Coronary flow reserve
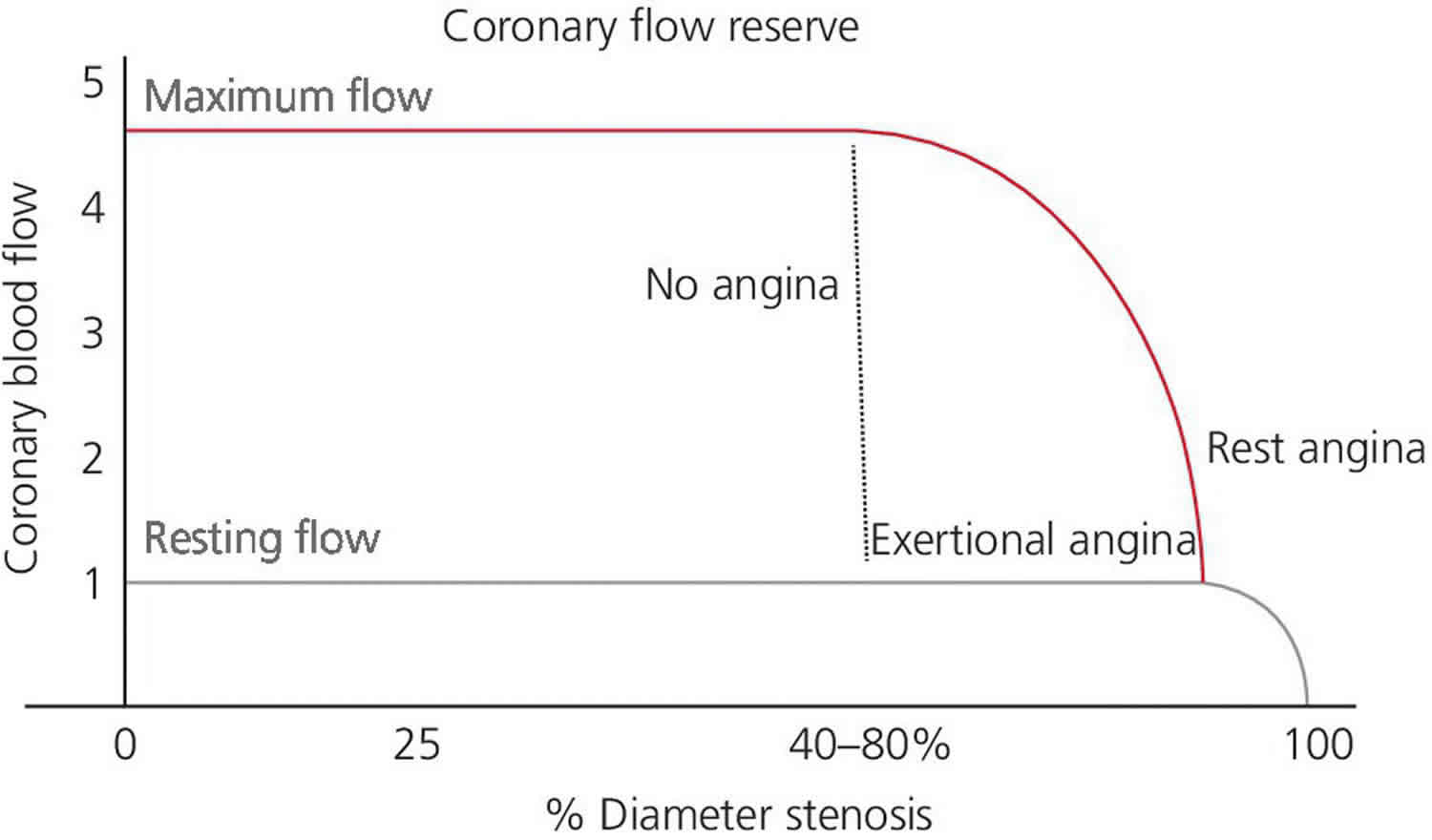
Coronary flow reserve (CFR) is defined as the ratio of coronary blood flow under maximal drug-induced coronary vasodilation to coronary blood flow under resting conditions. Coronary flow reserve is used to describe the amount of additional blood flow that can be supplied to the heart above baseline blood flow 1. The maximal vasodilatation can be brought with pharmacologic stress by using three different drug stressors such as adenosine, dipyridamole,or regadenoson 2. The coronary flow reserve mirrors the capacity of the coronary circulation to increase flow and thus, oxygen and substrate delivery in response to increased myocardial demand. The heart can increase blood flow through coronary circulation three to six times in the settings of increased demand compared to the flow under resting conditions. Consequently, the cut-off at coronary flow reserve >3 is regarded as the lower threshold for the normal value in the healthy human heart 3.
Coronary flow reserve accounts for flow through both the epicardial vessels and microvasculature. Coronary flow reserve is a strong and independent predictor of major adverse cardiovascular events both in individuals without epicardial coronary artery disease as well as in those with known coronary artery disease 4. Usually, in the absence of epicardial coronary artery disease, coronary flow reserve increases by factor 5 or more while in presenceof 50% epicardial coronary artery lumen reduction coronary flow reserve decreases up to be abnormal at rest in the presence of high degree of stenoses (>85%) 5.
Unfortunately, the coronary flow reserve is an expression of a pressure gradient between epicardial coronary artery and microcirculation and therefore it is reduced in case of collaterals or microcirculation disease even in theabsence of epicardial stenosis 6. For this reason, these stressperfusion tests are not able to distinguish between the two entities. To this regard, the invasive fractional flow reserve (FFR) has been introduced to overcome these limitations.
Coronary flow regulation is mainly controlled at the microcirculatory level, where endothelium has a central regulatory role. However, other factors influence coronary flow reserve (CFR) including atherosclerotic narrowing of the vessel lumen, rheological properties of blood, inflammation, and coagulation 7. The absence of coronary flow reserve implies maximal vasodilatation of the resistance vessels at rest and an inability to further increase myocardial blood flow. Coronary flow reserve can be thought of as the capacity of the coronary circulation to dilate and thus increase flow following an increase in myocardial metabolic demands 8. Coronary flow reserve (CFR) is a strong and independent predictor of major adverse cardiovascular events (e.g., death, heart attack and stroke) 3. The coronary flow reserve is a powerful tool to guide therapy and to assess prognosis. Changes in coronary flow reserve can assess both the presence 9 and severity 10 of coronary artery disease and can also be used in various other conditions (e.g. to determine if a patient presenting for the first time with heart failure has an ischemic or non-ischemic atiology or to determine prognosis in heart failure patients) 11, 12.
Figure 1. Coronary flow reserve
Footnote: The coronary flow reserve (CRF) is defined as the ratio between the coronary blood flow at maximum vasodilatation and the coronary blood flow at rest condition. Relationship between the coronary artery gradient pressure (difference between the epicardial coronary artery and microcirculation pressure) and coronary blood flow at rest condition (blue line) and at maximal vasodilatation (red line).
[Source 13 ]Coronary flow reserve can be measured invasively with a Doppler-tipped coronary guide wire that determines coronary velocity at rest and during hyperemia, typically induced with intracoronary or intravenous adenosine. Because velocity is proportional to flow, the coronary flow velocity reserve is a reflection of the coronary flow reserve. If in addition to the velocity the area of the coronary vessel is known, the absolute coronary flow reserve can be calculated. Coronary flow reserve also can be measured invasively by using a wire-based thermodilution technique. On one of the commercially available coronary pressure wires (St. Jude Medical, MIN), the pressure sensor also can act as a thermistor. With the commercially available software, the shaft of the wire acts as a proximal thermistor. Room temperature saline can be injected into the coronary artery and this system will calculate the transit time, which is inversely proportional to coronary flow. After three injections at rest, the resting mean transit time is calculated. Hyperemia is then induced with intravenous adenosine, and three injections are performed to determine the hyperemic mean transit time. coronary flow reserve is measured in this situation by dividing the resting mean transit time by the hyperemic mean transit time. The thermodilution-derived coronary flow reserve has been validated in animal and human models and has been compared in an animal model to a reference standard of absolute flow. The thermodilution-derived coronary flow reserve appears to correlate more closely to the standard than does Doppler-derived coronary flow reserve.
A normal coronary flow reserve is considered to be greater than 2.0 and in most patients should be somewhere between 3 and 5. Initially, invasive coronary flow reserve was performed to interrogate the functional significance of an intermediate coronary stenosis with studies showing a correlation between coronary flow reserve and noninvasive tests for ischemia.8 However, a number of limitations of invasively measured coronary flow reserve impaired its broad clinical utility. First, it can be difficult to measure with a Doppler wire because of the challenge in obtaining a suitable Doppler signal. Second, because coronary flow reserve relies on resting flow for its calculation, the repeatability of measurements is less than optimal. Any hemodynamic perturbation such as a change in heart rate, blood pressure, or left ventricular contractility will significantly change the coronary flow reserve value as a result of the change in resting flow. The lack of a clear cut-off between a normal and abnormal coronary flow reserve makes it difficult to use for clinical decisions. Because there is a range of normal coronary flow reserve values between approximately 2.5 and 6, in one patient a value of 3.0 might be normal whereas in another patient normal coronary flow reserve may be 5.0 and therefore a recorded value of 3.0 could be quite abnormal. Finally, by definition coronary flow reserve is a measure of the entire coronary circulation. It interrogates the epicardial vessel as well as the coronary microvasculature. Therefore, a low coronary flow reserve value may be a result of significant epicardial coronary artery disease, microvascular dysfunction, or both. For all of these reasons, invasively measured coronary flow reserve has largely been abandoned as a method for interrogating intermediate coronary lesions. However, in patients with normal appearing epicardial coronary vessels, invasively measured coronary flow reserve can be used to assess microvascular function. However, because of the previously mentioned limitations and the availability of other methods for assessing the microvasculature independently of the epicardial system (for example, the index of microcirculatory resistance), invasively measured coronary flow reserve is not performed routinely on a clinical basis.
Fractional flow reserve
Fractional flow reserve (FFR) measurement involves determining the ratio between the maximum achievable blood flow in a diseased coronary artery and the theoretical maximum flow in a normal coronary artery. FFR measures the intracoronary pressure before and after aspecific coronary lesion in the presence of hyperemic stimuli by adenosine reaching a direct relationship between pressure and flow. A FFR of 1.0 is widely accepted as normal. An fractional flow reserve lower than 0.75-0.80 is generally considered to be associated with myocardial ischemia (MI) 14. Note that fractional flow reserve (FFR) procedure is not intended for use in the setting of a total vessel occlusion. Coronary artery lesions with FFR ≤0.80 have been proved to receive benefits from revascularization while, in a setting of a stenosis with a FFR>0.80, the patient can be safely deferred to optimal medical treatment 15
More important, unlike the ischemia stressors induced, FFR is not influenced by systemic hemodynamic 16, it takes into account the contribution of collaterals 16, it specifically relates to the severity of the stenoses and to the mass of tissue to be perfused 17 and it reaches a per-lesion accuracy rather than per-myocardial territory with a very high spatial resolution 6.
- The 2014 European Society of Cardiology guidelines recommend the use of FFR to detect a hemodynamically relevant coronary lesion in stable patients when other evidence of ischemia is not available 18.
- The 2012 American College of Cardiology/American Heart Association guidelines recommends revascularization of coronary stenoses with FFR ≤ 0.8 19.
- The 2017 Society of Cardiovascular Angiography and Interventions guidelines recommend that if no stress test is available or if the stress results are indeterminate, the FFR ≤ 0.8 can be used to guide revascularization 20.
FFR (fractional flow reserve) is easily measured during routine coronary angiography by using a pressure guidewire to calculate the ratio between coronary pressure distal to a coronary artery stenosis and aortic pressure under conditions of maximum myocardial hyperemia 14. This ratio represents the potential decrease in coronary flow distal to the coronary stenosis. More recently, computed tomography (CT)-based fractional flow reserve computations have been used to evaluate the functional severity of coronary artery stenoses, with fractional flow reserves derived from outflow boundary conditions based on conventional morphology generally agreeing with those based on positron-emission tomography (PET) conditions 21. However, fractional flow reserves measurements based on conventional morphology had a tendency to overestimate functional severity, particularly in the setting of reduced vasodilatory response under hyperemia (and thus abnomal myocardial perfusion) 21.
Over the past two decades, fractional flow reserve measurement has been increasingly used in cardiac catheterization laboratories. It provides a quantitative assessment of the functional severity of a coronary artery stenosis identified during coronary angiography and cardiac catheterization.
A severe coronary artery stenosis can limit myocardial blood flow, resulting in myocardial ischemia. In most cases, the severity of a coronary artery stenosis is judged by visual inspection by the cardiologist during cardiac angiography. A lesion is generally considered severe and flow-limiting if the narrowing of the luminal diameter is estimated to be 70% or greater 22.
After a diagnostic cardiac catheterization has been performed and a stenosis has been identified, the cardiologist makes the decision as to whether FFR measurement is likely to be useful.
During angiography, the cardiologist typically assesses the patient’s symptoms and clinical characteristics, evaluates the angiographic appearance of the coronary tree, and then decides whether revascularization with angioplasty, stenting, or coronary bypass surgery is most appropriate 22.
However, the ability of the cardiologist to discriminate between lesions that can cause myocardial ischemia and lesions that are physiologically insignificant on the basis of coronary angiography alone is limited 23. The use of fractional flow reserve measurement provides the cardiologist with a straightforward, readily available, quantitative technique for evaluating the physiologic significance of a coronary stenosis.
Risks specific to the FFR procedure include the need for additional contrast use and radiation exposure, as well as a slightly increased risk of coronary arterial dissection with FFR wire passage.
Fractional flow reserve indications
Indications for FFR measurement are as follows:
- To determine the physiologic and hemodynamic significance of an angiographically intermediate coronary stenosis
- To identify appropriate culprit lesion(s) in multivessel coronary artery disease (CAD)
- To measure the functional importance of stenosis in the presence of distal collateral flow
- To identify the precise location of a coronary lesion when the angiographic image is unclear.
Fractional flow reserve measurement technique
Typically, conscious sedation is administered as part of the cardiac catheterization. Unless the patient is uncomfortable, no other anesthesia is required. The patient is placed in the supine position.
To measure fractional flow reserve (FFR), the operator crosses the coronary stenosis with an FFR-specific guide wire designed to record the coronary arterial pressure distal to the stenosis. The pressure transducer is located approximately 20 mm proximal to the distal tip of the wire, and it can be seen fluoroscopically.
Once the transducer is distal to the stenosis, a hyperemic stimulus is administered by injection through the guide catheter, and the FFR is monitored for a significant change. To achieve maximum hyperemia, adenosine is typically used: a 15-30 µg bolus in the right coronary artery, a 20-40 µg bolus in the left coronary artery, or intravenous (IV) infusion for 3-4 minutes at 140 µg/kg/min. The mean arterial pressures from the pressure wire transducer and from the guide catheter are then used to calculate FFR.
An FFR value lower than 0.75 indicates a hemodynamically significant stenosis. An FFR value higher than 0.8 indicates a stenosis that is not hemodynamically significant. Values between 0.75 and 0.80 are indeterminate and should be considered in the context of patient’s clinical history to determine if revascularization is necessary.
Fractional flow reserve complications
Complications associated with cardiac catheterization are similar to any percutaneous coronary intervention and include the following:
- Coronary vessel dissection, occlusion, or perforation
- Embolism (coronary, cerebral, or other arterial)
- Coronary artery spasm
- Local or systemic infection
- Acute renal failure or contrast induced nephropathy
- Myocardial infarction
- Stroke
- Serious arrhythmias
- Death
Fractional flow reserve outcomes
In a study 24 designed to test the hypothesis that experienced interventional cardiologists could identify patients with fractional flow reserves below 0.75 by means of coronary angiography, FFR was measured in 83 angiographically moderate coronary lesions, which were also visually assessed by 3 interventional cardiologists; the reviewers’ classification matched the FFR in only about half of the lesions, and concordance between reviewers was poor. In this study, when visual assessment was compared with fractional flow reserve, it resulted in good sensitivity (80%) and negative predictive value (91%) but poor specificity (47%) and positive predictive value (25%) 24. Angiographic assessment of an angiogram by experienced interventional cardiologists did not predict the significance of most moderate coronary lesions.
In the DEFER study, which assessed patients with single-vessel coronary artery disease (CAD) and angiographically intermediate coronary stenosis, patients with an FFR above 0.75 were randomized to either medical management or stent implantation; at 5-year follow-up, those who did not receive a stent had the same risk of death or acute myocardial ischemia as those who did, which suggests that patients with an fractional flow reserve higher than 0.75 do not benefit from revascularization of the stenosis.
The Fractional Flow Reserve versus Angiography for Multivessel Evaluation (FAME) study 25, which studied the role of fractional flow reserve in the evaluation of multivessel coronary artery disease, reported results suggesting that a revascularization strategy using fractional flow reserve yields superior clinical outcomes in patients with multivessel coronary artery disease (CAD). In this study 25, patients with multivessel coronary artery disease identified by angiography were randomized to undergo either angiography alone or fractional flow reserve plus angiography. Patients in the angiography-only arm underwent stenting of all angiographically severe lesions. Patients in the fractional flow reserve-plus-angiography arm underwent stenting only if fractional flow reserve was 0.80 or less. At 2-year follow-up, patients who underwent fractional flow reserve-driven stenting had fewer stents than those in the angiography-only group, along with reductions in mortality, MI, and repeat revascularization.
More recently, investigators retrospectively (2016-2018) evaluated fractional flow reserve in 246 German patients with coronary artery disease (CAD) undergoing transcatheter aortic valve implantation who had coronary lesions with a diameter stenosis of at least 50% 26. They found concomitant coronary artery disease in 53.3% of transcatheter aortic valve implantation patients 26. Postprocedure fractional flow reserve measurements performed in those with a positive fractional flow reserve up to and including 0.80 did not significantly change 6-8 weeks after transcatheter aortic valve implantation, which the investigators indicated confirmed the validity of fractional flow reserve for assessing coronary lesions in this specific clinical setting 26.
References- Imaging Techniques for the Assessment of Coronary Flow Reserve. European Cardiology 2008;4(1):37–40 https://doi.org/10.15420/ecr.2008.4.1.37
- Pontone, Gianluca & Andreini, Daniele & Baggiano, Andrea & Bertella, Erika & Mushtaq, Saima & Conte, Edoardo & Beltrama, Virginia & Guaricci, Andrea Igoren & Pepi, Mauro. (2015). Functional Relevance of Coronary Artery Disease by Cardiac Magnetic Resonance and Cardiac Computed Tomography: Myocardial Perfusion and Fractional Flow Reserve. BioMed Research International. 2015. 10.1155/2015/297696
- Haraldsson I, Gan LM, Svedlund S, et al. PROspective evaluation of coronary FLOW reserve and molecular biomarkers in patients with established coronary artery disease the PROFLOW-trial: cross-sectional evaluation of coronary flow reserve. Vasc Health Risk Manag. 2019;15:375-384. Published 2019 Aug 28. doi:10.2147/VHRM.S209003 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6718055
- Gan LM, Svedlund S, Wittfeldt A, et al. Incremental value of transthoracic doppler echocardiography-assessed coronary flow reserve in patients with suspected myocardial ischemia undergoing myocardial perfusion scintigraphy. J Am Heart Assoc. 2017;6:e004875
- K. L. Gould, R. L. Kirkeeide, and M. Buchi, “Coronary flowreserve as a physiologic measure of stenosis severity,” Journal ofthe American College of Cardiology,vol.15,no.2,pp.459–474,1990.
- N. H. J. Pijls and J.-W. E. M. Sels, “Functional measurement ofcoronary stenosis,”Journal of the American College of Cardiol-ogy,vol.59,no.12,pp.1045–1057,2012.
- Gan LM, Wikstrom J, Fritsche-Danielson R. Coronary flow reserve from mouse to man–from mechanistic understanding to future interventions. J Cardiovasc Transl Res. 2013;6:715–728. doi:10.1007/s12265-013-9497-5
- Assessment of Coronary Flow Reserve (CFR). The evidence for use of contrast in clinical echocardiography: Myocardial Contrast Echocardiography – MCE. https://www.escardio.org/Education/Practice-Tools/EACVI-toolboxes/Contrast-Echo/Lectures/Assessment-of-Coronary-Flow-Reserve-CFR
- Moir S, Haluska BA, Jenkins C, McNab D, Marwick TH. Myocardial blood volume and perfusion reserve responses to combined dipyridamole and exercise stress: a quantitative approach to contrast stress echocardiography. J Am Soc Echocardiogr 2005;18(11):1187-93
- Hickman M, Jeetley P, Senior R. Usefulness of myocardial contrast echocardiography derived coronary flow reserve to accurately determine severity of left anterior descending coronary artery stenosis. Am J Cardiol. 2004;93(9):1159-1162. doi:10.1016/j.amjcard.2004.01.047
- Senior R, Janardhanan R, Jeetley P, Burden L. Myocardial contrast echocardiography for distinguishing ischemic from nonischemic first-onset acute heart failure: insights into the mechanism of acute heart failure. Circulation. 2005;112(11):1587-1593. doi:10.1161/CIRCULATIONAHA.104.530089
- Anantharam B, Janardhanan R, Hayat S, Hickman M, Chahal N, Bassett P, et al. Coronary flow reserve assessed by myocardial contrast echocardiography predicts mortality in patients with heart failure. Eur J Echocardiogr 2011;12(1):69-75
- Pontone, Gianluca & Andreini, Daniele & Baggiano, Andrea & Bertella, Erika & Mushtaq, Saima & Conte, Edoardo & Beltrama, Virginia & Guaricci, Andrea Igoren & Pepi, Mauro. (2015). Functional Relevance of Coronary Artery Disease by Cardiac Magnetic Resonance and Cardiac Computed Tomography: Myocardial Perfusion and Fractional Flow Reserve. BioMed Research International. 2015. 10.1155/2015/297696.
- Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996 Jun 27. 334(26):1703-8.
- B. de Bruyne, N. H. J. Pijls, B. Kalesan et al., “Fractional flowreserve-guided PCI versus medical therapy in stable coronarydisease,”The New England Journal of Medicine,vol.367,no.11,pp. 991–1001, 2012.
- G. J. W. Bech, B. de Bruyne, N. H. J. Pijls et al., “Fractionalflow reserve to determine the appropriateness of angioplastyin moderate coronary stenosis: a randomized trial,”Circulation,vol. 103, no. 24, pp. 2928–2934, 2001.
- M. B. Iqbal, N. Shah, M. Khan, and W. Wallis, “Reduction inmyocardial perfusion territory and its effect on the physiologi-cal severity of a coronary stenosis,”Circulation: CardiovascularInterventions,vol.3,no.1,pp.89–90,2010.
- Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014;46(4):517-592. doi:10.1093/ejcts/ezu366
- Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):e44-e164. doi:10.1016/j.jacc.2012.07.013
- Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease : A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons [published correction appears in J Nucl Cardiol. 2018 May 10;:]. J Nucl Cardiol. 2017;24(5):1759-1792. doi:10.1007/s12350-017-0917-9
- Lo EW, Menezes LJ, Torii R. On outflow boundary conditions for CT-based computation of FFR: examination using PET images. Med Eng Phys. 2019 Dec 19.
- Silber S, Albertsson P, Aviles FF, et al. Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J. 2005 Apr. 26(8):804-47.
- Bartunek J, Sys SU, Heyndrickx GR, Pijls NH, De Bruyne B. Quantitative coronary angiography in predicting functional significance of stenoses in an unselected patient cohort. J Am Coll Cardiol. 1995 Aug. 26(2):328-34.
- Fischer JJ, Samady H, McPherson JA, et al. Comparison between visual assessment and quantitative angiography versus fractional flow reserve for native coronary narrowings of moderate severity. Am J Cardiol. 2002 Aug 1. 90(3):210-5.
- Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009 Jan 15. 360(3):213-24.
- Stundl A, Shamekhi J, Bernhardt S, et al. Fractional flow reserve in patients with coronary artery disease undergoing TAVI: a prospective analysis. Clin Res Cardiol. 2019 Nov 2.