CSF rhinorrhea
CSF rhinorrhea also known as cerebrospinal fluid rhinorrhea, can occur whenever there is open communication between the subarachnoid space and other spaces via meningeal disruption resulting in cerebrospinal fluid (CSF) coming out of your nose. Disruption of the barriers between the sinonasal cavity and the anterior and middle cranial fossae is the underlying factor leading to the discharge of CSF into the nasal cavity. The resulting communication with the central nervous system (CNS) can result in a multitude of infectious complications that impart significant morbidity and potentially disastrous long-term deficits for the patient.
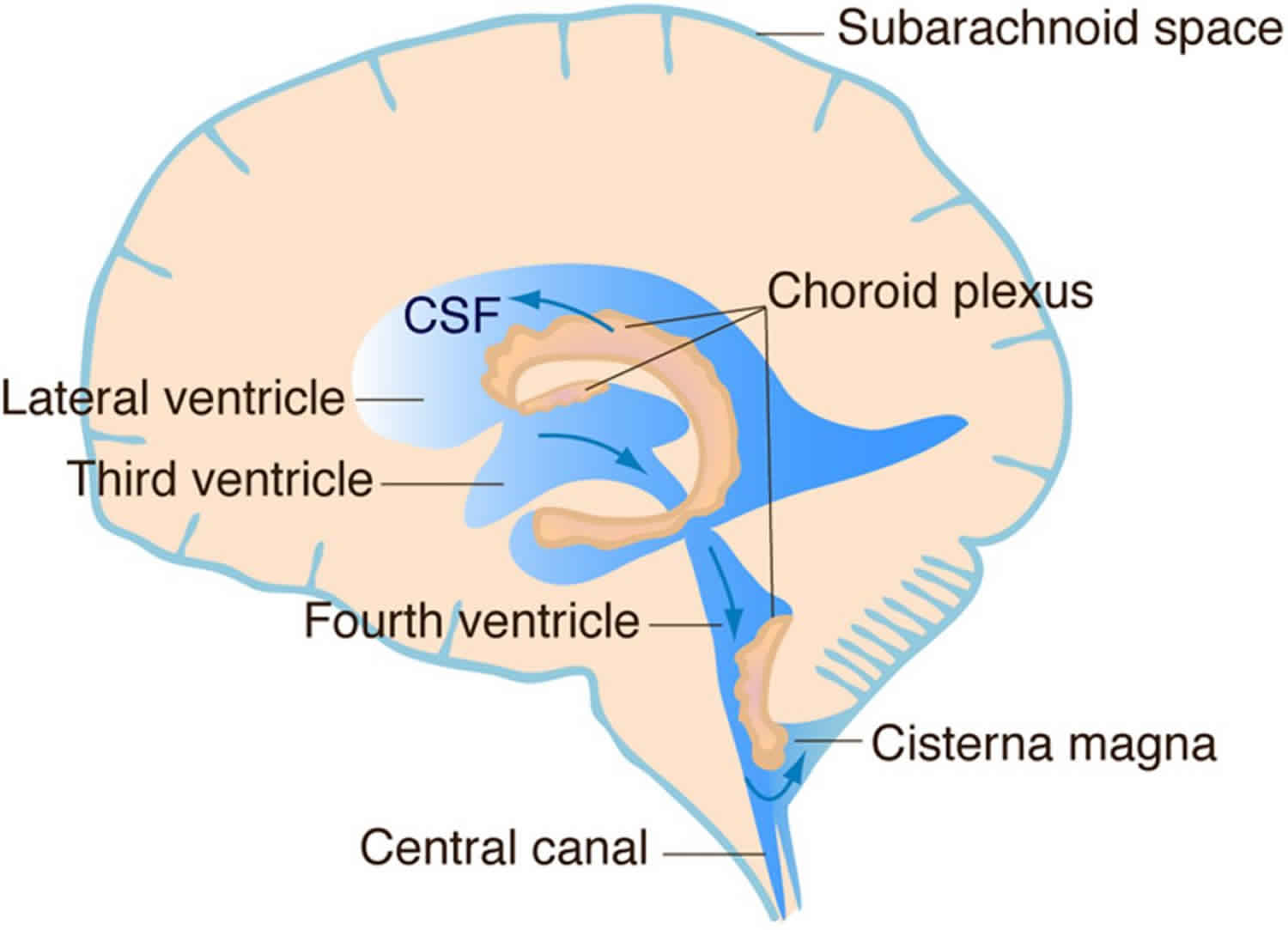
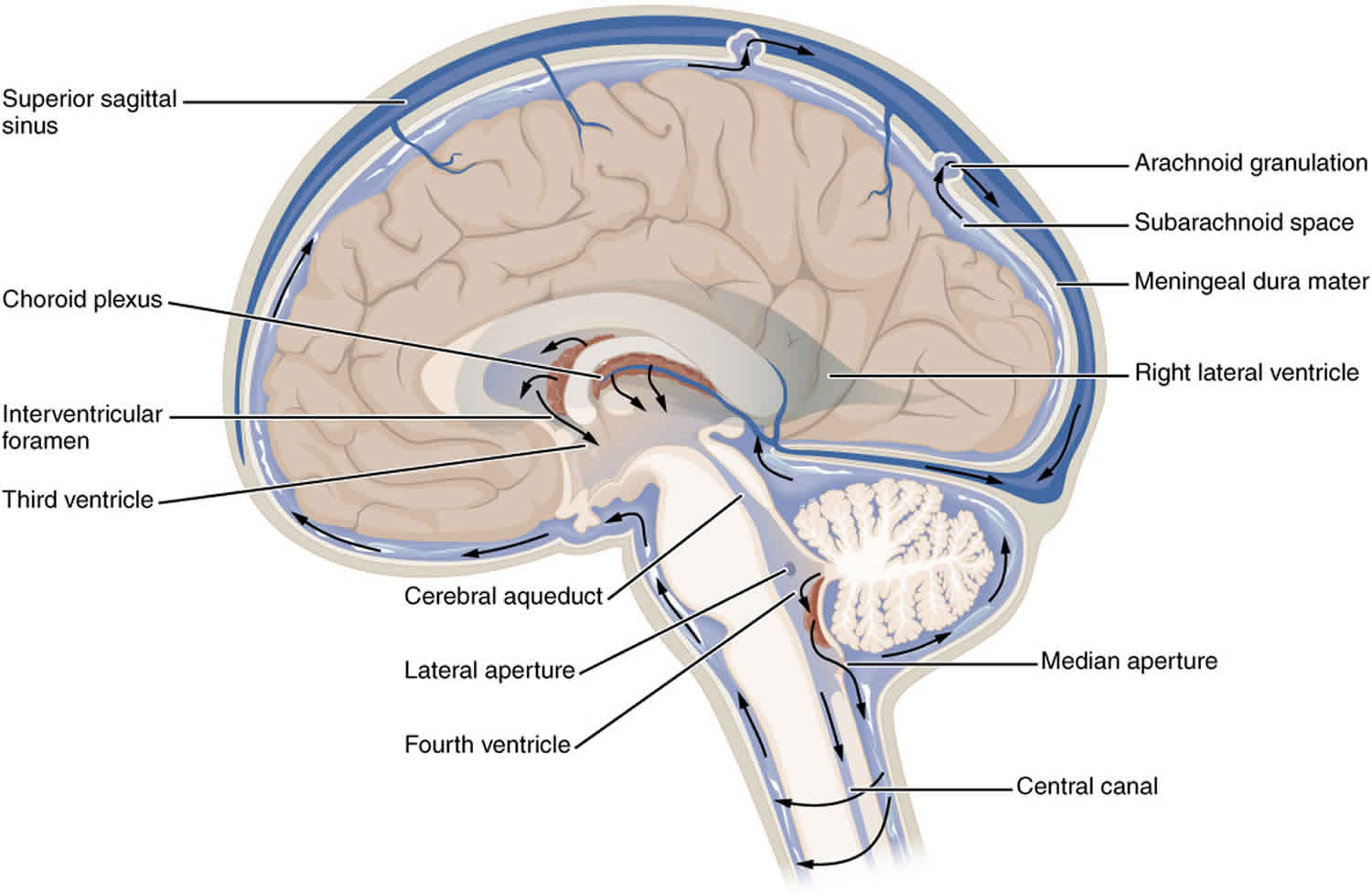
Cerebrospinal fluid (CSF) is a clear protein- and glucose-rich liquid in the subarachnoid space of the central nervous system. CSF is found in the ventricles, surrounding the brain, and within the central spinal column. It has been estimated that there is approximately 125 mL to 150 mL of CSF in the body at any given time 1. However, it should be noted that CSF is continuously generated and reabsorbed. Depending on the rate of production and absorption (which varies person to person), the supply of CSF can be replaced about every 7.5 hours. CSF regulates central nervous system temperature, cushions the brain and spinal cord, and provides a delicately balanced buoyant force that allows the brain to retain its shape and circulatory integrity despite its weight and lack of intrinsic rigid support 1. A leak in this system, therefore, can be detrimental to brain blood supply and function and can increase the risk of direct trauma to brain parenchyma due to loss of fluid cushion. Additionally, the presence of CSF leak indicates the need for further evaluation and management as it may be due to a frontobasilar or temporal skull fracture. Open communication of the subarachnoid space with CSF leak presents a pathway for life-threatening CNS infection including meningitis.
Figure 1. CSF circulaton
CSF rhinorrhea causes
A CSF rhinorrhea can occur whenever there is open communication between the subarachnoid space and other spaces via meningeal disruption. The most common cause of leaking cerebrospinal fluid is a structural compromise secondary to craniofacial trauma, making up 80% of CSF rhinorrhea. Iatrogenic causes make up 16% of CSF rhinorrhea, with the last 4% of CSF rhinorrhea due to varied causes, including spontaneous leak and congenital defects 2.
Craniofacial trauma can lead to varied presentations of CSF rhinorrhea, determined primarily by injury location and mechanism of action. Anterior skull base fractures are frequently associated with moderate-to high-velocity impact. They are, thus, more commonly associated with CSF leak compared to injuries to other locations due to the generally more extensive force of trauma, such as involvement in a motor vehicle accident. The cribriform plate, ethmoid bone, and frontal and sphenoid sinuses are thin and closely associated with the dura. Thus, trauma can easily disrupt both osseous structures and dura. Less frequently, fractures of the temporal bone are associated with dural disruption which can also result in CSF leak. Rarely, injury and disruption to the orbit can result in CSF occulorrhea 3.
Iatrogenic CSF rhinorrhea occur most frequently as complications to functional endoscopic sinus surgery with the cribriform plate and ethmoid bone being the most commonly injured, followed by the frontal and sphenoid sinuses 4. Neurosurgical interventions also contribute to iatrogenic CSF rhinorrhea, especially with the increased prevalence of endoscopic transnasal pituitary surgeries. In one study, pituitary tumor resection made up nearly half of cases where tumor removal led to confirmed CSF rhinorrhea 4. Spinal CSF leaks may also occur after certain procedures such as lumbar punctures, epidural anesthesia, or spinal surgery.
The growth of benign tumors does not commonly result in CSF rhinorrhea. However, locally aggressive lesions such as inverted papilloma and malignant neoplasms can erode the bone of the anterior cranial fossa. The enzymatic breakdown or destruction of the bony architecture results in inflammation and potential violation of the dura. Even if the tumor itself does not lead to CSF rhinorrhea, the resection typically results in immediate leakage. Hence, the surgical team should be prepared to repair the resulting CSF leak at the time of the resection, either transcranially or endoscopically.
Spontaneous CSF rhinorrhea occurs without an obvious inciting event. Increasingly, spontaneous CSF rhinorrhea are attributed to underlying conditions that result in increased intracranial pressure (ICP) such as idiopathic intracranial hypertension [idiopathic intracerebral hypertension -pseudotumor cerebrii)]. This condition is frequently associated with obesity and female sex; In some studies, 60-70% of subjects presenting with spontaneous leak were female and BMI was overweight or obese; in two studies the mean BMI was approximately 35 5. These CSF rhinorrhea were most likely secondary to erosion of thin bony structures discussed above due to chronically increased intracranial pressure.
Congenital CSF rhinorrhea. Defects in the closure of the anterior neuropore can result in the herniation of central nervous tissue through anterior cranial fossa. These are infrequently associated with CSF rhinorrhea. The embryologic defect is typically a patent fonticulus frontalis or foramen cecum. Meningoencephaloceles usually present in childhood as an intranasal/extranasal mass that transilluminates and expands with crying (Furstenberg sign). A high index of suspicion should be maintained with all pediatric intranasal masses, particularly those occurring at the midline. A biopsy should never be obtained unless a complete imaging workup has been conducted.
CSF rhinorrhea symptoms
As most CSF leaks are secondary to either accidental trauma or iatrogenic causes, the history of a patient presenting with rhinorrhea or otorrhea should raise suspicion for CSF leak; thus one should obtain a recent history of trauma or a surgical procedure. The most common presenting symptom across all causes is clear rhinorrhea that may be accompanied by a headache. In those with spontaneous leaks, presentation frequently includes a pressure-like headache that may be positional in nature as well as pulsatile tinnitus 6. On occasion, the patient has a history of headache relieved by drainage of CSF. Drainage may be intermittent as the fluid accumulates in one of the paranasal sinuses and drains externally with changes in head position (ie, reservoir sign).
Delayed fistulas are difficult to diagnose and can occur years after the trauma or operation. These cases often lead to a misdiagnosis of allergic and vasomotor rhinitis.
A history of headache and visual disturbances suggests increased intracranial pressure. Sometimes, associated symptoms can assist in localizing the leak. For example, anosmia (present in 60% of individuals with post-traumatic rhinorrhea), indicates an injury in the olfactory area and anterior fossa, especially when it is unilateral. Optic nerve deficits suggest a lesion in the region of tuberculum sellae, sphenoid sinus, or posterior ethmoid cells. Patients with recurrent meningitis, especially pneumococcal meningitis, should be evaluated for a defect that exposes the intracranial space to the upper airway, regardless of the presence or absence of CSF rhinorrhea.
CSF rhinorrhea diagnosis
Physical examination should include complete rhinologic (including endoscopic), otologic, head and neck, and neurologic evaluations. Endoscopy may reveal an encephalocele or meningocele. Drainage of CSF in some cases may often be elicited on endoscopy by having the patient perform a Valsalva maneuver or by compressing both jugular veins (Queckenstedt-Stookey test). However, most of the time physical examination is unrevealing, especially in patients with intermittent CSF rhinorrhea.
In patients with head trauma, a mixture of blood and CSF may make the diagnosis difficult. CSF separates from blood when it is placed on filter paper, and it produces a clinically detectable sign: the ring sign, double-ring sign, or halo sign. However, the presence of a ring sign is not exclusive to CSF and can lead to false-positive results 7. In contrast to unilateral rhinorrhea, bilateral rhinorrhea gives no clue of the laterality of the defect. However, even in this situation, exceptions can occur. Paradoxical rhinorrhea occurs when midline structures that act as separating barriers (eg, crista galli, vomer) are dislocated. This dislocation allows CSF to flow to the opposite side and manifest at the contralateral naris. The clinical findings most frequently associated with CSF rhinorrhea are meningitis (30%) and pneumocephalus (30%).
CSF rhinorrhea test
Evaluation of a suspected leak should include testing of rhinorrhea or otorrhea for beta-2 transferrin, a compound found only in CSF and perilymph making it a highly specific and sensitive test. If negative, there is a low likelihood of a leak 8.
Glucose testing of rhinorrhea liquid was more frequently done in the past but has poor sensitivity and specificity when compared to beta-2 transferrin. Beta-2 transferrin is currently single best laboratory test for identifying the presence of CSF in sinonasal fluid. It should be kept in mind, however, that beta-2 transferrin test does not provide information regarding the site or laterality of the defect. Not all centers are capable of testing fluid for beta2-transferrin; therefore, sending the laboratory specimen out for processing may delay diagnosis.
Beta-2 transferrin is produced by neuraminidase activity within the central nervous system. Therefore, beta-2 transferrin is located only within the CSF, perilymph, and aqueous humor. The assay has a high sensitivity and specificity, it is performed rapidly, and it is noninvasive 9. A minimum of 0.5 mL of fluid is necessary for electrophoresis, but difficulties in collection of this fluid have been noted, especially in intermittent, low-volume leaks. Beta-2 transferrin is stable at room temperature for approximately 4 hours; therefore, immediate refrigeration following collection is recommended. Specimens should not be frozen.
Beta-trace protein also known as prostaglandin D synthase, this protein is synthesized primarily in arachnoid cells, oligodendrocytes, and the choroids plexus within the central nervous system (CNS). Beta-trace protein is also present in the human testes, heart, and serum. It is altered by the presence of renal failure, multiple sclerosis, cerebral infarction, and certain CNS tumors. This test has been used to diagnose CSF rhinorrhea in multiple studies, with a sensitivity of 92% and specificity of 100%. Beta-trace protein test is not specific for side or site of leak and can be difficult to collect if the leak is intermittent.
If beta-transferrin is positive during an acute leak or if there is a high index of suspicion, imaging is indicated to localize the source. High-resolution CT of paranasal sinuses and temporal bone is typically sufficient for identifying single osseous defects. If multiple defects are suspected on high-resolution CT, CT cisternography is useful to localize the lesions further If initial CT is suspicious for meningoencephalocele, magnetic resonance cisternography is highly sensitive for soft tissue findings. If the leak is intermittent but active, high-resolution CT is still the first line imaging test of choice, but if the suspected leak is inactive at the time of imaging, consider contrast-enhanced MR cisternography or radionucleotide cisternography 10.
In cases of chronic CSF leak or intracranial hypotension, MRI of the brain may show intracranial pachymeningeal thickening and enhancement with contrast, subdural fluid collections, and downward displacement of the brain. MRI of the spine can also show dural collapse and may demonstrate CSF leakage from spinal dural defects 11.
CSF rhinorrhea treatment
Cases of csf rhinorrhea are managed according to their cause. In cases of craniofacial trauma, it has been posited that since a number of these resolve with no intervention that conservative management and observation should be employed. However, the risk of developing meningitis in these patients is up to 29%, so this course should be pursued with caution 12. For cases of spontaneous leak due to elevated intracranial pressures, multiple therapies have been employed. These include acetazolamide, the use of lumbar shunts or repeat lumbar punctures to lower intracranial pressure, endoscopic repair, and in cases of refractory or particularly high intracranial pressure, ventriculoperitoneal (VP) shunts. VP shunts can be effective but have relatively high complication rates 4.
In cases of iatrogenic injury during intracranial surgery, the obvious treatment is repair of the affected site which may require multiple procedures to fix 13. In cases with basilar skull fractures that are surgically managed, an endonasal endoscopic approach has a first attempt success rate ranging from 80 to 91%. The remaining cases may need further endoscopic revision with less than 10% of cases requiring open surgical revision 5. Overall success rates range from 99 to 100% 5. The surgical failure rate is higher among those with elevated intracranial pressure 14.
CSF rhinorrhea prognosis
Overall prognosis of CSF leak is very favorable, with one study citing 90% first attempt success rate of endoscopic repair of CSF rhinorrhea, and another study citing an overall success rate of 98% across traumatic, iatrogenic, and congenital causes 15.
Long-term outcomes following endoscopic repair have been well described. Various authors have concluded that most recurrent leaks manifest within 2 years after the repair. The overall success of the repair is determined by the etiology of the leak, with higher failure rates among patients with increased intracranial pressure. Spontaneous leaks recur in an average of 7 months, while traumatic leaks recur in an average of 4 months. Half of the traumatic leaks recur within 2 weeks postoperatively. This is attributed to a technical error and is unlikely to represent a true recurrence.
A study by Teachey et al indicated that in cases of spontaneous CSF rhinorrhea, evaluation and treatment of the patients for increased intracranial pressure results in a greater success rate for primary endoscopic leak repair. In patient cohorts that underwent such evaluation and treatment (with acetazolamide or CSF shunting), the repair success rate was 92.82%, compared with 81.87% in patients who were not actively managed for increased intracranial pressure 16.
A retrospective study by Adams et al found that in endoscopic repair of CSF rhinorrhea, outcomes were comparable between patients treated on an outpatient basis and those who were admitted to the hospital postoperatively. However, the proportion of small defects (< 1 cm²) was greater among the outpatients, and the operative technique differed significantly between the two groups 17.
- Huff T, Tadi P, Varacallo M. Neuroanatomy, Cerebrospinal Fluid. [Updated 2019 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470578[↩][↩]
- Le C, Strong EB, Luu Q. Management of Anterior Skull Base Cerebrospinal Fluid Leaks. J Neurol Surg B Skull Base. 2016 Oct;77(5):404-11.[↩]
- Baugnon KL, Hudgins PA. Skull base fractures and their complications. Neuroimaging Clin. N. Am. 2014 Aug;24(3):439-65, vii-viii.[↩]
- Banks CA, Palmer JN, Chiu AG, O’Malley BW, Woodworth BA, Kennedy DW. Endoscopic closure of CSF rhinorrhea: 193 cases over 21 years. Otolaryngol Head Neck Surg. 2009 Jun;140(6):826-33.[↩][↩][↩]
- Englhard AS, Volgger V, Leunig A, Meßmer CS, Ledderose GJ. Spontaneous nasal cerebrospinal fluid leaks: management of 24 patients over 11 years. Eur Arch Otorhinolaryngol. 2018 Oct;275(10):2487-2494.[↩][↩][↩]
- Wang EW, Vandergrift WA, Schlosser RJ. Spontaneous CSF Leaks. Otolaryngol. Clin. North Am. 2011 Aug;44(4):845-56, vii.[↩]
- Dula DJ, Fales W. The ‘ring sign’: is it a reliable indicator for cerebral spinal fluid?. Ann Emerg Med. 1993 Apr. 22(4):718-20.[↩]
- Meco C, Oberascher G, Arrer E, Moser G, Albegger K. Beta-trace protein test: new guidelines for the reliable diagnosis of cerebrospinal fluid fistula. Otolaryngol Head Neck Surg. 2003 Nov;129(5):508-17.[↩]
- Oakley GM, Alt JA, Schlosser RJ, Harvey RJ, Orlandi RR. Diagnosis of cerebrospinal fluid rhinorrhea: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2016 Jan. 6 (1):8-16.[↩]
- Hiremath SB, Gautam AA, Sasindran V, Therakathu J, Benjamin G. Cerebrospinal fluid rhinorrhea and otorrhea: A multimodality imaging approach. Diagn Interv Imaging. 2019 Jan;100(1):3-15.[↩]
- Chiapparini L, Ciceri E, Nappini S, Castellani MR, Mea E, Bussone G, Leone M, Savoiardo M. Headache and intracranial hypotension: neuroradiological findings. Neurol. Sci. 2004 Oct;25 Suppl 3:S138-41.[↩]
- Bernal-Sprekelsen M, Bleda-Vázquez C, Carrau RL. Ascending meningitis secondary to traumatic cerebrospinal fluid leaks. Am J Rhinol. 2000 Jul-Aug;14(4):257-9.[↩]
- Platt MP, Parnes SM. Management of unexpected cerebrospinal fluid leak during endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg. 2009 Feb;17(1):28-32.[↩]
- Mirza S, Thaper A, McClelland L, Jones NS. Sinonasal cerebrospinal fluid leaks: management of 97 patients over 10 years. Laryngoscope. 2005 Oct;115(10):1774-7.[↩]
- Daele JJ, Goffart Y, Machiels S. Traumatic, iatrogenic, and spontaneous cerebrospinal fluid (CSF) leak: endoscopic repair. B-ENT. 2011;7 Suppl 17:47-60.[↩]
- Teachey W, Grayson J, Cho DY, Riley KO, Woodworth BA. Intervention for elevated intracranial pressure improves success rate after repair of spontaneous cerebrospinal fluid leaks. Laryngoscope. 2017 Sep. 127 (9):2011-6.[↩]
- Adams AS, Francis DO, Russell PT. Outcomes of outpatient endoscopic repair of cerebrospinal fluid rhinorrhea. Int Forum Allergy Rhinol. 2016 Nov. 6 (11):1126-30.[↩]