What is breech birth
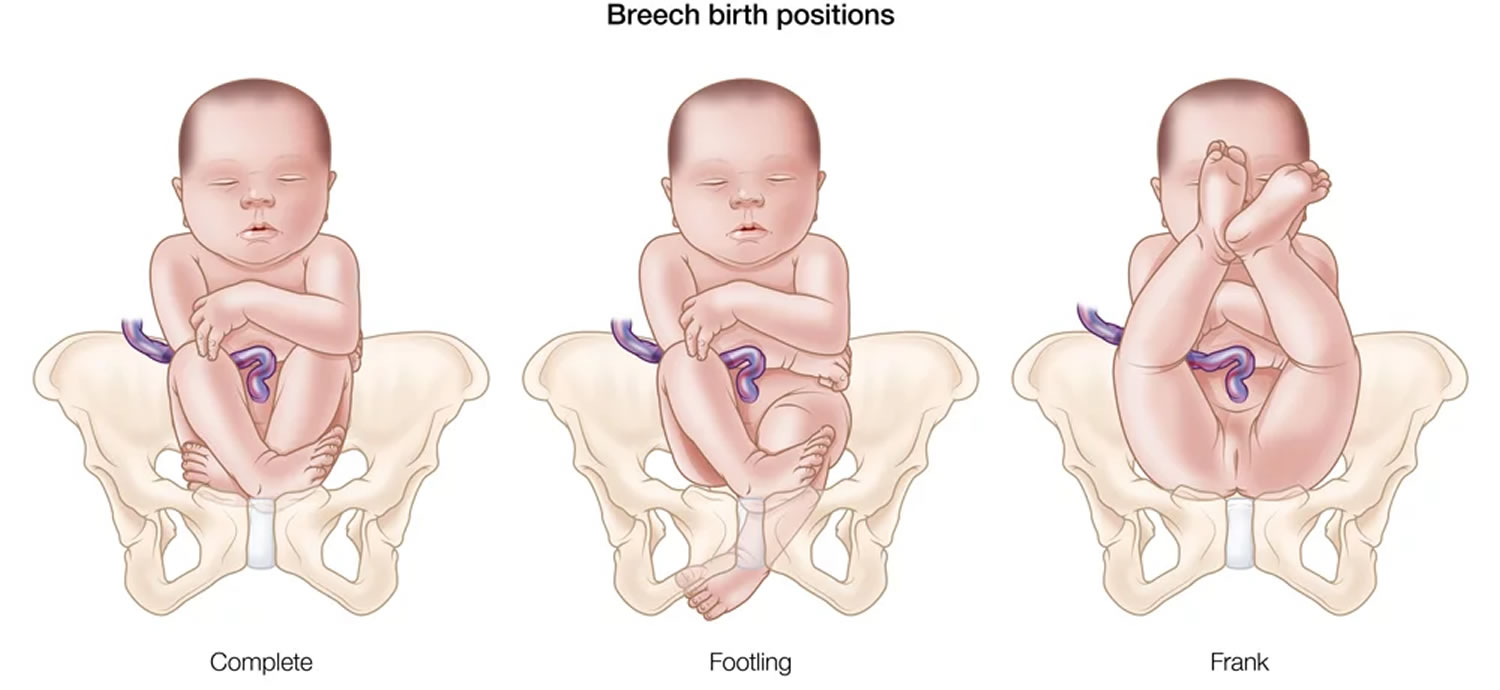
In breech birth or breech presentation, the baby’s bottom is down. In breech birth the baby is positioned to deliver feet or bottom first. There are a few types of breech 1:
- Complete breech means the baby is bottom-first, with knees bent.
- Frank breech means the baby’s legs are stretched up, with feet near the head.
- Footling breech means one leg is lowered over the mother’s cervix.
The danger of breech birth is mostly due to the fact that the largest part of a baby is its head. When the breech baby’s pelvis or hips deliver first, the woman’s pelvis may not be large enough for the head to be delivered also. This can result in a baby getting stuck in the birth canal, which can cause injury or death.
The umbilical cord may also be damaged or blocked. This can reduce the baby’s oxygen supply.
You are more likely to have a breech baby if you:
- Go into early labor
- Have an abnormally shaped uterus, uterine fibroids or too much amniotic fluid (polyhydramnios)
- Have more than one baby in your womb
- Have placenta previa (when the placenta is on the lower part of the uterine wall, blocking the cervix)
The best position for your baby inside your uterus at the time of delivery is head down. This position makes it easier and safer for your baby to pass through the birth canal.
In the last weeks of pregnancy, your doctor will check to see what position your baby is in.
If your baby’s position does not feel normal, you may need an ultrasound. If the ultrasound shows your baby is breech, your doctor will talk with you about your options for a safe delivery.
If your doctor determines that the baby cannot be turned through abdominal manipulation, you will need to have a cesarean delivery.
What are my choices during pregnancy?
If your baby is not in a head-down position after your 36th week, your doctor can explain your choices and their risks to help you decide what steps to take next.
Your doctor may offer to try to guide the baby into the right position. This is called external version or external cephalic version. It involves pushing on your belly while watching the baby on an ultrasound. The pushing may cause some discomfort.
Performed correctly, external cephalic version is safe and does not cause labor to begin. Your baby’s heart rate will be monitored before and after the external cephalic version. Like any medical procedure, complications can sometimes occur. To minimize these risks, an external cephalic version should be carried out in a place where the baby can be delivered by emergency caesarean section, if necessary. About one in 200 (0.5%) babies will need to be delivered by emergency caesarean section immediately after an external cephalic version because of bleeding from the placenta or changes in the baby’s heartbeat.
If your doctor tries to change your baby’s position, you may be given a medicine that relaxes the muscles of your uterus. You can also expect:
- An ultrasound to show your provider where the placenta and baby are located.
- Your doctor to push on your abdomen to try and turn your baby’s position.
- Your baby’s heartbeat to be monitored (also known as a CTG).
If external cephalic version is successful but your baby turns back into the breech position, or if external cephalic version is unsuccessful and your baby does not want to turn, it may be possible to have a second attempt on another day. If your baby does not turn after a second attempt, your obstetrician will discuss your options for birth.
Success is higher if your doctor tries this procedure at about 35 to 37 weeks. At this time, your baby is a little smaller, and there is most often more fluid around the baby. Your baby is also old enough in case there is a problem during the procedure that makes it necessary to deliver the baby promptly. This is rare. External version cannot be done once you are in active labor.
External cephalic version is not suitable for everyone and should not be carried out if:
- you need a caesarean section for other reasons
- you have had vaginal bleeding during the previous seven days
- the baby’s heart rate tracing (also known as a CTG) is not normal
- your uterus is not the normal (pear) shape
- your waters have broken before you go into labour
- you are expecting twins or more (except delivery of the last baby)
If you have had a previous cesarean section, external cephalic version can usually still be performed, however there are special considerations that need to be discussed with your doctor.
Risks are low for external cephalic version procedure when a skilled doctor does it. Rarely, it may lead to an emergency cesarean birth (C-section) if:
- Part of the placenta tears away from the lining of your womb
- Your baby’s heartbeat drops too low, which can happen if the umbilical cord is tightly wrapped around the baby.
Why do some babies remain in a breech position?
Often it is unclear why a baby remains in a breech position, however, some of the common reasons include:
- too much or too little amniotic fluid around the baby
- the length of the umbilical cord
- multiple pregnancy – for example, often one twin will be in a cephalic position and the other in a breech position
- uterine fibroids
- an irregular size or shape of the mother’s uterus
Can my baby still turn after 36 weeks?
Some breech babies turn themselves naturally in the last month of pregnancy. If this is your first baby and they are breech at 36 weeks, the chance of the baby turning itself naturally before you go into labor is about 1 in 8. If you’ve already had a baby and this one is breech at 36 weeks, the chance of them turning naturally is about 1 in 3.
If your baby is in a breech position at 36 weeks, your doctor or midwife might suggest you think about an external cephalic version, or external cephalic version, after 37 weeks. This will increase your chances of your baby turning to a head-down position.
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground. Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work.
Talk to your doctor or midwife before trying any techniques to be sure they do not harm you or your baby.
What are my choices for birth if the baby remains breech?
Depending on your situation, you may consider:
- planned cesarean section
- attempted vaginal birth
Most babies in the breech position at term are now delivered by cesarean section. However, with careful case selection and labor care, in a hospital with adequate experienced staff and resources, it is possible to plan for a vaginal breech birth in some cases.
This will depend upon your individual circumstances and the experience of the clinical team, and the facilities available. Sometimes the clinical team will not have sufficient experience to support a planned vaginal breech birth safely. In this case, you may discuss options for referral elsewhere.
There are benefits and risks associated with both cesarean delivery and vaginal breech birth and these should be discussed between you and your obstetrician or midwife, so that you can choose the best plan for you and your baby.
Vaginal breech birth
Your doctor will discuss with you whether you are suitable for a planned vaginal breech birth. There may be reasons specific to you or your baby that a planned vaginal breech birth is not advised.
Some of these reasons include:
- you have a narrow pelvis
- your baby is presenting as a footling breech
- your baby is large (>3800g)
- your baby is small (<2000g)
- other reasons preventing a vaginal birth, such as low lying placenta
- your doctor or hospital do not have the necessary skills and resources for a vaginal breech birth.
What can I expect in labor with a breech baby?
When you plan a vaginal breech birth your labor will be considered more complicated so you will be advised that your baby’s heart rate should be monitored continuously during labor and a pediatrician present at the birth. Vaginal breech birth is more complex, but not necessarily more difficult.
Your labor and pain relief options will be the same as with a baby who is head first.
If my baby doesn’t turn, will I have a C-section?
Most babies who remain breech after an attempt at turning them will be delivered by C-section. Your doctor will explain the risk of delivering a breech baby vaginally.
Today, the option to deliver a breech baby vaginally is not offered in most cases. The safest way for a breech baby to be born is by C-section.
If a C-section is planned, it will most often be scheduled for no earlier than 39 weeks. You will have an ultrasound at the hospital to confirm the position of your baby just before the surgery.
There is also a chance that you will go into labor or your water will break before your planned C-section. If that happens, call your provider right away and go to the hospital. It is important to go in right away if you have a breech baby and your bag of water breaks. This is because there is a higher chance that the umbilical cord will come out even before you are in labor. This can be very dangerous for the baby.
Because the cesarean is major surgery, it will take you longer to recover from this type of delivery than it would from a vaginal delivery. Depending on your condition, you will probably stay in the hospital from 2 to 4 days.
Once the anesthesia wears off, you will begin to feel the pain from the incisions, so be sure to ask for pain medicine. You might also experience gas pains and have trouble taking deep breaths. You will also have a vaginal discharge after the surgery due to the shedding of the uterine wall. The discharge will be red at first and then gradually change to yellow. Be sure to call your healthcare provider if you experience heavy bleeding or a foul odor from the vaginal discharge.
Alternative therapies
There are a number of alternative therapies that have been used to turn babies from a breech to a head-down position. These include postural exercises, acupuncture, moxibustion and chiropractic treatment.
There is no evidence to prove the effectiveness of alternative therapies. The American College of Obstetricians and Gynecologists will not endorse any techniques until they have been shown to be scientifically beneficial. You will need to consider if there are any risks associated with specific alternative therapies.
As with all treatments, medical or alternative, you must ask yourself three questions:
- Does this treatment work?
- Are there any risks to this treatment?
- Are the risks greater than any potential advantages of the treatment?
What causes a breech birth?
Breech presentation may be more common if you have:
- a low-lying placenta
- lax muscles of the uterus (usually due to having a number of babies)
- too much, or too little, amniotic fluid (waters) around the baby
- an uncommon shape of the uterus, or large fibroids
- previous breech presentation
- twins
If a baby is found to be in a breech position near the due date, an ultrasound will be performed to try to identify the reason. Most commonly though, no specific cause is found.
How is a breech birth diagnosed?
A few weeks prior to the due date, your health care provider will place her hands on your lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound to confirm the position.
Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Breech birth complications
If your baby is in a breech position near the due date, there is a greater chance of having a complicated vaginal birth or a cesarean section.
In some situations, with the right resources available, it can be safe to attempt a vaginal birth when the baby is in a breech position. However, there may be increased risks to the baby.
In other cases a cesarean section will be recommended, which also has risks for the mother and future pregnancies. You should discuss all the benefits and risks of both options when deciding what is right for you and your baby.
If your baby is still breech near the due date, the chances of it turning to a head down position without help are low. Attempts to encourage your baby to turn into the head first position may be part of the care which is offered to you.
Risks involved in a cesarean delivery
Like any surgery, a cesarean section involves some risks. These might include:
- Infection
- Loss of blood or need for a blood transfusion
- A blood clot that may break off and enter the bloodstream (embolism)
- Injury to the bowel or bladder
- A cut that might weaken the uterine wall
- Abnormalities of the placenta in subsequent pregnancies
- Difficulty becoming pregnant
- Risks from general anesthesia (if used)
- Fetal injury.
Breech baby complications after birth
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery. While your baby is still in the womb, it is just as safe for them to be in a breech position as it is for them to be head-down. There are no long-term effects upon children who were in a breech position during pregnancy. The birth process, however, is often more challenging when babies are still breech at the start of labor.
- Gray CJ, Shanahan MM. Breech Presentation. [Updated 2019 Mar 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448063[↩]