Bethlem myopathy
Bethlem myopathy is a rare genetic disease affecting the skeletal muscles and connective tissue. Bethlem myopathy is a sub-type (milder form) of collagen VI-related myopathy 1. Bethlem myopathy is characterized by slowly progressive proximal muscle weakness and joint stiffness (contractures). Proximal muscles are the muscles that are closest to the center of the body such as the muscles of the shoulder, pelvis, and upper arms and legs. Muscle weakness may eventually affect the distal muscles to a lesser degree. Distal muscles are those farther from the center of the body and include the muscles of the lower arms and legs and the hands and feet. Bethlem myopathy most often affects the fingers, wrists, elbows, and ankles 1. Signs and symptoms may begin before birth with decreased fetal movements; shortly after birth with low muscle tone (hypotonia) or torticollis; in early childhood with delayed motor skills, muscle weakness, and contractures or in adulthood with weakness, Achilles tendon, or finger contractures. In some adults, noticeable muscle weakness may not occur until after 40 years of age. Due to the disease’s progression, most people with Bethlem myopathy over age 50 require mobility aids (such as a cane, crutches, or wheelchair) for outdoor mobility. Rarely, severe muscle weakness may lead to respiratory difficulties in later life due to weakness of the diaphragm muscles 2. Heart (cardiac) function, which may become impaired in other forms of myopathy, is usually unaffected in individuals with Bethlem myopathy.
In some cases, a skin condition may occur that is characterized by thickening and hardening (hyperkeratosis) of hair follicles, resulting in the development of rough, elevated growths (papules) on the skin.
Bethlem myopathy is caused by mutations (changes) in the COL6A1, COL6A2, or COL6A3 genes. Most cases are inherited in an autosomal dominant manner, but in rare cases the disease is autosomal recessive 2. The diagnosis is based on clinical examination and laboratory tests, but genetic testing may confirm the diagnosis 2. Treatment depends on individual symptoms but routinely involves physical therapy. Surgery to correct joint contractures may be needed 2.
Collagen VI myopathy
Collagen type VI-related disorders encompass two genetic muscle disorders formerly thought to be separate entities: Bethlem myopathy and Ullrich congenital muscular dystrophy. Researchers have determined that collagen type VI-related disorders represent a disease spectrum associated with disruptions or changes (mutations) in genes that contain instructions to produce (encode) collagen type VI proteins 3. Bethlem myopathy represents the milder form of this spectrum and Ullrich congenital muscular dystrophy represents the severe end. Common symptoms include progressive muscle weakness and degeneration (atrophy) and abnormally fixed joints that occur when thickening and shortening of tissue such as muscle fibers and tendons cause deformity and restrict the movement of an affected area (contractures). Both Bethlem myopathy and Ullrich congenital muscular dystrophy can be inherited as autosomal dominant or autosomal recessive traits.
Ullrich congenital muscular dystrophy is characterized by diminished muscle tone (hypotonia), weakness and degeneration of the proximal muscles, and abnormally flexible (hyperelastic) joints of the wrists and ankles. Additional early symptoms of Ullrich congenital muscular dystrophy include the failure to gain weight and grow at the expected rate (failure to thrive), abnormal front-to-back and side-to-side curvature of the spine (kyphoscoliosis), a twisted or tilted neck (torticollis), congenital dislocation of the hip, contractures of the joints, and stiffness (rigidity) of the spine.
Intelligence is normal in most cases. The amount of motor development varies from case to case. Some children are able to walk independently; others require assistance to walk. In some cases, affected children may never be able to walk. In addition, some children who develop the ability to walk independently lose that ability because of the progression of the disease (e.g., worsening contractures, rigidity of spine).
Additional symptoms may occur including breathing (respiratory) difficulties and frequent chest infections. Breathing difficulties can result in life-threatening complications and may require respiratory support, especially at night.
As the disorder progress, previously flexible (lax) joints such as those of the wrists and ankles may stiffen. Some affected individuals may exhibit a skin condition characterized by thickening and hardening (hyperkeratosis) of hair follicles, resulting in the development of rough, elevated growths (papules). In some cases, scars may heal slowly or affected individuals may develop hardened, raised bumps at the site of an injury (hypertrophic keloid scars).
Some individuals with Ullrich congenital muscular dystrophy may have a distinctive facial appearance with a rounded face with prominent ears.
Bethlem myopathy cause
Bethlem myopathy is caused by mutations (changes) in the COL6A1, COL6A2, or COL6A3 genes. These genes each provide instructions for making one component of a protein called type VI collagen. This protein plays an important role in the muscles, particularly skeletal muscles. Type VI collagen makes up part of the extracellular matrix, an intricate lattice that forms in the space between cells and provides structural support to the muscles 1.
Mutations in the type VI collagen genes result in the formation of abnormal type VI collagen or reduced amounts of type VI collagen. This decrease in amounts of normal type VI collagen disrupts the extracellular matrix surrounding muscle cells, which leads to the progressive muscle weakness and other signs and symptoms of Bethlem myopathy 1.
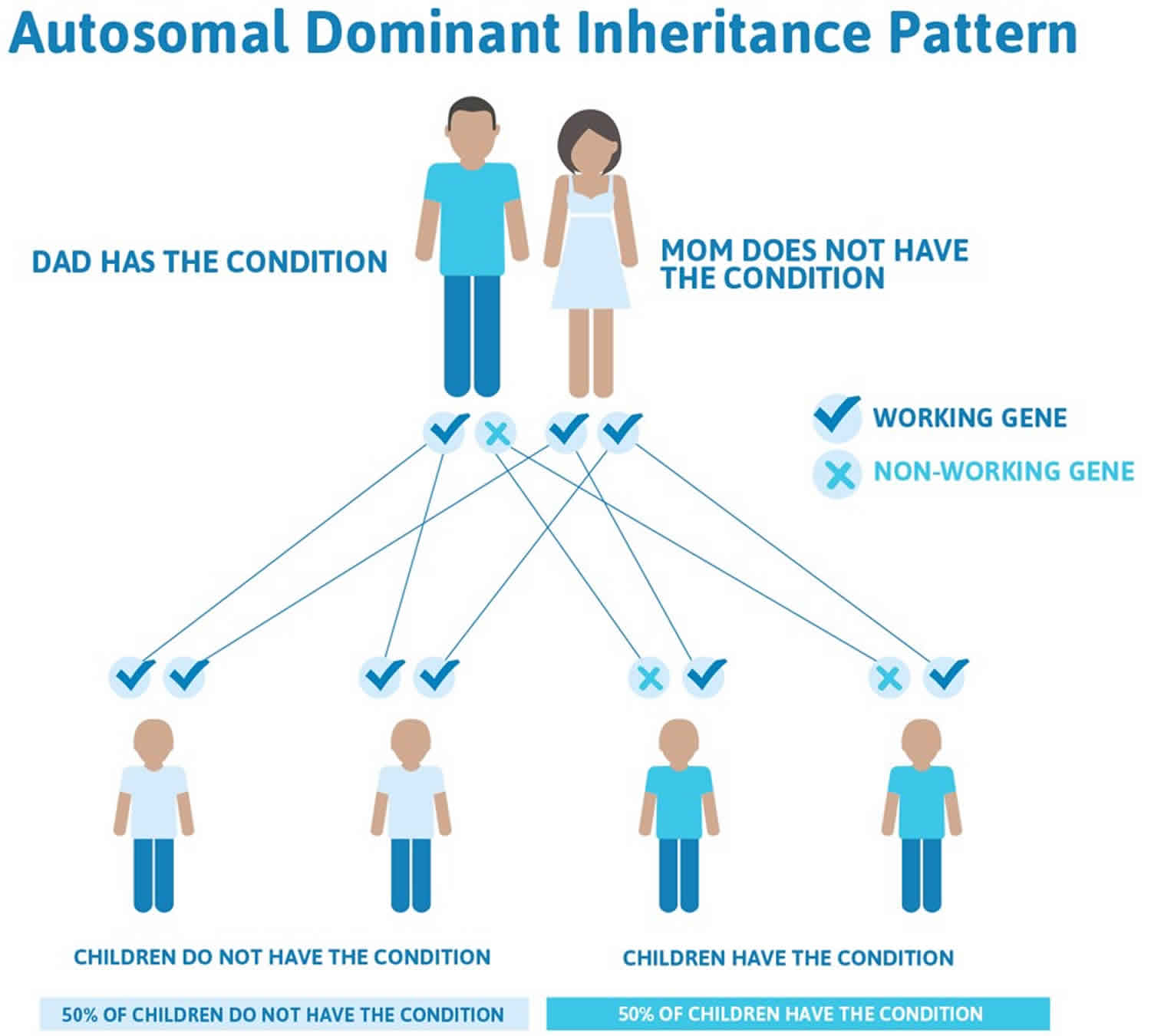
Bethlem myopathy inheritance pattern
Bethlem myopathy is typically inherited in an autosomal dominant manner, meaning one copy of the altered gene in each cell is sufficient to cause the disease. You inherit one copy of each of our genes from our mother and the other from our father. Many cases of Bethlem myopathy result from new (de novo) mutations in the gene, meaning the mutations were not inherited from either parent. When people who have a new mutation in a gene causing Bethlem myopathy go on to have children, each of their children will have a 50% chance of inheriting the disease.
In some cases, a person who has Bethlem myopathy inherited the mutation from one affected parent. In these cases, future children of this parent will also have a 50% chance to inherit the disease. The parent who has the disease may be so mildly affected that they didn’t know they were showing symptoms of the disease at all.
In rare cases, Bethlem myopathy is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive disease each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the disease 1. These individuals are known as carriers. When two carriers of a gene mutation causing Bethlem myopathy have children, for each child there is a:
- 25% chance that the child will have Bethlem myopathy
- 50% chance that the child will be a carrier of Bethlem myopathy like the parents
- 25% chance that the child will have two working copies of the gene that makes type VI collagen, so the child will not have Bethlem myopathy and will not be a carrier.
Figure 1. Bethlem myopathy autosomal dominant inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
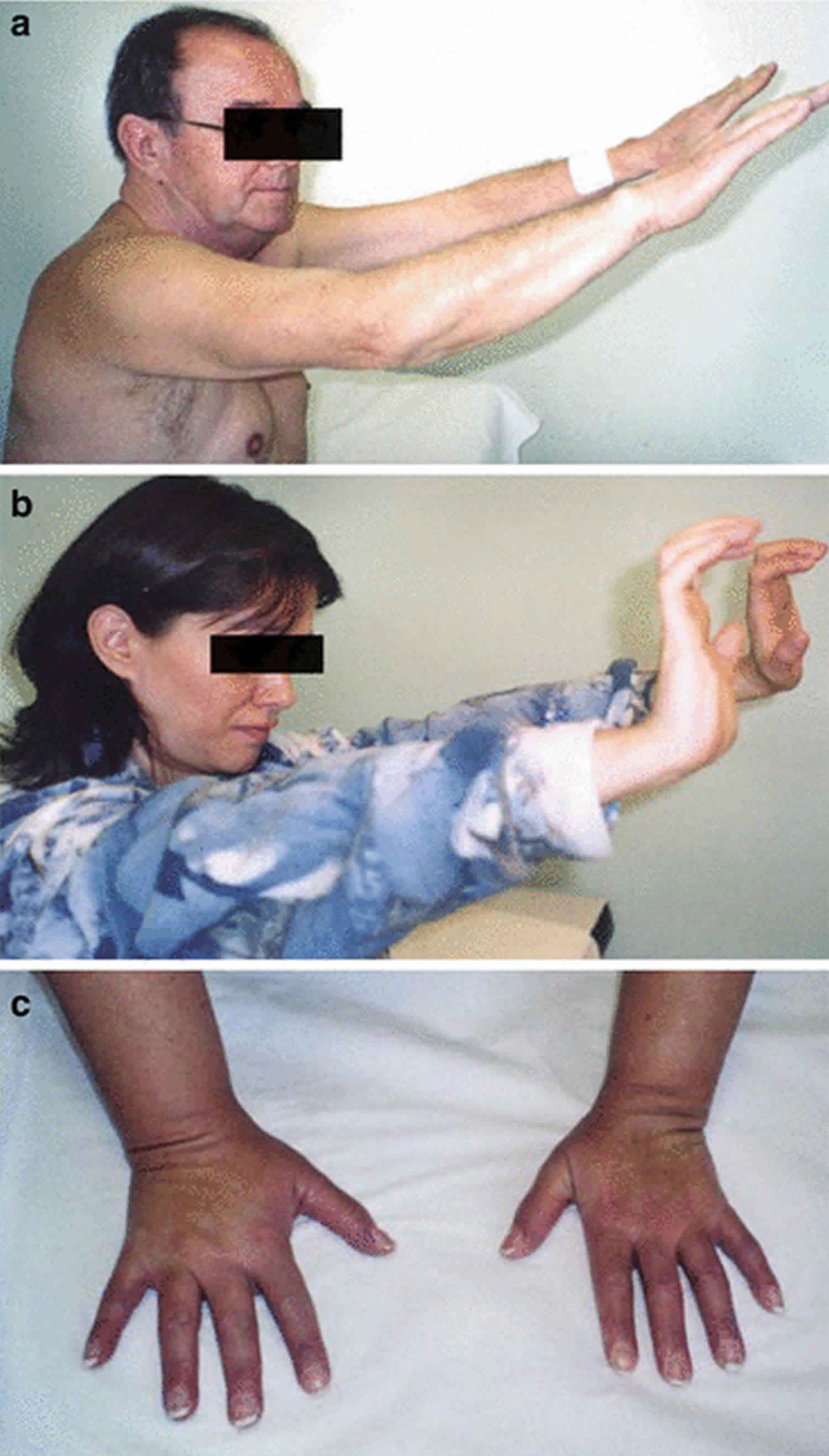
Bethlem myopathy symptoms
Bethlem myopathy mainly affects skeletal muscles, which are the muscles used for movement. People with this disease experience progressive muscle weakness and joint stiffness (contractures) in their fingers, wrists, elbows, and ankles. The features of Bethlem myopathy can appear at any age. In some cases, the symptoms start before birth with decreased fetal movements. In others, low muscle tone (hypotonia) and a stiff neck (torticollis) develop during infancy. During childhood, developmental delay may be noted. For example a baby with Bethlem myopahy may learn to sit by themselves or walk later than usual. In some, symptoms don’t occur until adulthood, when a person may notice muscle weakness. By the age of 50-years-old, approximately two-thirds (66%) of people with Bethlem myopathy will need to use a walker, cane, or wheelchair 2.
Bethlem myopathy is recognized clinically by the combination of the following 4:
- Proximal muscle weakness
- Variable contractures, affecting most frequently the long finger flexors, elbows, and ankles
In addition to the muscle problems, some people with Bethlem myopathy have skin abnormalities. These abnormalities may include small bumps called follicular hyperkeratosis that develop around the elbows and knees or soft, velvety skin on the palms and soles. Some people may also have wounds that split open with little bleeding and widen over time to create shallow scars 1. Rarely, individuals with Bethlem myopathy may develop breathing problems as the disease progresses 2.
Bethlem myopathy diagnosis
Bethlem myopathy is typically diagnosed based on a clinical evaluation that identifies signs and symptoms typical of people with the disease. A healthcare provider may recommend additional laboratory test including 3:
- Blood test measuring creatine kinase (CK) levels: Creatine kinase (CK), an enzyme that is often found in abnormally high levels when muscle is damaged. Creatine kinase (CK) levels will typically be normal or only slightly elevated. The detection of elevated CK levels can confirm that muscle is damaged or inflamed, but cannot confirm a diagnosis.
- Muscle biopsy, a surgical removal and microscopic examination (biopsy) of affected muscle tissue that may reveal characteristic changes to muscle fibers
- Skin biopsy
- Muscle MRI
- Electromyography (EMG) a test that assesses the health of muscles and the nerves that control muscles. During an electromyography, a needle electrode is inserted through the skin into an affected muscle. The electrode records the electrical activity of the muscle. This record shows how well a muscle responds to the nerves and can determine whether muscle weakness is caused by the muscle themselves or by the nerves that control the muscles. An electromyography can rule out nerve disorders such as motor neuron disease and peripheral neuropathy.
- Tests that evaluate the presence and number of certain muscle proteins (immunohistochemistry)
Genetic testing of the COL6A1, COL6A2, and COL6A3 genes can confirm the diagnosis.
Bethlem myopathy treatment
Treatment for Bethlem myopathy is symptomatic and supportive. This means that treatment aims to relieve symptoms and improve quality of life. There is currently no cure for the disease, and there are no specific medications for Bethlem myopathy. In many cases, physical therapy, stretching exercises, braces, splints, and mobility aids such as a walker or wheelchair are helpful. In rare cases, surgery may be needed to help with joint contractures or scoliosis 2.
Bethlem myopathy prognosis
Bethlem myopathy is not expected to shorten a person’s lifespan. People with Bethlem myopathy have symptoms that affect them for their whole lives, including progressive muscle weakness. About 66% of people with this disease require a walker, cane, or wheelchair after the age of 50 years. In some cases, people with Bethlem myopathy may require respiratory therapy, especially at night, to help them breathe. However, life-threatening complications associated with the disease are rare 2.
- Collagen VI-related myopathy. https://medlineplus.gov/genetics/condition/collagen-vi-related-myopathy[↩][↩][↩][↩][↩][↩]
- Lampe AK, Flanigan KM, Bushby KM, et al. Collagen Type VI-Related Disorders. 2004 Jun 25 [Updated 2012 Aug 9]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1503[↩][↩][↩][↩][↩][↩][↩][↩]
- Collagen Type VI-Related Disorders. https://rarediseases.org/rare-diseases/collagen-type-vi-related-disorders[↩][↩]
- Jöbsis GJ, Boers JM, Barth PG, de Visser M. Bethlem myopathy: a slowly progressive congenital muscular dystrophy with contractures. Brain. 1999;122:649–55.[↩]