Circumvallate placenta
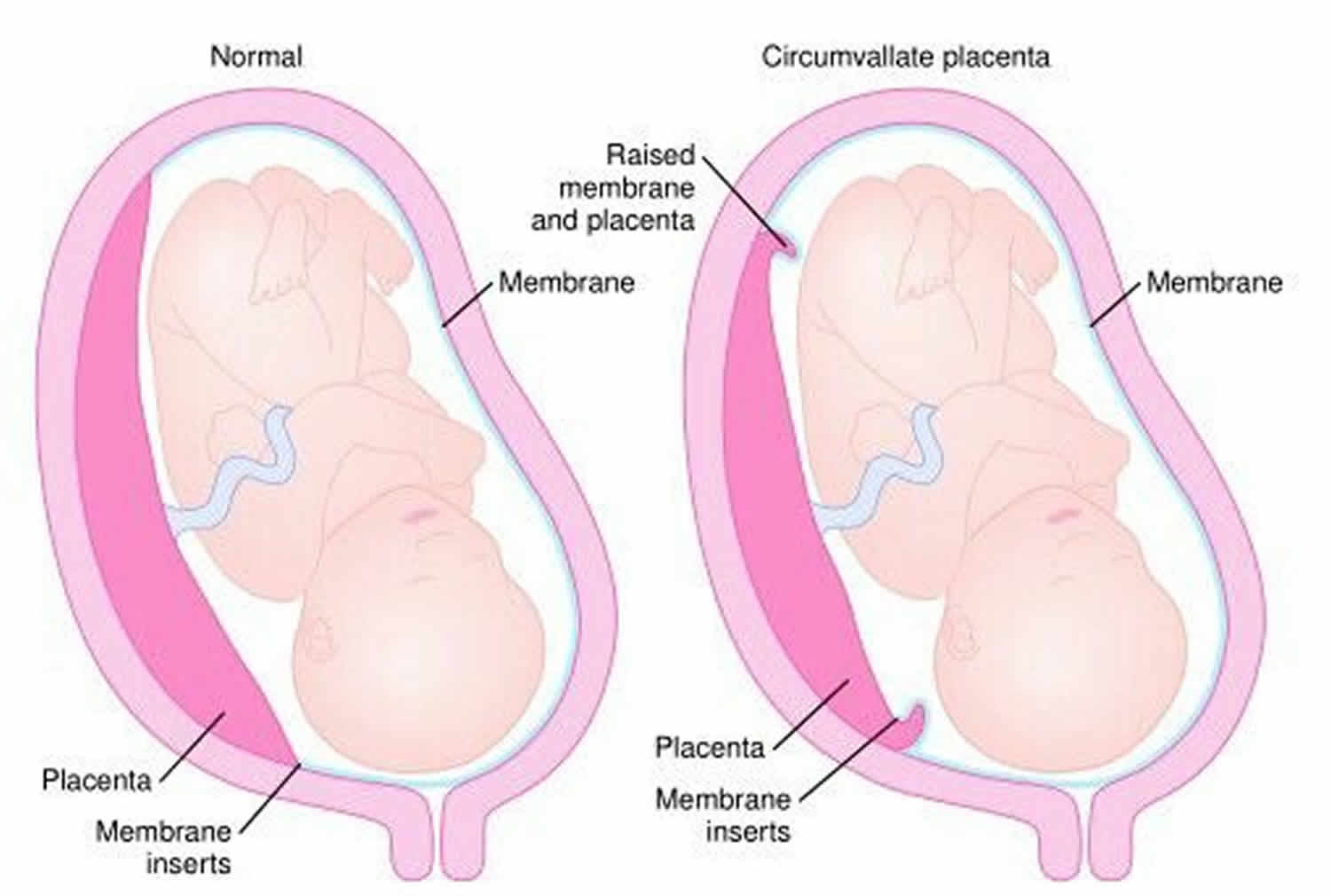
Circumvallate placenta also called placenta circumvallata, is an abnormality of the placental shape, an annularly-shaped placenta, where there is a central depression on the fetal surface surrounded by a greyish white thickened ring at the periphery 1. Here the chorion and amnion are folded upon themselves at the placental margin making the chorionic plate on the fetal side smaller than the basal plate on the maternal side leaving a part of the placenta uncovered at the periphery 2. In circumvallate placenta, the chorionic plate is smaller than the basal plate, resulting in hematoma retention in the placental margin 3. Within the ring, the fetal surface has the usual appearance except that the large vessels terminate abruptly at the margin of the ring. Circumvallate placenta is associated with poor pregnancy outcomes due to increased risk of vaginal bleeding beginning in the first and second trimesters, preterm premature rupture of the membranes (PPROM), preterm delivery, subchorionic hematoma, oligohydramnios, placental insufficiency, and placental abruption 4. Circumvallate placenta diagnosis is difficult to make during pregnancy and is made most often on visual inspection of the placenta after delivery 5.
The prevalence of circumvallate placenta is not documented which could be because of its rarity 1.
The diagnosis of circumvallate placenta antenatally is however very difficult. The accuracy of diagnosis by ultrasound is limited with high false positive and high false negative rates 6. Second trimester bleeding per vagina and premature rupture of membranes (PROM) had a sensitivity of 28.8% and specificity of 99.9% when both are used as predictors for circumvallate placenta 3. Women with circumvallate placenta if detected antenatally should be considered as high risk pregnancy due to possible poor pregnancy outcome.
In the past as stated by Williams 7, circumvallate placenta was considered to be a mere interesting anatomic variation of placenta without any clinical significance. Since then, various studies have been conducted and in one of the earlier studies by Russell et al. 8, high incidence of late abortions, preterm labors and maternal hemorrhage have been found to be associated with circumvallate placenta. Although high incidence of fetal demise was associated with circumvallate placenta, it was rarely listed as the cause 9.
Subsequently, other studies have also shown increased incidence of complications in patients with circumvallate placenta like placental abruption (abruptio placentae), preterm births, intrauterine growth restriction (IUGR), oligohydramnios, non-reassuring fetal heart rate patterns 10 and even a study reported increased incidence of early intrauterine fetal death (IUFD) as compared to controls 10. Also, in addition to these complications, Hanako Taniguchi et al. 3 stated that circumvallate placenta was associated with increased incidence of emergency Cesarean Section, neonatal intensive care unit (NICU) admission, neonatal death and even chronic lung disease.
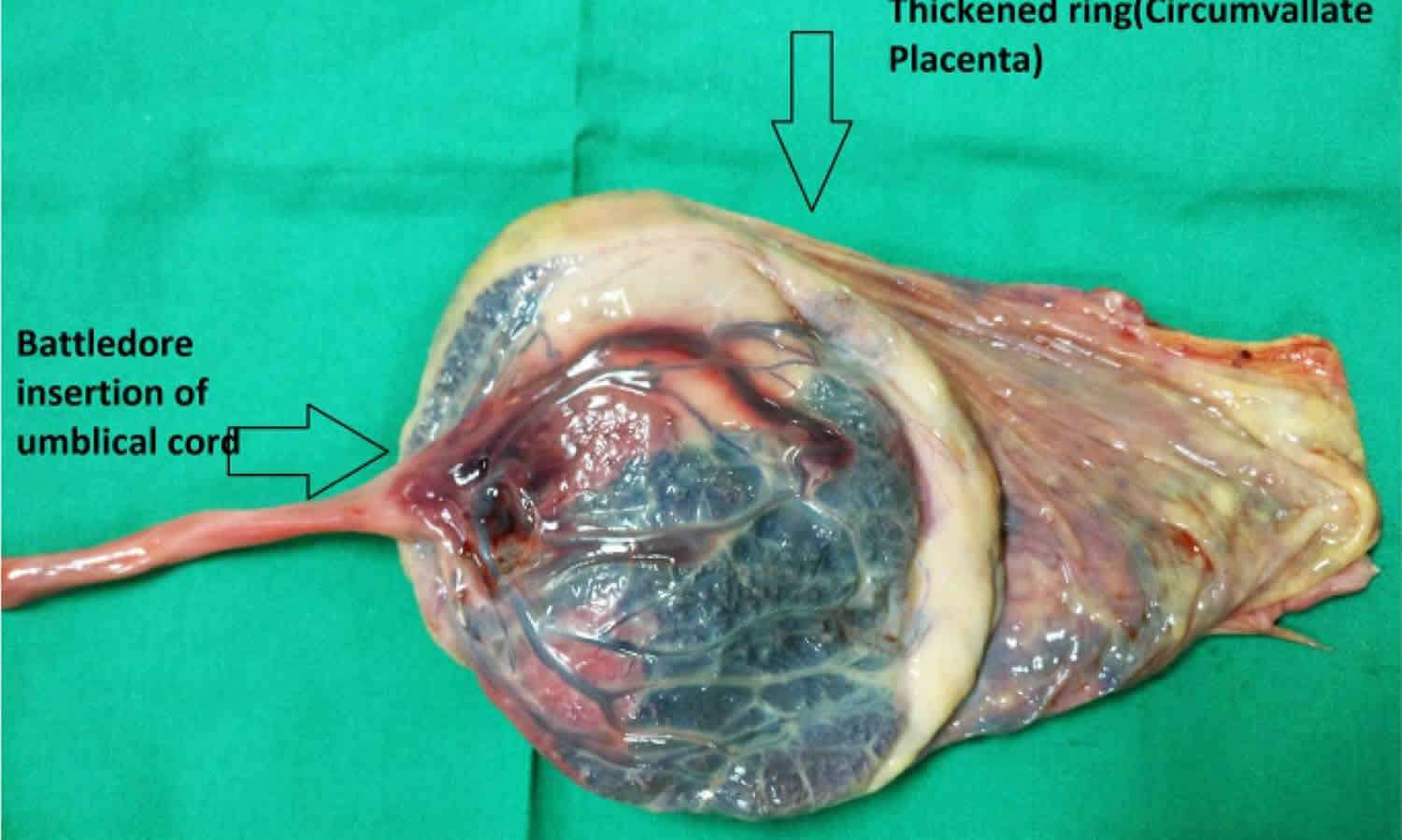
Figure 1. Circumvallate placenta
Footnote: Coexistent Battledore insertion of umbilical cord and circumvallate placenta. In Battledore placenta, the umbilical cord is attached to the placental margin 2. also known as marginal insertion of umbilical cord. Both abnormalities are very rare individually. Both circumvallate placenta and Battledore insertion of the umbilical cord are known to adversely affect the pregnancy outcome individually and in these women, their coexistence leads to a more serious untoward consequence of early intrauterine fetal death (IUFD). Thus, if such placental and cord abnormalities are suspected or diagnosed antennatally by ultrasonography, the pregnancy should be regarded as high risk and the women would require more stringent follow up in the antenatal period and continuous intrapartum monitoring to avoid such a catastrophe and to achieve favorable maternal and foetal outcome.
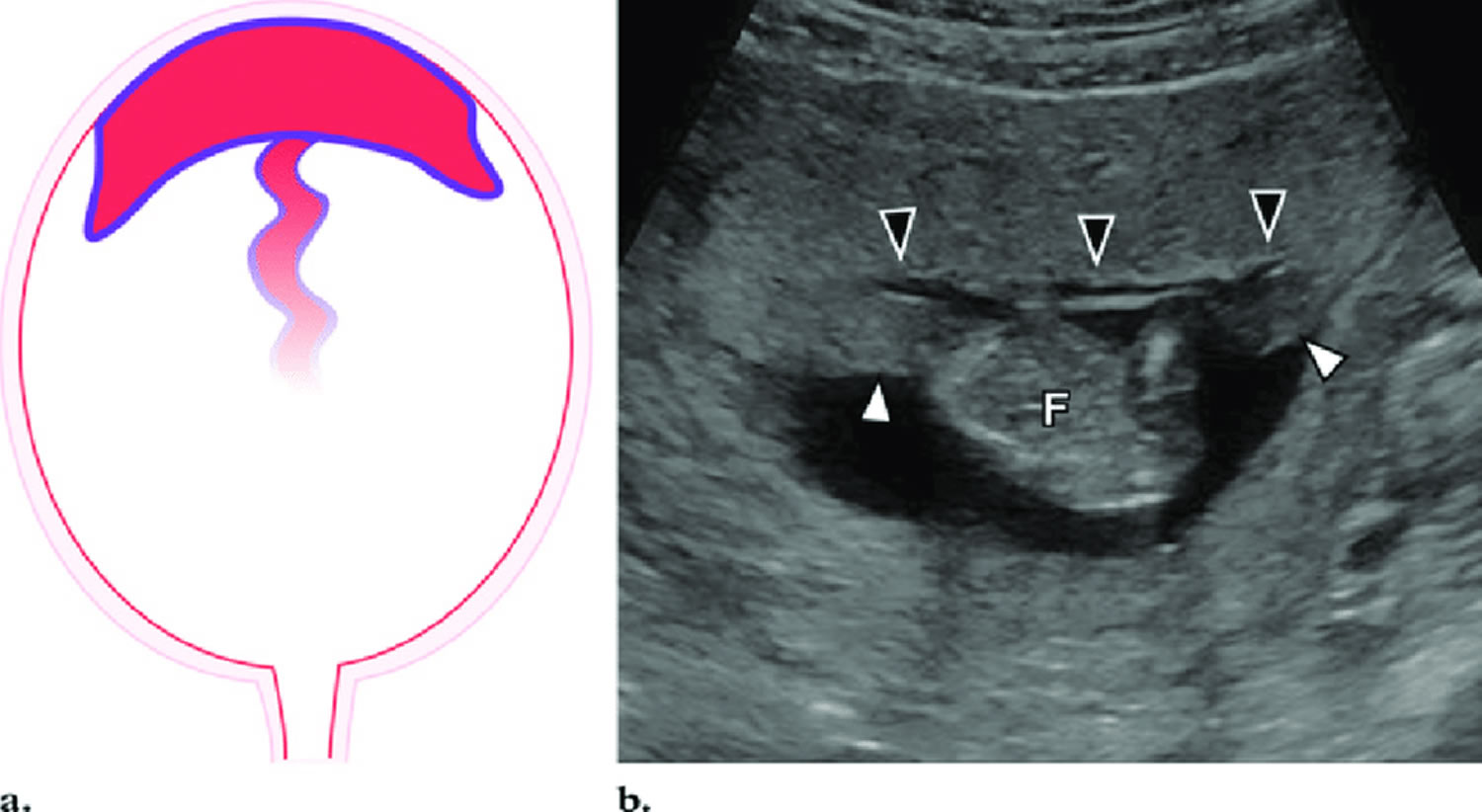
[Source 1 ]Figure 2. Circumvallate placenta ultrasound
Footnote: (a) Diagram shows a circumvallate placenta. (b) Ultrasound image shows a circumvallate placenta. The chorionic plate (the fetal surface of the placenta) (black arrowheads) is smaller than the basal plate (the surface interfacing with the uterus), with rolling and shouldering of the placental margins (white arrowheads). F = fetus.
[Source 11 ]Circumvallate placenta symptoms
Women with circumvallate placenta frequently had clinical symptoms of vaginal bleeding during pregnancy and preterm premature rupture of the membranes (PPROM) 3. Particularly, among those with circumvallate placenta who delivered before term, 28.8% had vaginal bleeding during the 2nd trimester and premature chemical rupture of membranes (PCROM) findings. Thus, these two features were supposed to be useful for antenatal prediction of circumvallate placenta. Bey et al. 12 say that when vaginal bleeding occurs in the 2nd trimester despite a normally implanted placenta, circumvallate placenta should be included in the differential diagnosis.
In the study by Taniguchi et al. 3, circumvallate placenta was suspected antenatally in only 4 (4.3%) of 92 women. In all four women, circumvallate placenta had been suspected based on a combination of characteristic clinical symptoms (i.e., oligohydramnios, vaginal bleeding during the 2nd trimester, and fetal growth restriction) and ultrasonographic findings (e.g., a thickened placenta and a hematoma at the placental margin). Circumvallate placenta was not suggested by ultrasonographic findings alone. Women with circumvallate placenta had characteristic clinical symptoms. When vaginal bleeding during the 2nd trimester and premature chemical rupture of membranes (PCROM) were both used as predictions of circumvallate placenta, sensitivity was 28.8% and specificity was 99.9%. In women with these two features, circumvallate placenta should be strongly suspected.
Circumvallate placenta complications
In the past as stated by Williams 7, circumvallate placenta was considered to be a mere interesting anatomic variation of placenta without any clinical significance. Since then, various studies have been conducted and in one of the earlier studies by Russell et al. 8, high incidence of late abortions, preterm labors and maternal hemorrhage have been found to be associated with circumvallate placenta. Although high incidence of fetal demise was associated with circumvallate placenta, it was rarely listed as the cause 9.
Subsequently, other studies have also shown increased incidence of complications in patients with circumvallate placenta like placental abruption (abruptio placentae), preterm births, intrauterine growth restriction (IUGR), oligohydramnios, non-reassuring fetal heart rate patterns 10 and even a study reported increased incidence of early intrauterine fetal death (IUFD) as compared to controls 10. Also, in addition to these complications, Hanako Taniguchi et al. 3 stated that circumvallate placenta was associated with increased incidence of emergency Cesarean Section, neonatal intensive care unit (NICU) admission, neonatal death and even chronic lung disease.
Even when adjusted by gestational week at delivery, the incidences of small-for-gestational age, neonatal death, and chronic lung disease were also significantly higher in the circumvallate placenta than in the control group, indicating poor neonatal outcomes 3. In women with circumvallate placenta who delivered before term especially, clinical symptoms including vaginal bleeding during the 1st and 2nd trimesters and premature chemical rupture of membranes (PCROM) were more common than in those delivering term babies. Notably, women with both vaginal bleeding during the 2nd trimester and premature chemical rupture of membranes (PCROM) accounted for 28.8% of the circumvallate placenta group delivering before term, as compared with 0.1% of controls. Thus, these two features might suggest circumvallate placenta during pregnancy.
The circumvallate placenta group shows poor pregnancy and delivery outcomes. Circumvallate placenta may lead to vaginal bleeding during the 2nd trimester, preterm premature rupture of the membranes (PPROM), and preterm delivery. A hematoma reportedly forms in the circumvallate placenta margin, causing ascending infection progressing to chorioamnionitis 13. Suzuki 4 examined obstetrical outcomes in 139 circumvallate placenta cases and reported preterm delivery (22%), oligohydramnios (3.6%), placental abruption (5.0%), and emergency cesarean section (16%) incidences to be significantly higher in these women than in controls.
Small-for-gestational age and chronic lung disease incidences were higher in the circumvallate placenta group than in controls. As to the association between circumvallate placenta and small-for-gestational age, fetal growth restriction has been speculated to be caused by placental insufficiency due to a marginal infarct, hemorrhage, and hemosiderin deposition, in addition to a hypoplastic placenta 4. It has also been suggested that prolonged vaginal bleeding during pregnancy causes hemosiderin deposition in the placenta and chorion, resulting in diffuse chorioamniotic hemosiderosis, and that the fetus may swallow bloody amniotic fluid and thereby develop chronic lung disease 14.
In complete opposite to all the above studies, a 2018 retrospective cohort study involving 67 women with circumvallate placenta by Lorene et al. 15, stated that “antenatally diagnosed circumvallate placenta was not associated with an increased risk of small-for-gestational age at birth or other adverse obstetric and neonatal outcomes”. This suggests that antenatal diagnosis of circumvallate placenta may be benign and women may be managed with routine obstetric care.
Circumvallate placenta diagnosis
Several studies have reported that circumvallate placenta can be diagnosed based on ultrasonographic abnormalities in placental appearance 16. McCarthy et al. 17 reported diagnostic criteria based on an irregular, uplifted placental edge (rounded placental margin) or a marginal shelf or rim (thin or sheet-like placental edge). Suzuki 5 described measurement of placental thickness (thickest part ≥3.0 cm) as being useful for circumvallate placenta screening. Arlicot et al. 16 recently reported that circumvallate placenta was diagnosed by 3-dimensional sonographic imaging showing a circumferential depression with a thick peripheral ring in the placenta. Harris et al. 18 found the accuracy of sonography for the diagnosis of complete circumvallate placenta to be 2% based on their criteria, concluding that it is difficult to diagnose this condition using sonography. Circumvallate placenta diagnosis is difficult to make during pregnancy and is made most often on visual inspection of the placenta after delivery 19.
Circumvallate placenta treatment
In women where circumvallate placenta is suspected and their clinical courses should be carefully monitored 3.
Circumvallate placenta outcomes
In the past as stated by Williams 7, circumvallate placenta was considered to be a mere interesting anatomic variation of placenta without any clinical significance. Since then, various studies have been conducted and in one of the earlier studies by Russell et al. 8, high incidence of late abortions, preterm labors and maternal hemorrhage have been found to be associated with circumvallate placenta. Although high incidence of fetal demise was associated with circumvallate placenta, it was rarely listed as the cause 9.
Subsequently, other studies have also shown increased incidence of complications in patients with circumvallate placenta like placental abruption (abruptio placentae), preterm births, intrauterine growth restriction (IUGR), oligohydramnios, non-reassuring fetal heart rate patterns 10 and even a study reported increased incidence of early intrauterine fetal death (IUFD) as compared to controls 10. Also, in addition to these complications, Hanako Taniguchi et al. 3 stated that circumvallate placenta was associated with increased incidence of emergency Cesarean Section, neonatal intensive care unit (NICU) admission, neonatal death and even chronic lung disease.
Even when adjusted by gestational week at delivery, the incidences of small-for-gestational age, neonatal death, and chronic lung disease were also significantly higher in the circumvallate placenta than in the control group, indicating poor neonatal outcomes 3. In women with circumvallate placenta who delivered before term especially, clinical symptoms including vaginal bleeding during the 1st and 2nd trimesters and premature chemical rupture of membranes (PCROM) were more common than in those delivering term babies. Notably, women with both vaginal bleeding during the 2nd trimester and premature chemical rupture of membranes (PCROM) accounted for 28.8% of the circumvallate placenta group delivering before term, as compared with 0.1% of controls. Thus, these two features might suggest circumvallate placenta during pregnancy.
The circumvallate placenta group shows poor pregnancy and delivery outcomes. Circumvallate placenta may lead to vaginal bleeding during the 2nd trimester, preterm premature rupture of the membranes (PPROM), and preterm delivery. A hematoma reportedly forms in the circumvallate placenta margin, causing ascending infection progressing to chorioamnionitis 13. Suzuki 4 examined obstetrical outcomes in 139 circumvallate placenta cases and reported preterm delivery (22%), oligohydramnios (3.6%), placental abruption (5.0%), and emergency cesarean section (16%) incidences to be significantly higher in these women than in controls.
Small-for-gestational age and chronic lung disease incidences were higher in the circumvallate placenta group than in controls. As to the association between circumvallate placenta and small-for-gestational age, fetal growth restriction has been speculated to be caused by placental insufficiency due to a marginal infarct, hemorrhage, and hemosiderin deposition, in addition to a hypoplastic placenta 4. It has also been suggested that prolonged vaginal bleeding during pregnancy causes hemosiderin deposition in the placenta and chorion, resulting in diffuse chorioamniotic hemosiderosis, and that the fetus may swallow bloody amniotic fluid and thereby develop chronic lung disease 14.
In complete opposite to all the above studies, a 2018 retrospective cohort study involving 67 women with circumvallate placenta by Lorene et al. 15, stated that “antenatally diagnosed circumvallate placenta was not associated with an increased risk of small-for-gestational age at birth or other adverse obstetric and neonatal outcomes”. This suggests that antenatal diagnosis of circumvallate placenta may be benign and women may be managed with routine obstetric care 15.
- Sharma N, Das R, Salam S, Jethani R, Singh AS. Coexistent Circumvallate Placenta and Battledore Insertion of Umbilical Cord Resulting in Grave Obstetric Outcome: A Case Report. J Reprod Infertil. 2017;18(4):390–392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691256[↩][↩][↩]
- Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong CY. Williams Obstetrics. 22nd ed New York: McGraw Hill Professional; 2009. 1600 p.[↩][↩]
- Taniguchi H, Aoki S, Sakamaki K, et al. Circumvallate placenta: associated clinical manifestations and complications-a retrospective study. Obstet Gynecol Int. 2014;2014:986230. doi:10.1155/2014/986230 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4248327[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Suzuki S. Clinical significance of pregnancies with circumvallate placenta. Journal of Obstetrics and Gynaecology Research. 2008;34(1):51–54. doi: 10.1111/j.1447-0756.2007.00682.x[↩][↩][↩][↩][↩]
- Suzuki S. Antenatal screening for circumvallate placenta. Journal of Medical Ultrasonics. 2008;35(2):71–73. doi: 10.1007/s10396-007-0168-5[↩][↩]
- Holzman J, Zalud I, Bartholomew ML. Ultrasound of the placenta. Donald Sch J Ultrasound Obstet Gynaecol. 2007;1(4):47–60.[↩]
- Placenta circumvallata. Am J Obstet Gynecol. January 1927 Volume 13, Issue 1, Pages 1–16 https://doi.org/10.1016/S0002-9378(27)90108-2[↩][↩][↩]
- Circumvallate placenta. Am J Obstet Gynecol. March 1953 Volume 65, Issue 3, Pages 491–497 https://doi.org/10.1016/0002-9378(83)90605-1[↩][↩][↩]
- Paalman RJ, Vander Veer CG, Rapids G. Circumvallate placenta. Am J Obstet Gynecol. 1953;65(3): 491–7.[↩][↩][↩]
- Suzuki S. Clinical significance of pregnancies with circumvallate placenta. J Obstet Gynaecol Res. 2008; 34(1):51–4.[↩][↩][↩][↩][↩][↩]
- Elsayes, Khaled & Trout, Andrew & Friedkin, Aaron & Liu, Peter & Bude, Ronald & Platt, Joel & Menias, Christine. (2009). Imaging of the Placenta: A Multimodality Pictorial Review. Radiographics : a review publication of the Radiological Society of North America, Inc. 29. 1371-91. 10.1148/rg.295085242. [↩]
- Bey M., Dott A., Miller J. M., Jr. The sonographic diagnosis of circumvallate placenta. Obstetrics and Gynecology. 1991;78(3):515–517.[↩]
- Takeda S., Baba K., Kojima T., Kinoshita K., Satoh K., Sakamoto S. Ultrasonographic monitoring of the placenta in patients with bleeding during the first and second trimesters. Asia-Oceania Journal of Obstetrics and Gynaecology. 1990;16(3):211–218.[↩][↩]
- Yoshida S., Kikuchi A., Sunagawa S., et al. Pregnancy complicated by diffuse chorioamniotic hemosiderosis: obstetric features and influence on respiratory diseases of the infant. Journal of Obstetrics and Gynaecology Research. 2007;33(6):788–792. doi: 10.1111/j.1447-0756.2007.00657.x[↩][↩]
- Clinical significance of circumvallate placenta. American Journal of Obstetrics&GynecologySupplement to JANUARY 2018 https://www.ajog.org/article/S0002-9378(17)31606-X/pdf[↩][↩][↩]
- Arlicot C., Herve P., Simon E., Perrotin F. Three-dimensional surface rendering of the chorionic placental plate: the “tire” sign for the diagnosis of a circumvallate placenta. Journal of Ultrasound in Medicine. 2012;31(2):340–341.[↩][↩]
- McCarthy J., Thurmond A. S., Jones M. K., Sistrom C., Scanlan R. M., Jacobson S. L., Lowensohn R. Circumvallate placenta: sonographic diagnosis. Journal of Ultrasound in Medicine. 1995;14(1):21–26.[↩]
- Harris R. D., Wells W., Black W., Chertoff J. D., Poplack S. P., Sargent S. K., Crow H. C. Accuracy of prenatal sonography for detecting circumvallate placenta. The American Journal of Roentgenology. 1997;168(6):1603–1608. doi: 10.2214/ajr.168.6.9168736[↩]
- Rathbun KM, Hildebrand JP. Placenta Abnormalities. [Updated 2019 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459355[↩]