What is Pepto Bismol
Pepto-Bismol is an antacid and anti-diarrhea medication. Pepto-Bismol is used to treat diarrhea in adults and children 12 years of age and older. Pepto-Bismol is also used to relieve the symptoms of an upset stomach, such as heartburn, indigestion, and nausea in adults and children 12 years of age and older. The active ingredient in Pepto-Bismol is bismuth subsalicylate.
Pepto-Bismol is available without a prescription. However, if you are taking Pepto Bismol (bismuth subsalicylate) medicine for diarrhea, check with your doctor:
- if your symptoms do not improve within 2 days or if they become worse.
- if you also have a high fever.
Pepto Bismol (bismuth subsalicylate) is available in the following dosage forms:
- Suspension
- Tablet
- Tablet, Chewable
How does Pepto Bismol work?
Pepto Bismol (bismuth subsalicylate) is in a class of medications called antidiarrheal agents. It works by decreasing the flow of fluids and electrolytes into the bowel, reduces inflammation within the intestine, and may kill the organisms that can cause diarrhea.
Why does Pepto-Bismol sometimes darken the tongue/stool and how long does it last?
This discoloration is temporary and harmless. The active ingredient in Pepto-Bismol contains bismuth. When a small amount of bismuth combines with trace amounts of sulfur in your saliva and gastrointestinal tract, a black-colored substance (bismuth sulfide) is formed. This discoloration is temporary and harmless. It can last several days after you stop taking Pepto-Bismol. Individual bowel habits, your age (the intestinal tract slows down with age), and the amount of the product taken all help to determine how long Pepto-Bismol is in your system.
Can I give Pepto-Bismol to my child?
Pepto-Bismol is indicated only for adults and children 12 years and over. Use only as directed.
For children 2 years and older, Children’s Pepto Antacid (contains Calcium Carbonate 400 mg in each Children’s Pepto Antacid chewable tablet) can be used to relieve heartburn, acid indigestion, sour stomach, and upset stomach due to these symptoms. Note the difference between Children’s Pepto Antacid that contains Calcium Carbonate unlike the actual Pepto-Bismol that contains Bismuth subsalicylate. Subsalicylate is chemically related to aspirin; therefore, includes similar warning statements to aspirin.
I have been giving Pepto-Bismol to my child when he/she had an upset stomach – should I be concerned?
Pepto-Bismol is indicated only for adults and children 12 years and over. Use only as directed.
Pepto Bismol contains both bismuth and subsalicylate. Subsalicylate is chemically related to aspirin; therefore, includes similar warning statements. Hepatic injury has been reported with chronic therapeutic use 1. Salicylates have been linked with Reye’s syndrome in children. Hypoglycemia may develop, especially in children 1.
The acute ingestion of less than 150 mg/kg or 6.5 g of aspirin equivalent, whichever is less, is not expected to cause significant toxicity.
In young children, the initial respiratory alkalosis from salicylate intoxication is transient, they often have a predominant metabolic acidosis (and in severe cases also respiratory alkalosis) on presentation.
What does the label say about Reye’s syndrome and Pepto-Bismol?
Children and teenagers who have or are recovering from chicken pox or flu-like symptoms should not use Pepto-Bismol. When using this product, if changes in behavior with nausea or vomiting occur, consult a doctor because these symptoms could be an early sign of Reye’s syndrome, a rare but serious illness. Subsalicylate is chemically related to aspirin; therefore, includes similar warning statements.
How should Pepto Bismol be used?
Pepto Bismol (bismuth subsalicylate) comes as a liquid, tablet, or chewable tablet to be taken by mouth, with or without food. Follow the directions on the package carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take Pepto Bismol (bismuth subsalicylate) exactly as directed. Do not take more or less of it or take it more often than recommended by the manufacturer or your doctor.
Swallow the tablets whole; do not chew them.
Shake the liquid well before each use to mix the medication evenly.
If your symptoms get worse or if your diarrhea lasts longer than 48 hours, stop taking this medication and call your doctor.
Ask your doctor or pharmacist before taking other antacids or diarrhea medications together with Pepto Bismol (bismuth subsalicylate).
Should I take Pepto-Bismol with or without food?
Pepto-Bismol can be taken either with or without food. Use as directed for relief of travelers’ diarrhea, diarrhea or upset stomach due to overindulgence in food and drink, including: heartburn, indigestion, nausea, gas, belching and fullness.
When can I take Pepto-Bismol?
Pepto-Bismol is an upset stomach reliever and antidiarrheal product. It can be taken any time you are experiencing diarrhea, travelers’ diarrhea or an upset stomach due to overindulgence in food and drink, including: heartburn, indigestion, nausea, gas, belching and fullness. When using the product follow the directions. Do not exceed 8 doses in a 24 hour period when using Pepto-Bismol.
Before taking Pepto Bismol – Precautions
In deciding to use Pepto Bismol, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
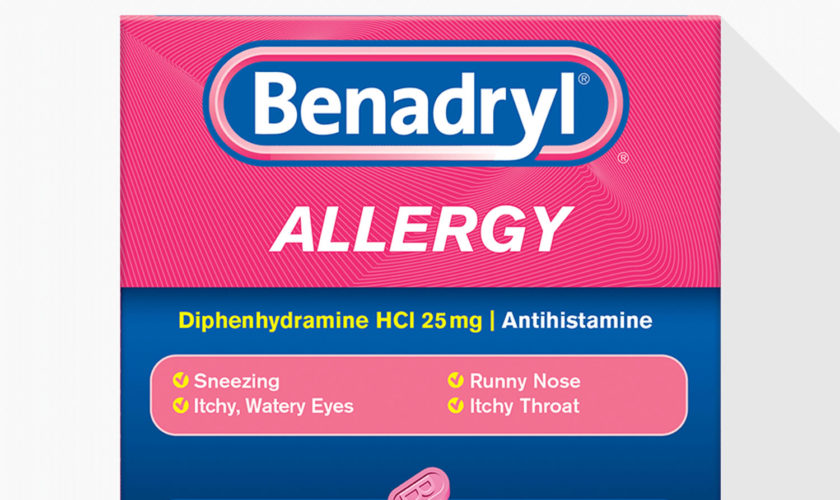
- tell your doctor or pharmacist if you are allergic to salicylate pain relievers such as aspirin, choline magnesium trisalicylate, choline salicylate (Arthropan), diflunisal (Dolobid), magnesium salicylate (Doan’s, others), and salsalate (Argesic, Disalcid, Salgesic); or any other medication.
- check the labels of all over-the-counter (OTC), nonprescription, and prescription medicines you now take. If any contain aspirin or other salicylates, be especially careful. Using other salicylate-containing products while taking Pepto Bismol (bismuth subsalicylate) may lead to overdose. If you have any questions about this, check with your health care professional or pharmacist.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking or plan to take. Be sure to talk to your doctor or pharmacist about taking Pepto Bismol (bismuth subsalicylate) if you take: anticoagulants (‘blood thinners’) such as warfarin (Coumadin); a daily aspirin; or medication for diabetes, arthritis or gout.
- if you are taking tetracycline antibiotics such as demeclocycline (Declomycin), doxycycline (Doryx, Vibramycin), minocycline (Dynacin, Minocin), and tetracycline (Sumycin), take them at least 1 hour before or 3 hours after taking Pepto Bismol (bismuth subsalicylate).
- ask your doctor before taking this medication if you have ever had an ulcer, bleeding problem, stools that are bloody or blackened, or kidney disease. Also ask your doctor before taking Pepto Bismol (bismuth subsalicylate) if you have a fever or mucus in your stool. If you will be giving Pepto Bismol (bismuth subsalicylate) to a child or teenager, tell the child’s doctor if the child has any of the following symptoms before he or she receives the medication: vomiting, listlessness, drowsiness, confusion, aggression, seizures, yellowing of the skin or eyes, weakness, or flu-like symptoms. Also tell the child’s doctor if the child has not been drinking normally, has had excessive vomiting or diarrhea, or appears dehydrated.
- ask your doctor about taking this medication if you are pregnant or are breast-feeding.
Use exactly as directed on the label, or as prescribed by your doctor. Do not use in larger or smaller amounts or for longer than recommended.
- Do not take more than 8 doses in one day (24 hours).
Shake the liquid medicine well just before you measure a dose. Measure the liquid with a special dose-measuring spoon or medicine cup, not with a regular table spoon. If you do not have a dose-measuring device, ask your pharmacist for one.
- The chewable tablet must be chewed before you swallow it.
Pepto Bismol (bismuth subsalicylate) can cause you to have a black or darkened tongue. This is a harmless side effect.
This medication can also cause unusual results with certain medical tests, thyroid scans, or stomach x-rays. Tell any doctor who treats you that you have recently taken Pepto Bismol (bismuth subsalicylate).
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Do not freeze.
Keep out of the reach of children. In case of Pepto Bismol overdose, call the Poison Control Helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help.
Overdose symptoms may include increased thirst, anxiety, muscle spasm, ringing in your ears, dizziness, confusion, severe headache, problems with speech or vision, severe stomach pain, or worsening diarrhea or vomiting.
Do not keep outdated medicine or medicine no longer needed.
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric patients
This medicine should NOT be used in children younger than 12 years of age. The fluid loss caused by diarrhea may result in a severe condition. In older children with diarrhea, medicine for diarrhea may be used, but it is also very important that a sufficient amount of liquids be given to replace the fluid lost by the body. If you have any questions about this, check with your health care professional.
Also, children are usually more sensitive to the effects of salicylates, especially if they have a fever or have lost large amounts of body fluid because of vomiting, diarrhea, or sweating.
The bismuth in Pepto Bismol may cause severe constipation in children.
In addition, do not use Pepto Bismol (bismuth subsalicylate) to treat nausea or vomiting in children or teenagers who have or are recovering from the flu or chickenpox. If nausea or vomiting is present, check with the child’s doctor immediately because this could be an early sign of Reye’s syndrome.
Geriatric patients
The fluid loss caused by diarrhea may result in a severe condition. For this reason, elderly persons with diarrhea should not take this medicine without first checking with their doctor. It is also very important that a sufficient amount of liquids be taken to replace the fluid lost by the body. If you have any questions about this, check with your health care professional.
Also, the elderly may be more sensitive to the effects of salicylates. This may increase the chance of side effects during treatment. In addition, the bismuth in this medicine may cause severe constipation in the elderly.
Breastfeeding
Studies in women breastfeeding have demonstrated harmful infant effects. An alternative to Pepto Bismol (bismuth subsalicylate) should be prescribed or you should stop breastfeeding while using Pepto Bismol (bismuth subsalicylate).
Diabetic patients
- False urine sugar test results may occur if you are regularly taking large amounts of bismuth subsalicylate or other salicylates.
- Smaller doses or occasional use of Pepto Bismol (bismuth subsalicylate) usually will not affect urine sugar tests. However, check with your health care professional (especially if your diabetes is not well-controlled) if:
- you are not sure how much salicylate you are taking every day.
- you notice any change in your urine sugar test results.
- you have any other questions about this possible problem
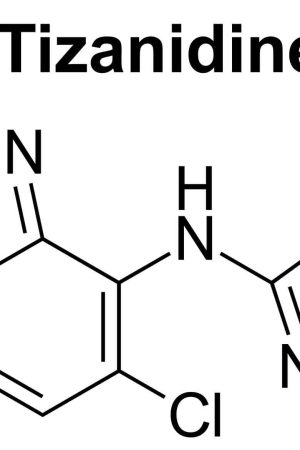
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking Pepto Bismol (bismuth subsalicylate), it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Ask a doctor or pharmacist if it is safe for you to use Pepto Bismol (bismuth subsalicylate) if you are also using any of the following drugs:
- a blood thinner such as warfarin (Coumadin, Jantoven);
- insulin or oral diabetes medications;
- probenecid (Benemid);
- an antibiotic such as doxycycline (Doryx, Oracea, Periostat, Vibramycin), minocycline (Dynacin, Minocin, Solodyn), or tetracycline (Ala-Tet, Brodspec, Panmycin, Sumycin, Tetracap);
- medication used to prevent blood clots, such as alteplase (Activase), tenecteplase (TNKase), urokinase (Abbokinase); or
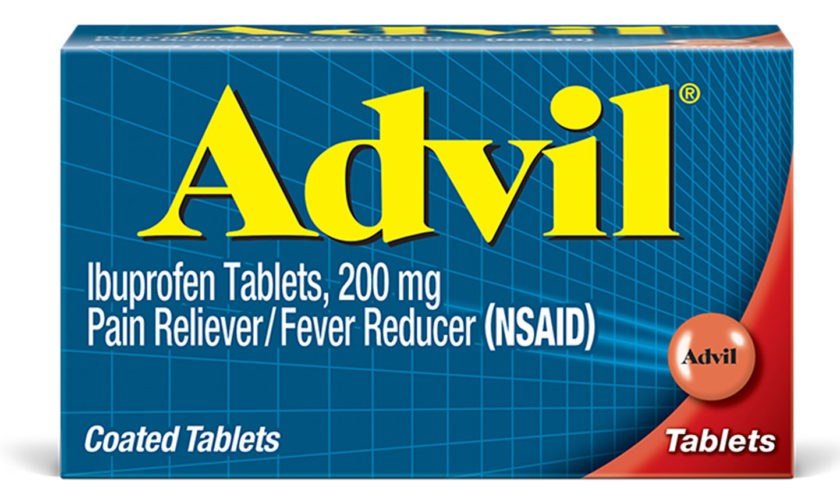
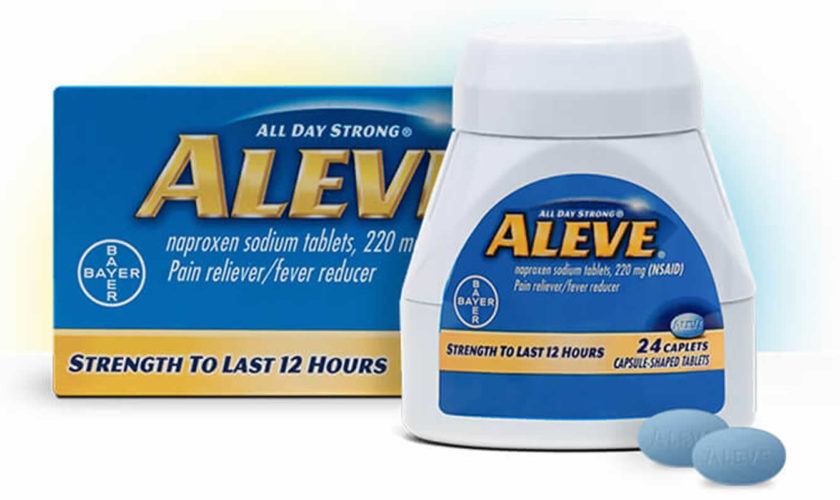
- other salicylates such as aspirin, Nuprin Backache Caplet, Kaopectate, KneeRelief, Pamprin Cramp Formula, Pepto-Bismol, Tricosal, Trilisate, and others.
Using Pepto Bismol (bismuth subsalicylate) with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Aceclofenac
- Acemetacin
- Amtolmetin Guacil
- Bromfenac
- Bufexamac
- Celecoxib
- Clonixin
- Dexibuprofen
- Dexketoprofen
- Diclofenac
- Digoxin
- Dipyrone
- Droxicam
- Etodolac
- Etofenamate
- Etoricoxib
- Felbinac
- Fenoprofen
- Fepradinol
- Feprazone
- Floctafenine
- Flufenamic Acid
- Flurbiprofen
- Ibuprofen
- Indomethacin
- Ketoprofen
- Lornoxicam
- Loxoprofen
- Lumiracoxib
- Meclofenamate
- Mefenamic Acid
- Meloxicam
- Morniflumate
- Nabumetone
- Naproxen
- Nepafenac
- Niflumic Acid
- Nimesulide
- Nimesulide Beta Cyclodextrin
- Oxaprozin
- Oxyphenbutazone
- Parecoxib
- Phenylbutazone
- Piketoprofen
- Piroxicam
- Proglumetacin
- Propyphenazone
- Proquazone
- Rofecoxib
- Sulindac
- Tenoxicam
- Tiaprofenic Acid
- Tolfenamic Acid
- Tolmetin
- Valdecoxib
Using Pepto Bismol (bismuth subsalicylate) with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Doxycycline
- Probenecid
- Sulfinpyrazone
- Tamarind
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your Pepto Bismol (bismuth subsalicylate) with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Dysentery—This condition may get worse; a different kind of treatment may be needed
- Gout—The salicylate in Pepto Bismol (bismuth subsalicylate) may worsen the gout and make the medicines taken for gout less effective
- Hemophilia or other bleeding problems—The salicylate in Pepto Bismol (bismuth subsalicylate) may increase the chance of bleeding
- Kidney disease—There is a greater chance of side effects because the body may be unable to get rid of the Pepto Bismol (bismuth subsalicylate)
- Stomach ulcer—Use of this medicine may make the ulcer worse
Pepto Bismol Pregnancy and Breastfeeding
Pepto Bismol Pregnancy Warnings
Safety has not been established during pregnancy; use is NOT recommended.
US FDA pregnancy category: Not assigned
Animal studies are inadequate. There are no controlled data in human pregnancy. Bismuth subsalicylate lacks reports of adverse fetal outcomes; however salicylates may cause congenital defects, increased perinatal mortality from ductus arteriosus in utero, intrauterine growth restriction, and salicylate intoxication.
US FDA pregnancy category Not Assigned: The US FDA has amended the pregnancy labeling rule for prescription drug products to require labeling that includes a summary of risk, a discussion of the data supporting that summary, and relevant information to help health care providers make prescribing decisions and counsel women about the use of drugs during pregnancy. Pregnancy categories A, B, C, D and X are being phased out.
Although the risk for toxicity may be small, significant fetal adverse effects have resulted from chronic exposure to salicylates Because of this, the use of bismuth subsalicyate during gestation should be restricted to the first half of pregnancy and then only in amounts that do not exceed the recommended doses 2.
Pepto Bismol Breastfeeding Warnings
Use is NOT recommended.
Excreted into human milk: Yes
The excretion of large amounts of bismuth obtained from bismuth subsalicylate into breast milk is not expected because of the poor absorption of bismuth into the systemic circulation. Salicylates, however, are excreted in milk and are eliminated more slowly from milk than from plasma with milk:plasma ratios, rising from 0.03-0.08 at 3 hours to 0.34 at 12 hours 2. Due to the potential for adverse effects in the nursing infant, the American Academy of Pediatrics recommends that salicylates should be used cautiously during breast feeding. A recent review also states that bismuth subsalicylate should be avoided during lactation because of systemic salicylate absorption.
Comments:
- Bismuth is not expected to appear in high concentrations in breast milk due to poor systemic absorption.
- Salicylates are excreted in breast milk.
What does Pepto Bismol do
Relieves travelers’ diarrhea, diarrhea and upset stomach due to over indulgence in food and drink including: heartburn, indigestion, nausea, gas, belching and fullness.
Pepto Bismol uses
Make certain your health care professional knows if you are on any special diet, such as a low-sodium or low-sugar diet.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
For safe and effective use of Pepto Bismol (bismuth subsalicylate):
- Follow your doctor’s instructions if Pepto Bismol (bismuth subsalicylate) was prescribed.
- Follow the manufacturer’s package directions if you are treating yourself.
For patients using Pepto Bismol (bismuth subsalicylate) to treat diarrhea:
- It is very important that the fluid lost by the body be replaced and that a proper diet be followed. For the first 24 hours you should drink plenty of clear liquids, such as ginger ale, decaffeinated cola, decaffeinated tea, broth, and gelatin. During the next 24 hours you may eat bland foods, such as cooked cereals, bread, crackers, and applesauce. Fruits, vegetables, fried or spicy foods, bran, candy, and caffeine and alcoholic beverages may make the diarrhea worse.
- If too much fluid has been lost by the body due to the diarrhea a serious condition may develop. Check with your doctor as soon as possible if any of the following signs of too much fluid loss occur:
- Decreased urination
- Dizziness and lightheadedness
- Dryness of mouth
- Increased thirst
- Wrinkled skin
If you are taking the oral suspension
- Use the dose cup that is included to measure out the right amount of Pepto Bismol (bismuth subsalicylate). If you are unsure, contact your doctor or pharmacist.
If you are taking the oral tablets
- Swallow the tablet whole with a glass of water. Do not crush or chew the tablet.
If you are taking the chewable tablets
- Chew up the tablet or allow it to completely disintegrate in your mouth before swallowing it.
Pepto Bismol Dosing
Pepto Bismol (bismuth subsalicylate) is used to treat diarrhea, nausea, heartburn, indigestion, and upset stomach.
Pepto Bismol (bismuth subsalicylate) should NOT be given to a child or teenager who has a fever, especially if the child also has flu symptoms or chicken pox. Salicylates can cause a serious and sometimes fatal condition called Reye’s syndrome in children.
You should not use Pepto Bismol (bismuth subsalicylate) if you have a stomach ulcer, a recent history of stomach or intestinal bleeding, or if you are allergic to salicylates such as aspirin, Doan’s Extra Strength, Salflex, Tricosal, and others.
- The dose of Pepto Bismol (bismuth subsalicylate) will be different for different patients. Follow your doctor’s orders or the directions on the label. The following information includes only the average doses of Pepto Bismol (bismuth subsalicylate). If your dose is different, do not change it unless your doctor tells you to do so.
The amount of Pepto Bismol (bismuth subsalicylate) that you take depends on the strength of the Pepto Bismol (bismuth subsalicylate) medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
For oral dosage form (Pepto Bismol suspension):
- For diarrhea or upset stomach:
- Adults and children 12 years of age and older—The usual dose is 2 tablespoonfuls every half-hour to one hour if needed. You should not take more than 16 tablespoonfuls of the regular-strength suspension or 8 tablespoonfuls of the concentrate in twenty-four hours.
- Children under 12 years—Should NOT be used in children younger than 12 years of age.
For oral dosage forms (Pepto Bismol tablets or chewable tablets):
- For diarrhea or upset stomach:
- Adults and children 12 years of age and older—The usual dose is 2 tablets every half-hour to one hour. You should not take more than 16 tablets in twenty-four hours.
- Children under 12 years—Should NOT be used in children younger than 12 years of age.
Usual Adult Dose for Dyspepsia
524 mg orally every 30 to 60 minutes as needed not to exceed 8 doses in any 24 hour period.
Alternatively, 1048 mg to 1050 mg may be given orally every hour not to exceed 4 doses in any 24 hour period.
Comments:
- Use until diarrhea stops but not longer than 2 days.
- Pepto Bismol (bismuth subsalicylate) may be useful in the prevention of traveler’s diarrhea during periods of risk. The duration of use for traveler’s diarrhea should not exceed approximately 3 weeks.
- -Shake liquid formulations well before using.
Usual Adult Dose for Traveler’s Diarrhea
524 mg orally every 30 to 60 minutes as needed not to exceed 8 doses in any 24 hour period.
Alternatively, 1048 mg to 1050 mg may be given orally every hour not to exceed 4 doses in any 24 hour period.
Comments:
- Use until diarrhea stops but not longer than 2 days.
- Pepto Bismol (bismuth subsalicylate) may be useful in the prevention of traveler’s diarrhea during periods of risk. The duration of use for traveler’s diarrhea should not exceed approximately 3 weeks.
- Shake liquid formulations well before using.
Usual Adult Dose for Diarrhea
524 mg orally every 30 to 60 minutes as needed not to exceed 8 doses in any 24 hour period.
Alternatively, 1048 mg to 1050 mg may be given orally every hour not to exceed 4 doses in any 24 hour period.
Comments:
- Use until diarrhea stops but not longer than 2 days.
- Pepto Bismol (bismuth subsalicylate) may be useful in the prevention of traveler’s diarrhea during periods of risk. The duration of use for traveler’s diarrhea should not exceed approximately 3 weeks.
- Shake liquid formulations well before using.
Usual Adult Dose for Helicobacter pylori Infection
524 mg orally 4 times a day.
Usual Pediatric Dose for Diarrhea
Non-specific diarrhea:
- <3 years: Ask your doctor
- 3 to 6 years: Use with caution, 87 mg every 30 minutes to 1 hour as needed.
- 6 to 9 years: Use with caution, 175 mg every 30 minutes to 1 hour as needed.
- 9 to 12 years: Use with caution, 262 mg every 30 minutes to 1 hour as needed.
Usual Pediatric Dose for Chronic Diarrhea
Chronic Infantile Diarrhea:
- 2 to 24 months: Use with caution, 44 mg every 4 hours
- 24 to 48 months: Use with caution, 87 mg every 4 hours
- 48 to 70 months: Use with caution, 175 mg every 4 hours
Usual Pediatric Dose for Helicobacter pylori Infection
Dosage in children with Helicobacter Pylori Infection is not well established, the following doses have been used in conjunction with ampicillin and metronidazole.
- <= 10 years: 262 mg four times a day for six weeks
- > 10 years: 524 mg four times a day for six weeks
Renal Dose Adjustments
- Data not available
Liver Dose Adjustments
- Data not available
Dialysis
- Data not available
What should I do if I forget a dose?
Pepto Bismol (bismuth subsalicylate) is usually taken as needed. If your doctor has told you to take Pepto Bismol (bismuth subsalicylate) regularly, take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
What special dietary instructions should I follow?
Drink plenty of water or other beverages to replace fluids that you may have lost while having diarrhea.
Unless your doctor tells you otherwise, continue your normal diet.
What should I do if I forget a dose?
This medication is usually taken as needed. If your doctor has told you to take bismuth subsalicylate regularly, take the missed dose as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Pepto Bismol dosage
Pepto Bismol Liquid
Active Ingredient: Bismuth Subsalicylate 525 mg in each 30 ml dose
Inactive Ingredients: Benzoic Acid, D&C Red No. 22, D&C Red No. 28, Flavor, Gellan Gum, Magnesium Aluminum Silicate, Methylcellulose, Salicylic Acid, Sodium Salicylate, Sorbic Acid, Sucralose, Water
Storage Instructions
- Protect from freezing. Avoid excessive heat (over 104°F or 40°C).
Pepto Bismol Liquid Usage Warning
Reye’s syndrome: Children and teenagers who have or are recovering from chicken pox or flu-like symptoms should not use this product. When using this product, if changes in behavior with nausea and vomiting occur, consult a doctor because these symptoms could be an early sign of Reye’s syndrome, a rare but serious illness.
Allergy alert: Contains salicylate. Do not take if you are allergic to salicylates (including aspirin), taking other salicylate products.
Do not use if you have an ulcer, a bleeding problem, bloody or black stool. Ask a doctor before use if you have: fever, mucus in the stool.
Ask a doctor or pharmacist before use if you are taking any drug for: anticoagulation (thinning the blood), diabetes, gout, arthritis. When using this product a temporary, but harmless, darkening of the stool and/or tongue may occur.
Stop use and ask a doctor if: symptoms get worse or last more than 2 days.
Pepto Bismol Liquid directions of use
- Shake well before use.
- Only use dose cup provided.
Pepto Bismol Liquid Dosage
- Adults and children 12 years and over:
- 30 mL (1 dose) every ½ hour or 60 mL (2 doses) every hour as needed for diarrhea/traveler’s diarrhea. Use until diarrhea stops but not more than 2 days. Drink plenty of clear fluids to help prevent dehydration caused by diarrhea.
- 30 mL (1 dose) every ½ hour as needed for overindulgence (upset stomach, heartburn, indigestion, nausea).
- Do not exceed 8 doses (240 mL) in 24 hours.
- Children under 12 years: ask a doctor.
Pepto-Bismol Swallowable Caplets
Active Ingredient: Bismuth Subsalicylate 262 mg in each caplet
Inactive Ingredients: Calcium Carbonate, Magnesium Stearate, Mannitol, Microcrystalline Cellulose, Polysorbate 80, Povidone, D&C Red No. 27 Aluminum Lake, Silicon Dioxide, Sodium Starch Glycolate
Storage Instructions
- Avoid excessive heat (over 104°F or 40°C)
Pepto-Bismol Swallowable Caplets Usage Warning
Reye’s syndrome: Children and teenagers who have or are recovering from chicken pox or flu-like symptoms should not use this product. When using this product, if changes in behavior with nausea and vomiting occur, consult a doctor because these symptoms could be an early sign of Reye’s syndrome, a rare but serious illness.
Allergy alert: Contains salicylate. Do not take if you are allergic to salicylates (including aspirin), taking other salicylate products.
Do not use if you have an ulcer, a bleeding problem, bloody or black stool. Ask a doctor before use if you have: fever, mucus in the stool.
Ask a doctor or pharmacist before use if you are taking any drug for: anticoagulation (thinning the blood), diabetes, gout, arthritis. When using this product a temporary, but harmless, darkening of the stool and/or tongue may occur.
Stop use and ask a doctor if: symptoms get worse or last more than 2 days.
Pepto-Bismol Swallowable Caplets directions of use
- Swallow whole with water, do not chew.
Pepto-Bismol Swallowable Caplets Dosage
- Adults and children 12 years and over:
- 2 caplets (1 dose) every ½ hour or 4 caplets (2 doses) every hour as needed for diarrhea. Use until diarrhea stops but not more than 2 days. Drink plenty of clear fluids to help prevent dehydration caused by diarrhea.
- 2 caplets (1 dose) every ½ hour as needed for overindulgence (upset stomach, heartburn, indigestion, nausea).
- Do not exceed 8 doses (16 caplets) in 24 hours.
- Children under 12 years: ask a doctor.
Pepto-Bismol Original Chewable Tablets
Active Ingredient: Bismuth Subsalicylate 262 mg in each chewable tablet
Inactive Ingredients: Calcium Carbonate, Flavor, Magnesium Stearate, Mannitol, Povidone, D&C Red No. 27, Saccharin Sodium, Talc
Storage Instructions
- Avoid excessive heat (over 104°F or 40°C)
Pepto-Bismol Original Chewable Tablets Usage Warning
Reye’s syndrome: Children and teenagers who have or are recovering from chicken pox or flu-like symptoms should not use this product. When using this product, if changes in behavior with nausea and vomiting occur, consult a doctor because these symptoms could be an early sign of Reye’s syndrome, a rare but serious illness.
Allergy alert: Contains salicylate. Do not take if you are allergic to salicylates (including aspirin), taking other salicylate products.
Do not use if you have an ulcer, a bleeding problem, bloody or black stool. Ask a doctor before use if you have: fever, mucus in the stool.
Ask a doctor or pharmacist before use if you are taking any drug for: anticoagulation (thinning the blood), diabetes, gout, arthritis. When using this product a temporary, but harmless, darkening of the stool and/or tongue may occur.
Stop use and ask a doctor if: symptoms get worse or last more than 2 days.
Pepto-Bismol Original Chewable Tablets directions of use
- Chew or dissolve in mouth.
Pepto-Bismol Original Chewable Tablets Dosage
- Adults and children 12 years and over:
- 2 tablets (1 dose) every ½ hour or 4 tablets (2 doses) every hour as needed for diarrhea. Use until diarrhea stops but not more than 2 days. Drink plenty of clear fluids to help prevent dehydration caused by diarrhea.
- 2 tablets (1 dose) every ½ hour as needed for overindulgence (upset stomach, heartburn, indgestion and nausea).
- Do not exceed 8 doses (16 tablets) in 24 hours.
- Children under 12 years: ask a doctor.
Children’s Pepto Antacid
Active Ingredient: Calcium Carbonate 400 mg in each Children’s Pepto Antacid chewable tablet
Inactive Ingredients: D&C Red No.27 Aluminum Lake, Flavor, Magnesium Stearate, Mannitol, Povidone, Sorbitol, Sugar, Talc
Storage Instructions
- Do not exceed 25°C. Preserve in well-closed containers.
Children’s Pepto Antacid Chewable Tablets Usage Warning
Ask a doctor or pharmacist before use if the child is presently taking a prescription drug. Antacids may interact with certain prescription drugs. Stop use and ask a doctor if symptoms last more than two weeks. Keep this and all drugs out of the reach of children.
Children’s Pepto Antacid Chewable Tablets directions of use
Ask a doctor or pharmacist before use.
Children’s Pepto Antacid Chewable Tablets Dosage
Find the right dose on the chart below based on weight (preferred). Otherwise, use age. Repeat dose as needed. Do not take more than 3 tablets (ages 2-5) or 6 tablets (ages 6-11) in a 24-hour period, or use the maximum dosage for more than two weeks, except under the advice and supervision of a doctor.
- Under 24 lbs or under 2 years: Ask a doctor
- 24-47 lbs or 2-5 years: 1 Children’s Pepto Antacid tablet
- 48-95 lbs or 6-11 years: 2 Children’s Pepto Antacid tablets
- Do not take more than 3 tablets (ages 2-5) or 6 tablets (ages 6-11) in a 24-hour period.
Pepto Bismol side effects
Along with Pepto Bismol (bismuth subsalicylate) needed effects, Pepto Bismol (bismuth subsalicylate) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Common side effects include:
- constipation
- dark colored stools
- black or darkened tongue.
Check with your doctor immediately if any of the following side effects occur:
In some patients Pepto Bismol (bismuth subsalicylate) may cause dark tongue and/or grayish black stools. This is only temporary and will go away when you stop taking this medicine.
Pepto Bismol side effects
- anxiety
- any loss of hearing
- confusion
- constipation (severe)
- diarrhea (severe or continuing)
- difficulty in speaking or slurred speech
- dizziness or lightheadedness
- drowsiness (severe)
- fast or deep breathing
- headache (severe or continuing)
- increased sweating
- increased thirst
- mental depression
- muscle spasms (especially of face, neck, and back)
- muscle weakness
- nausea or vomiting (severe or continuing)
- ringing or buzzing in ears (continuing)
- stomach pain (severe or continuing)
- trembling
- uncontrollable flapping movements of the hands (especially in elderly patients) or other uncontrolled body movements
- vision problems
Nervous system
- Rare (less than 0.1%): Myoclonic encephalopathy
- Frequency not reported: Weakness, fatigue, depression, anxiety, irritability, insomnia, unsteady gait, motor incoordination, loss of memory, jerky movements, mental confusion, disorientation, difficulty in walking and speaking, tremor, myoclonic jerks, incontinence
Nervous system toxicity is a common feature of bismuth toxicity. Bismuth toxicity is characterized by the insidious onset of weakness and fatigue, depression, anxiety, irritability, insomnia, unsteady gait, motor incoordination, loss of memory, and jerky movements. Acute toxicity may result in the development of mental confusion, disorientation, difficulty in walking and speaking, tremor, myoclonic jerks, and incontinence.
Myoclonic encephalopathy has occurred in patients who have ingested bismuth for several months to years, but the incidence is very rare. Recovery of patients from bismuth encephalopathy may take several months following discontinuation of use. Bismuth encephalopathy has generally been reported in patients ingesting salts other than subsalicylate.
Other
Salicylism has been reported in patients who chronically ingest bismuth subsalicylate (the active ingredient contained in Pepto-Bismol). Common complaints include vertigo, diminished hearing, lethargy, CNS (central nervous system) dysfunction, confusion, tinnitus, vomiting, and abdominal pain. Patients may present with respiratory alkalosis and metabolic acidosis, azotemia, and hypoprothrombinemia and platelet dysfunction. The elderly may be particularly vulnerable to the development of salicylism.
Frequency not reported: Salicylism
Gastrointestinal
- Very common (10% or more): Black stool
- Common (1% to 10%): Black tongue
- Frequency not reported: Nausea, vomiting
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Some side effects can be serious.
If you experience this symptom, stop taking this medication and call your doctor immediately:
- ringing or buzzing in your ear(s)
- diarrhea lasting longer than 2 days
- worsened stomach symptoms.
Pepto Bismol (bismuth subsalicylate) may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Human Toxicity Reports
Six examples of poisoning by bismuth subsalicylate were reported 3 arising from treatment of syphilis involving the simultaneous occurrence of stomatitis and albuminuria. The study author noted that bismuth tended to be mobilized during acidosis and advised caution in administration of bismuth to patients subject to acidosis 3.
A case was described in which encephalopathy occurred in a 60 year old man that was attributed to use of bismuth subsalicylate for diarrhea 4. The diagnosis was supported by an electroencephalogram and a blood bismuth level of 72 uG/L. The patient recovered completely within one month after the drug was discontinued 4.
Inorganic bismuth salts, formed from metabolism of bismuth subsalicylate in the gastrointestinal tract, apparently present little or no risk to the fetus from normal therapeutic doses, but the data available for bismuth in pregnancy are poor, and the actual fetal risk cannot be determined 2. On the other hand, the potential actions of salicylate on the fetus are complex. Although the risk for toxicity may be small, significant fetal adverse effects have resulted from chronic exposure to salicylates. Because of this, the use of bismuth subsalicyate during gestation should be restricted to the first half of pregnancy and then only in amounts that do not exceed the recommended doses 2.
Bioavailability of doxycycline was significantly reduced by 37% and 51% respectively, when bismuth subsalicylate was given simultaneously and as a multiple dose regimen before doxycycline. Bismuth subsalicylate should not be taken when doxycycline is used for therapeutic purposes. The study authors suggest travelers should not take these agents together to prevent diarrhea 5.
Pepto Bismol overdose
In case of Pepto Bismol overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your emergency services number.
Moderately toxic and probable oral lethal dose in human is 500mg to 5,000mg per kg body weight for a 70 kg (150 lb) person 6.
If you think that you or anyone else may have taken a Pepto Bismol overdose, get emergency help at once. Taking an overdose of Pepto Bismol (bismuth subsalicylate) may cause unconsciousness or death. Signs of overdose include convulsions (seizures), hearing loss, confusion, ringing or buzzing in the ears, severe drowsiness or tiredness, severe excitement or nervousness, and fast or deep breathing.
- BISMUTH SUBSALICYLATE. https://toxnet.nlm.nih.gov/cgi-bin/sis/search2/f?./temp/~nTtVSk:1[↩][↩]
- Briggs, G.G, R.K. Freeman, S.J. Yaffe. A Reference Guide to Fetal and Neonatal Risk. Drugs in Pregnancy and Lactation. 4th ed. Baltimore, MD: Williams & Wilkins 1994., p. 96[↩][↩][↩][↩]
- Hayes, W.J., Jr., E.R. Laws, Jr., (eds.). Handbook of Pesticide Toxicology. Volume 2. Classes of Pesticides. New York, NY: Academic Press, Inc., 1991., p. 543[↩][↩]
- HASKING GJ, DUGGAN JM; MED J AUST 2 (AUG 21): 167;1982[↩][↩]
- Influence of Subsalicylate Bismuth on Absorption of Doxycycline; JAMA 247 (16): 2266; 1982 https://jamanetwork.com/journals/jama/article-abstract/371748[↩]
- Gosselin, R.E., H.C. Hodge, R.P. Smith, and M.N. Gleason. Clinical Toxicology of Commercial Products. 4th ed. Baltimore: Williams and Wilkins, 1976., p. II-93[↩]