Blast injury
An explosion creates a blast wave. An intense blast wave can tear tissue. A less intense blast can damage the eardrums, lungs, and abdomen. Blast waves also throw debris at very high speed that can injure any part of the body. Primary blast injury is organ and tissue damage caused solely by the effect of transmitted blast waves associated with high-order explosives. The principle mechanism driving the extent of blast injuries is the amount of kinetic energy released over a short time by the explosion 1. Blast injury from explosions that have the capability to cause multisystem, life-threatening injuries in single or multiple victims simultaneously. These types of events present complex triage, diagnostic, and management challenges for the health care provider.
High-energy events in which a solid or liquid is converted rapidly to a gas can occur at 3 rates:
- Deflagration: Rapid burning but minimal blast
- Explosion: Subsonic ignition and blast wind (low-grade explosive)
- Detonation: Supersonic ignition and blast wave (high-grade explosive)
An example of deflagration would be the rapid flash (without a bang) that results when an open pile of black powder (gunpowder) is ignited. The same black powder confined tightly in a container would cause a low-grade explosion. In high-grade explosives, the ignition wave travels through the material at supersonic speed and causes a supersonic blast (detonation) wave; common examples include nitroglycerin and trinitrotoluene (TNT).
In mass casualty incidents involving explosions, 3 concentric zones are identified:
- Blast epicenter
- Secondary perimeter
- Blast periphery
In the blast epicenter (kill zone), any survivors are probably mortally injured, technical rescue capabilities and extrication are likely to be required, and advanced life support and high victim-to-care-provider ratios are required for any survivors. In the secondary perimeter (critical casualty zone), survivors will have multiple injuries, and standard rescue capabilities and moderate victim-to-care-provider ratios are required. In the blast periphery (walking-wounded zone), most casualties will have non–life-threatening injuries and psychologic trauma, no rescue is required, and basic support and self-help are needed.
Blast injuries occur on various scales. In 2014 it was estimated that there were over 10,000 blast injuries related to fireworks in the United States 2. The Federal Bureau of Investigation reported that from 1987 to 1997, over 4,000 injuries and 448 deaths occurred in the United States due to illegal explosions of bombs or incendiary devices. In 2013, a notable explosion occurred at a fertilizer plant in Texas resulting in 15 deaths and many injuries. On a global scale, explosive devices are used as a means of terrorism. Blast injuries caused the vast majority of injuries to military personnel in recent wars and conflicts.
Blast injury causes
Explosives are categorized as high order explosives or low order explosives 2. High order explosives have a strong supersonic pressure wave, known as the blast wave or shock wave. Low order explosions have a subsonic explosion and lack the high order explosive blast wave. Examples of low order explosives include – pipe bombs, gun powder, petroleum-based bombs. In addition to the blast wave, an explosion can cause blast wind. Blast wind is the flow of superheated air that can interact with people and objects and cause injury or damage.
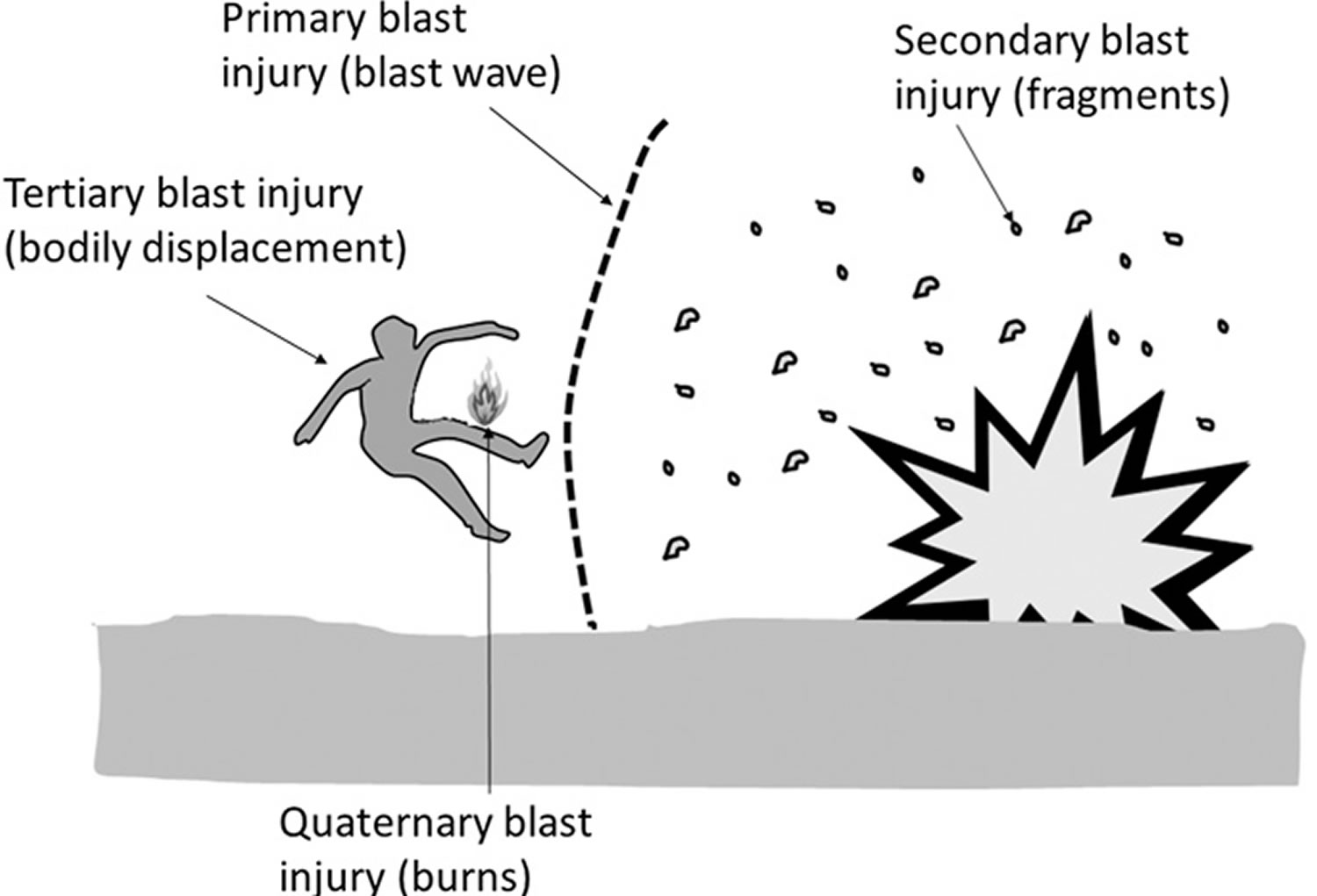
Chemical explosions cause injuries in four categories (primary, secondary, tertiary, and quaternary). The four categories are based on the impact on the human body due to the blast wave, blast wind, environmental/material factors present in the area of the blast.
Immediate death can occur from an explosion as a result of extensive pulmonary injury with pulmonary hemorrhage causing suffocation. Immediate death can also be caused by a pulmonary air embolism, severe head injury, significant internal injury, amputation, or impalement on an object 3.
Blast injury types
Blast injuries are generally categorized as primary to quaternary.
Primary blast injury
Primary blast injuries result from the impact of supersonic blast wave on body and preferentially affects hollow or gas-filled structures 4. Since only high order explosives create a blast wave, primary blast injuries are unique to high order explosions. The blast wave causes damage to more extensively to air-filled organs. The resulting barotrauma can affect the lungs, auditory organs, the eye, brain, and gastrointestinal tract.
- Blast ear – tympanic membrane rupture and middle ear damage
- Blast lung – injury to the lung parenchyma, can have delayed symptom presentation
- Blast brain – injury to brain parenchyma, even without direct injury to the head
- Blast eye – rupture of the globe of the eye
- Blast belly – injury causing abdominal hemorrhage and perforation (immediate and delayed). It can also cause injury to solid organs and testicular rupture.
Primary blast injuries can be subtle and have a delayed presentation. Blast lung should be considered in any victim that has dyspnea, cough, hemoptysis, and/or chest pain. The respiratory system can sustain significant injury, as a result of the blast wave. If the pressure exceeds 40 psi, the victim could sustain a pulmonary contusion, pneumothorax, air embolism, interstitial parenchyma damage, and/or subcutaneous emphysema. Pulmonary contusion is the most common respiratory system injury and it can be delayed in presentation up to 48 hours. Blast ear should be considered in any victim that has decreased hearing or hearing loss, tinnitus, vertigo and/or bleeding from the ear. If there is bleeding from the ear, consider that the blast was intense enough to cause injury to the lungs and hollow organs. In instances when the ear is over pressurized (greater than 5 psi), the bony ossicles of the ear can be dislocated, fractured and /or permanently destroyed 5. Blast belly should be considered in any victim presenting with abdominal pain, nausea, vomiting, vomiting blood, rectal pain, testicular pain, unexplained hypovolemia, abdominal distention, and/or rigidity. The colon is the most common area of hemorrhage and perforation. As with blast lung, intestinal perforation can occur acutely or may have a delayed presentation of up to 48 hours. Solid internal abdominal organs can also be contused or lacerated; however, solid organ damage occurs much less than does hollow organ damage. Blast brain should be considered in any victim presenting with headache, fatigue, confusion, poor concentration, amnesia, decreased level of consciousness, depression, anxiety, and/or insomnia. Blast eye should be considered in victims with eye pain, swelling, contusion or ecchymosis around the orbit, bleeding from the eye, decreased vision, and/or blindness 6. The heart can also be damaged by the blast wave. Victims can have chest pain, tachycardia, decreased pulse pressure, cardiac dysrhythmias and/or hypotension as a result of heart involvement. In victims with multiple presenting injuries or in incidents with multiple causalities, the injuries could be easy to miss. Victims of primary blast injuries may not initially show any obvious signs of injury.
Secondary blast injury
Secondary blast injuries are caused by the impact of airborne debris onto body. The secondary blast injuries are caused by debris that penetrates or interacts with the body surface. The debris can be from pieces of the explosive device itself and its contents, or material located around the initial blast device at the time of the explosion.
Secondary blast injuries account for the majority of injuries from an explosion event. The blast wave can carry debris a considerable distance causing injuries to anyone in its path. In intentional explosive devices, often they are constructed with the intent to injure as many people as possible. The device could be constructed with nails, metal ball bearings, screws, or other objects with the intent that they will be forcefully displaced during the blast to increase injuries to anyone in their path.
Secondary blast injuries are more common than primary blast injuries. Secondary blast injuries are the most common cause of mortality in victims of an explosion. Exposed areas of the victims’ body are at high risk for penetration of debris that is propelled by the explosion. Often areas of highest risk for injury are the head, neck, and extremities. Secondary blast injuries can be obvious or be deceiving. The force of the explosion can propel debris many times faster than a bullet. Thus, a seeming small wound could be hiding a devastating injury underneath. Injuries can include fractures, amputations, lacerations, dislocations, and any type of soft tissue injury 7.
Tertiary blast injury
Tertiary blast injury is caused by high-energy explosions; occurs when people fly through the air and strike other objects 8 or when a structure collapses and causes injury to the person. The resulting injury can be either blunt trauma due to the impact or penetrating injury if the victim is propelled and the striking structure enters the body. Injuries are determined by what the victim strikes. The strength of the explosion determines the severity of the injuries sustained. High explosive blasts can cause skull fractures, fractured bones, head injuries, or any traumatic injury (open or closed injuries, chest, abdominal, pelvic injuries, amputations, spinal injuries, and any others).
Structural collapse and entrapment can cause crush injuries and compartment syndrome. The longer it takes to extricate the victim the higher their mortality.
Quaternary blast injury
Quaternary blast injuries are comprised of all injuries that are not included in primary, secondary, or tertiary blast injury categories and encompass all other injuries caused by explosions (e.g., burns (chemical or thermal), toxic inhalation, crush injuries from collapsed structures and displaced heavy objects, injury from falling objects, falls resulting from the explosion, aggravation of medical disorders, toxic dust, gas, or radiation exposure) 9. Acute methemoglobinemia has been reported after nitroglycerine transcutaneous absorption resulting from a bomb explosion 10.
Quaternary blast injuries can be caused by exposure to resulting, fire, fumes, radiation, biological agents, smoke, dust, toxins, environmental exposure, and the psychological impact of the event. As a result of all the debris, wounds can be extremely contaminated with a wide variety of sources 11.
- Fire – burn injuries (flash, partial, full-thickness, airway)
- Fumes/smoke/dust – inhalation injuries and respiratory compromise
- Toxins – toxidromes from chemical exposures
- Environmental – heat/cold, exposure injuries
- Radiation – minor injury to death, depending on the type, amount, and exposure time to the source.
- Biological – variety of illness related to the agent released
A casualty’s underlying medical condition has a major impact on the effects on the impact of the resulting exposure on their mortality and morbidity.
- Lung disease – exacerbation of chronic obstructive pulmonary disease (COPD) or asthma.
- Heart disease – unstable angina, acute myocardial infarction
- High blood pressure – hypertensive emergency or urgency
Psychological disease – exacerbation of anxiety, depression, contribute to post-traumatic stress disorder (PTSD).
In an intentional explosion, other substances can be added to cause more injury, illness, or to induce more fear and panic in the community 12.
Quinary blast injury
Quinary blast injury is thought to result from toxic materials absorbed by the body from the blast 4. Quinary blast injury affects the immune system and perhaps the autonomic nervous system, leading to an immediate hyperinflammatory state.
Blast injury signs and symptoms
Unique patterns of injury are found in all blast types. The lungs, bowel, and middle ear are most susceptible to primary blast injuries. People who have sustained blast injury to the lungs may have shortness of breath, cough (including coughing up blood), chest pain, rapid breathing, and wheezing. People with an abdominal blast injury may have abdominal pain, nausea, vomiting, blood in their vomit, rectal pain, and testicular pain. Other blast injuries include blindness, deafness, spinal cord injury, or pain while walking. Some people may appear to have suffered a stroke or heart attack.
Primary blast injuries include:
- Pulmonary barotrauma (blast lung)
- Tympanic membrane rupture and middle ear damage
- Abdominal hemorrhage and intestinal perforation
- Eyeball rupture
- Mild traumatic brain injury (concussion)
Pulmonary barotrauma, the most common fatal primary blast injury, may include the following:
- Pulmonary contusion
- Systemic air embolism, which most commonly occlude blood vessels in the brain or spinal cord
- Free radical–associated injuries such as thrombosis, lipoxygenation, and disseminated intravascular coagulation (DIC)
- Impaired pulmonary performance lasting hours to days
- ARDS may be a result of direct lung injury or of shock from other body injuries
Acoustic barotrauma consists of the following:
- Tympanic membrane rupture (most common)
- Hemotympanum without perforation
- Ossicle fracture or dislocation may occur with very high-energy explosions
Thoracic primary blast injury produces the following unique cardiovascular response:
- A decrease in heart rate, stroke volume, and cardiac index
- The normal reflex increase in systemic vascular resistance does not occur, so blood pressure falls
- If this response is not fatal, recovery usually occurs within 15 minutes to 3 hours
Secondary blast injuries include:
- Penetrating or blunt injuries
- Eye penetration (evident or occult)
Tertiary blast injuries include:
- Fractures and traumatic amputations
- Closed and open brain injury
Quaternary blast injury include:
- Burns
- Crush injuries with rhabdomyolysis and compartment syndrome
- Respiratory tract injury from inhaled toxicants
- Asthma, angina, or myocardial infarction triggered by the event
Quaternary blast injury include:
- Fever
- Diaphoresis
- Low central venous pressure
- Tissue edema
Blast injury diagnosis
A history and physical directed to determined the extent of injuries is required. First you have to ensure that you and the environment is safe. The evaluate for any injury or compromise to the airway, breathing, or circulation. A determination of the the victims disability and the events leading to the incident can help guide the needs of further evaluation and treatment.
If possible, determine what material caused the explosion. High-order explosives undergo detonation, an almost instantaneous transformation of the original explosive material into gases occupying the same volume of space under extremely high pressure. These high-pressure gases rapidly expand, compress the surrounding medium, and produce a defining supersonic, overpressurization blast wave. Examples of high-order explosives include materials such as TNT, ammonium nitrate fuel oil, dynamite, and C-4 “plastic” explosives. In general, only high-order explosions produce severe primary blast injury.
Low-order explosives are composed of propellants, such as black powder, and pyrotechnics, such as fireworks. low-order explosives undergo deflagration rather than detonation and release energy relatively slowly compared with high-order explosives. This results in a subsonic explosion lacking the overpressurization blast wave that characterizes high-order explosives. Although low-order explosions can be deadly, low-order explosions very uncommonly cause the pulmonary and central nervous system injuries unique to primary blast injury.
If possible, determine the patient’s location relative to the center of the explosion. An explosion that occurs in an enclosed space (including a building, a mine, or a relatively lightly constructed enclosed space such as a bus) or in water tends to cause more serious injury. Intensity of an explosion pressure wave declines with the cubed root of the distance from the explosion. A person 3 m (10 ft) from an explosion experiences 9 times more overpressure than a person 6 m (20 ft) away. Proximity of the person to the explosion is an important factor in a primary blast injury. Blast waves are reflected by solid surfaces; thus, a person standing next to a wall may suffer increased primary blast injury.
Because explosions often cause multiple casualties, anticipate activating the hospital or regional disaster plan.
Another ominous consideration is the tactic of setting dual explosions. The initial explosion is intended to injure civilians and to attract law enforcement and rescue personnel, followed by a delayed explosion designed to injure rescuers. Hospital disaster plans should include tight security at all hospital entrances in the event of a terrorist explosion in the community. All hospital personnel should be alert for unattended packages.
In addition to protecting hospital patients and staff, sealing entrances helps control the chaotic flow of patients and visitors.
Industrial accidents and terrorist explosions may be associated with the release of toxic and/or radioactive materials. The Federal Bureau of Investigation (FBI) is particularly concerned about the possibility that a terrorist could attach a radioactive substance (eg, a radiopharmaceutical or part of an old radiography machine) to a conventional explosive device, causing radiation contamination of the scene and casualties. In the 1993 attack on the World Trade Center, terrorists attached cyanide to a bomb placed in the underground parking garage. Fortunately, in that incident the cyanide was destroyed by the combustion. Physicians and EMS personnel must diligently search for evidence of radiation and/or chemical contamination in persons with blast injuries.
Question plant managers, fire department officials, EMS personnel, and law enforcement personnel about these possibilities.
EMS agencies should check for radiation contamination at the scene of a deliberately caused explosion. In addition, hospital personnel should screen persons who have been exposed to deliberate explosions for radioactivity with a Geiger counter or similar radiation dosimeter. Each hospital has a radiation safety officer (usually a radiology technician) who can assist with this task.
Physical examination
The evaluation should begin with the ABCDEs as determined by the history and physical. The nature of the injuries will dictate what imaging, laboratory studies, ECG/echocardiogram, ultrasounds, compartment pressure measurements that need to be obtained.
Examine lungs for evidence of pulmonary contusion and pneumothorax.
- Assume that a patient’s wheezing associated with a blast injury is from pulmonary contusion.
- Other causes of wheezing in this setting may include inhalation of irritant gases or dusts, pulmonary edema from myocardial contusion, and adult respiratory distress syndrome (ARDS).
Many experts recommend obtaining a chest radiograph in the presence of isolated tympanic membrane rupture since this may indicate exposure to significant overpressure. In a large series of victims of terrorist bombings, mostly involving closed spaces, 22% of patients with eardrum perforation had other significant injuries.
- However, a patient with isolated tympanic membrane perforation, but no other immediately identified injuries, does not automatically require an extended period of observation. In the above study, none of the 137 patients initially identified as having isolated tympanic membrane rupture and well enough to be discharged developed later manifestation of pulmonary or intestinal blast injury.
- Intact tympanic membranes do not imply the absence of serious injury, especially if the patient was wearing some type of hearing protection as is common in certain types of military or law enforcement operations.
Abdominal injuries from explosions may be occult, and serial examinations are often required.
- A recent large Israeli case series found that abdominal injuries occurred only as a result of massive trauma. This finding may be the result of selection bias, as all the explosions in their series occurred in open air. Air is a poor conductor of blast-wave energy, thus those who were subjected to enough energy to damage abdominal organs probably were situated near the explosive devices.
- Other authors have reported occult injuries to both solid and hollow abdominal organs in people injured by closed-space explosions and blast injuries occurring in water.
Lab tests
Lab tests are essential for accurate diagnosis in the mass-casualty situation. Considerations include the following:
- Do not overwhelm the laboratory with screening or protocol laboratory tests of little clinical benefit
- Most patients injured by significant explosions should have a screening urinalysis
- If the explosion occurred in an enclosed space or was accompanied by fire, test carboxyhemoglobin (HbCO) and electrolytes to assess acid/base status
- Pulse oximetry readings may be misleading in cases of carbon monoxide (CO) poisoning
- Victims of major trauma should have baseline hemoglobin determinations, crossmatching for potential blood transfusion, and screening for disseminated intravascular coagulation (DIC)
Imaging studies
Indications for chest radiography are as follows:
- History of exposure to high overpressure
- Tympanic membrane rupture
- Respiratory symptoms
- Abnormal findings on chest auscultation
- Visible external signs of thoracic trauma
If significant abdominal pain is present, consider an immediate abdominal radiographic series (flat and upright films) or abdominal CT to detect pneumoperitoneum from enteric rupture. Intestinal barotrauma is more common with underwater than air blast injuries.
Focused Abdominal Sonography for Trauma (FAST) is a potentially useful tool for rapidly screening patients, especially in the setting of multiple seriously injured victims. A positive FAST examination in an unstable patient is an indication for surgical exploration of the abdomen in the operating room. A negative FAST examination is unreliable in the setting of penetrating trauma to the abdomen, flank, buttocks, or back, and it should be followed up with CT examination of the abdomen and pelvis.
Blast injury treatment
Treatment and managements are dictated by the injuries found on the history and physical examination. Carefully review and evaluation for blast injuries that can be delayed in presentation need to be specifically evaluated for if indicated 13.
Prehospital care
- Screen for radioactive contamination with a hand-held Geiger counter for any explosion that may involve radioactive material, including any explosion that may have been deliberately set; if radioactive material is detected, decontamination of personnel and equipment as well as notification of the receiving hospital is required
- Rapidly identify patients with life-threatening external hemorrhage and control bleeding; early use of tourniquets may be life-saving, especially in the setting of multiple seriously injured casualties
- High-flow oxygen should be administered to all patients with respiratory distress, abnormal findings on auscultation, and evidence of significant thoracic trauma
- Avoid administration of large quantities of IV fluid in patients with a high suspicion of ongoing internal hemorrhage; judicious fluid boluses may be required if patients exhibit signs and symptoms of inadequate perfusion, such as deteriorating mental status
- Initiate measures to reduce heat loss and prevent hypothermia.
EMS personnel should attempt to determine and report any information regarding the nature and size of the explosion; the time of occurrence; the proximity of the victim to the epicenter of the blast; victim displacement by the blast wind if any; the presence of secondary fires, smoke, dust, or chemical or radioactive contamination; and history of entrapment in collapsed structures. EMS personnel are responsible for activating appropriate disaster and/or hazardous material responses as early as possible.
- Screening for radioactive contamination with a hand-held Geiger counter is a prudent precaution for any explosion that may involve radioactive material, including any explosion that may have been deliberately set. If radioactive material is detected, decontamination of personnel and equipment as well as notification of the receiving hospital is required. The Radiation Emergency Action Center and Training Site provides advice and assistance (https://orise.orau.gov/reacts/).
- Significant extremity trauma and associated death from exsanguination is a major cause of preventable death. EMS personnel should rapidly identify patients with life-threatening external hemorrhage and control bleeding. Early use of tourniquets may be life-saving, especially in the setting of multiple seriously injured casualties.
- High-flow oxygen should be administered to all patients with respiratory distress, abnormal findings on auscultation, and evidence of significant thoracic trauma.
- EMS personnel should avoid administration of large quantities of intravenous fluid in patients with a high suspicion of ongoing internal hemorrhage. Judicious fluid boluses may be required if patients exhibit signs and symptoms of inadequate perfusion, such as deteriorating mental status, in this setting. Recent experiences on the battlefield suggest that Hextend is the preferred resuscitation fluid for the prehospital setting.
- EMS personnel should initiate measures to reduce heat loss and prevent hypothermia in the trauma patient since this condition is associated with increased mortality.
- In cases of life-threatening extremity trauma secondary to blast injuries, early use of tourniquets may prove lifesaving. In a study comparing combat application tourniquet (CAT) to the newer emergency and military tourniquet (EMT) pneumatic tourniquet, the CAT tourniquet proved ineffective in controlling arterial blood flow when applied at mid-thigh level while EMT was successful in a significantly larger number of patients 14.
The FDA has approved an expandable, multi-sponge, temporary wound dressing (XSTAT) to control bleeding from certain types of wounds received in battle. The dressing, which can be used for up to four hours, consists of 3 syringe-style applicators with 92 compressed cellulose sponges that have an absorbent coating. These sponges expand and swell to fill the wound cavity, creating a temporary physical barrier to blood flow. Each tablet-shaped sponge measures 9.8 millimeters in diameter and 4 to 5 millimeters in height, and can absorb 3 milliliters of blood or body fluid. This dressing is currently approved for military use only 15.
Emergency department care
- Penetrating wounds (secondary blast injury), blunt trauma (tertiary/secondary blast injury), and burns receive standard treatment
- Shrapnel wounds (secondary blast injury) are treated as low-velocity gunshot wounds
- Hemodynamically unstable patients with significant trauma may benefit from early use of packed red blood cells and fresh frozen plasma (FFP) in a 1:1 ratio, as well as platelets
- Consider early use of fresh whole blood if available
- In patients with severe trauma, also consider cryoprecipitate and recombinant factor VIIa
- In patients with traumatic brain injury, prevention of hypoxia and hypotension is critical
- Because pulmonary contusion tends to evolve over several hours, a period of observation and repeat radiography may be necessary if indicated; definitive airway management and ventilatory support may be required
- If abdominal pain persists or vomiting develops, consider admitting the patient for observation, as intestinal hematoma may be difficult to detect in the emergency department
- In patients with open wounds from blasts, consider broad-spectrum prophylactic antibiotics and provide tetanus toxoid if immunization is not up to date.
Examine the lungs, abdomen, and tympanic membranes of all patients exposed to a significant explosion.
Penetrating wounds (secondary blast injury), blunt trauma (tertiary/secondary blast injury), and burns receive standard treatment.
Shrapnel wounds (secondary blast injury) are treated as low-velocity gunshot wounds.
Hemodynamically unstable patients with significant trauma may benefit from early use of packed red blood cells and fresh frozen plasma (FFP) in a 1:1 ratio, as well as platelets. Recent battlefield experience suggests a benefit to the early use of fresh whole blood if available. Additionally, cryoprecipitate and recombinant factor VIIa should be considered in the severe trauma patient, especially in the setting of massive transfusion requirements. One review of 3 mass casualty incidents following explosive events in Iraq suggested that this resuscitation strategy resulted in the transfusion of an average 3.5 units of PRBC and 3.8 units of plasma, as well as a mortality rate of 8% 16.
The prevention of hypoxia and hypotension are critical in patients with traumatic brain injury to prevent significant increases in mortality 17.
Because pulmonary contusion tends to evolve over several hours, a period of observation and repeat radiography may be necessary if indicated. Definitive airway management and ventilatory support may be required.
If abdominal pain persists or vomiting develops, consider admitting the patient for observation. Intestinal hematoma may be difficult to detect in the emergency department.
White phosphorus burns require unique management. Initial management of white phosphorus-contaminated burns consists of copious lavage of the area, removing identifiable particles (which should be placed in water to prevent further combustion), and covering the area with saline-soaked gauze to prevent further combustion. Use of a Wood lamp in a darkened resuscitation suite or operating room may help identify white phosphorus particles in the wound.
Definitive treatment consists of a rinse using 1% copper sulfate (CuSO4) solution and removing the white phosphorus particles. Copper sulfate combines with phosphorous particles to create a blue-black cupric phosphide coating. This impedes further white phosphorus combustion and makes particles easier to find. Rinse the contaminated burn with copper sulfate solution, remove white phosphorus particles, and then use copious saline lavage to rinse off the copper sulfate. Never apply copper sulfate as a dressing. Excess copper sulfate absorption can cause intravascular hemolysis and renal failure.
White phosphorus injury can lead to hypokalemia and hyperphosphatemia with ECG changes, cardiac arrhythmias, and death. Place the patient on a cardiac monitor and closely track serum calcium levels. Intravenous (IV) calcium may be required. Moistened face masks and good ventilation help protect patients and medical personnel from the pulmonary effects of phosphorous pentoxide gas. Naturally, avoid the use of flammable anesthetic agents and excessive oxygen around white phosphorus.
- Temizkan S, Kelestimur F. A clinical and pathophysiological approach to traumatic brain injury-induced pituitary dysfunction. Pituitary. 2019 Jun;22(3):220-228.[↩]
- Jorolemon MR, Krywko DM. Blast Injuries. [Updated 2019 Nov 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430914[↩][↩]
- Dokoupil M, Marecová K, Uvíra M, Joukal M, Mrázková E, Chmelová J, Handlos P. Fatal delayed hemopericardium and hemothorax following blunt chest trauma. Forensic Sci Med Pathol. 2019 Jun;15(2):272-275.[↩]
- Explosives and Blast Injuries. https://www.merckmanuals.com/professional/injuries-poisoning/mass-casualty-weapons/explosives-and-blast-injuries[↩][↩]
- Van Haesendonck G, Van Rompaey V, Gilles A, Topsakal V, Van de Heyning P. Otologic Outcomes After Blast Injury: The Brussels Bombing Experience. Otol. Neurotol. 2018 Dec;39(10):1250-1255.[↩]
- Williams ST, Harding TH, Statz JK, Martin JS. Blast Wave Dynamics at the Cornea as a Function of Eye Protection Form and Fit. Mil Med. 2017 Mar;182(S1):226-229.[↩]
- Shuker ST. Emergency Treatment of Blast, Shell Fragment and Bullet Injuries to the Central Midface Complex. J Maxillofac Oral Surg. 2019 Mar;18(1):124-130.[↩]
- Blast Injuries. https://emedicine.medscape.com/article/822587-overview[↩]
- Mathews ZR, Koyfman A. Blast Injuries. J Emerg Med. 2015 Oct. 49 (4):573-87.[↩]
- Badii F, Maghelli S, Costa N, Borreggine D, Zoccali G, Durì D. Acute methemoglobinemia after nitroglycerine transcutaneous absorption after bomb explosion: a case report. J Trauma. 2009 Mar. 66(3):936-7.[↩]
- Singh AK, Ditkofsky NG, York JD, Abujudeh HH, Avery LA, Brunner JF, Sodickson AD, Lev MH. Blast Injuries: From Improvised Explosive Device Blasts to the Boston Marathon Bombing. Radiographics. 2016 Jan-Feb;36(1):295-307.[↩]
- Prat NJ, Daban JL, Voiglio EJ, Rongieras F. Wound ballistics and blast injuries. J Visc Surg. 2017 Dec;154 Suppl 1:S9-S12.[↩]
- Webster CE, Clasper J, Gibb I, Masouros SD. Environment at the time of injury determines injury patterns in pelvic blast. J R Army Med Corps. 2019 Feb;165(1):15-17.[↩]
- Taylor DM, Vater GM, Parker PJ. An evaluation of two tourniquet systems for the control of prehospital lower limb hemorrhage. J Trauma. 2011 Sep. 71(3):591-5.[↩]
- https://www.accessdata.fda.gov/cdrh_docs/reviews/K130218.pdf[↩]
- Propper BW, Rasmussen TE, Davidson SB, Vandenberg SL, Clouse WD, Burkhardt GE. Surgical response to multiple casualty incidents following single explosive events. Ann Surg. 2009 Aug. 250(2):311-5.[↩]
- DeWitt DS, Prough DS. Blast-induced brain injury and posttraumatic hypotension and hypoxemia. J Neurotrauma. 2009 Jun. 26(6):877-87.[↩]