Breech baby
Breech baby also called breech birth, means your baby is lying bottom-first or feet-first in the uterus (womb) instead of in the usual head-first position. Right before birth, most babies are in a headfirst position in the mother’s uterus. Babies can be breech early in pregnancy. Most of them turn on their own to be headfirst by the time of delivery. As you get closer to your due date, your doctor will be able to tell if your baby is breech. They can check by a physical exam, ultrasound, or both.
Babies are more likely to be breech if:
- They are early, or premature.
- They are part of a multiple birth (two or more babies).
- There is an abnormal level of amniotic fluid.
- The mother has an abnormal shaped uterus.
Babies born in the breech position (bottom first) are at increased risk of complications at birth because of a delay in birth of the head. Turning a breech baby to head first in late pregnancy may reduce these complications. A procedure called external cephalic version (ECV) describes when obstetricians use their hands on the woman’s abdomen to gently try to turn the baby from the breech position to head first presentation at birth so as to avoid the adverse effects of breech vaginal birth or caesarean section. A number of treatments may help the success of external cephalic version (ECV). These include using tocolytic drugs (drugs like beta stimulants and calcium channel blockers that relax the womb), stimulating the baby with sound through the mother’s abdomen (acoustic stimulation), increasing the fluid surrounding the baby (transabdominal amnioinfusion), injecting pain‐relieving drugs into the mother’s lower back to produce regional analgesia (epidural or spinal analgesia), giving the mother opioid drugs to help her relax, using hypnosis and applying gel or talcum powder to the mother’s abdomen 1. Clinical studies involving 2786 women showed that babies are more likely to turn head first during external cephalic version (ECV) and to remain head first for the start of labor, if women receive beta stimulants 1. These drugs also reduced the number of caesarean sections, but insufficient data on possible adverse effects were collected. Little information on other types of tocolytic drugs was available, although nitric oxide donors were associated with an increase in headaches. In addition, too little evidence was available to show whether the other ways of trying to help external cephalic version (ECV) are effective. Further research is needed if to increase the success of external cephalic version (ECV).
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
It is not always possible to turn your baby from being breech. Some breech babies can be safely delivered through the vagina, but usually doctors deliver them by C-section (caesarean section). Risks involved with a C-section C-section (caesarean section) include bleeding and infection. There also can be a longer hospital stay for both the mother and her baby.
Other risks can occur for breech babies who are born vaginally. These include:
- An injury during or after delivery.
- An injury where the baby’s hip socket and thigh bone become separated.
- Problems with the umbilical cord. For example, the umbilical cord can be flattened during delivery. This can cause nerve and brain damage due to a lack of oxygen.
Key points to remember
- Breech is very common in early pregnancy, and by 36–37 weeks of pregnancy most babies will turn into the head-first position. If your baby remains breech, it does not usually mean that you or your baby have any problems 2.
- Towards the end of pregnancy, only 3–4 in every 100 (3–4%) babies are in the breech position 2.
- Turning your baby into the head-first position so that you can have a vaginal delivery is a safe option 2.
- The alternative to turning your baby into the head-first position is to have a planned Caesarean section or a planned vaginal breech birth.
Why turn my baby head-first?
Successful external cephalic version (ECV) lowers your chances of requiring a caesarean section and its associated risks. If your external cephalic version (ECV) is successful and your baby is turned into the head-first position you are more likely to have a vaginal birth.
Is there anything else I can do to help my baby turn?
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of a registered healthcare practitioner.
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground. Other options you might hear include acupuncture and chiropractic treatment. There is no good evidence that these work. Discuss with your doctor or midwife before undergoing any treatment during pregnancy.
Natural methods
Some people look to natural ways to try and turn their baby. These methods include exercise positions, certain stimulants, and alternative medicine. They may help but there is no scientific evidence that they work.
- Breech tilt, or pelvic tilt: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Stay in the tilt for about 10 to 20 minutes. You can do this exercise three times a day. It may help to do it at a time when your baby is actively moving in your uterus.
- Inversion: There are a few moves you can do that use gravity to turn the baby. They help relax your pelvic muscles and uterus. One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity.
- Music: Certain sounds may appeal to your baby. Place headphones or a speaker at the bottom of your uterus to encourage them to turn.
- Temperature: Like music, your baby may respond to temperature. Try placing something cold at the top of your stomach where your baby’s head is. Then, place something warm (not hot) at the bottom of your stomach.
- Webster technique: This is a chiropractic approach. It is meant to align your pelvis and hips, and relax your uterus. The goal is to promote your baby to turn.
- Acupuncture: This is a form of Chinese medicine. It involves placing needles at pressure points to balance your body’s energy. It can help relax your uterus and stimulate your baby’s movement.
What are my options for birth if my baby remains breech?
Depending on your situation, your choices are:
- planned caesarean section
- planned vaginal breech birth.
There are benefits and risks associated with both caesarean section and vaginal breech birth, and these should be discussed with you so that you can choose what is best for you and your baby.
Caesarean section
If your baby remains breech towards the end of pregnancy, you should be given the option of a caesarean section. Research has shown that planned caesarean section is safer for your baby than a vaginal breech birth 2. Caesarean section carries slightly more risk for you than a vaginal birth.
Caesarean section can increase your chances of problems in future pregnancies. These may include placental problems, difficulty with repeat caesarean section surgery and a small increase in stillbirth in subsequent pregnancies.
If you choose to have a caesarean section but then go into labor before your planned operation, your healthcare professional will examine you to assess whether it is safe to go ahead. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
Vaginal breech birth
After discussion with your healthcare professional about you and your baby’s suitability for a breech delivery, you may choose to have a vaginal breech birth. If you choose this option, you will need to be cared for by a team trained in helping women to have breech babies vaginally. You should plan a hospital birth where you can have an emergency caesarean section if needed, as 4 in 10 (40%) women planning a vaginal breech birth do need a caesarean section. Induction of labor is not usually recommended.
While a successful vaginal birth carries the least risks for you, it carries a small increased risk of your baby dying around the time of delivery 2. A vaginal breech birth may also cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby. Your individual risks should be discussed with you by your healthcare team.
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your healthcare professional. They may advise against a vaginal birth if:
- your baby is a footling breech (one or both of the baby’s feet are below its bottom)
- your baby is larger or smaller than average (your healthcare team will discuss this with you)
- your baby is in a certain position, for example, if its neck is very tilted back (hyper extended)
- you have a low-lying placenta (placenta previa: a low-lying placenta after 20 weeks)
- you have pre-eclampsia or any other pregnancy problems.
What if I go into labor early?
If you go into labor before 37 weeks of pregnancy, the balance of the benefits and risks of having a caesarean section or vaginal birth changes and will be discussed with you.
What can I expect in labor with a breech baby?
With a breech baby you have the same choices for pain relief as with a baby who is in the head-first position. If you choose to have an epidural, there is an increased chance of a caesarean section. However, whatever you choose, a calm atmosphere with continuous support should be provided.
If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously as this has been shown to improve your baby’s chance of a good outcome.
In some circumstances, for example, if there are concerns about your baby’s heart rate or if your labor is not progressing, you may need an emergency caesarean section during labor. A pediatrician (a doctor who specializes in the care of babies, children and teenagers) will attend the birth to check your baby is doing well.
What if I am having more than one baby and one of them is breech?
If you are having twins and the first baby is breech, your healthcare professional will usually recommend a planned caesarean section.
If, however, the first baby is head-first, the position of the second baby is less important. This is because, after the birth of the first baby, the second baby has lots more room to move. It may turn naturally into a head-first position or a doctor may be able to help the baby to turn.
If you would like further information on breech babies and breech birth, you should speak with your healthcare professional.
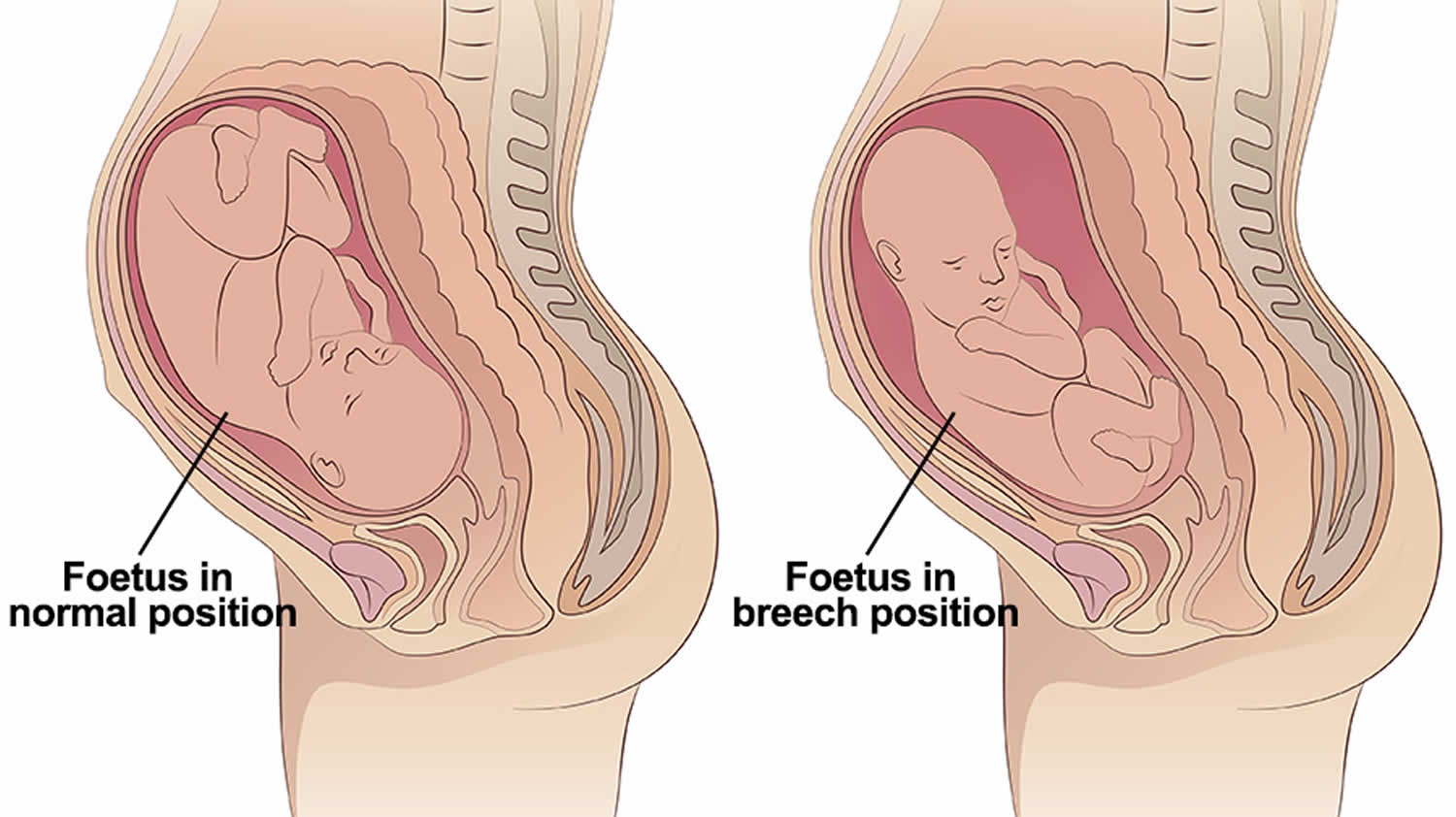
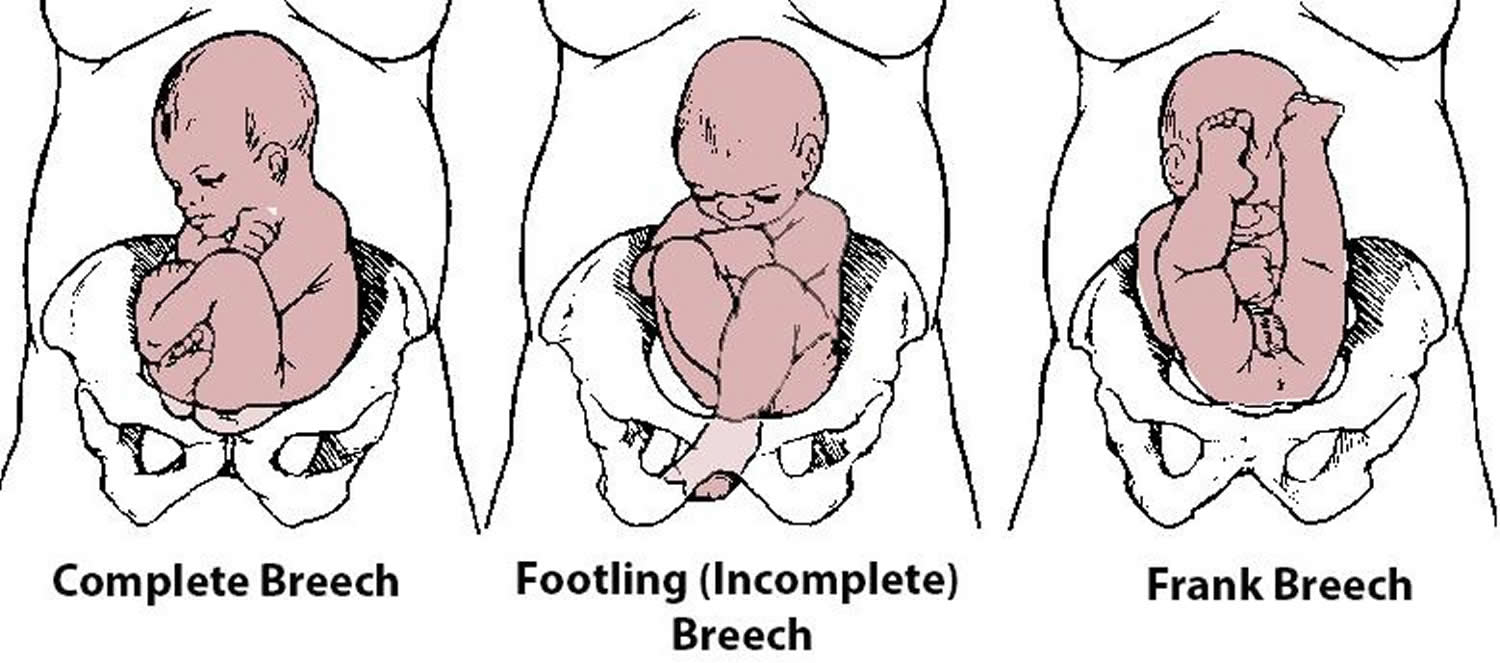
Breech position of baby
A breech baby may be lying in one of the following positions:
- Frank or extended breech – the baby is bottom first, with the thighs against its chest and feet up by its ears. Most breech babies are in this position.
- Flexed or complete breech – the baby is bottom first with its feet right next to its bottom. The thighs are against its chest and the knees are bent.
- Footling or incomplete breech – when one or both of the baby’s feet are below its bottom.
Figure 1. Breech position of baby
Breech baby causes
Breech presentation may be caused by an underlying fetal or maternal abnormality, or may be an apparently chance occurrence, or may be related to an otherwise benign variant such as the placenta situated in an upper lateral corner of the uterus (cornual placental position) 3. In the latter two instances, breech presentation places a healthy baby and mother at increased risk of a complicated vaginal birth or caesarean section.
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
- if this is your first pregnancy
- if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information A low-lying placenta (placenta previa) after 20 weeks
- if you have too much (polyhydramnios) or too little fluid (amniotic fluid) (oligohydramnios) around your baby
- if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the ultrasound scan you are offered at around 20 weeks of pregnancy.
How to turn a breech baby
External cephalic version (ECV) should be carried out by a doctor or a midwife trained in external cephalic version (ECV). It should be carried out in a hospital where you can have an emergency caesarean section if needed.
External cephalic version (ECV) can be carried out on most women, even if they have had one caesarean section before 2.
During an external cephalic version (ECV), obstetricians use their hands on the woman’s abdomen to gently try to turn the baby from the breech position to the head-down position. External cephalic version (ECV) involves applying gentle but firm pressure on your abdomen to help your baby turn in the uterus to lie head-first.
- A cardiotocograph (CTG), will monitor your baby’s wellbeing for 20-30 minutes before the procedure.
- A small needle will be inserted into your hand so that medication to relax your uterus can be administered directly into your vein.
- An obstetrician will then perform an ultrasound to confirm the position of the baby, and then attempt to turn the baby by pressing their hands firmly on your abdomen. Some women find this uncomfortable, while others don’t. The pressure on your abdomen lasts a few minutes. If the first attempt is unsuccessful, the obstetrician might try again.
- The CTG might be applied again after the procedure to assess your baby’s wellbeing before you leave.
- It usually takes about 3 hours from start to finish.
Relaxing the muscle of your uterus with medication has been shown to improve the chances of turning your baby 1. This medication is given by injection before the external cephalic version (ECV) and is safe for both you and your baby. It may make you feel flushed and you may become aware of your heart beating faster than usual but this will only be for a short time.
Before the external cephalic version (ECV) you will have an ultrasound scan to confirm your baby is breech, and your pulse and blood pressure will be checked. After the external cephalic version (ECV), the ultrasound scan will be repeated to see whether your baby has turned. Your baby’s heart rate will also be monitored before and after the procedure. You will be advised to contact the hospital if you have any bleeding, abdominal pain, contractions or reduced fetal movements after external cephalic version (ECV).
External cephalic version (ECV) is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labor. You do not need to make any preparations for your external cephalic version (ECV).
External cephalic version (ECV) can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the external cephalic version (ECV) and to have a blood test.
Figure 2. Turning a breech baby
Footnote: Counterclockwise external cephalic version (ECV). In case of engaged fetus, each hand takes one fetal pole and fetal buttocks pushed out of the maternal pelvis. Fetal head gently pushed toward direction of fetal face, counterclockwise in this figure.
[Source 4]External cephalic version contraindications
External cephalic version (ECV) should NOT be carried out if:
- you need a caesarean section for other reasons, such as placenta previa (a low-lying placenta after 20 weeks)
- you have had recent vaginal bleeding
- your baby’s heart rate tracing (also known as cardiotocography [CTG]) is abnormal
- your waters have broken
- you are pregnant with more than one baby (multiple pregnancy: having more than one baby).
Is external cephalic version safe for me and my baby?
External cephalic version (ECV) is generally safe with a very low complication rate 2. Overall, there does not appear to be an increased risk to your baby from having external cephalic version (ECV). After external cephalic version (ECV) has been performed, you will normally be able to go home on the same day.
- About 1 in 1,000 women go into labor after an external cephalic version (ECV).
- About 1 in 200 women need an immediate caesarean section.
When you do go into labor, your chances of needing an emergency caesarean section, forceps or vacuum (suction cup) birth is slightly higher than if your baby had always been in a head-down position 2.
Immediately after external cephalic version (ECV), there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat 2.
Is external cephalic version always successful?
External cephalic version (ECV) is successful for about 50% of women 2. It is more likely to work if you have had a vaginal birth before. Your healthcare team should give you information about the chances of your baby turning based on their assessment of your pregnancy.
If your baby does not turn then your healthcare professional will discuss your options for birth (see below). It is possible to have another attempt at external cephalic version (ECV) on a different day.
If external cephalic version (ECV) is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful external cephalic version (ECV) 2.
- Cluver C, Gyte GML, Sinclair M, Dowswell T, Hofmeyr GJ. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No.: CD000184. DOI: 10.1002/14651858.CD000184.pub4 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD000184.pub4/full[↩][↩][↩]
- Breech baby at the end of pregnancy. Royal College of Obstetricians & Gynaecologists. https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/breech-baby-patient-information-leaflet.pdf[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Cluver C, Hofmeyr GJ, Gyte GM, Sinclair M. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. The Cochrane database of systematic reviews. 2012;1:CD000184. doi:10.1002/14651858.CD000184.pub3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4171393/[↩]
- Kim M-Y, Park M-Y, Kim GJ. External cephalic version experiences in Korea. Obstetrics & Gynecology Science. 2016;59(2):85-90. doi:10.5468/ogs.2016.59.2.85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4796091/[↩]