What is chromhidrosis
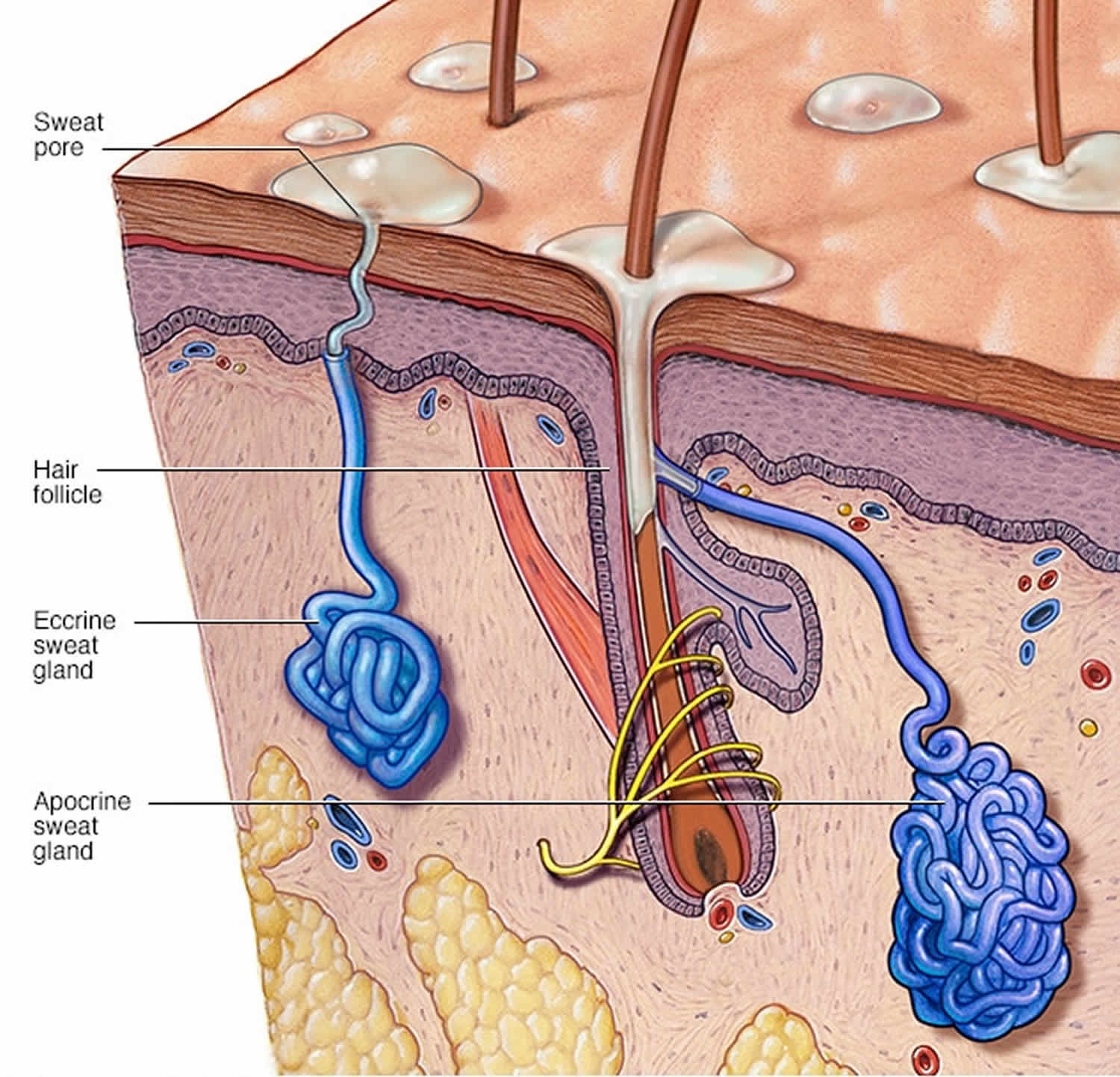
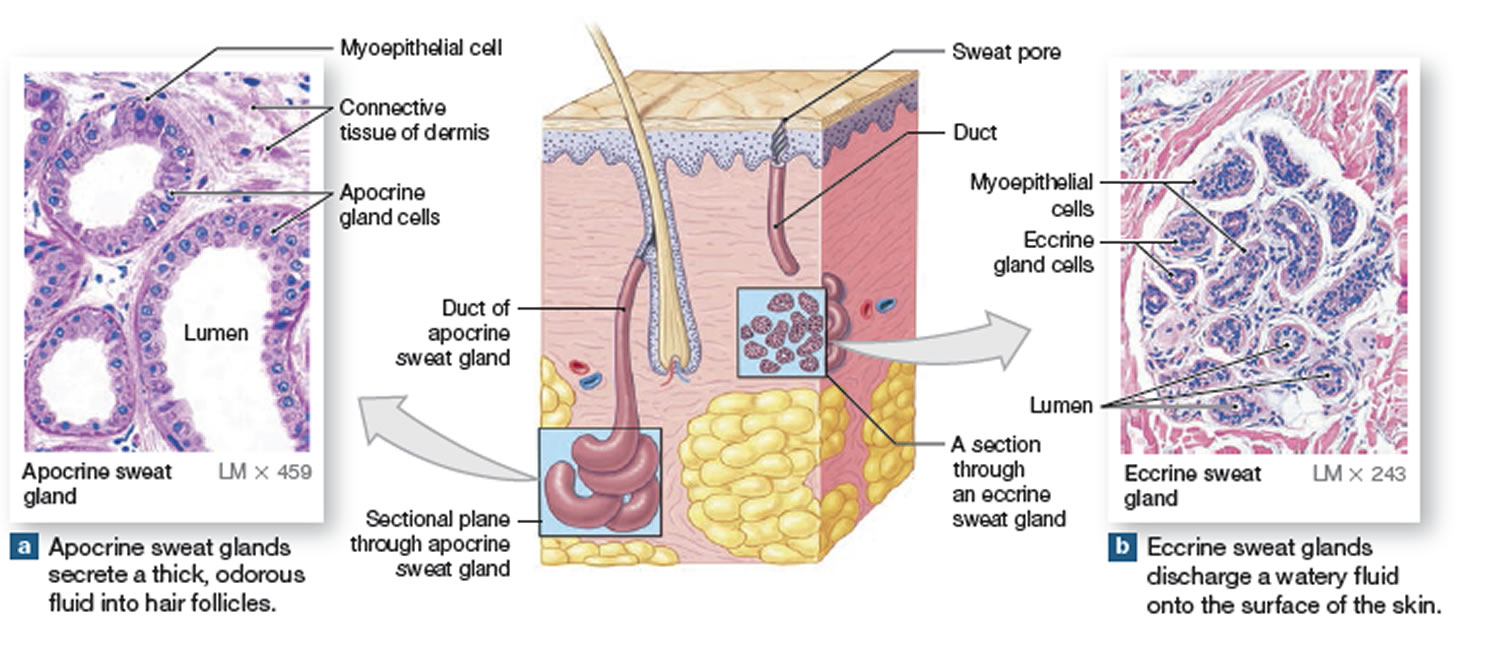
Chromhidrosis is a rare condition characterized by secretion of colored sweat from eccrine and apocrine sweat glands 1. Eccrine sweat glands secrete a clear, odorless fluid that serves to regulate body temperature. Apocrine sweat glands secrete a thick, milky sweat that, once broken down by bacteria, is the main cause of body odor. Chromhidrosis can be caused by various agents such as coloring agents used as food additives.
Normally, apocrine sweat glands secrete scant amounts of odorless, oily fluid into the hair canal that, upon reaching the skin surface, is degraded by bacteria producing a pheromonal body odor 2.
Chromhidrosis can subdivide into three categories 3:
- Apocrine chromhidrosis: Apocrine chromhidrosis occurs in the areas where apocrine glands are present and are mostly limited to the anogenital and axillary areas, eyelids, ears, scalp, trunk, and areola. Although apocrine glands are found in the genital, axillary, areolar, and facial skin, chromhidrosis is reported only on the face 4, armpits 5 and breast areola 6. Lipofuscin pigment is responsible for the colored sweat. This pigment is produced in the apocrine gland, and its various oxidative states account for the characteristic yellow, green, blue, or black secretions observed in apocrine chromhidrosis. Apocrine chromhidrosis appears to be more common in blacks than in whites, but facial chromhidrosis is described only in whites.
- Eccrine chromhidrosis: Eccrine chromhidrosis is rare and occurs with ingestion of certain dyes or drugs. Eccrine chromhidrosis may occur almost anywhere on the body as eccrine glands are distributed with varying density throughout the skin except for the ear canal, lips, prepuce, glans penis, clitoris, and labia minora. Eccrine glands are smaller than apocrine glands, secrete a dilute salty sweat composed mainly of water and electrolytes directly onto the skin surface, and are innervated by the sympathetic nervous system. They are irregularly spaced on the epidermal ridges of the pads of the digits; however, there are no pores within the furrows. They are involved in thermoregulation, protection of the skin barrier, and excretion of electrolytes 3.
- Pseudochromhidrosis (pseudo-eccrine chromhidrosis): Pseudochromhidrosis results from the interaction of colorless eccrine sweat with extrinsic dyes, paints, or chromogenic bacteria, subsequently producing a colored sweat 7.
The yellow, green, and blue apocrine secretions produce a yellow fluorescence under a Wood lamp (UV 360 nm), whereas the dark brown and black apocrine secretions seldom autofluoresce. Substance P is also postulated to be an important neurotransmitter in this process.
Several extrinsic causes of eccrine chromhidrosis and pseudochromhidrosis include chromogenic bacteria, especially Corynebacterium species, fungi, dyes, drugs, and chemical contactants 8.
Apocrine chromhidrosis may appear at any age but usually appears after puberty, when the apocrine secretory function begins. However, rare cases in infants have been reported 9. The disease is considered chronic, however, may regress with age as apocrine secretion diminishes 3. Apocrine chromhidrosis displays no occupational or geographical predisposition and is not influenced by climatic or seasonal variation 10. There is no gender predilection, but chromhidrosis has been reported in the literature more commonly in blacks, barring facial chromhidrosis, which has been reported more commonly in whites 3. However, there are too few patients reported to draw meaningful conclusions 11.
Approximately 10% of people without chromhidrosis have colored sweat that is regarded as acceptable and within the normal range 12.
While there are no complications directly associated with chromhidrosis, there may be implications secondary to psycho-social issues 13.
Figure 1. Sweat glands
Figure 2. Sweat glands anatomy
Figure 3. Chromhidrosis
Chromhidrosis causes
Three subtypes of chromhidrosis have been described by Cilliers and de Beer 14:
- Apocrine chromhidrosis:
- True eccrine chromhidrosis,
- Pseudo-eccrine chromhidrosis.
Several extrinsic causes of eccrine chromhidrosis and pseudochromhidrosis include chromogenic bacteria, especially Corynebacterium species, fungi, dyes, drugs, and chemical contactants 8.
Apocrine chromhidrosis is seen after puberty, usually confined to face and axilla, rarely areola. It is often noticed by patients as yellow, blue, green, and blue-black staining of the underclothing, which depends on the level of oxidation of the lipofuscin granules in the apocrine glands. Lipofuscin is a yellowish brown pigment that is normally found in the cytoplasm of relatively nondividing cells (eg, neurons). In chromhidrosis, lipofuscins are found in a higher-than-normal concentration or a higher-than-normal state of oxidation in apocrine glands. However, why some glands experience these changes is unclear. This increased level of oxidation results in the green, blue, and even black sweat seen in chromhidrosis. The yellow, green, and blue apocrine secretions produce a yellow fluorescence under a Wood lamp (UV 360 nm), whereas the dark brown and black apocrine secretions seldom autofluoresce. Substance P is also postulated to be an important neurotransmitter in this process.
Tyrosine, melanin, and heme breakdown products are also implicated as the color-producing molecules 15. Under light microscopy using hematoxylin-eosin staining, yellow-brown lipofuscin granules may be present and autofluorescence may be noted at 360 nm in nonstained paraffin-embedded sections, skin, and stained clothes 1.
Pseudo-eccrine chromhidrosis occurs when the colorless sweat gets colored on reaching the skin on reaction with exogenous chromogenic bacterial products such as Corynebacterium, piedraia, bacillus species, chemicals, paints, and dyes 16.
True eccrine chromhidrosis is a less common generalized disorder mostly caused by coloring of the clear eccrine sweat by dyes, pigments, or metals 1. Hurley and Wilkowski 17 found that dyes from quinine and imine groups are readily excreted by eccrine glands in a sufficient concentration to be readily visualized.
As per the available literature, the causes of eccrine chromhidrosis can be classified as follows 18:
- Exogenous: Due to ingestion of the drugs containing quinines 1, dyes such as tartrazine 19, coloring/flavoring agents present in food products 14 and heavy metals such as copper 20.
- Endogenous: Due to hyperbilirubinemia associated with liver disorders. Patients present with greenish discoloration of palms and soles with or without pompholyx-like lesions. The brown-colored water-soluble direct bilirubin is said to be secreted through the eccrine glands and converted into green-colored biliverdin by an oxidative process and hence giving rise to green-colored sweat 21.
Familial chromhidrosis has been reported 22.
Chromhidrosis symptoms
Chromhidrosis is a rare condition characterized by secretion of colored sweat from eccrine and apocrine sweat glands 1. Patients with chromhidrosis will present with colored sweat, with or without staining of their clothing. Some patients may describe warmth or a prickly sensation upon emotional or physical stress preceding the appearance of colored sweat 7.
Quantities of apocrine sweat are less than those of eccrine sweat. Usually, patients report axillary staining of their undershirt, staining of their bra 23 or, less frequently, staining of the face or areola. Yellow is the most common color of axillary staining. An aura of warmth or a prickly sensation prompted by emotional or physical stimuli may precede the onset of colored sweat. Facial apocrine chromhidrosis is rarely described. It occurs most frequently on the cheeks and malar eminences. The secretion can often be expressed mechanically 24.
Chromhidrosis diagnosis
The initial assessment should include a detailed history of the patient’s environment and lifestyle to exclude exogenous causes, including any new medications, started before the onset of chromhidrosis, including vitamins, supplements, and herbal medications 13.
While chromhidrosis is a clinical diagnosis, further studies may be needed to ascertain the type and cause of chromhidrosis if not apparent from the history and physical examination. A Wood’s lamp examination of colored sweat may be positive and will fluoresce green, blue, and yellow apocrine gland secretions yellow, while black and dark brown secretions usually do not fluoresce. If no sweat is produced at the time of the test, manual expression or pharmacologic stimulation with intradermal epinephrine or oxytocin (Pitocin) can be used to stimulate sweat secretion. Clothing fibers in contact with the secretions may also fluoresce yellow-green with standard UV microscopy 25.
Skin biopsies can be sent for hematoxylin/eosin staining and fluorescence microscopy to detect and measure lipofuscins within apocrine glands 7.
Cytological examination of secretion smears may aid in detecting lipofuscin pigment within apocrine gland cells. Spectrophotometer analysis of samples from sweat, sebum, urine, skin scrapings, and extraction samples from clothing can help to aid in the diagnosis 13. Bacterial and fungal cultures of the skin may be an option to rule out pseudochromhidrosis 26. Other studies may be necessary to rule out other causes of pigmentation and include complete blood cell counts to rule out a bleeding diathesis and urinary homogentisic acid level to exclude alkaptonuria 7.
On careful inspection, the following signs can often be observed in chromhidrosis:
- An odorless yellow, green, blue, brown, or black and turbid secretion that can be manually expressed from apocrine-bearing skin
- Staining that is accentuated in the follicular orifices and pores
- Glistening, adherent, deeply colored flecks that appear as the secretions dry.
Laboratory studies
No significant laboratory abnormalities have been noted with apocrine chromhidrosis. The following test may help to rule out other causes:
- Determination of complete blood cell counts to exclude bleeding diathesis
- Tests of urinary homogentisic acid levels to exclude alkaptonuria
- Fungal and bacteriologic cultures to exclude infectious causes of pseudochromhidrosis
- Liver function tests and bilirubin levels to exclude hyperbilirubinemia
Apocrine glands biopsy
The apocrine glands appear normal in size and morphology, but the number of glands varies. The increased number of yellow-brown lipofuscin granules is observed in the cytoplasm of secretory cells on routine hematoxylin-eosin staining. The granules are positive on periodic acid-Schiff stains and demonstrate autofluorescence under a UV excitation wavelength of 360-395 nm. Schmorl stains may also be weakly positive 24.
Chromhidrosis treatment
Apocrine chromhidrosis has no fully satisfactory cure or treatment. Patients can manually or pharmacologically empty the glands to achieve a symptom-free period of about 48-72 hours or until the glands replenish the pigment 13. Capsaicin, applied once or twice daily, depletes the neurons of substance P and can improve the appearance in some patients 27. Burning sensation at the application site is a common side effect of capsaicin. Topical aluminum chloride and injections of botulinum toxin type A (BOTOX) have also reportedly shown benefit in patients 28. The condition usually recurs after cessation of therapy 7.
BOTOX® injections have been attempted in 5 cases of chromhidrosis, with mixed results. BOTOX® is predominantly used to decrease eccrine sweat in persons with hyperhidrosis. However, recent reports demonstrated improvement of facial and axillary chromhidrosis with BOTOX® 29. The mechanism by which BOTOX® suppresses apocrine chromhidrosis is unclear. BOTOX® may suppress apocrine secretion by blocking cholinergic stimulation and substance P release 30.
A few reports have described successful treatment of chromhidrosis with capsaicin cream 27. Capsaicin, a crystalline alkaloid found in red peppers, is commonly used for the temporary relief of pain from rheumatoid arthritis, osteoarthritis, and neuralgias. Capsaicin depletes neurons of substance P, a neurotransmitter important in apocrine sweat production. Clinical relapse occurs when therapy is stopped.
The treatment of eccrine chromhidrosis revolves around stopping or replacing the causative agent 13.
In cases of pseudochromhidrosis, topical or systemic antimicrobials are often used to eradicate the offending microorganism. Of note, medications may have implications in altering the normal flora, allowing for chromogenic organisms to take their place 13. Discontinuation of these medications should be a consideration in such situations.
Chromhidrosis prognosis
Chromhidrosis persists throughout life, but slow regression of the disease is noted, as apocrine glands regress with time. The prognosis for chromhidrosis is good if an extrinsic cause can be identified and addressed appropriately. However, it may lead to significant anxiety, depression, or embarrassment requiring frequent clothing changes during the day 10.
- Wiseman MC. Disorders of Apocrine glands. In: Goldsmith LA, Wolff K, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. 7th ed. New York: McGraw-Hill; 2008. pp. 731–8.[↩][↩][↩][↩][↩]
- Erdol S, Karakaya S, Saglam H, Tarim O. Chromhidrosis due to exogenous oxidizing heavy metals: Clinical and laboratory findings. Pediatr Dermatol. 2018 Jul;35(4):448-452.[↩]
- Ingvaldsen CA, Leegaard TM, Kravdal G, Mørk C. Infectious Pseudochromhidrosis: A Case Report and Literature Review. Acta Derm Venereol. 2020;100(1):adv00005. Published 2020 Jan 7. doi:10.2340/00015555-3338[↩][↩][↩][↩]
- Barankin B, Alanen K, Ting PT, Sapijaszko MJ. Bilateral facial apocrine chromhidrosis. J Drugs Dermatol. 2004 Mar-Apr. 3(2):184-6.[↩]
- Mali-Gerrits MM, van de Kerkhof PC, Mier PD, Happle R. Axillary apocrine chromhidrosis. Arch Dermatol. 1988 Apr. 124(4):494-6.[↩]
- Griffith JR. Isolated areolar apocrine chromhidrosis. Pediatrics. 2005 Feb. 115(2):e239-41.[↩]
- Semkova K, Gergovska M, Kazandjieva J, Tsankov N. Hyperhidrosis, bromhidrosis, and chromhidrosis: Fold (intertriginous) dermatoses. Clin. Dermatol. 2015 Jul-Aug;33(4):483-91.[↩][↩][↩][↩][↩]
- Krishnaram AS, Bharathi S, Krishnan S. An interesting case of bisacodyl (dulcolax)-induced chromhidrosis. Indian J Dermatol Venereol Leprol. 2012 Nov-Dec. 78(6):756-8.[↩][↩]
- Yöntem A, Kör D, Hızlı Karabacak B, Karakaş M, Önenli Mungan N. Blue-colored sweating: four infants with apocrine chromhidrosis. Turk J Pediatr. 2015 May-Jun. 57 (3):290-3.[↩]
- Bilgin I, Kelekci KH, Catal S, Calli A. Late-onset apocrine chromhidrosis. Indian J Dermatol Venereol Leprol. 2014 Nov-Dec;80(6):579.[↩][↩]
- Beer K, Oakley H. Axillary chromhidrosis: report of a case, review of the literature and treatment considerations. J Cosmet Dermatol. 2010 Dec;9(4):318-20.[↩]
- Chromhidrosis. https://emedicine.medscape.com/article/1072254-overview[↩]
- Gaffney DC, Cooper HL. Coloured sweat in two brothers: First report of familial chromhidrosis. Australas. J. Dermatol. 2016 Feb;57(1):e23-5.[↩][↩][↩][↩][↩][↩]
- Cilliers J, de Beer C. The case of the red lingerie – Chromhidrosis revisited. Dermatology. 1999;199:149–52.[↩][↩]
- Shelley WB, Hurley HJ., Jr Localized chromhidrosis; a survey. AMA Arch Derm Syphilol. 1954;69:449–71.[↩]
- Koley S, Mandal RK. Red and black pseudochromhidrosis. Indian J Dermatol. 2016;61:454–7.[↩]
- Hurley HJ, Witkowski J. Dye clearance and eccrine sweat secretion in human skin. J Invest Dermatol. 1961;36:259–72.[↩]
- Jaiswal AK, Ravikiran SP, Roy PK. Red Eccrine Chromhidrosis with Review of Literature. Indian J Dermatol. 2017;62(6):675. doi:10.4103/ijd.IJD_755_16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5724326[↩]
- Krishnaram AS, Bharathi S, Krishnan S. An interesting case of bisacodyl (Dulcolax ®)-induced chromhidrosis. Indian J Dermatol Venereol Leprol. 2012;78:756–8.[↩]
- Ghosh SK, Rudra O, Kar R, Ghosh A, Agarwal M. A curious case of blue-green discoloration in a middle-aged Indian man: Chromhidrosis. Dermatol Online J. 2015;21 pii: 13030/qt5jj4859x[↩]
- Keum DI, Hong H, Lee SH, Ahn SK. Eccrine chromhidrosis resembling clinical features of pompholyx with bile-like greenish pigmentation on the right palm and soles. Ann Dermatol. 2015;27:482–3.[↩]
- Gaffney DC, Cooper HL. Coloured sweat in two brothers: First report of familial chromhidrosis. Australas J Dermatol. 2016 Feb. 57 (1):e23-5[↩]
- Polat M, Dikilitas M, Gozubuyukogullari A, Alli N. Apocrine chromhidrosis. Clin Exp Dermatol. 2009 Oct. 34(7):e373-4.[↩]
- Wang A, Wysong A, Nord KM, Egbert BM, Kosek J. Chromhidrosis: A Rare Diagnosis Requiring Clinicopathologic Correlation. Am J Dermatopathol. 2013 Mar 14.[↩][↩]
- Cox NH, Popple AW, Large DM. Autofluorescence of clothing as an adjunct in the diagnosis of apocrine chromhidrosis. Arch Dermatol. 1992 Feb. 128(2):275-6.[↩]
- Blalock TW, Crowson AN, Danford B. A case of generalized red sweating. Dermatol. Online J. 2014 Dec 14;21(3).[↩]
- Rumsfield JA, West DP. Topical capsaicin in dermatologic and peripheral pain disorders. DICP. 1991 Apr. 25(4):381-7.[↩][↩]
- Suessman A, Srinivasan S. Chromhidrosis: An Unusual Cause of Skin Discoloration. Pediatr Emerg Care. 2019 Apr 04[↩]
- Pérez-Tato B, Zamora-Martínez E, Sánchez-Albisua B, Pérez-González YC, Polimón-Olabarrieta I, Marinero-Escobedo S, et al. Facial and axillary apocrine chromhidrosis. Dermatol Online J. 2012 Mar 15. 18(3):13.[↩]
- Wu JM, Mamelak AJ, Nussbaum R, McElgunn PS. Botulinum toxin a in the treatment of chromhidrosis. Dermatol Surg. 2005 Aug. 31(8 Pt 1):963-5.[↩]