What is brain natriuretic peptide
Brain natriuretic peptide also called B-type natriuretic peptide, are small proteins (peptide) secreted by the brain and the heart atria, stored mainly in cardiac ventricular myocardium. Brain natriuretic peptide was originally discovered in porcine brain, where it was thought to be a neurotransmitter 1, hence its original name, brain natriuretic peptide. Subsequently, it was shown to be 10-fold more abundant in the heart than in the brain, hence the current term, B-type natriuretic peptide 2. Brain natriuretic peptide or B-type natriuretic peptide (BNP) is actually produced primarily by cells in the left ventricle of the heart and it is distinguished from a similar protein made in the atria, or upper chambers, of the heart, termed atrial natriuretic peptide (ANP). Brain natriuretic peptide is produced by direct synthesis in response to the degree of ventricular stretch, and also upregulated in failing ventricular myocardium 3.
The left ventricle is the heart’s main pumping chamber and is responsible for sending oxygenated blood from the lungs to the remainder of the body. It is associated with blood volume and pressure and with the work that the heart must do in pumping blood throughout the body. Small amounts of a precursor protein, pro-BNP, are continuously produced by the heart. Pro-BNP is then split by the enzyme called corin to release the active hormone brain natriuretic peptide (BNP) and an inactive fragment, N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP), into the blood.
The N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP), is secreted alongside brain natriuretic peptide and has been documented to have important diagnostic value in heart failure and act as a reliable biomarker of ventricular dilatation 4. Brain natriuretic peptide and N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP) are continually produced in small quantities in the heart. When the left ventricle of the heart is having difficulty pumping sufficient amounts of blood to the body, the concentrations of active hormone brain natriuretic peptide (BNP) and inactive fragment N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP) produced can increase markedly. This may occur with many diseases that affect the heart and circulatory system. The increase in circulating brain natriuretic peptide or NT-proBNP will reflect this diminished capacity to deliver oxygenated blood to the body.
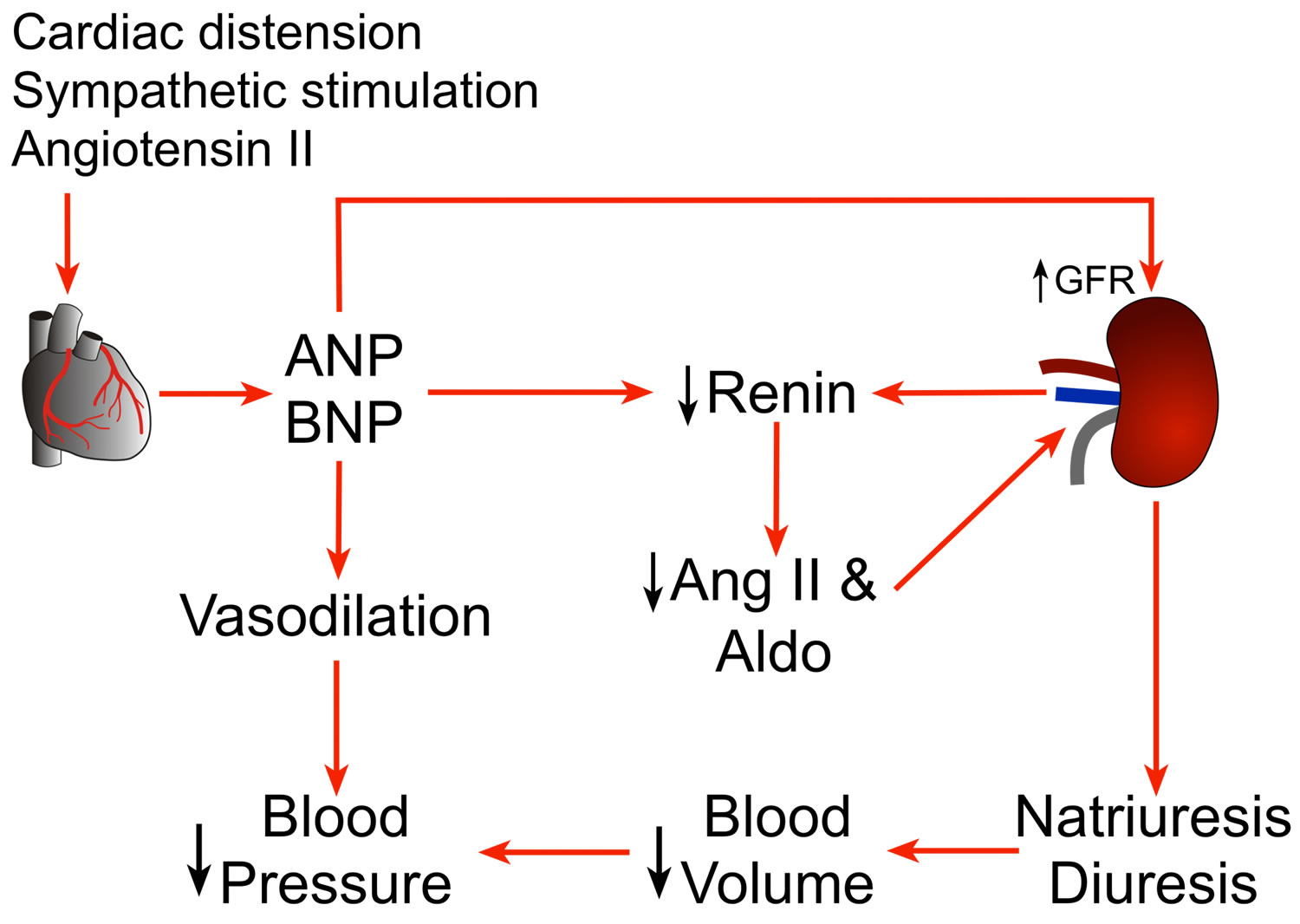
Brain natriuretic peptide can cause natriuresis (excretion of sodium in the urine), diuresis (increased production of urine), vasodilation (dilatation of blood vessels, which decreases blood pressure) and inhibits secretion of renin and aldosterone 5. This supports fluid retention and volume expansion in the arteries and veins. Subsequently, the heart muscle is stretched and works hard to pump blood under normal resting condition. Tests for brain natriuretic peptide and N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP) measure their levels in the blood in order to detect and evaluate heart failure.
According to the American Heart Association, more than 6 million people in the United States are living with heart failure and the number is growing. It is estimated that one in five American adults age 40 and older will develop heart failure in their lifetime. You may be at increased risk of developing heart failure if you have conditions such as heart disease, high blood pressure, or diabetes, or if you have had a heart attack. Other risk factors include tobacco use, alcohol use, and obesity.
Brain natriuretic peptide is eliminated by binding to the natriuretic peptide clearance receptor (NPR-C) or degradation by neutral endopeptidase on endothelial cells, smooth muscle cells, cardiac myocytes, renal epithelium, and fibroblasts 3. NT-proBNP is cleared mainly by the kidney 6. Brain natriuretic peptide has a relatively shorter half-life of about 20 minutes; the half-life of N-terminal part of the prohormone of brain natriuretic peptide (NT-proBNP) is about 60–90 minutes and would be expected to be longer in the setting of renal dysfunction. Obese patients especially those who have body mass index greater than 30 tend to have lower brain natriuretic peptide levels than others. Neutral endopeptidases that are secreted by adipose tissue may be related to increased brain natriuretic peptide clearance in obese patients 7.
Nesiritide, a recombinant form of brain natriuretic peptide (BNP), is approved for the treatment of acute heart failure. However, it has not been recommended for routine use in treatment of acute heart failure exacerbations, based on randomized controlled trial data demonstrating no difference in the rate of death or rehospitalization with nesiritide compared with placebo and its association with an increased risk of hypotension 8.
Brain natriuretic peptide test
A test for brain natriuretic peptide or NT-pro brain natriuretic peptide is primarily used to help detect, support diagnosis, and in some instances evaluate the severity of heart failure. The two tests are not interchangeable and should not be used together. Your healthcare practitioner should order one or the other but not both.
Brain natriuretic peptide and NT-pro brain natriuretic peptide (NT-proBNP) measurement is a powerful diagnostic and prognostic tool for detection of ventricular dysfunction. It is an ideal test for detection of cardiac failure in primary care, allowing cardiac failure to be definitively ruled out as a cause of shortness of breath (dyspnea). However, this test lacks specificity, and a high level of this hormone is not diagnostic of acute heart failure 9. Other laboratory tests include troponin T (to detect heart attack [myocardial infarction], although the levels may be high due to heart failure itself), complete blood count, basic metabolic panel (low sodium, in particular, indicates advanced disease) and liver function tests (to detect liver injury due to volume overload).
A brain natriuretic peptide or NT pro brain natriuretic peptide test may be ordered in a healthcare practitioner’s office when you have signs and symptoms that could be due to heart failure. These may include:
- Difficulty breathing, shortness of breath
- Fatigue
- Swelling in the feet, ankles, legs, abdomen
Testing may be done in the emergency room or in a hospital bed when you are in crisis and/or have symptoms that could be due to heart failure and healthcare practitioners need to quickly distinguish whether you are suffering from heart failure or some other medical problem.
Several brain natriuretic peptide or NT-pro brain natriuretic peptide tests may be done over a period of time when you are being treated for heart failure to monitor the effects of therapy.
A brain natriuretic peptide test or NT-pro brain natriuretic peptide test can be used, along with other cardiac biomarker tests, to detect heart stress and damage and/or along with lung function tests to distinguish between causes of shortness of breath. Chest X-rays and an ultrasound test called echocardiography may also be performed. Your healthcare practitioner may also prescribe a stress test, which takes place on a treadmill.
Heart failure can be confused with other conditions, and it may co-exist with them. Brain natriuretic peptide and NT-pro brain natriuretic peptide levels can help healthcare practitioners differentiate between heart failure and other problems, such as lung disease. An accurate diagnosis is important because the treatments are often different and must be started as soon as possible.
Although brain natriuretic peptide and NT-pro brain natriuretic peptide are usually used to recognize heart failure, an increased level in people who have had a heart attack may indicate an increased risk of further heart disease. Thus, a healthcare practitioner may use either brain natriuretic peptide or NT-pro brain natriuretic peptide to evaluate risk of further heart disease in someone who has had a heart attack.
Several tests are available for further evaluation of heart failure:
- Electrocardiography can show nonspecific findings, like ischemic changes, left ventricular hypertrophy, or arrhythmias.
- Echocardiography can help distinguish heart failure with reduced ejection fraction (HFrEF with EF less than 40%) from heart failure with preserved ejection fraction (HFpEF with EF over 50%) by determining the ejection fraction, and diastolic left ventricular function can evaluate associated regional wall motion abnormalities that may be suggestive of an ischemic component, as well as valvular and pericardial pathologies.
- Coronary angiography is indicated in patients with anginal symptoms and may also be indicated in patients with worsening heart failure symptoms 10.
Brain natriuretic peptide levels
Normal results indicate that signs and symptoms are likely due to something other than heart failure. In general, results of less than 100 picograms/milliliter (pg/mL) are a sign a person does not have heart failure. Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Talk to your health care provider about the meaning of your specific test results.
Higher-than-normal results suggest that you have some degree of heart failure and the level of brain natriuretic peptide or NT-pro brain natriuretic peptide in the blood may be related to its severity. A result greater than 100 picograms/mL is abnormal. The higher the number, the more likely heart failure is present and the more severe it is. Increased plasma levels of circulating brain natriuretic peptide or NT-pro brain natriuretic peptide have been described in patients with congestive heart failure and are directly proportional to the severity of congestive heart failure as classified by the New York Heart Association criteria 11. This rise is seen consistently and has been reported for long-acting natriuretic peptide, brain natriuretic peptide and NT-pro brain natriuretic peptide 12. The current American College of Cardiology/American Heart Association guidelines for managing heart failure have incorporated using natriuretic peptide levels in establishing the prognosis and disease severity of chronic heart failure and acutely decompensated heart failure 13. N-terminal proANP and brain natriuretic peptide have been reported to be more sensitive indicators of systolic left ventricular dysfunction 14. Higher levels of brain natriuretic peptide or NT-pro brain natriuretic peptide are often associated with an increased need for aggressive therapy. In some individuals with chronic heart failure, the markers may remain elevated and cannot be used to monitor response.
In general, the following cut off values may be employed for acutely dyspneic patients 15:
Brain natriuretic peptide (BNP)
- < 100 pg/mL – heart failure unlikely
- >400 pg/mL – heart failure likely
- 100-400 pg/mL – Use clinical judgment
NT-pro brain natriuretic peptide (NT pro-BNP)
- < 300 pg/mL – heart failure unlikely
- Age < 50 years, NT-pro brain natriuretic peptide >450 pg/mL – heart failure likely
- Age 50-75 years, NT-pro brain natriuretic peptide >900 pg/mL – heart failure likely
- Age >75 years, NT-pro brain natriuretic peptide >1800 pg/mL – heart failure likely
In patients with a prior diagnosis of heart failure, knowledge of optivolemic natriuretic peptide values is important when interpreting elevated levels of these molecules.
Sometimes other conditions can cause high brain natriuretic peptide levels. These include 13:
- Kidney failure .e.g, acute renal failure and chronic renal failure
- Pulmonary embolism
- Pulmonary hypertension
- Severe infection (sepsis)
- Lung problems e.g., severe chronic obstructive pulmonary disease (COPD), adult respiratory distress syndrome (ARDS), pneumonia
- Hypertension
- Cardiac causes -myocardial infarction, atrial fibrillation, acute coronary syndrome, cardioversion, valvular heart disease, myocarditis
- Older age
- Female sex
- Liver cirrhosis
- Hyperthyroidism
- Chemotherapy
Brain natriuretic peptide and NT-pro brain natriuretic peptide levels decrease in most people who are taking drug therapies for heart failure, such as angiotensin-converting enzyme (ACE) inhibitors, beta blockers, and diuretics.
Levels of both brain natriuretic peptide and NT-pro brain natriuretic peptide tend to increase with age in the absence of disease.
Levels of NT-pro brain natriuretic peptide and brain natriuretic peptide may be increased in persons with kidney disease due to reduced clearance. Obese individuals may have lower concentrations of brain natriuretic peptide or NT-pro brain natriuretic peptide.
While both brain natriuretic peptide and NT-pro brain natriuretic peptide will rise with left ventricle dysfunction and either can be measured for diagnosis or monitoring therapy, they are not interchangeable and the results cannot be directly compared.
Conditions associated with lower than expected brain natriuretic peptide are as follows:
- Obesity
- Flash pulmonary edema
- Pericardial constriction
- Sudoh T, Kangawa K, Minamino W, Matsuo H. A new natriuretic peptide in porcine brain. Nature. 1988;332:78–81.[↩]
- Saito Y, Nakao K, Itoh H, Yamada T, Mukoyama M, Arai H, et al. Brain natriuretic peptide is a novel cardiac hormone. Biochem Biophys Res Commun. 1989;158:360–8.[↩]
- Pandit K, Mukhopadhyay P, Ghosh S, Chowdhury S. Natriuretic peptides: Diagnostic and therapeutic use. Indian J Endocrinol Metab. 2011;15 Suppl 4(Suppl4):S345–S353. doi:10.4103/2230-8210.86978 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3230091[↩][↩]
- Witthaut R. Science review: Natriuretic peptides in critical illness. Crit Care. 2004;8:342–9.[↩]
- Nakao K, Ogawa Y, Suga S, Imura H. Molecular biology and biochemistry of the natriuretic system. I. Natriuretic peptides. J Hypertens. 1992;10:907–12.[↩]
- Schrier RW, Abraham WT. Hormones and hemodynamics in heart failure. N Engl J Med. 1999;341:577–85.[↩]
- Young JB, Correia NG, Francis GS, Maisel A, Michota F. Testing for B-type natriuretic peptide in the diagnosis and assessment of heart failure: What are the nuances? Cleve Clin J Med. 2004;71(Suppl 5):S1–17.[↩]
- O’Connor CM, Starling RC, Hernandez AF, Armstrong PW, Dickstein K, Hasselblad V, et al. Effect of Nesiritide in Patients with Acute Decompensated Heart Failure. N Engl J Med 2011; 365: 32-43.[↩]
- Kelder JC, Cramer MJ, van Wijngaarden J, van Tooren R, Mosterd A, Moons KG, Lammers JW, Cowie MR, Grobbee DE, Hoes AW. The diagnostic value of physical examination and additional testing in primary care patients with suspected heart failure. Circulation. 2011 Dec 20;124(25):2865-73.[↩]
- Ferreira JP, Rossignol P, Demissei B, Sharma A, Girerd N, Anker SD, Cleland JG, Dickstein K, Filippatos G, Hillege HL, Lang CC, Metra M, Ng LL, Ponikowski P, Samani NJ, van Veldhuisen DJ, Zwinderman AH, Voors A, Zannad F. Coronary angiography in worsening heart failure: determinants, findings and prognostic implications. Heart. 2018 Apr;104(7):606-613.[↩]
- Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007 May 15. 49(19):1943-50.[↩]
- Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al. Breathing Not Properly Multinational Study Investigators.Bedside B-type natriuretic peptide in the emergency diagnosis of heart failure: Primary results from the Breathing Not Properly (BNP) Multinational Study. N Engl J Med. 2002;347:161–7.[↩]
- [Guideline] Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15. 128(16):e240-327.[↩][↩]
- Muders F, Kromer E, Griese DP, Pfeifer M, Hense HW, Riegger GA, et al. Evaluation of plasma natriuretic peptides as markers for left ventricular dysfunction. Am Heart J. 1997;134:442–9.[↩]
- Maisel A, Mueller C, Adams K Jr, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008 Sep. 10(9):824-39.[↩]