Cullen sign
Cullen’s sign is blue-black bruising or irregular hemorrhagic patch of the area around the umbilicus, which is suggestive of intrabdominal bleed 1. Cullen sign appears due to collection of blood in subcutaneous tissue around umbilicus 2. Cullen sign has been described in acute pancreatitis, rectus sheath hematoma, splenic rupture, perforated ulcer, intra-abdominal cancer, and acute ruptured ectopic pregnancy, and as a complication of anticoagulation 3. Cullen’s sign may also be seen in any condition in which there is pigmented peritoneal fluid, such as cases of retroperitoneal bleeds in ectopic endometriosis or acute abdominal aortic aneurysmal rupture 4. Cullen sign is seen in approximately 3 per cent of patients and is associated with a mortality of 37 per cent 1. Clinical evaluation along with biochemical marker of raised amylase and lipase with contrast enhanced CT abdomen showing heterogeneous enhancement of the pancreatic gland with shaggy contour, blurring of peripancreatic fat planes with the presence of intraperitoneal and retroperitoneal fluid collections confirmed the diagnosis of acute pancreatitis.
Cullen’s sign may be accompanied by Grey-Turner’s sign (bruising of the flank). Grey Turner sign refers to bruising of the flanks and may occur in conjunction with Cullen sign, especially in patients with retroperitoneal hemorrhage 5. When Cullen or Grey Turner signs result from acute pancreatitis, they signal severe disease, with a mortality estimate as high as 37% 5.
Fox’s sign (ecchymosis of the upper thigh with a sharply defined superior border paralleling and inferior to the inguinal ligament) and Bryant’s sign (blue discoloration of the scrotum).
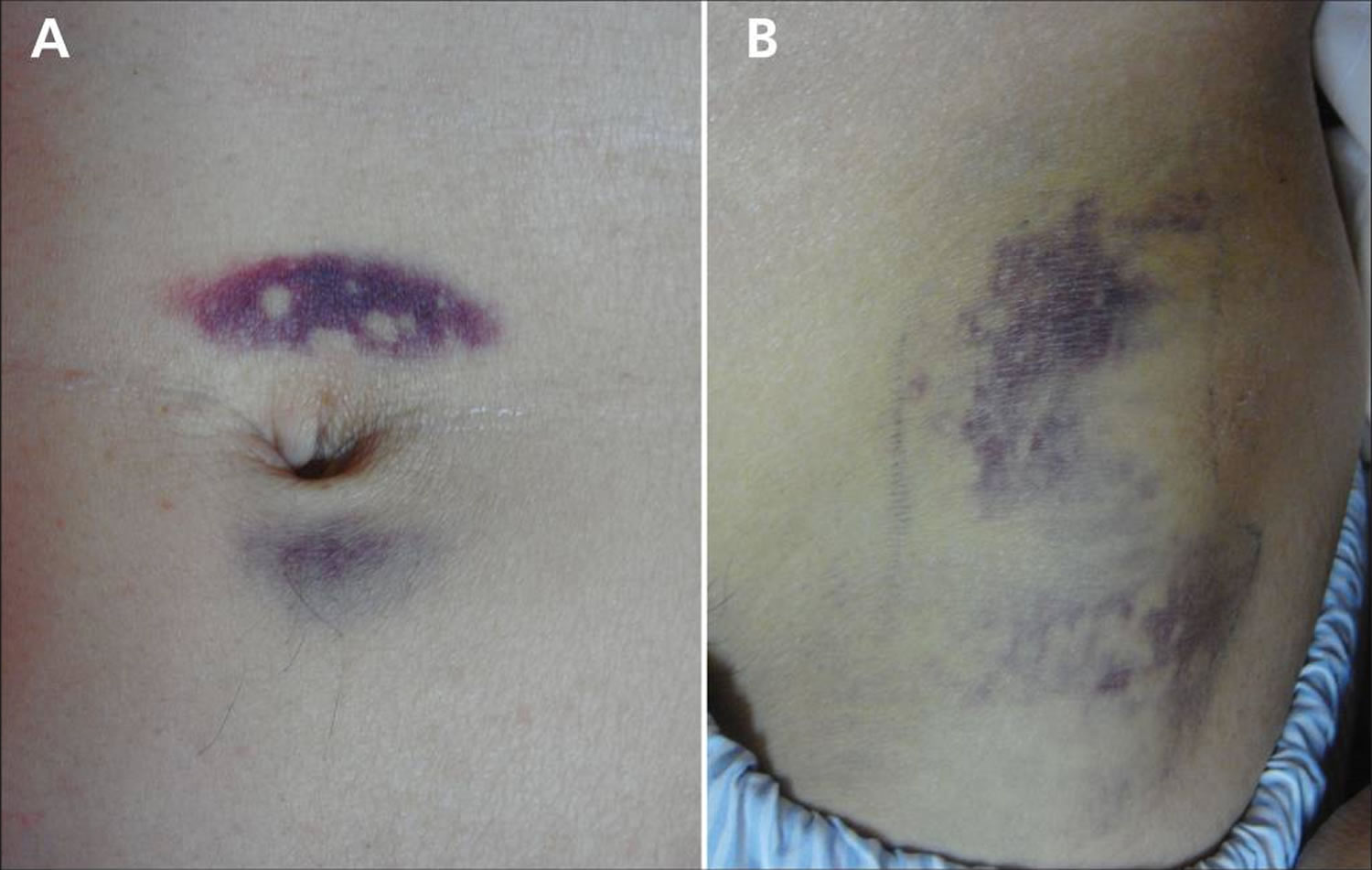
Figure 1. Cullen sign
[Source 1 ]Figure 2. Cullen and Grey Turner sign
Footnote: (A) Periumbilical ecchymosis (Cullen sign) and (B) connecting patches of ecchymosis on the left flank (Grey Turner sign) in a 47-year-old man with sudden onset of left-flank pain.
[Source 6 ]Cullen sign causes
Cullen sign causes include:
- acute pancreatitis, where methaemalbumin formed from digested blood tracks around the abdomen from the inflamed pancreas
- bleeding from blunt abdominal trauma
- bleeding from ruptured ectopic pregnancy
Grey Turner sign
Grey Turner’s sign refers to an uncommon subcutaneous manifestation of intra-abdominal pathology manifesting as ecchymosis or discoloration of the flanks 7. Classically Grey Turner sign is associated with severe acute necrotizing pancreatitis often in association with Cullen’s sign (periumbilical ecchymosis) 8. Grey Turner’s sign may also be seen in many other conditions that result in intra-abdominal or retroperitoneal hemorrhage 8. The discoloration may be green, yellow, or purple depending on the degree of red blood cell breakdown in the abdominal wall tissues and may not occur until several days into the course of an illness.
A careful physical examination, including visualization of the abdominal wall itself in select patients, may show a Grey Turner’s sign suggesting potentially serious intra-abdominal pathology, in particular, intra-abdominal or retroperitoneal bleeding. This may be especially important in the setting of patients who cannot provide an otherwise adequate history or demonstrate abdominal tenderness on examination due to altered mental status or intubation with mechanical ventilation. Additionally, Grey Turner’s sign may guide a clinician to consider retroperitoneal hemorrhage in unstable patients. This is particularly important in an unstable patient with a bedside ultrasound that reveals no intra-abdominal bleeding, given that ultrasonography cannot reliably detect retroperitoneal bleeding 9. Thus, when clinicians are searching for the location of hemorrhage and a clear intra-abdominal source is not present on bedside ultrasonography, a retroperitoneal source may exist and occasionally may produce a Grey Turner’s sign. Although historically associated with severe acute necrotizing pancreatitis Grey Turner’s sign is non-specific and may be present with almost any condition causing intra-abdominal or retroperitoneal bleeding including ruptured abdominal aortic aneurysm, ruptured ectopic pregnancy, splenic rupture, ruptured hepatocellular carcinoma, perforated duodenal ulcer, bleeding intra-abdominal metastases, perirenal hemorrhage, and hemorrhagic ascites among others 10.
In addition to the physical exam finding of flank ecchymosis, CT scanning may reveal a radiographic Grey Turner’s sign. In a review of patients with severe acute pancreatitis who underwent CT imaging, researchers found that radiographic evidence of extension of retroperitoneal fluid collections laterally beyond the aponeurotic layer to the abdominal wall predicted organ failure and death with an overall mortality rate near 40%.
Figure 3. Grey Turner sign
Footnote: Bilateral Grey Turner’s sign. Contrast enhanced CT of the abdomen showing a huge hematoma in the right lateral abdominal wall.
[Source 11 ]Grey Turner sign causes
Classically Grey Turner sign is associated with severe acute necrotizing pancreatitis often in association with Cullen’s sign (periumbilical ecchymosis) 8. Grey Turner’s sign may also be seen in many other conditions that result in intra-abdominal or retroperitoneal hemorrhage 8.
In severe acute pancreatitis, the injured pancreas releases pancreatic enzymes that cause fat necrosis and inflammation occasionally resulting in peri-pancreatic bleeding. The resulting fluid collection can travel via an anatomical defect of the transversalis fascia to the space between the 2 leaves of the renal fascia. It then flows to the pararenal space followed by the lateral edge of the quadratus lumborum muscle and finally to the subcutaneous tissue of the flanks 12. Even in the presence of intra-abdominal or retroperitoneal hemorrhage Grey Turner’s sign may not manifest for several days. In the setting of pancreatitis, it appeared most commonly on day 3 or 4 in some older case series. One review of a case series found that subcutaneous abdominal wall signs of intra-abdominal bleeding occur more commonly in women than men with a ratio of 3:1 13. However, no large well-controlled study exists to confirm this finding.
Researchers have not adequately determined the sensitivity and specificity of Grey Turner’s sign in detecting intra-abdominal or retroperitoneal pathology although sensitivity is almost certainly low. Studies have shown it is an uncommon finding among patients with pancreatitis, present in about 1% 14. Thus, the sensitivity of Grey Turner’s sign in detecting pancreatitis in general likely approaches zero. The sensitivity for detecting severe necrotizing pancreatitis, which has a higher probability of intra-abdominal bleeding, is probably somewhat higher though still too low to rule out the condition. The sensitivity of Grey Turner’s sign for other etiologies of intra-abdominal or retroperitoneal bleeding is unknown though too low to be of clinical utility to rule out pathology. The specificity likely is higher but in isolation the finding predicts only intra-abdominal pathology not any specific diagnosis. Additionally, direct trauma to the flank may cause subcutaneous findings that mimic Grey Turner’s sign but are not associated with intra-abdominal pathology (hence, a false positive Grey Turner’s sign). With these caveats, clinicians should know that when Grey Turner’s sign is present in the absence of known direct trauma to the flank, for example, a patient presenting with non-traumatic abdominal pain, it appears to be a marker of severe illness with a potentially high mortality rate. For example, in one case series 37% of patients with pancreatitis and Grey Turner’s sign succumbed to the disease 13. Nonetheless, a finding of Grey Turner’s sign should lead to a consideration of imaging (generally computed tomography [CT]) to determine the severity of underlying pathology and to reveal unanticipated diagnoses many of which are fatal if not detected and treated early.
- Parikh RP, Upadhyay KJ. Cullen’s sign for acute haemorrhagic pancreatitis. Indian J Med Res. 2013;137(6):1210. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3734730[↩][↩][↩]
- Cullen TS. A new sign in ruptured extrauterine pregnancy. Am J Obstet Gynecol 1918;78:457[↩]
- Harris S, Naina HVK. Cullen’s sign revisited. Am J Med 2008;121:682–3[↩]
- Reuben A. Examination of the abdomen. Clin Liver Dis (Hoboken). 2016;7(6):143–150. Published 2016 Jun 28. doi:10.1002/cld.556 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6490278[↩]
- Mookadam F, Cikes M. Cullen’s and Turner’s signs. N Engl J Med 2005;353:1386.[↩][↩]
- Chung KM, Chuang SS. Cullen and Grey Turner signs in idiopathic perirenal hemorrhage. CMAJ. 2011;183(16):E1221. doi:10.1503/cmaj.101548 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3216450[↩]
- Mookadam F, Cikes M. Images in clinical medicine. Cullen’s and Turner’s signs. N. Engl. J. Med. 2005 Sep 29;353(13):1386.[↩]
- Guldner GT, Magee EM. Grey-Turner Sign. [Updated 2019 Jan 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534296[↩][↩][↩][↩]
- Carnevale-Maffé G, Modesti PA. Out of the blue: the Grey-Turner’s sign. Intern Emerg Med. 2015 Apr;10(3):387-8.[↩]
- Chauhan S, Gupta M, Sachdev A, D’Cruz S, Kaur I. Cullen’s and Turner’s sign associated with portal hypertension. Lancet. 2008 Jul 05;372(9632):54.[↩]
- Fan Z, Zhang Y. Grey Turner’s and Cullen’s signs induced by spontaneous hemorrhage of the abdominal wall after coughing. Ann Surg Treat Res. 2017 Aug;93(2):115-117. doi: 10.4174/astr.2017.93.2.115[↩]
- Sugimoto M, Takada T, Yasuda H, Nagashima I, Amano H, Yoshida M, Miura F, Uchida T, Isaka T, Toyota N, Wada K, Takagi K, Kato K, Takeshita K. MPR-hCT imaging of the pancreatic fluid pathway to Grey-Turner’s and Cullen’s sign in acute pancreatitis. Hepatogastroenterology. 2005 Sep-Oct;52(65):1613-6.[↩]
- Dickson AP, Imrie CW. The incidence and prognosis of body wall ecchymosis in acute pancreatitis. Surg Gynecol Obstet. 1984 Oct;159(4):343-7.[↩][↩]
- Jacobs ML, Daggett WM, Civette JM, Vasu MA, Lawson DW, Warshaw AL, Nardi GL, Bartlett MK. Acute pancreatitis: analysis of factors influencing survival. Ann. Surg. 1977 Jan;185(1):43-51.[↩]