142-e148. doi: 10.1016/S1470-2045(16)00037-1[↩]
- World Health Organization, United Nations High Commissioner for Refugees. Thiamine deficiency and its prevention and control in major emergencies. https://apps.who.int/iris/bitstream/handle/10665/66139/WHO_NHD_99.13.pdf[↩][↩][↩][↩][↩][↩][↩]
- Lakhani SV, Shah HN, Alexander K, Finelli FC, Kirkpatrick JR, Koch TR. Small intestinal bacterial overgrowth and thiamine deficiency after Roux-en-Y gastric bypass surgery in obese patients. Nutr Res. 2008 May;28(5):293-8. doi: 10.1016/j.nutres.2008.03.002[↩][↩]
- Shah HN, Bal BS, Finelli FC, Koch TR. Constipation in patients with thiamine deficiency after Roux-en-Y gastric bypass surgery. Digestion. 2013;88(2):119-24. doi: 10.1159/000353245[↩][↩][↩]
- DiNicolantonio, J.J., Niazi, A.K., Lavie, C.J., O’Keefe, J.H. and Ventura, H.O. (2013), Thiamine Supplementation for the Treatment of Heart Failure: A Review of the Literature. Congest Heart Fail, 19: 214-222. https://doi.org/10.1111/chf.12037[↩][↩][↩][↩]
- Brown, G. (2014), Defects of thiamine transport and metabolism. J Inherit Metab Dis, 37: 577-585. https://doi.org/10.1007/s10545-014-9712-9[↩][↩]
- Beriberi. https://medlineplus.gov/ency/article/000339.htm[↩][↩]
- Rindi G. Thiamin. In: Ziegler E, Filer L, eds. Present Knowledge in Nutrition. Washington D.C.: ILSI Press; 1996:160-166.[↩]
- Arnold D. British India and the “beriberi problem”, 1798-1942. Med Hist. 2010 Jul;54(3):295-314. doi: 10.1017/s0025727300004622[↩][↩]
- Baeltz B. Ueber das Verhältniss der multiplen peripherischen Neuritis zur Beriberi (Panneuritis endemica) [in German]. Z Klin Med. 1882;4:616–617.[↩]
- Truswell, A.S. (2000), Australian experience with the Wernicke–Korsakoff syndrome. Addiction, 95: 829-832. https://doi.org/10.1046/j.1360-0443.2000.9568291.x[↩]
- Beriberi (Thiamine Deficiency). https://emedicine.medscape.com/article/116930-overview[↩][↩]
- Greenspon J, Perrone EE, Alaish SM. Shoshin beriberi mimicking central line sepsis in a child with short bowel syndrome. World J Pediatr. 2010 Nov;6(4):366-8. doi: 10.1007/s12519-010-0022-5[↩]
- Saad L, Silva LF, Banzato CE, Dantas CR, Garcia C Jr. Anorexia nervosa and Wernicke-Korsakoff syndrome: a case report. J Med Case Rep. 2010 Jul 20;4:217. doi: 10.1186/1752-1947-4-217[↩]
- Jung ES, Kwon O, Lee SH, Lee KB, Kim JH, Yoon SH, Kim GM, Jeung HC, Rha SY. Wernicke’s encephalopathy in advanced gastric cancer. Cancer Res Treat. 2010 Jun;42(2):77-81. doi: 10.4143/crt.2010.42.2.77[↩]
- Becker DA, Balcer LJ, Galetta SL. The Neurological Complications of Nutritional Deficiency following Bariatric Surgery. J Obes. 2012;2012:608534. doi: 10.1155/2012/608534[↩]
- Nath A, Tran T, Shope TR, Koch TR. Prevalence of clinical thiamine deficiency in individuals with medically complicated obesity. Nutr Res. 2017 Jan;37:29-36. doi: 10.1016/j.nutres.2016.11.012[↩]
- Polegato, B.F., Pereira, A.G., Azevedo, P.S., Costa, N.A., Zornoff, L.A.M., Paiva, S.A.R. and Minicucci, M.F. (2019), Role of Thiamin in Health and Disease. Nutrition in Clinical Practice, 34: 558-564. https://doi.org/10.1002/ncp.10234[↩]
- Oudman E, Wijnia JW, Oey M, van Dam M, Painter RC, Postma A. Wernicke’s encephalopathy in hyperemesis gravidarum: A systematic review. Eur J Obstet Gynecol Reprod Biol. 2019 May;236:84-93. doi: 10.1016/j.ejogrb.2019.03.006[↩]
- Meggs WJ, Lee SK, Parker-Cote JN. Wernicke encephalopathy associated with hyperemesis gravidarum. Am J Emerg Med. 2020 Mar;38(3):690.e3-690.e5. doi: 10.1016/j.ajem.2019.09.012[↩]
- Sequeira Lopes da Silva JT, Almaraz Velarde R, Olgado Ferrero F, Robles Marcos M, Pérez Civantos D, Ramírez Moreno JM, Luengo Pérez LM. Wernicke’s encephalopathy induced by total parental nutrition. Nutr Hosp. 2010 Nov-Dec;25(6):1034-6.[↩]
- Francini-Pesenti F, Brocadello F, Manara R, Santelli L, Laroni A, Caregaro L. Wernicke’s syndrome during parenteral feeding: not an unusual complication. Nutrition. 2009 Feb;25(2):142-6. doi: 10.1016/j.nut.2008.08.003[↩]
- Zastre JA, Sweet RL, Hanberry BS, Ye S. Linking vitamin B1 with cancer cell metabolism. Cancer Metab. 2013 Jul 24;1(1):16. doi: 10.1186/2049-3002-1-16[↩]
- Thurnham DI, Cathcart AE, Livingstone MB. A retrospective investigation of thiamin and energy intakes following an outbreak of beriberi in The Gambia. Nutrients. 2011 Jan;3(1):135-51. doi: 10.3390/nu3010135[↩][↩]
- Seligmann H, Levi R, Konijn AM, Prokocimer M. Thiamine deficiency in patients with B-chronic lymphocytic leukaemia: a pilot study. Postgrad Med J. 2001 Sep;77(911):582-5. doi: 10.1136/pmj.77.911.582[↩]
- Koike H, Misu K, Hattori N, Ito S, Ichimura M, Ito H, Hirayama M, Nagamatsu M, Sasaki I, Sobue G. Postgastrectomy polyneuropathy with thiamine deficiency. J Neurol Neurosurg Psychiatry. 2001 Sep;71(3):357-62. doi: 10.1136/jnnp.71.3.357[↩]
- Spinazzi M, Angelini C, Patrini C. Subacute sensory ataxia and optic neuropathy with thiamine deficiency. Nat Rev Neurol. 2010 May;6(5):288-93. doi: 10.1038/nrneurol.2010.16[↩]
- Sobue G, Li M, Terao S, Aoki S, Ichimura M, Ieda T, Doyu M, Yasuda T, Hashizume Y, Mitsuma T. Axonal pathology in Japanese Guillain-Barré syndrome: a study of 15 autopsied cases. Neurology. 1997 Jun;48(6):1694-700. doi: 10.1212/wnl.48.6.1694[↩]
- Ohnishi A, Tsuji S, Igisu H, Murai Y, Goto I, Kuroiwa Y, Tsujihata M, Takamori M. Beriberi neuropathy. Morphometric study of sural nerve. J Neurol Sci. 1980 Mar;45(2-3):177-90. doi: 10.1016/0022-510x(80)90164-1[↩]
- Koike, H., Iijima, M., Sugiura, M., Mori, K., Hattori, N., Ito, H., Hirayama, M. and Sobue, G. (2003), Alcoholic neuropathy is clinicopathologically distinct from thiamine-deficiency neuropathy. Ann Neurol., 54: 19-29. https://doi.org/10.1002/ana.10550[↩]
- Khounnorath S, Chamberlain K, Taylor AM, Soukaloun D, Mayxay M, Lee SJ, Phengdy B, Luangxay K, Sisouk K, Soumphonphakdy B, Latsavong K, Akkhavong K, White NJ, Newton PN. Clinically unapparent infantile thiamin deficiency in Vientiane, Laos. PLoS Negl Trop Dis. 2011 Feb 22;5(2):e969. doi: 10.1371/journal.pntd.0000969[↩]
- Chiappetta S, Stein J. Refeeding Syndrome: An Important Complication Following Obesity Surgery. Obes Facts. 2016;9(1):12-6. doi: 10.1159/000442534[↩]
- Boateng AA, Sriram K, Meguid MM, Crook M. Refeeding syndrome: treatment considerations based on collective analysis of literature case reports. Nutrition. 2010 Feb;26(2):156-67. doi: 10.1016/j.nut.2009.11.017[↩]
- Marinella MA. Refeeding syndrome: implications for the inpatient rehabilitation unit. Am J Phys Med Rehabil. 2004 Jan;83(1):65-8. doi: 10.1097/01.PHM.0000104666.88102.99[↩]
- Raziel A. Thiamine deficiency after bariatric surgery may lead to Wernicke encephalopathy. Isr Med Assoc J. 2012 Nov;14(11):692-4[↩]
- Krishna S, Taylor AM, Supanaranond W, Pukrittayakamee S, ter Kuile F, Tawfiq KM, Holloway PA, White NJ. Thiamine deficiency and malaria in adults from southeast Asia. Lancet. 1999 Feb 13;353(9152):546-9. doi: 10.1016/s0140-6736(98)06316-8[↩]
- Mayxay M, Taylor AM, Khanthavong M, Keola S, Pongvongsa T, Phompida S, Phetsouvanh R, White NJ, Newton PN. Thiamin deficiency and uncomplicated falciparum malaria in Laos. Trop Med Int Health. 2007 Mar;12(3):363-9. doi: 10.1111/j.1365-3156.2006.01804.x[↩]
- Müri RM, Von Overbeck J, Furrer J, Ballmer PE. Thiamin deficiency in HIV-positive patients: evaluation by erythrocyte transketolase activity and thiamin pyrophosphate effect. Clin Nutr. 1999 Dec;18(6):375-8. doi: 10.1016/s0261-5614(99)80019-3[↩]
- Stanga Z, Brunner A, Leuenberger M, Grimble RF, Shenkin A, Allison SP, Lobo DN. Nutrition in clinical practice-the refeeding syndrome: illustrative cases and guidelines for prevention and treatment. Eur J Clin Nutr. 2008 Jun;62(6):687-94. doi: 10.1038/sj.ejcn.1602854[↩]
- Vimokesant SL, Hilker DM, Nakornchai S, Rungruangsak K, Dhanamitta S. Effects of betel nut and fermented fish on the thiamin status of northeastern Thais. Am J Clin Nutr. 1975 Dec;28(12):1458-63. doi: 10.1093/ajcn/28.12.1458[↩]
- Ventura A, Mafe MC, Bourguet M, Tornero C. Wernicke’s encephalopathy secondary to hyperthyroidism and ingestion of thiaminase-rich products. Neurologia. 2013 May;28(4):257-9. English, Spanish. doi: 10.1016/j.nrl.2012.01.005[↩]
- Bettendorff L. Thiamin. In: Erdman Jr. JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Ames: Wiley-Blackwell; 2012:261-279.[↩]
- Soukaloun D, Lee SJ, Chamberlain K, Taylor AM, Mayxay M, Sisouk K, Soumphonphakdy B, Latsavong K, Akkhavong K, Phommachanh D, Sengmeuang V, Luangxay K, McDonagh T, White NJ, Newton PN. Erythrocyte transketolase activity, markers of cardiac dysfunction and the diagnosis of infantile beriberi. PLoS Negl Trop Dis. 2011 Feb 22;5(2):e971. doi: 10.1371/journal.pntd.0000971[↩]
- Earl JW, McCleary BV. Mystery of the poisoned expedition. Nature. 1994 Apr 21;368(6473):683-4. doi: 10.1038/368683a0[↩]
- MATSUKAWA D, CHANG S, MISAWA H, FUJIMIYA M, KOBAYASHI N, HORIKAWA Y, TAKATO K. Studies on the thiamine deficiency due to bacterial thiaminase. I. Investigations on intestinal contents. J Vitaminol (Kyoto). 1954 Jul 10;1(1):43-8. doi: 10.5925/jnsv1954.1.43[↩]
- Nishimune T, Watanabe Y, Okazaki H, Akai H. Thiamin is decomposed due to Anaphe spp. entomophagy in seasonal ataxia patients in Nigeria. J Nutr. 2000 Jun;130(6):1625-8. doi: 10.1093/jn/130.6.1625[↩]
- Vimokesant, S., Kunjara, S., Rungruangsak, K., Nakornchai, S. and Panijpan, B. (1982), BERIBERI CAUSED BY ANTITHIAMIN FACTORS IN FOOD AND ITS PREVENTION. Annals of the New York Academy of Sciences, 378: 123-136. https://doi.org/10.1111/j.1749-6632.1982.tb31191.x[↩]
- Bender DA. Nutritional Biochemistry of the Vitamins. 1st ed. Cambridge, UK: Cambridge University Press; 2003.[↩][↩]
- Carvajal-Moreno M. Mycotoxins that affect the human cardiovascular system. J Biomol Res Ther. 2015;4:2.[↩]
- Rosa CA, Keller KM, Oliveira AA, Almeida TX, Keller LA, Marassi AC, Kruger CD, Deveza MV, Monteiro BS, Nunes LM, Astoreca A, Cavaglieri LR, Direito GM, Eifert EC, Lima TA, Modernell KG, Nunes FI, Garcia AM, Luz MS, Oliveira DC. Production of citreoviridin by Penicillium citreonigrum strains associated with rice consumption and beriberi cases in the Maranhão State, Brazil. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2010 Feb;27(2):241-8. doi: 10.1080/19440040903289712[↩]
- Sulfiting agents: affirmation of GRAS status. Fed Regis. 1988;53:51065–51084.[↩]
- Sulfites – USA. https://farrp.unl.edu/sulfites-usa[↩]
- https://www.fda.gov/media/80337/download[↩]
- https://www.fda.gov/media/136310/download[↩]
- Suter PM, Haller J, Hany A, Vetter W. Diuretic use: a risk for subclinical thiamine deficiency in elderly patients. J Nutr Health Aging. 2000;4(2):69-71.[↩]
- Rieck J, Halkin H, Almog S, Seligman H, Lubetsky A, Olchovsky D, Ezra D. Urinary loss of thiamine is increased by low doses of furosemide in healthy volunteers. J Lab Clin Med. 1999 Sep;134(3):238-43. doi: 10.1016/s0022-2143(99)90203-2[↩]
- Sica, D.A. (2007), Loop Diuretic Therapy, Thiamine Balance, and Heart Failure. Congestive Heart Failure, 13: 244-247. https://doi.org/10.1111/j.1527-5299.2007.06260.x[↩]
- Zenuk C, Healey J, Donnelly J, Vaillancourt R, Almalki Y, Smith S. Thiamine deficiency in congestive heart failure patients receiving long term furosemide therapy. Can J Clin Pharmacol. 2003 Winter;10(4):184-8.[↩]
- Shimon I, Almog S, Vered Z, Seligmann H, Shefi M, Peleg E, Rosenthal T, Motro M, Halkin H, Ezra D. Improved left ventricular function after thiamine supplementation in patients with congestive heart failure receiving long-term furosemide therapy. Am J Med. 1995 May;98(5):485-90. doi: 10.1016/s0002-9343(99)80349-0[↩]
- Misumida N, Umeda H, Iwase M. Shoshin beriberi induced by long-term administration of diuretics: a case report. Case Rep Cardiol. 2014;2014:878915. doi: 10.1155/2014/878915[↩]
- Hung SC, Hung SH, Tarng DC, Yang WC, Chen TW, Huang TP. Thiamine deficiency and unexplained encephalopathy in hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2001 Nov;38(5):941-7. doi: 10.1053/ajkd.2001.28578[↩]
- Wilcox CS. Do diuretics cause thiamine deficiency? J Lab Clin Med. 1999 Sep;134(3):192-3. doi: 10.1016/s0022-2143(99)90198-1[↩]
- Nixon PF, Diefenbach RJ, Duggleby RG. Inhibition of transketolase and pyruvate decarboxylase by omeprazole. Biochem Pharmacol. 1992 Jul 7;44(1):177-9. doi: 10.1016/0006-2952(92)90053-l[↩][↩]
- Toh JW, Ong E, Wilson R. Hypomagnesaemia associated with long-term use of proton pump inhibitors. Gastroenterol Rep (Oxf). 2015 Aug;3(3):243-53. doi: 10.1093/gastro/gou054[↩][↩]
- Basu TK, Aksoy M, Dickerson JW. Effects of 5-fluorouracil on the thiamin status of adult female rats. Chemotherapy. 1979;25(2):70-6. doi: 10.1159/000237825[↩]
- Cho KP, Lee JS, Seong JS, Woo YM, Cho YJ, Jeong BJ, Sohn JH, Kim SJ. [Two cases of Wernicke´s encephalopathy that developed during total parenteral nutrition in colon cancer patients treated with 5-fluorouracil-based chemotherapy]. Korean J Gastroenterol. 2014 Sep 25;64(3):158-63. Korean. doi: 10.4166/kjg.2014.64.3.158[↩]
- Koenig H, Patel A. Biochemical basis for fluorouracil neurotoxicity. The role of Krebs cycle inhibition by fluoroacetate. Arch Neurol. 1970 Aug;23(2):155-60. doi: 10.1001/archneur.1970.00480260061008[↩]
- Arellano M, Malet-Martino M, Martino R, Gires P. The anti-cancer drug 5-fluorouracil is metabolized by the isolated perfused rat liver and in rats into highly toxic fluoroacetate. Br J Cancer. 1998;77(1):79-86. doi: 10.1038/bjc.1998.12[↩]
- Schümann K. Interactions between drugs and vitamins at advanced age. Int J Vitam Nutr Res. 1999;69:173–178. doi:10.1024/0300-9831.69.3.173[↩]
- Chen L, Shu Y, Liang X, Chen EC, Yee SW, Zur AA, Li S, Xu L, Keshari KR, Lin MJ, Chien HC, Zhang Y, Morrissey KM, Liu J, Ostrem J, Younger NS, Kurhanewicz J, Shokat KM, Ashrafi K, Giacomini KM. OCT1 is a high-capacity thiamine transporter that regulates hepatic steatosis and is a target of metformin. Proc Natl Acad Sci U S A. 2014 Jul 8;111(27):9983-8. doi: 10.1073/pnas.1314939111[↩]
- Liang X, Chien HC, Yee SW, Giacomini MM, Chen EC, Piao M, Hao J, Twelves J, Lepist EI, Ray AS, Giacomini KM. Metformin Is a Substrate and Inhibitor of the Human Thiamine Transporter, THTR-2 (SLC19A3). Mol Pharm. 2015 Dec 7;12(12):4301-10. doi: 10.1021/acs.molpharmaceut.5b00501[↩]
- Subramanya SB, Subramanian VS, Said HM. Chronic alcohol consumption and intestinal thiamin absorption: effects on physiological and molecular parameters of the uptake process. Am J Physiol Gastrointest Liver Physiol. 2010 Jul;299(1):G23-31. doi: 10.1152/ajpgi.00132.2010[↩]
- Salem A, Roland BC. Small intestinal bacterial overgrowth (SIBO). J Gastroint Dig Syst. 2014;4:225.[↩]
- Pelton R, LaValle JB, Hawkins E, Krinsky DL, eds. Drug-Induced Nutrient Depletion Handbook. Hudson, OH: Wolters Kluwer Clinical Drug Information (Lexicomp; );1999:258.[↩]
- Vognar, L. and Stoukides, J. (2009), The Role of Low Plasma Thiamin Levels in Cognitively Impaired Elderly Patients Presenting with Acute Behavioral Disturbances. Journal of the American Geriatrics Society, 57: 2166-2168. https://doi.org/10.1111/j.1532-5415.2009.02542.x[↩]
- T J Wilkinson, H C Hanger, P M George, R Sainsbury, Is thiamine deficiency in elderly people related to age or co-morbidity?, Age and Ageing, Volume 29, Issue 2, March 2000, Pages 111–116, https://doi.org/10.1093/ageing/29.2.111[↩]
- Ito Y, Yamanaka K, Susaki H, Igata A. A cross-investigation between thiamin deficiency and the physical condition of elderly people who require nursing care. J Nutr Sci Vitaminol (Tokyo). 2012;58(3):210-6. doi: 10.3177/jnsv.58.210[↩]
- NICHOLAS P. O’ROURKE, VALDA W. BUNKER, ANITA J. THOMAS, PAUL M. FINGLAS, ANGELA L. BAILEY, BARBARA E. CLAYTON, Thiamine Status of Healthy and Institutionalized Elderly Subjects: Analysis of Dietary Intake and Biochemical Indices, Age and Ageing, Volume 19, Issue 5, September 1990, Pages 325–329, https://doi.org/10.1093/ageing/19.5.325[↩]
- Lu’o’ng KV, Nguyễn LT. The role of thiamine in cancer: possible genetic and cellular signaling mechanisms. Cancer Genomics Proteomics. 2013 Jul-Aug;10(4):169-85.[↩]
- Boldorini R, Vago L, Lechi A, Tedeschi F, Trabattoni GR. Wernicke’s encephalopathy: occurrence and pathological aspects in a series of 400 AIDS patients. Acta Biomed Ateneo Parmense. 1992;63(1-2):43-9.[↩]
- Larsen TR, Dragu D, Williams M. Wernicke’s Encephalopathy: An Unusual Consequence of the Acquired Immune Deficiency Syndrome-Case Report and Literature Review. Case Rep Med. 2013;2013:709474. doi: 10.1155/2013/709474[↩]
- Al-Attas OS, Al-Daghri NM, Alfadda AA, Abd-Alrahman SH, Sabico S. Blood thiamine and its phosphate esters as measured by high-performance liquid chromatography: levels and associations in diabetes mellitus patients with varying degrees of microalbuminuria. J Endocrinol Invest. 2012 Dec;35(11):951-6. doi: 10.3275/8126[↩]
- Thornalley PJ, Babaei-Jadidi R, Al Ali H, Rabbani N, Antonysunil A, Larkin J, Ahmed A, Rayman G, Bodmer CW. High prevalence of low plasma thiamine concentration in diabetes linked to a marker of vascular disease. Diabetologia. 2007 Oct;50(10):2164-70. doi: 10.1007/s00125-007-0771-4[↩]
- Jermendy G. Evaluating thiamine deficiency in patients with diabetes. Diab Vasc Dis Res. 2006 Sep;3(2):120-1. doi: 10.3132/dvdr.2006.014[↩]
- Saito N, Kimura M, Kuchiba A, Itokawa Y. Blood thiamine levels in outpatients with diabetes mellitus. J Nutr Sci Vitaminol (Tokyo). 1987 Dec;33(6):421-30. doi: 10.3177/jnsv.33.421[↩]
- Aasheim ET. Wernicke encephalopathy after bariatric surgery: a systematic review. Ann Surg. 2008 Nov;248(5):714-20. doi: 10.1097/SLA.0b013e3181884308[↩]
- Xanthakos SA. Nutritional deficiencies in obesity and after bariatric surgery. Pediatr Clin North Am. 2009 Oct;56(5):1105-21. doi: 10.1016/j.pcl.2009.07.002[↩]
- Shenoy VV, Patil PV, Nagar VS, Deshpande AK, Shedge RT, Badiye AP, Saigaonkar R. Congestive cardiac failure and anemia in a 15-year-old boy. J Postgrad Med. 2005 Jul-Sep;51(3):225-7.[↩]
- Karaiskos I, Katsarolis I, Stefanis L. Severe dysphagia as the presenting symptom of Wernicke-Korsakoff syndrome in a non-alcoholic man. Neurol Sci. 2008 Feb;29(1):45-6. doi: 10.1007/s10072-008-0859-8[↩]
- Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Front Psychiatry. 2019 Apr 4;10:207. doi: 10.3389/fpsyt.2019.00207[↩]
- Zuccoli G, Gallucci M, Capellades J, Regnicolo L, Tumiati B, Giadás TC, Bottari W, Mandrioli J, Bertolini M. Wernicke encephalopathy: MR findings at clinical presentation in twenty-six alcoholic and nonalcoholic patients. AJNR Am J Neuroradiol. 2007 Aug;28(7):1328-31. doi: 10.3174/ajnr.A0544[↩]
- Mifsud F, Messager D, Jannot AS, Védie B, Balanant NA, Poghosyan T, Flamarion E, Carette C, Lucas-Martini L, Czernichow S, Rives-Lange C. Clinical diagnosis, outcomes and treatment of thiamine deficiency in a tertiary hospital. Clin Nutr. 2022 Jan;41(1):33-39. doi: 10.1016/j.clnu.2021.10.021[↩][↩][↩]
- S. Narasimha Rao, Shalini Mani, Karuna Madap, M. V. Kranthi Kumar, Lalji Singh, Giriraj Ratan Chandak, High Prevalence of Infantile Encephalitic Beriberi with Overlapping Features of Leigh’s Disease, Journal of Tropical Pediatrics, Volume 54, Issue 5, October 2008, Pages 328–332, https://doi.org/10.1093/tropej/fmn031[↩]
- Isenberg-Grzeda E, Shen MJ, Alici Y, Wills J, Nelson C, Breitbart W. High rate of thiamine deficiency among inpatients with cancer referred for psychiatric consultation: results of a single site prevalence study. Psychooncology. 2017 Sep;26(9):1384-1389. doi: 10.1002/pon.4155[↩][↩]
- Jain A, Mehta R, Al-Ani M, Hill JA, Winchester DE. Determining the Role of Thiamine Deficiency in Systolic Heart Failure: A Meta-Analysis and Systematic Review. J Card Fail. 2015 Dec;21(12):1000-7. doi: 10.1016/j.cardfail.2015.10.005[↩][↩]
- Parrott J, Frank L, Rabena R, Craggs-Dino L, Isom KA, Greiman L. American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: Micronutrients. Surg Obes Relat Dis. 2017 May;13(5):727-741. doi: 10.1016/j.soard.2016.12.018[↩][↩]
- Kessels R. Korsakoff syndrome. In: Weiner I, Craighead W, editors. The Corsini Encyclopedia of Psychology. New York: Wiley; 2010. pp. 902–904.[↩]
- Fujiwara E, Brand M, Borsutzky S, Steingass HP, Markowitsch HJ. Cognitive performance of detoxified alcoholic Korsakoff syndrome patients remains stable over two years. J Clin Exp Neuropsychol. 2008 Jul;30(5):576-87. doi: 10.1080/13803390701557271[↩]
- Arts N, Wiersma J. Psychofarmaca bij de behandeling van langetermijngevolgen van chronisch alcoholmisbruik. Psyfar. 2011;(3):54–57.[↩]