Best foods for digestion problems
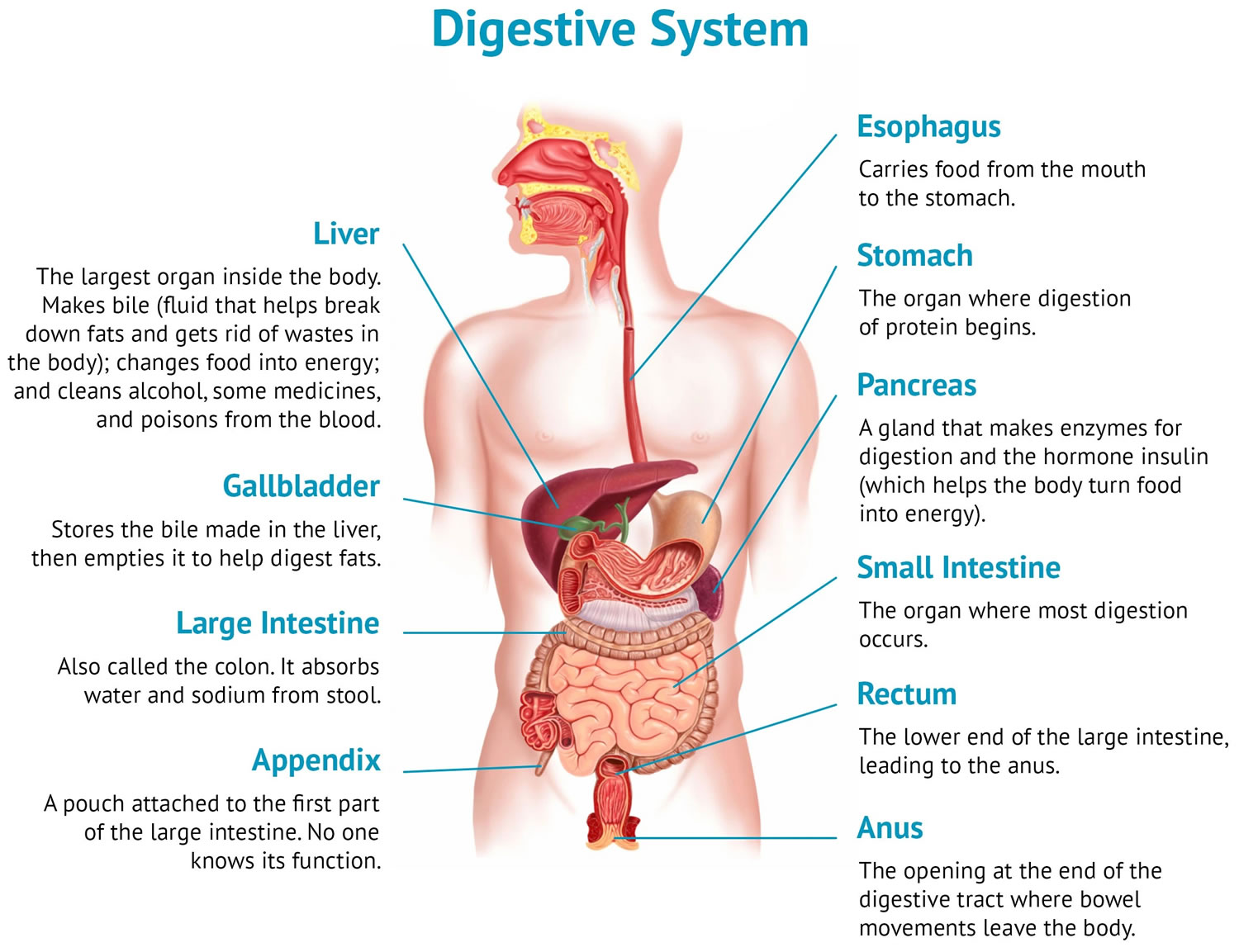
The digestive system begins at the mouth and ends at the anus. The digestive system is made up of the gastrointestinal tract (GI), liver, pancreas, and gallbladder that help your body digest food (break down and absorb food). Digestion is important for breaking down food into nutrients such as carbohydrates like glucose, fats or fatty acids and proteins (amino acids), which your body uses for energy, growth, and cell repair. Unused materials are discarded as feces (poop). The digestive system is a long, twisting tube that starts at your mouth and goes through the esophagus, stomach, small intestine (also called the small bowel), large intestine (also called the large bowel or colon) and anus.
A large reservoir of microbes also known as microbiota, such as bacteria, live within your large intestine and, to a lesser degree, in the rest of your digestive system. These bacteria play an important role in healthy digestion. The exact types of bacteria are particular to each person. Other factors that influence the type of bacteria in your digestive system include where you live in the world, what health conditions you have and what medications you have received.
Some digestive diseases and conditions are acute, lasting only a short time, while others are chronic, or long-lasting.
Some common problems related to the digestive system include:
- Gastro-esophageal reflux (GER) or heartburn: Gastro-esophageal reflux (GER) occurs when acidic stomach contents move from the stomach back up the esophagus. It causes a burning sensation in the chest or throat.
- Diverticulitis: Diverticulitis is caused by inflammation or infection of abnormal pouches in the lower part of the large intestine. It can cause mild or severe pain on the lower left-hand side of the abdomen.
- Stomach ulcers: Stomach ulcers are commonly caused by the bacterium Helicobacter pylori that can live in the stomach. They can cause long-term, low-level inflammation of the stomach lining in some people. It is not well understood why they cause stomach ulcers in some people and not in others.
- Hemorrhoids: Hemorrhoids are itchy or painful lumps that occur in and around the anus. The lumps contain swollen blood vessels. Hemorrhoids can cause bleeding when you go to the toilet (do a poop) — you might notice bright red blood on the toilet paper or in the toilet. If you find blood on the toilet paper or in the toilet, always seek medical advice.
- Colitis – inflammation of the bowel
- Gastroenteritis – an infection that causes vomiting and diarrhea
- Constipation – Constipation is a common condition that makes it difficult to have a bowel movement. A bowel movement occurs when the food you eat passes through your digestive system. The stool can be hard and dry. Sometimes it is painful to pass. Constipation usually means that a person has three or fewer bowel movements in a week. However, people can have different bowel movement patterns, and only you know what’s normal for you. The American College of Gastroenterology defines constipation based upon symptoms including unsatisfactory defecation with either infrequent stools, difficult stool passage or both 1. Constipation is not a disease, but may be a symptom of another medical problem. Any recent change in bowel habits, if persistent, may be cause for concern.
Figure 1. Digestive system
How does the digestive system work?
Each organ of the digestive system has an important role in digestion.
Mouth
Digestion begins in the mouth. When you eat, your teeth chew food into very small pieces. Glands in your cheeks and under your tongue produce saliva that coats the food, making it easier to be chewed and swallowed. Saliva also contains enzymes that start to digest the carbohydrates in food into sugars. Once swallowed, muscular contractions of the esophagus massage the ball of food down into the stomach.
Esophagus
The esophagus is the muscular tube that carries food from your mouth to your stomach after it is swallowed. A ring of muscle at the end of the esophagus called the lower esophageal sphincter (LES) relaxes to let food into the stomach and contracts to prevent stomach contents from escaping back up the esophagus.
Stomach
The stomach wall produces gastric juice (hydrochloric acid and enzymes) that digests proteins. The stomach acts like a concrete mixer, churning and mixing food with gastric juice to form chyme — a thick, soupy liquid. The food is then squeezed through a second sphincter into the first part of the small intestine, called the duodenum.
Small intestine
Once in the duodenum (the first part of the small intestine), the food is mixed with more digestive enzymes from the pancreas and bile from the liver. Bile is produced by your liver and stored in the gallbladder and enzymes in digestive juices from the pancreas empty into the upper section of the small intestine and help to break down protein into amino acids and fat into fatty acids. These smaller particles, along with sugars, vitamins and minerals, are absorbed into the bloodstream through the wall of the small intestine. Nutrients are absorbed from the ileum, which is lined with millions of finger-like projections called villi. Each villus is connected to a mesh of capillaries. This is how nutrients pass into the bloodstream.
It is called small intestine because it is about 3.5cm in diameter, but it is about 5 meters long to provide lots of area for absorption. Most of the chemical digestion of proteins, fats and carbohydrates is completed in the small intestine.
Pancreas
The pancreas is one of the largest glands in the human body. As well as digestive juices, it secretes a hormone called insulin. Insulin helps to regulate the amount of sugar in the blood. Diabetes is a condition caused by problems with insulin production.
Liver
The liver has a number of different roles in the body, including:
- breaking down fats, using bile stored in the gall bladder
- processing proteins and carbohydrates
- filtering and processing impurities, drugs and toxins
- generation of glucose for short-term energy needs from other compounds like lactate and amino acids.
Large intestine and anus
Once all the nutrients have been absorbed, the waste is moved into the large intestine (colon) or bowel. The lining of the large intestine absorbs water, mineral salts and vitamins. Undigested fiber is mixed with mucus and bacteria — which partly break down the fibre — to nourish the cells of the large intestine wall and so help keep the large intestine healthy. Feces are formed and stored in the last part of the large intestine (the rectum) before being passed out of the body through the anus.
Best food for indigestion and gas
Indigestion also known as dyspepsia or upset stomach, is a general term used to describe one or more symptoms including a feeling of fullness during a meal, uncomfortable fullness after a meal, and burning or pain in the upper abdomen 2. Indigestion can feel like a stomachache. Indigestion is not a disease, but rather some symptoms you experience, including abdominal pain and a feeling of fullness soon after you start eating. Indigestion can happen when your body has trouble digesting food. However, indigestion is not always related to eating. Indigestion occurs in your gastrointestinal (GI) tract. Although indigestion is common, each person may experience indigestion in a slightly different way. Symptoms of indigestion may be felt occasionally or it can be an ongoing problem. The symptoms and causes vary by case.
Indigestion can be a symptom of another digestive disease. Sometimes digestive tract diseases such as peptic ulcer disease, gastritis, and stomach cancer cause chronic indigestion. However, most often doctors do not know what causes chronic indigestion. Chronic indigestion without a health problem or digestive tract disease that could explain symptoms is referred to as functional dyspepsia. Indigestion that isn’t caused by an underlying disease may be eased with lifestyle changes and medication.
Indigestion may be:
- occasional—happening once in a while
- chronic—happening regularly for a few weeks or months
- functional—having chronic symptoms without a specific cause
People with indigestion may have one or more of the following symptoms:
- Early fullness during a meal. You haven’t eaten much of your meal, but you already feel full and may not be able to finish eating.
- Uncomfortable fullness after a meal. Fullness lasts longer than it should.
- Discomfort in the upper abdomen. You feel a mild to severe pain in the area between the bottom of your breastbone and your navel.
- Burning in the upper abdomen. You feel an uncomfortable heat or burning sensation between the bottom of your breastbone and your navel.
- Bloating in the upper abdomen. You feel an uncomfortable sensation of tightness due to a buildup of gas.
- Burping
- Gurgling stomach and/or gas
- Acid reflux
- Heartburn
- Nausea. You feel as though you want to vomit.
Less frequent symptoms include vomiting and belching.
Sometimes people with indigestion also experience heartburn, but heartburn and indigestion are two separate conditions. Heartburn is a pain or burning feeling in the center of your chest that may radiate into your neck or back during or after eating.
Indigestion is a common condition, affecting about 1 in 4 people in the United States each year 3.
Of those people with indigestion who see a doctor, almost 3 in 4 are diagnosed with functional dyspepsia 4.
If you have indigestion see your doctor. This is especially important if any one of the following is true for you:
- You’re older than 50 years of age.
- You recently lost weight without trying to.
- You have trouble swallowing.
- You have severe vomiting.
- You have black, tarry bowel movements.
Mild indigestion can often be helped with lifestyle changes, including:
- Eating smaller, more-frequent meals. Chew your food slowly and thoroughly.
- You should eat a healthy, well-balanced diet. A healthy diet can improve your overall health, help manage certain diseases and conditions, and reduce the chance of disease.
- Avoiding triggers. Avoid certain foods and drinks that may cause indigestion or make your symptoms worse, such as:
- alcoholic beverages
- carbonated, or fizzy, drinks
- foods or drinks that contain caffeine
- foods that contain a lot of acid, such as tomatoes, tomato products, and oranges
- spicy, fatty, or greasy foods
- Smoking can trigger indigestion
- Maintaining a healthy weight. Excess pounds put pressure on your abdomen, pushing up your stomach and causing acid to back up into your esophagus.
- Exercising regularly. Exercise helps you keep off extra weight and promotes better digestion.
- Managing stress. Create a calm environment at mealtime. Practice relaxation techniques, such as deep breathing, meditation or yoga. Spend time doing things you enjoy. Get plenty of sleep.
- Changing your medications. With your doctor’s approval, stop or cut back on pain relievers or other medications that may irritate your stomach lining. If that’s not an option, be sure to take these medications with food.
What causes indigestion?
Indigestion has many possible causes. Often, indigestion is related to lifestyle and may be triggered by food, drink or medication. Common causes of indigestion include:
- Overeating or eating too quickly
- Eating certain foods that are hard to process, such as foods that are high in spice, fat, acid, and/or fiber
- Eating too late in the day
- Too much caffeine, alcohol, chocolate or carbonated beverages
- Smoking
- Anxiety
- Stress
- Depression
- Certain antibiotics, pain relievers, nonsteroidal anti-inflammatory drugs (NSAIDs) and iron supplements
Sometimes indigestion is caused by other digestive conditions, including:
- Acid reflux, gastroesophageal reflux (GER), or gastroesophageal reflux disease (GERD): A reaction to food and drink where contents come back up from your stomach. The acid can come up into your esophagus, the tube-like organ connecting your mouth and stomach. Acid reflux also can produce vomiting. This condition causes heartburn because of the high acid contents.
- Inflammation of the stomach (gastritis)
- Ulcer: A sore on the lining of your stomach (peptic ulcer), small intestine, or esophagus.
- Gastritis: Inflammation of your stomach lining
- Helicobacter pylori (H. pylori) infection
- Celiac disease
- Gallstones
- Gallbladder inflammation
- Constipation
- Lactose intolerance
- Pancreas inflammation (pancreatitis)
- Stomach cancer: This is a rare condition, but indigestion can be one of its signs.
- Intestinal blockage
- Irritable bowel syndrome (IBS): A disorder that affects your intestines. Symptoms include stomach pain, bloating, gas, constipation, and diarrhea.
- Infection: A bacterial infection from Helicobacter pylori (H. pylori) can cause indigestion.
- Gastroparesis: A condition that affects digestion. If muscles in your gastrointestinal tract stop working, your body slows down or stops the movement of food. Symptoms include nausea, vomiting, stomach pain, bloating, and acid reflux.
- Reduced blood flow in the intestine (intestinal ischemia)
Indigestion with no obvious cause is known as functional or nonulcer dyspepsia.
Researchers do not know what causes functional dyspepsia or nonulcer dyspepsia. Some research suggests that the following factors may play a role in functional dyspepsia 5:
- eating
- gastroparesis
- problems in the first part of your small intestine, including inflammation and being overly sensitive to stomach acids
- infection by microorganisms such as H. pylori, Salmonella, Escherichia coli (E. coli), Campylobacter, giardia or norovirus
- psychological problems, especially anxiety
- genes—a trait passed from parent to child.
When should I see a doctor for indigestion?
Mild indigestion is usually nothing to worry about. If you have indigestion and any of the following symptoms, you may have a more serious condition and should see a doctor right away:
- black, tarlike stools
- bloody vomit
- difficulty swallowing or painful swallowing that gets progressively worse
- frequent vomiting
- losing weight without trying
- pain in your chest, jaw, neck, or arm
- chest pain on exertion or with stress
- severe and constant pain in your abdomen
- shortness of breath
- sweating
- yellowing of your eyes or skin
- fatigue or weakness, which may indicate anemia
You should also see a doctor if your indigestion lasts longer than 2 weeks.
How is indigestion diagnosed?
To start, your doctor will review your symptoms and perform a physical exam. If there are warning signs in your history or during your exam, your doctor may order tests to determine the cause of indigestion. Those tests can include blood work, urine/stool tests, or an X-ray or ultrasound. Sometimes the doctor will perform an upper GI endoscopy to see inside your stomach. Your doctor will insert a thin tube with a camera on the end into your esophagus. A doctor may recommend an upper GI endoscopy for people with indigestion who are older than 55 or for people with indigestion of any age who have:
- a family history of cancer
- difficulty swallowing
- evidence of bleeding in the digestive tract
- frequent vomiting
- weight loss
But if your indigestion began suddenly, and you are experiencing severe symptoms or are older than age 55, your doctor may recommend:
- Laboratory tests, to check for anemia or metabolic disorders.
- Breath and stool tests, to check for Helicobacter pylori (H. pylori), the bacterium associated with peptic ulcers, which can cause indigestion. H. pylori testing is controversial because studies suggest limited benefit from treating the bacterium unless it is associated with a peptic ulcer.
- Endoscopy, to check for abnormalities in your upper digestive tract. A tissue sample (biopsy) may be taken for analysis.
- Imaging tests (X-ray or CT scan), to check for intestinal obstruction or another issue.
If initial testing fails to provide a cause, your doctor may diagnose functional dyspepsia.
Can indigestion be prevented or avoided?
There are ways to prevent indigestion. To start, you need to know your body and how it reacts to different food and drinks. Spicy and acidic foods and carbonated drinks can trigger indigestion. Try to avoid those things when possible. Eat smaller meals throughout the day, and don’t eat too late at night. Don’t lie down too soon after eating. Limit the use of alcohol. If you use tobacco, try to quit. Stress and lack of sleep also can worsen symptoms.
In addition to making changes in what you eat and drink, you can help prevent indigestion by making lifestyle changes such as:
- avoiding exercise right after eating
- chewing food carefully and completely
- losing weight
- not eating late-night snacks
- not taking a lot of nonsteroidal anti-inflammatory drugs (NSAIDs)
- quitting smoking
- trying to reduce stress in your life
- waiting 2 to 3 hours after eating before you lie down
What are the treatments for indigestion?
Your treatment will depend on what is causing your indigestion. The prevention methods for indigestion also are forms of treatment. These include changing your diet and the way you eat. Getting more sleep and reducing stress also help.
If you have a stomach ulcer, it can be cured. You may need to take an acid-blocking medicine. If you have an infection in your stomach, you may also need to take an antibiotic.
In addition, you can try to avoid or take certain over-the-counter medicines. Check with your doctor before starting something new.
- Pain and anti-inflammatory medicines, like Advil or Aleve, do not help with indigestion. They can worsen your condition, especially if used often.
- Antacids are meant to work against the acid in your system. Brands such as Tums or Alka-Seltzer can help reduce some symptoms of indigestion.
- Histamine blockers include Pepcid. These can help reduce pain and symptoms, but should not be used long-term.
- Proton pump inhibitors omeprazole and lansoprazole are now available over the counter. These medicines help block the site of acid production in your stomach.
You may need other treatment, based on the cause of your indigestion.
Doctor recommended treatments:
- Changing what you eat and drink
- Avoiding foods that trigger indigestion
- Eating five or six small meals a day instead of three large meals
- Reducing or eliminating the use of alcohol and caffeine
- Avoiding certain pain relievers, such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve)
- Finding alternatives for medications that trigger indigestion
- Controlling stress and anxiety
- Psychological therapies
If your indigestion persists, over-the-counter and prescription medicines may help. Over-the-counter antacids are generally the first choice.
Antacids. Doctors often first recommend antacids—over-the-counter medicines that neutralize acids in your stomach. Antacids include:
- calcium carbonate (Rolaids, Tums)
- loperamide (Imodium)
- simethicone (Maalox, Mylanta)
- sodium bicarbonate (Alka-Seltzer)
Other options include:
- Proton pump inhibitors (PPIs), which can reduce stomach acid. PPIs may be recommended if you experience heartburn along with indigestion.
- H-2-receptor antagonists (H2RAs), which can also reduce stomach acid.
- Prokinetics, which may be helpful if your stomach empties slowly.
- Antibiotics, if H. pylori bacteria are causing your indigestion.
- Antidepressants or anti-anxiety medications, which may ease the discomfort from indigestion by decreasing your sensation of pain.
You can buy many medicines to treat indigestion without a prescription, such as antacids, H2 blockers, or proton pump inhibitors. However, if your indigestion lasts longer than 2 weeks, you should see your doctor. Your doctor may prescribe acid-suppressing medicines that are stronger than the ones you can buy, antibiotics, prokinetics, or psychological medicines.
Antibiotics. To treat a Helicobacter pylori (H. pylori) infection, your doctor will prescribe antibiotics—medicines that kill bacteria. He or she will prescribe at least two of the following:
- amoxicillin (Amoxil)
- clarithromycin (Biaxin)
- metronidazole (Flagyl)
- tetracycline (Sumycin)
- tinidazole (Tindamax)
H2 blockers. H2 blockers are medicines that decrease the amount of acid your stomach produces. H2 blockers provide short-term or on-demand relief for many people with indigestion. You can buy an H2 blocker or your doctor can prescribe one. H2 blockers include:
- cimetidine (Tagamet HB)
- famotidine (Pepcid AC)
- nizatidine (Axid AR)
- ranitidine (Zantac 75)
Proton pump inhibitors (PPIs). PPIs are most effective in treating indigestion if you also have heartburn. You can buy some PPIs or your doctor can prescribe one. PPIs include:
- esomeprazole (Nexium)
- lansoprazole (Prevacid)
- omeprazole (Prilosec, Zegerid)
- pantoprazole (Protonix)
- rabeprazole (AcipHex)
Prokinetics. Prokinetics help your stomach empty faster. Prescription prokinetics include:
- bethanechol (Urecholine)
- metoclopramide (Reglan)
Psychological therapies
Your doctor may recommend a type of psychological therapy called “talk therapy” to help treat anxiety and depression that may be causing your indigestion. If stress is causing your indigestion, your doctor may recommend ways to help you reduce your stress, such as meditation, relaxation exercises or counseling. Talk therapy can also help you learn how to reduce your stress.
Alternative medicine
Alternative and complementary treatments may help ease indigestion, although none of these treatments has been well-studied. These treatments include:
- Herbal therapies such as peppermint and caraway.
- Psychological treatment, including behavior modification, relaxation techniques, cognitive behavioral therapy and hypnotherapy.
- Acupuncture, which may work by blocking the pathways of nerves that carry sensations of pain to the brain.
- Mindfulness meditation.
- STW 5 (Iberogast), a liquid supplement that contains extracts of herbs including bitter candytuft, peppermint leaves, caraway and licorice root. STW 5 may work by reducing the production of gastric acid.
Always check with your doctor before taking any supplements to be sure you’re taking a safe dose and that the supplement won’t adversely interact with any other medications you’re taking.
Best foods for stomach ulcers
An “ulcer” is an open sore. The word “peptic” means that the cause of the problem is due to acid. Most of the time when a gastroenterologist is referring to an “ulcer” the doctor means a peptic ulcer which is a sore or raw area in the lining of the stomach. The two most common types of peptic ulcer are called “gastric ulcers” and “duodenal ulcers” 6. These names refer to the location where the ulcer is found. Gastric ulcers are located in the stomach. Duodenal ulcers are found at the beginning of the small intestine known as the duodenum. A person may have both gastric and duodenal ulcers at the same time. Rarely, a peptic ulcer may develop just above your stomach in your esophagus. Doctors call this type of peptic ulcer an esophageal ulcer. The lining is damaged by the acids your body uses to digest food.
The most common symptom of peptic ulcer is a burning pain in your stomach. It usually lasts for a few minutes to a few hours. It comes and goes for days or weeks at a time. TStomach acid makes the pain worse, as does having an empty stomach. The pain can often be relieved by eating certain foods that buffer stomach acid or by taking an acid-reducing medication, but then it may come back. he burning typically occurs between meals and at night. Small ulcers may cause no symptoms. Many people with peptic ulcers don’t even have symptoms.
Other symptoms can include:
- A feeling of fullness
- Difficulty drinking as much liquid as usual
- Hunger or an empty feeling in your stomach after you eat
- Mild nausea
- Stomach pain that wakes you up at night
Less common symptoms include:
- Bloating
- Burping
- Poor appetite
- Dark blood in stools, or stools that are black or tarry
- Chest pain
- Trouble breathing
- Feeling faint
- Fatigue
- Weight loss
- Vomiting or vomiting blood — which may appear red or black
- Nausea or vomiting
- Unexplained weight loss
- Appetite changes
Peptic ulcer complications. Left untreated, peptic ulcers can result in:
- Bleeding (this occurs from a broken blood vessel in the small intestine). Internal bleeding can occur as slow blood loss that leads to anemia or as severe blood loss that may require hospitalization or a blood transfusion. Severe blood loss may cause black or bloody vomit or black or bloody stools.
- A hole (perforation) in your stomach wall. Peptic ulcers can eat a hole through (perforate) the wall of your stomach or small intestine, putting you at risk of serious infection of your abdominal cavity (peritonitis).
- A blockage or obstruction. Peptic ulcers can block passage of food through the digestive tract, causing you to become full easily, to vomit and to lose weight either through swelling from inflammation or through scarring.
- Peritonitis (infection).
- Gastric cancer. Studies have shown that people infected with H. pylori have an increased risk of gastric cancer.
The most common causes of peptic ulcers are infection with the bacterium Helicobacter pylori (H. pylori) and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin IB, others), aspirin and naproxen sodium (Aleve). Rare causes include cancerous and noncancerous tumors in the stomach, duodenum, or pancreas—known as Zollinger-Ellison syndrome (ZES).
Researchers have not found that diet and nutrition play an important role in causing or preventing peptic ulcers. Alcohol and smoking do contribute to ulcers and should be avoided. Stress and spicy foods do not cause peptic ulcers. However, they can make your symptoms worse. Before acid blocking drugs became available, milk was used to treat ulcers. However, milk is not an effective way to prevent or relieve a peptic ulcer.
What causes peptic ulcers?
Peptic ulcers occur when acid in the digestive tract eats away at the inner surface of the stomach or small intestine. The acid can create a painful open sore that may bleed. Your digestive tract is coated with a mucous layer that normally protects against acid. But if the amount of acid is increased or the amount of mucus is decreased, you could develop an ulcer.
- The main cause of peptic ulcers is the Helicobacter pylori (H. pylori) bacterial infection. Helicobacter pylori bacteria commonly live in the mucous layer that covers and protects tissues that line the stomach and small intestine. Often, the H. pylori bacterium causes no problems, but it can cause inflammation of the stomach’s inner layer, producing an ulcer. It’s not clear how H. pylori infection spreads. It may be transmitted from person to person by close contact, such as kissing. People may also contract H. pylori through food and water.
- Another common cause is long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). Nonsteroidal anti-inflammatory drugs (NSAIDs) can irritate or inflame the lining of your stomach and small intestine. NSAIDs medications include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, Anaprox DS, others), ketoprofen and others. They do not include acetaminophen (Tylenol, others).
- Other medications. Taking certain other medications along with NSAIDs, such as steroids, anticoagulants, low-dose aspirin, selective serotonin reuptake inhibitors (SSRIs), alendronate (Fosamax) and risedronate (Actonel), can greatly increase the chance of developing ulcers.
- In rare cases, peptic ulcers can be caused by cancerous and noncancerous tumors in the stomach, duodenum, or pancreas—known as Zollinger-Ellison syndrome. Zollinger-Ellison syndrome is a rare disorder that happens when one or more tumors form in your pancreas and duodenum. The tumors release large amounts of gastrin, a hormone that causes your stomach to produce large amounts of acid. The extra acid causes peptic ulcers to form in your duodenum and in the upper intestine. Doctors use medicines, surgery, and chemotherapy to treat Zollinger-Ellison syndrome.
Risk factors for developing peptic ulcers
In addition to having risks related to taking NSAIDs, you may have an increased risk of peptic ulcers if you:
- Smoke. Smoking may increase the risk of peptic ulcers in people who are infected with H. pylori.
- Drink alcohol. Alcohol can irritate and erode the mucous lining of your stomach, and it increases the amount of stomach acid that’s produced.
- Have untreated stress.
- Eat spicy foods.
Alone, these factors do not cause ulcers, but they can make ulcers worse and more difficult to heal.
When should I see a doctor for peptic ulcers?
See your doctor if you have the severe signs or symptoms such as:
- Vomiting or vomiting blood — which may appear red or black
- Dark blood in stools, or stools that are black or tarry
- Trouble breathing
- Feeling faint
- Nausea or vomiting
- Unexplained weight loss
- Appetite changes
Also see your doctor if over-the-counter antacids and acid blockers relieve your pain but the pain returns.
How is peptic ulcers diagnosed?
Your doctor will do a physical exam. They will ask you questions about your medical history. Tell your doctor if you take aspirin, ibuprofen, or naproxen frequently. Your doctor will look for stomach bloating. They will listen to sounds in your stomach with a stethoscope. Your doctor will tap your stomach to check for pain.
Your doctor may schedule a special procedure to look at your stomach. This is called an endoscopy. For this procedure, you’ll be given medicine to relax. The medicine may make you fall asleep. The doctor will insert a thin, flexible tube down your throat. A tiny camera on the end of the tube displays the lining of your stomach and duodenum. The doctor may take a sample of your stomach lining (a biopsy). This is done to test for H. pylori. Blood, breath, and stool sample testing can also be used to check for H. pylori.
Can peptic ulcers be prevented or avoided?
You may reduce your risk of peptic ulcer if you follow these strategies:
- Protect yourself from H. pylori infections. It’s not clear just how H. pylori spreads, but there’s some evidence that it could be transmitted from person to person or through food and water. You can take steps to protect yourself from infections, such as H. pylori, by frequently washing your hands with soap and water and by eating foods that have been cooked completely.
- Use caution with pain relievers. If you regularly use pain relievers that increase your risk of peptic ulcer, take steps to reduce your risk of stomach problems. For instance, take your medication with meals. Talk to your doctor if you take aspirin, ibuprofen, or naproxen regularly. Work with your doctor to find the lowest dose possible that still gives you pain relief. Avoid drinking alcohol when taking your medication, since the two can combine to increase your risk of stomach upset. If you need an NSAID, you may need to also take additional medications such as an antacid, a proton pump inhibitor, an acid blocker or cytoprotective agent. A class of NSAIDs called COX-2 inhibitors may be less likely to cause peptic ulcers, but may increase the risk of heart attack.
- Stress and spicy foods don’t cause ulcers. However, they can make them worse.
- Smoking and alcohol can cause a peptic ulcer. Men should limit alcohol to no more than 2 drinks per day. Women should have no more than 1 drink per day.
What are the treatments for peptic ulcers?
Treatment for peptic ulcers depends on the cause. Usually treatment will involve killing the H. pylori bacterium if present, eliminating or reducing use of NSAIDs if possible, and helping your ulcer to heal with medication. If you have H. pylori, your doctor will treat the infection with “triple therapy.” This is a combination of 2 antibiotics and bismuth subsalicylate (one brand name: Pepto-Bismol). H. pylori can be stubborn. Take all your medicine as prescribed.
- Antibiotic medications to kill H. pylori. If H. pylori is found in your digestive tract, your doctor may recommend a combination of antibiotics to kill the bacterium. These may include amoxicillin (Amoxil), clarithromycin (Biaxin), metronidazole (Flagyl), tinidazole (Tindamax), tetracycline and levofloxacin. The antibiotics used will be determined by where you live and current antibiotic resistance rates. You’ll likely need to take antibiotics for two weeks, as well as additional medications to reduce stomach acid, including a proton pump inhibitor and possibly bismuth subsalicylate (Pepto-Bismol). Medicines containing bismuth subsalicylate such as Pepto-Bismol, coat a peptic ulcer and protect it from stomach acid. Although bismuth subsalicylate can kill H. pylori, doctors sometimes prescribe it with antibiotics, not in place of antibiotics.
- An antacid may make the pain from a peptic ulcer go away temporarily, yet it will not kill H. pylori. If you receive treatment for an H. pylori-induced peptic ulcer, check with your doctor before taking antacids. Some of the antibiotics may not work as well if you take them with an antacid.
Your doctor may recommend medicines to neutralize your stomach acid. This will protect the lining in your stomach, too. These include:
- Proton pump inhibitors (PPIs). Proton pump inhibitors (PPIs) reduce stomach acid and protect the lining of your stomach and duodenum. Proton pump inhibitors (PPIs) include esomeprazole (Nexium), dexlansoprazole (Dexilant), lansoprazole (Prevacid), omeprazole (Prilosec, Zegerid), pantoprazole (Protonix) or rabeprazole (AcipHex). Long-term use of proton pump inhibitors, particularly at high doses, may increase your risk of hip, wrist and spine fracture. Ask your doctor whether a calcium supplement may reduce this risk.
- Histamine receptor blockers. Histamine receptor blockers work by blocking histamine, a chemical in your body that signals your stomach to produce acid. Histamine receptor blockers include cimetidine (Tagamet), famotidine (Pepcid), ranitidine (Zantac) or nizatidine (Axid)
- Cytoprotective agents. Protectants coat ulcers and protect them against acid and enzymes so that healing can occur. Protectants includes sucralfate (one brand name: Carafate). Tell your doctor if the medicines make you feel sick or dizzy or cause diarrhea or headaches. Your doctor can change your medicines.
If nonsteroidal anti-inflammatory drugs (NSAIDs) cause your ulcer, you may need to stop or reduce the amount you take. You may need to switch to another type of medicine for pain.
If you take NSAIDs for other conditions, such as arthritis, you should talk with your doctor about the benefits and risks of using NSAIDs. Your doctor may prescribe a medicine used to prevent NSAID-induced ulcers called Misoprosotol.
If you need NSAIDs, you can reduce the chance of a peptic ulcer returning by:
- taking the NSAID with a meal
- using the lowest effective dose possible
- quitting smoking
- avoiding alcohol.
How doctors treat an H.pylori-induced peptic ulcer
Doctors may prescribe triple therapy, quadruple therapy, or sequential therapy to treat an H. pylori-induced peptic ulcer.
- Triple therapy: For triple therapy, your doctor will prescribe that you take the following for 7 to 14 days:
- the antibiotic clarithromycin
- the antibiotic metronidazole or the antibiotic amoxicillin
- a proton pump inhibitor (PPI)
- Quadruple therapy: For quadruple therapy, your doctor will prescribe that you take the following for 14 days:
- a proton pump inhibitor (PPI)
- bismuth subsalicylate
- the antibiotics tetracycline and metronidazole
- Doctors prescribe quadruple therapy to treat patients who:
- can’t take amoxicillin because of an allergy to penicillin. Penicillin and amoxicillin are similar.
- have previously received a macrolide antibiotic, such as clarithromycin.
- are still infected with H. pylori after triple therapy treatment.
- Doctors prescribe quadruple therapy after the first treatment has failed. In the second round of treatment, the doctor may prescribe different antibiotics than those that he or she prescribed the first time.
- Doctors prescribe quadruple therapy to treat patients who:
- Sequential therapy: For sequential therapy, your doctor will prescribe that you take the following for 5 days:
- a proton pump inhibitor (PPI)
- amoxicillin
- Then the doctor will prescribe you the following for another 5 days:
- a proton pump inhibitor (PPI)
- clarithromycin
- the antibiotic tinidazole
Triple therapy, quadruple therapy, and sequential therapy may cause nausea and other side effects, including:
- an altered sense of taste
- darkened stools
- a darkened tongue
- diarrhea
- headaches
- temporary reddening of the skin when drinking alcohol
- vaginal yeast infections
Talk with your doctor about any side effects that bother you. He or she may prescribe you other medicines.
If an H. pylori infection caused your peptic ulcer, you should finish all of your antibiotics and take any other medicines your doctor prescribes. The infection and peptic ulcer will heal only if you take all medicines as your doctor prescribes.
When you have finished your medicines, your doctor may do another breath or stool test in 4 weeks or more to be sure the H. pylori infection is gone. Sometimes, H. pylori bacteria are still present, even after you have taken all the medicines correctly. If the infection is still present, your peptic ulcer could return or, rarely, stomach cancer could develop. Your doctor will prescribe different antibiotics to get rid of the infection and cure your peptic ulcer.
Treatment for peptic ulcers is often successful, leading to ulcer healing. But if your symptoms are severe or if they continue despite treatment, your doctor may recommend endoscopy to rule out other possible causes for your symptoms.
If an ulcer is detected during endoscopy, your doctor may recommend another endoscopy after your treatment to make sure your ulcer has healed. Ask your doctor whether you should undergo follow-up tests after your treatment.
Peptic ulcers that fail to heal
Peptic ulcers that don’t heal with treatment are called refractory ulcers. There are many reasons why an ulcer may fail to heal, including:
- Not taking medications according to directions
- The fact that some types of H. pylori are resistant to antibiotics
- Regular use of tobacco. Smoking may interfere with the protective lining of the stomach, making your stomach more susceptible to the development of an ulcer. Smoking also increases stomach acid.
- Excessive use of alcohol can irritate and erode the mucous lining in your stomach and intestines, causing inflammation and bleeding.
- Regular use of pain relievers — such as NSAIDs — that increase the risk of ulcers
Less often, refractory ulcers may be a result of:
- Extreme overproduction of stomach acid, such as occurs in Zollinger-Ellison syndrome
- An infection other than H. pylori
- Stomach cancer
- Other diseases that may cause ulcerlike sores in the stomach and small intestine, such as Crohn’s disease
Treatment for refractory ulcers generally involves eliminating factors that may interfere with healing, along with using different antibiotics.
If you have a serious complication from an ulcer, such as acute bleeding or a perforation, you may require surgery. However, surgery is needed far less often now than previously because of the many effective medications available.
Can a peptic ulcer come back?
Yes, a peptic ulcer can come back. If you smoke or take NSAIDs, peptic ulcers are more likely to come back. If you need to take an NSAID, your doctor may switch you to a different medicine or add medicines to help prevent a peptic ulcer. Peptic ulcer disease can return, even if you have been careful to reduce your risk.
Best foods for constipation
Constipation is a condition in which you may have:
- Fewer than three bowel movements a week. However, people can have different bowel movement patterns and only you know what’s normal for you.
- Stools that are hard, dry, or lumpy
- Stools that are difficult or painful to pass
- A feeling that not all stool has passed
More serious symptoms include:
- Constipation is new and unusual for you.
- You have been constipated for 3 weeks or more despite dietary changes to help.
- You have abdominal (stomach) pain.
- You lose weight without trying.
- You notice blood or white mucous in your stool.
- You cannot pass the stool on your own.
Constipation is not a disease, but may be a symptom of another medical problem. Constipation may last for a short or long time. The most common causes of constipation include a change in routine, not enough fiber in your daily diet, not enough fluids and lack of exercise. Most cases of constipation are successfully treated by eating a diet high in fiber, drinking more fluids and exercising daily. Over-the-counter laxatives are fine in the short term, but seek advice if the problem persists.
Complications of chronic constipation include:
- Anal fissure (a tear in the skin around your anus).
- Fecal impaction (when your stool becomes too large to pass on your own).
- Hemorrhoids.
- Rectal prolapse (when a small piece of your intestine comes out of your anus from straining to have a bowel movement).
- Encopresis (when your bowels are so backed up that only liquid can pass through). Many people mistake this for diarrhea take anti-diarrheal medicine, making constipation even worse.
Complications of constipation can become serious if left untreated. You may require surgery.
Constipation is common among all ages and populations in the United States. About 16 out of 100 adults have symptoms of constipation. About 33 out of 100 adults ages 60 and older have symptoms of constipation 7.
Certain people are more likely to become constipated, including 8:
- women, especially during pregnancy or after giving birth
- older adults
- non-Caucasians
- people who eat little to no fiber
- people who take certain medicines or dietary supplements
- people with certain health problems, including functional gastrointestinal disorders
Treatment for constipation
Most cases of constipation are easy to treat at home with diet and exercise. Some cases require doctor recommendations, prescription medicine, or a medical procedure.
- Eating a healthy diet with fiber and drinking plenty of fluids (water is the most helpful) can usually clear up constipation. Changing what you eat and drink may make your stools softer and easier to pass. To help relieve your symptoms:
- Eat more high-fiber foods
- Drink plenty of water and other liquids if you eat more fiber or take a fiber supplement
Fiber
Dietary fiber is found mainly in plant-based foods including fruits, vegetables, wholegrains and legumes — is probably best known for its ability to prevent or relieve constipation. Dietary fiber also known as roughage or bulk, includes the parts of plant foods your body can’t digest or absorb. Unlike other food components, such as fats, proteins or carbohydrates — which your body breaks down and absorbs — fiber isn’t digested by your body. Instead, it is completely or partially broken down (fermented) by bacteria in your large intestine. Once broken down in your large intestine, it has been suggested that dietary fibers increase the good bacteria in your gut. This improves your immune system and supports your immunity against inflammatory disorders and allergies. Furthermore, a high fiber diet can provide other health benefits as well, such as helping you to maintain a healthy weight and lowering your risk of type 2 diabetes, heart disease and some types of cancer including bowel cancer. For example, high quality randomized controlled trials have shown that eating oat bran leads to lower blood pressure and lower total cholesterol.
Eating a range of dietary fiber can:
- Improve the diversity of your microbiota
- Improve constipation and lactose intolerance
- Enhance immunity
- Reduce inflammation in your gut
Benefits of a high-fiber diet:
- Normalizes bowel movements. Dietary fiber increases the weight and size of your stool and softens it. A bulky stool is easier to pass, decreasing your chance of constipation. If you have loose, watery stools, fiber may help to solidify the stool because it absorbs water and adds bulk to stool.
- Helps maintain bowel health. A high-fiber diet may lower your risk of developing hemorrhoids and small pouches in your colon (diverticular disease). Studies have also found that a high-fiber diet likely lowers the risk of colorectal cancer. Some fiber is fermented in the colon. Researchers are looking at how this may play a role in preventing diseases of the colon.
- Lowers cholesterol levels. Soluble fiber found in beans, oats, flaxseed and oat bran may help lower total blood cholesterol levels by lowering low-density lipoprotein, or “bad,” cholesterol levels. Studies also have shown that high-fiber foods may have other heart-health benefits, such as reducing blood pressure and inflammation.
- Helps control blood sugar levels. In people with diabetes, fiber — particularly soluble fiber — can slow the absorption of sugar and help improve blood sugar levels. A healthy diet that includes insoluble fiber may also reduce the risk of developing type 2 diabetes.
- Aids in achieving healthy weight. High-fiber foods tend to be more filling than low-fiber foods, so you’re likely to eat less and stay satisfied longer. And high-fiber foods tend to take longer to eat and to be less “energy dense,” which means they have fewer calories for the same volume of food.
- Helps you live longer. Studies suggest that increasing your dietary fiber intake — especially cereal fiber — is associated with a reduced risk of dying from cardiovascular disease and all cancers.
Fiber includes carbohydrates called polysaccharides and resistant oligosaccharides. Recent research suggests that fiber should be categorized by its physical characteristics; how well it dissolves (solubility), how thick it is (viscosity) and how well it breaks down (fermentability). Some commonly known terms are described below:
- Soluble fiber including pectins and beta glucans is found in foods like oats, peas, beans, apples, citrus fruits, carrots, barley and psyllium. Soluble fiber dissolves in water to form a gel-like material. It can help lower blood cholesterol and glucose levels. Foods high in soluble fiber can help you feel full. They also help reduce constipation by speeding up the time it takes for feces (poop) to pass through your body.
- Insoluble fiber including cellulose is found in wheat bran and nuts. Insoluble fiber is a type of fibre that doesn’t dissolve in water. Because insoluble fiber absorbs water, it helps to soften the contents of your bowel, contributing to keep the bowels regular. Insoluble fiber promotes the movement of material through your digestive system and increases stool bulk, so it can be of benefit to those who struggle with constipation or irregular stools. Whole-wheat flour, wheat bran, nuts, beans and vegetables, such as cauliflower, green beans and potatoes, are good sources of insoluble fiber.
- Resistant starch is a soluble fiber that is highly fermentable in the gut. It gets broken down by good bacteria to produce short chain fatty acids (SCFAs). Resistant starch is naturally present in some foods such as bananas, potatoes, grains and pulses. Freekeh, a Middle Eastern grain available in some supermarkets, is another good source. In general, foods that are less highly processed contain more resistant starch. Different ways of cooking can create different amounts of resistant starch. For example, resistant starch is found in slightly undercooked (‘al dente’) pasta, cooked but cooled potatoes (including potato salad), under-ripe bananas, beans, lentils and a product called Hi-maize used in some breads and breakfast cereals.
- Prebiotics are types of carbohydrate that only our gut bacteria can feed upon. Some examples are onions, garlic, asparagus and banana
The amount of soluble and insoluble fiber varies in different plant foods. To receive the greatest health benefit, eat a wide variety of high-fiber foods.
Good sources of dietary fiber include:
- Pulses (like lentils and peas) and beans and legumes (think navy beans, small white beans, split peas, chickpeas, lentils, pinto beans)
- Fruits and vegetables, vegetables such as carrots, broccoli, green peas, and collard greens; fruits especially those with edible skin (like pears and apples with the skin on) and those with edible seeds (like berries)
- Nuts—try different kinds (pumpkin seeds, almonds, sunflower seeds, pistachios and peanuts are a good source of fiber and healthy fats, but be mindful of portion sizes, because they also contain a lot of calories in a small amount!)
- Whole grains such as:
- Quinoa, barley, bulgur, oats, brown rice and farro
- Whole wheat pasta
- Whole grain cereals, including those made from whole wheat, wheat bran and oats
Choose fiber rich foods from a variety of sources including wholegrains, fruit and vegetable, nuts and seeds, beans and pulses. When you read food labels check for the grams of fiber per serving or per 100g. Foods that are naturally high in fiber and contain at least 3 grams per 100 gram are often labeled as a “good source,” and foods labeled as “excellent source” contain more than 5 grams of fiber per serving.
Here’s a look at how much dietary fiber is found in some common foods. When buying packaged foods, check the Nutrition Facts label for fiber content. It can vary among brands.
Table 1. Fruits dietary fiber content
| Fruits | Serving size | Total fiber (grams)* |
| Raspberries | 1 cup | 8 |
| Pear | 1 medium | 5.5 |
| Apple, with skin | 1 medium | 4.5 |
| Banana | 1 medium | 3 |
| Orange | 1 medium | 3 |
| Strawberries | 1 cup | 3 |
Table 2. Vegetables dietary fiber content
| Vegetables | Serving size | Total fiber (grams)* |
| Green peas, boiled | 1 cup | 9 |
| Broccoli, boiled | 1 cup chopped | 5 |
| Turnip greens, boiled | 1 cup | 5 |
| Brussels sprouts, boiled | 1 cup | 4 |
| Potato, with skin, baked | 1 medium | 4 |
| Sweet corn, boiled | 1 cup | 3.5 |
| Cauliflower, raw | 1 cup chopped | 2 |
| Carrot, raw | 1 medium | 1.5 |
Table 3. Grains dietary fiber content
| Grains | Serving size | Total fiber (grams)* |
| Spaghetti, whole-wheat, cooked | 1 cup | 6 |
| Barley, pearled, cooked | 1 cup | 6 |
| Bran flakes | 3/4 cup | 5.5 |
| Quinoa, cooked | 1 cup | 5 |
| Oat bran muffin | 1 medium | 5 |
| Oatmeal, instant, cooked | 1 cup | 5 |
| Popcorn, air-popped | 3 cups | 3.5 |
| Brown rice, cooked | 1 cup | 3.5 |
| Bread, whole-wheat | 1 slice | 2 |
| Bread, rye | 1 slice | 2 |
Table 4. Legumes, nuts and seeds dietary fiber content
| Legumes, nuts and seeds | Serving size | Total fiber (grams)* |
| Split peas, boiled | 1 cup | 16 |
| Lentils, boiled | 1 cup | 15.5 |
| Black beans, boiled | 1 cup | 15 |
| Baked beans, canned | 1 cup | 10 |
| Chia seeds | 1 ounce | 10 |
| Almonds | 1 ounce (23 nuts) | 3.5 |
| Pistachios | 1 ounce (49 nuts) | 3 |
| Sunflower kernels | 1 ounce | 3 |
Footnote: *Rounded to nearest 0.5 gram
Depending on your age and sex, adults should get 25 to 31 grams of fiber a day 9. Older adults sometimes don’t get enough fiber because they may lose interest in food.
- Men over the age of 50 should get at least 38 grams of fiber per day.
- Women over the age of 50 should get 25 grams per day.
- Children ages 1 to 3 should get 19 grams of fiber per day.
- Children between 4 and 8 years old should get 25 grams per day.
- Girls between 9 and 18 should get 26 grams of fiber each day. Boys of the same age range should get between 31 and 38 grams of fiber per day.
Tips for fitting in more fiber
- For breakfast choose a high-fiber breakfast cereal — 5 or more grams of fiber a serving. Opt for cereals with “whole grain,” “bran” or “fiber” in the name. Or add a few tablespoons of unprocessed wheat bran to your favorite cereal.
- Switch to whole grains. Consume at least half of all grains as whole grains. Look for breads that list whole wheat, whole-wheat flour or another whole grain as the first ingredient on the label and have at least 2 grams of dietary fiber a serving. Experiment with brown rice, wild rice, barley, whole-wheat pasta and bulgur wheat.
- Bulk up baked goods. Substitute whole-grain flour for half or all of the white flour when baking. Try adding crushed bran cereal, unprocessed wheat bran or uncooked oatmeal to muffins, cakes and cookies.
- Lean on legumes. Beans, peas and lentils are excellent sources of fiber. Add kidney beans to canned soup or a green salad. Or make nachos with refried black beans, lots of fresh veggies, whole-wheat tortilla chips and salsa.
- Eat more fruit and vegetables. Fruits and vegetables are rich in fiber, as well as vitamins and minerals. Try to eat five or more servings daily.
- Make snacks count. Fresh fruits, raw vegetables, low-fat popcorn and whole-grain crackers are all good choices. A handful of nuts or dried fruits also is a healthy, high-fiber snack — although be aware that nuts and dried fruits are high in calories.
Keep in mind that if you haven’t been eating a lot of foods high in fiber on a daily basis, it’s important to increase your intake slowly to allow your body to adjust. A sudden increase in eating foods high in fiber (especially foods with added fiber or when using supplements) can cause gas, bloating or constipation. Be sure you are drinking enough water too, because fiber needs water to move through your body, making your stool soft and bulky.
You may wish to see a dietitian if you:
- are unsure about how much and/or what types of fiber you currently have in your diet
- suffer with constipation or diarrhea (e.g. irritable bowel syndrome [IBS])
- have a condition which can restrict your fiber intake (e.g. inflammatory bowel disease)
Water
You should drink water and other liquids, such as naturally sweetened fruit and vegetable juices and clear soups, to help the fiber work better. This change should make your stools softer and easier to pass.
Drinking enough water and other liquids is also a good way to avoid dehydration. Staying hydrated is good for your overall health and can help you avoid getting constipated. Ask a health care professional how much liquid you should drink each day based on your size, health, activity level, and where you live.
What causes constipation?
You may be constipated for many reasons and constipation may have more than one cause at a time. Constipation can be caused by your diet (too many processed foods and not enough fiber), certain medicines (opioid medicines given for pain and even too many laxatives, which usually help you have a bowel movement), dehydration (especially not enough water), too little physical activity, intestinal problems, and major life changes, such as pregnancy. Constipation becomes more common as you age. Certain diseases and disabilities also can cause constipation. These include multiple sclerosis, stroke, diabetes, hypothyroidism, and lupus.
Dehydration (not enough fluids) and dietary changes are the most common causes of constipation in babies. For example, changing from breast milk to cow’s milk or from baby food to solids can cause constipation.
Causes of constipation may include:
- slow movement of stool through your large intestine (colon)
- delayed emptying of the colon from pelvic floor disorders, especially in women, and colon surgery
- functional gastrointestinal disorders, such as irritable bowel syndrome
Certain medicines and dietary supplements
Medicines and dietary supplements that can make constipation worse include:
- antacids that contain aluminum and calcium
- anticholinergics and antispasmodics
- anticonvulsants—used to prevent seizures
- calcium channel blockers
- diuretics
- iron supplements
- medicines used to treat Parkinson’s disease
- narcotic pain medicines
- some medicines used to treat depression
Life changes or daily routine changes
Constipation can happen when your life or daily routine changes. For example, your bowel movements can change:
- if you become pregnant
- as you get older
- when you travel
- when you ignore the urge to have a bowel movement
- if you change your medicines
- if you change how much and what you eat
Certain health and nutrition problems
Certain health and nutrition problems can cause constipation:
- not eating enough fiber
- not drinking enough liquids, or dehydration
- not getting enough physical activity External link
- Celiac disease
- disorders that affect your brain and spine, such as Parkinson’s disease
- spinal cord or brain injuries
- conditions that affect your metabolism, such as diabetes
- conditions that affect your hormones, such as hypothyroidism
- inflammation linked to diverticular disease or proctitis
- intestinal obstructions, including anorectal blockage and tumors
- anatomic problems of your digestive tract
When should I see a doctor for constipation?
You should see a doctor if your symptoms do not go away with self-care or you have a family history of colon or rectal cancer.
You should see a doctor right away if you have constipation and any of the following symptoms:
- bleeding from your anus or rectum
- blood in your stool
- constant pain in your abdomen
- inability to pass gas
- vomiting
- fever
- lower back pain
- losing weight without trying.
How is constipation diagnosed?
Your doctor will ask you about your symptoms and medical history. This will include asking you about any medicines you take. Your doctor also will ask when you had your last bowel movement and how often you have them. Think about that before you see your doctor. It might be helpful to write it down for yourself or a child before your appointment. During the visit, your doctor may examine your rectum (the end of your large intestine near your anus). The doctor will insert his or her finger (while wearing rubber gloves) into your rectum to feel for blockages.
Your doctor may order additional tests, including a blood test and X-ray. A more thorough test is a colonoscopy. This is an invasive procedure done with anesthesia. During this test, your doctor will examine your colon with a long, flexible scope attached to a camera.
Can constipation be prevented or avoided?
There are things you can do to reduce constipation. These include:
- Add more fiber to your diet. Adults should eat between 20-35 grams of fiber each day. Foods, such as beans, whole grains, fruits, and vegetables are high in fiber.
- Drink more water. Being dehydrated causes your stool to dry out. This makes having a bowel movement more difficult and painful.
- Don’t wait. When you have the urge to have a bowel movement, don’t hold it in. This causes the stool to build up.
- Get active. Exercise is helpful in keeping your bowel movements regular.
- Beware of medicines. Certain prescription medicines (especially pain medicines) can slow your digestive system. This causes constipation. Talk to your doctor about how to prepare for this if you need these medicines.
- Talk to your doctor if you are being treated for certain diseases that are related to constipation. He or she may have additional guidance for lowering your risks.
Avoid eating
To help prevent or relieve constipation, avoid foods with little to no fiber, such as:
- chips
- fast food
- meat
- prepared foods, such as some frozen meals and snack foods
- processed foods, such as hot dogs or some microwavable dinners.
Fiber supplements and fortified foods
Whole foods rather than fiber supplements are generally better. Fiber supplements — such as Metamucil, Citrucel and FiberCon — don’t provide the variety of fibers, vitamins, minerals and other beneficial nutrients that foods do.
Another way to get more fiber is to eat foods, such as cereal, granola bars, yogurt and ice cream, with fiber added. The added fiber usually is labeled as “inulin” or “chicory root.” Some people complain of gassiness after eating foods with added fiber.
However, some people may still need a fiber supplement if dietary changes aren’t sufficient or if they have certain medical conditions, such as constipation, diarrhea or irritable bowel syndrome. Check with your doctor before taking fiber supplements.
What are the treatments for constipation?
At home treatment includes:
- Bowel training: Teach your children to go to the bathroom when they have to. Holding it can lead to constipation. This also may be necessary for your elderly parents, if you are caring for them.
- Laxatives: This is over-the-counter medicine that helps you have a bowel movement. Laxatives should only be used in rare instances. Do not use them on a regular basis. If you have to use a laxative, bulk-forming laxatives are best (two brands: Metamucil and Benefiber). These work naturally to add bulk and water to your stools so they can pass easily. Bulk-forming laxatives can cause some bloating (when your stomach feels full) and gas.
Doctor recommended treatments:
When stool is impacted, tap water enemas are commonly used. Usually people are positioned on their left side, with knees flexed. About 5 to 10 ounces of water, at body temperature, are gently instilled into the rectum and sigmoid colon. When the water is emptied, the impacted stool is passed with it. Non-prescription prepackaged enemas can be used in place of tap water. If enemas fail to work, a health care practitioner may need to remove the stool manually using a gloved finger. The person is then sometimes asked to drink a solution containing dissolved salts and polyethylene glycol, which cleanses the digestive tract.
After the impaction has been removed, the person may be told to add fiber to the diet or to use laxatives to prevent constipation. Laxatives may be used every two to three days if a bowel movement does not occur naturally.
If the stool is not impacted, several options are available for treating constipation. Increasing the intake of fluids and fiber is often the first step. Vegetables, fruit (especially prunes), whole-grain breads, and high-fiber cereals are excellent sources of fiber. Bran is an alternative source, although it may cause excessive gas and bloating. To work well, fiber should be consumed with plenty of fluids.
Laxatives and stool softeners are sometimes needed if changes in diet are insufficient. Most laxatives are safe for long-term uses, if used appropriately.
Bulking agents, such as psyllium and methylcellulose, are laxatives that help hold water in the stool and add bulk to it. The increased bulk stimulates the natural contractions of the large intestine. Bulkier stools are softer and easier to pass. Bulking agents act slowly and gently. These agents generally are taken in small amounts at first. The dose is increased gradually until regularity is achieved.
Osmotic agents are laxatives that keep large amounts of water in the large intestine, making the stool soft and loose. These laxatives consist of salts or sugars that are poorly absorbed. Some contain magnesium and phosphate, which can be partially absorbed resulting in harm to people with kidney failure.
Stimulant laxatives contain substances that directly stimulate the walls of the large intestine (such as senna and bisacodyl), causing them to contract. Taken by mouth, stimulant laxatives generally cause a bowel movement in six to eight hours. Some are available as suppositories. When taken as suppositories, these laxatives often work in 15 to 60 minutes. Stimulant laxatives are best used for brief periods. If longer use is needed, they may be used daily or every other day, and optimally under a doctor’s supervision.
Newer medications, which increase secretion of fluids into the intestine, are available only by prescription. They should be considered if constipation does not respond well to over-the-counter laxatives. When constipation is due to opiate drugs used to treat severe pain, new agents that block the effects of opiates on the gut sometimes can help. Occasionally, a problem with coordination of pelvic floor and anorectal muscles may be identified. This can be treated with biofeedback or muscle retraining exercises; such treatments are performed only in centers which specialize in this area and upon referral by a doctor.
- Constipation and Defecation Problems. https://gi.org/topics/constipation-and-defection-problems/[↩]
- Dyspepsia. https://gi.org/topics/dyspepsia[↩]
- Longstreth GF, Lacy BE. Approach to the adult with dyspepsia. https://www.uptodate.com/contents/approach-to-the-adult-with-dyspepsia[↩]
- Talley NJ, Ford AC. Functional dyspepsia. The New England Journal of Medicine. 2015;373(19):1853–1863.[↩]
- Talley NJ. Functional dyspepsia: new insights into pathogenesis and therapy. The Korean Journal of Internal Medicine. 2016:31(3):444–456.[↩]
- Peptic Ulcer Disease. https://gi.org/topics/peptic-ulcer-disease[↩]
- American Gastroenterological Association, Bharucha AE, Dorn SD, Lembo A, Pressman A. American Gastroenterological Association medical position statement on constipation. Gastroenterology. 2013;144(1):211–217.[↩]
- Rose S, ed. Constipation: A Practical Approach to Diagnosis and Treatment. New York, NY: Springer Science and Business Media; 2014.[↩]
- U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2015-2020. https://health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf[↩]