What is cylindroma
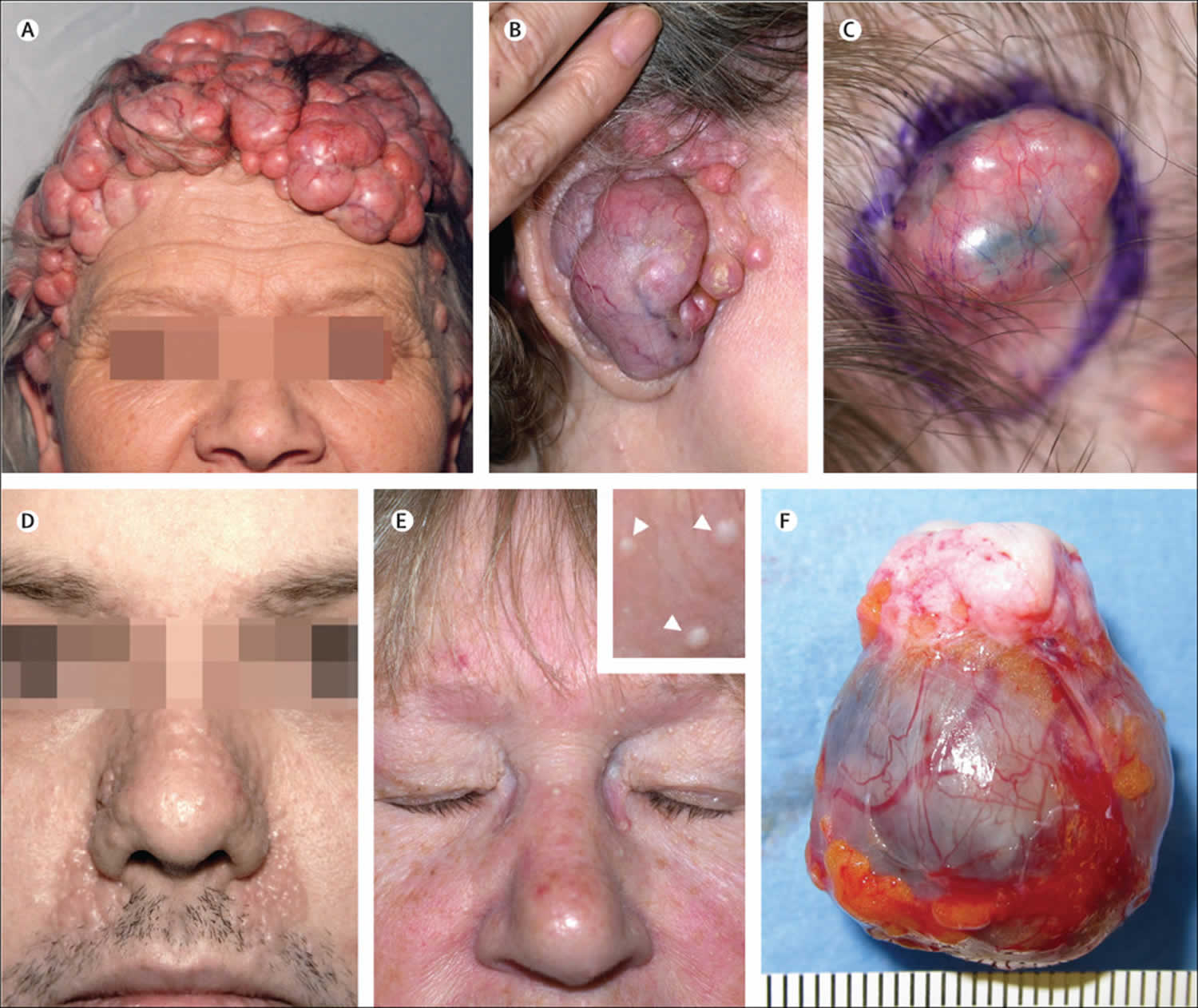
Cylindroma is a rare, slow-growing, benign (non-cancerous) appendage skin tumor that typically present as a skin colored, reddish or bluish smooth-surfaced dome-shaped nodule(s) that may range in size from a few millimeters to several centimeters (Figure 1) 1. Cylindromas are predominantly derived from likely apocrine cells in the dermis within the hair follicle bulge. Apocrine cells are secretory cells in exocrine glands that release a combination of lipids and proteins. They are found in the skin, breast, eyelids, and ears. Exocrine glands are glands that release substances through ducts onto the body’s surfaces. Examples of exocrine glands include sweat glands, lacrimal glands, salivary glands, mammary glands, and digestive glands in the stomach, pancreas, and intestines. Upon cross-sectional examination, cylindromas exhibit a round morphology akin to cylinders, hence their name, reflecting their cylindrical shape 1. Although cylindromas are typically slow-growing, they are generally benign (non-cancerous). However, exceedingly rare instances of malignant transformation and potential metastases have been reported, especially in conjunction with multiple lesions associated with Brooke-Spiegler syndrome 1.
Cylindromas can be seen in conjunction with spiradenomas (a rare, benign tumor that originates from sweat glands in the skin) and trichoepitheliomas (noncancerous tumors that grow from hair follicles) 2, 3. Multiple tumors are observed in an autosomal dominantly inherited manner may be seen in familial autosomal dominant cylidromatosis or Brooke-Spiegler syndrome or multiple familial trichoepitheliomas syndrome (cylindromas, trichoepitheliomas, and spiradenomas) typically appear after puberty with slowly growing and often numerous lesions. Cases of spiradenocylindromas, demonstrating characteristics of both spiradenoma and cylindroma in the same tumor mass, have also been observed, suggesting similar derivation of both tumors 4.
Cylindromas are slow-growing solitary or multiple tumors primarily found on the scalp, head, face and neck of individuals. Cylindromas occur sporadically, are solitary and occasionally painful. Solitary cylindromas occur sporadically and typically are not inherited. When multiple nodules enlarge and coalesce on the scalp, they form the distinctive “turban” tumor feature, creating an appearance reminiscent of headgear like a hat or turban 5, 6.
The incidence of cylindroma is more common in females than in males. Female-to-male ratios of 6:1 and 9:1 have been reported 7.
Solitary cylindromas are lesions that affect middle-aged and elderly persons. Multiple, inherited cylindromas usually begin in early adulthood and increase in size and number throughout life.
Cylindromas are benign but incomplete biopsy/removal may result in local recurrence.
Malignant cylindromas are very rare. Malignant transformation may develop within solitary cylindromas, or they may complicate the multiple variant (more common).
Multiple lesions are disfiguring and require extensive surgical management to restore anatomic appearance. An association with familial autosomal dominant cylindromatosis and basal cell carcinoma has been reported. Brooke-Speigler syndrome has been associated with other cutaneous findings, unilateral hearing loss, and manifesting with pegged teeth.
Figure 1. Cylindroma
[Source 8 ]Figure 2. Cylindroma histopathology
Footnotes: The neoplastic nodules are arranged in a jigsaw puzzle and are composed of monomorphic basaloid cells surrounded by eosinophilic basement membrane material. The cells at the periphery show palisading and are darker than the cells located in the central parts of the nodules
[Source 9 ]Cylindroma causes
Cylindromas may occur either sporadically (nonhereditary cylindroma) or in a familial manner (familial cylindromatosis), and they are generally not attributed to environmental factors 1, 10, 11, 12, 13. Cylindromas are most likely a very primitive sweat gland tumor differentiating toward either the eccrine or apocrine line. The cellular origin of cylindromas remains unknown.
Sporadic cylindromas typically involve solitary lesions 7. Unlike in familial inherited forms (familial cylindromatosis), there is often an expression of MYB-NFIB fusion transcripts in sporadically occurring cylindromas. MYB, an oncogene, fuses with NFIB to form a transcription factor gene, resulting in an oncoprotein that promotes neoplastic processes 14. MYB, when activated or overexpressed, can drive dermal cylindromas by assuming the role typically performed by the MYB-NFIB fusion oncoprotein 14.
Familial cylindromatosis syndromes are associated with mutations in the CYLD tumor-suppressor gene, except for rare exceptions. The CYLD gene was discovered in 2000 and implicated as the causal agent in the 3 inherited cylindromatosis syndromes 7. Of these syndromes, Brooke-Spiegler syndrome is probably the most well-known 7. Brooke-Spiegler syndrome or familial cylindromatosis is characterized by a heterozygous germ-line mutation in the carboxyl-terminal end of the CYLD gene (16q12-q13). The CYLD gene appears to function in tumor-suppressor gene regulation, since tumorigenic epidermal cells have been shown to diminish the deubiquitinating activity of the endogenous CYLD, resulting in increased expression of several angiogenic factors leading to accelerated proliferation and migration of tumoral cells. Brooke-Spiegler syndrome has been described as an autosomal dominant disease characterized by the development of multiple skin appendage tumors such as cylindromas, trichoepitheliomas, and spiradenomas, with a variable preponderance of any of the aforementioned subsets. Other lesions reported with Brooke-Spiegler syndrome include parotid basal cell adenomas, organoid nevi, syringomas, and basal cell carcinomas. Despite variable phenotypic expressions of a predominant tumor in Brooke-Spiegler syndrome, the gene responsible for multiple cylindromas, CYLD, is localized to band 16q12-q13. The mechanism of genotypic similarity and phenotypic variance is not yet understood 15.
Familial cylindromatosis and multiple familial trichoepitheliomas are the other 2 inheritable cylindromatosis syndromes and involve mutations in the CYLD gene. CYLD mutations are inherited in an autosomal dominant pattern but adhere to the 2-hit hypotheses. This necessitates a second gene mutation to occur randomly due to DNA damage to induce a neoplastic change 16.
Although the CYLD gene mutation follows an autosomal dominant pattern, the phenotypic expression of these mutations varies considerably 1. With ongoing discoveries, over 100 mutations have been identified in the CYLD gene 1. The most prevalent mutation occurs on chromosome 16q. However, it remains unclear which mutations will influence specific phenotypic expressions. Even within the same family, affected members often display differing phenotypes 17, 18, 19, 20
In 2006, Zhang et al 21 reported a large consanguineous Chinese family with Brooke-Spiegler syndrome demonstrating intrafamily phenotypic variability. Upon examination, some persons only manifested discrete, small, skin-coloured growths, while the proband manifested an expansion of multiple large growths on the nose and numerous dome-shaped papules on the scalp. Biopsy showed both trichoepitheliomas and cylindromas in the affected persons. By sequence analysis, Zhang et al identified a recurrent mutation 2272C→T (R758X) of the CYLD gene in the affected familial persons that had been previously identified in other ethnic kindreds with familial cylindromatosis.
In 2007, Stegmeier et al 22 noted that the CYLD gene encodes a deubiquitinating enzyme. The enzyme removes Lys-63–linked ubiquitin chains from I-kappaB kinase signaling components. By this mechanism, the enzyme inhibits NF-kappaB pathway activation. They demonstrated that CYLD is also required for the cell’s timely entry into mitosis. Consistent with a cell-cycle regulatory function, CYLD localizes to microtubules in interphase and the midbody during telophase. CYLD ‘s protein levels decrease as cells exit from mitosis. Stegmeier et al identified the protein kinase Plk1 as a potential target of CYLD as a regulator of mitotic entry, and they suggested this because of the physical interaction and similar loss-of-function and over-expression phenotypes.
These findings raise the possibility that, as with other genes that regulate tumorigenesis, CYLD has both tumor-suppressing (apoptosis regulation) and tumor-promoting activities (enhancer of mitotic entry). They suggested that this additional function of CYLD could provide an explanation for the benign nature of most cylindroma lesions.
Massoumi and Paus 23 and explained the manner in which CYLD interferes with tumor necrosis factor-alpha or Toll-like receptor–mediated signaling and with JNK or NF-kappaB-dependent p65/50 signaling to limit inflammation. Additionally, the manner by which CYLD interferes with activation of the proto-oncogene BCL3 and with cyclin D1 expression to limit tumorigenesis was also explained. Finally, the researchers discussed how tumor growth-promoting agents or UV light and inflammatory mediators may activate CYLD.
Researchers have noted a MYB-NFIB gene fusion, which provides a new genetic link between dermal cylindroma and adenoid cystic carcinoma 24.
As of 2012, researchers 25 have identified 68 unique mutations with variable penetrance and expression (which are both intrafamilial and interfamilial) in CYLD. CYLD functions as a putative tumor suppressor gene that encodes for a deubiquitinating enzyme with functions in cell proliferation and inflammation.
In 2013, a major international study 26 noted 86 CLYD mutations in Brooke-Spiegler syndrome and multiple familial trichoepitheliomas syndrome (MFT). Of the 76 tumors from 32 patients with a germline CYLD mutation, 26 were cylindromas, 12 were spiradenomas, 15 spiradenocylindromas, 7 were other tumor types, and 15 were trichoepitheliomas. Causes of mutations included frameshift mutations, nonsense mutations, missense mutations, splice-site mutations, somatic mutations, sequence alteration, and loss of heterozygosity. Sometimes the source of mutations remained unknown. The variability of somatic mutations is underlined by this study.
Down-regulation of CLYD occurred in a case of breast cancer and may be an independent genetic mutation associated with poor prognosis 27.
In a study of 97 tumors, all spiradenomas (27) and cylindromas (30) expressed CD200, while other eccrine (hidradenomas, poromas, dermal duct tumors, and hidroacanthoma simplex) were CD200-negative. CK15 distinguished between spiradenomas and cylindromas. This shows that cylindromas and spiradenomas are follicular tumors; specifically, Sellheyer proposed that both cylindromas and spiradenomas are adnexal neoplasms that were derived from the hair follicle bulge and that therefore cylindromas and spiradenomas represent the least differentiated follicular tumors 28.
Brooke-Spiegler syndrome with a new nonsense germline proband mutation of CYLD (c.1783C>T pGln 595*) has been noted 29.
Cylindroma pathophysiology
The pathogenesis of cylindromas is not yet well understood, and there are multiple theories regarding its origin 30. A follicular epithelium lineage is often defended as the tumor develops exclusively in hair-covered areas 31. The cells within the cylindroma also have exhibited expression of follicular keratin 2. However, many experts maintain that cylindroma’s origins are eccrine or apocrine differentiation, although some cytologic studies argue against the eccrine origin 2. Cylindromas do not develop on soles of feet or palms of hands, which contradicts an eccrine lineage hypothesis, as these areas contain numerous eccrine glands but lack hair follicles or apocrine glands. The more differentiated cells forming cylindromas exhibit morphological similarities to secretory cells, leading some to argue for the apocrine origin of cylindromas 10, 11.
Cylindroma histology
Cylindroma is a dermal tumor without attachment to the epidermis. The lesion is composed of numerous oval and polygonal nests molded into a jigsawlike pattern. Masses of epithelial cells are surrounded and penetrated by a hyaline sheath closely resembling a basement membrane. This sheath separates the tumor from the dermal mesenchyme, yet does not interfere with tumor growth and proliferation.
Malignant cylindromas demonstrate islands of cells displaying marked anaplasia and pleomorphism of nuclei. Mitoses are increased and are abnormal. Besides invasion into surrounding tissue, loss of the delicate hyaline sheath occurs.
Tumor islands are composed of 2 cell types. Peripheral cells are small and highly basophilic; palisading is suggested. Larger, more pale-staining cells are seen centrally. Small tubal lumina are sometimes found with careful observation.
A lack of lymphoid tissue is a histological feature that differentiates cylindromas from spiradenomas. Spiradenomas show a unique prominent presence of lymphocytes. Cylindromas, on the other hand, demonstrate a large number of prominent dendritic cells that most likely represent Langerhans cells that permeate the tumor. S-100 protein–, HLA-DR–, and CD1a-positive cells can be seen in cylindromas and represent the existence of Langerhans cells.
Hyaline bands, which surround tumor islands, are mostly composed of type IV collagen. This is equivalent to the subepidermal lamina densa. Fragments of anchoring fibrils, identical to type VII collagen, are also seen. These anchoring fibrils can also be seen embedded in basement membrane on electron microscopy (EM).
The hyaline membrane is highly enlarged compared with the dermoepidermal junction, as observed by electron microscopy. Electron microscopy demonstrates a basement membrane of 2.7-4.3 µm, compared with the dermoepidermal junction average basement membrane thickness of 60-90 nm. Electron microscopy also demonstrates that cylindromas lack clear distinction of lamina densa. Numerous abnormal inclusions of fibrillar material are noted and appear similar to lamina lucida.
Although hemidesmosomes (HDs) are seen with electron microscopy, they are irregularly spaced and can only be seen in high power, compared with normal basal keratinocytes, in which hemidesmosomes are seen at low power. Hemidesmosomes noted in the cylindroma cells have greater size variation and half the normal number of basal keratinocytes.
Immunohistochemical studies on cylindromas demonstrate a variation in cell matrix proteins compared with normal epidermal basal keratinocytes. Alpha-6-beta-4 integrin expression in tumor cells is weaker. In normal basal keratinocytes, laminin-5 is understood as necessary for hemidesmosome and basement membrane formation. Further studies have shown an improper processing of laminin-5 in cylindromas. This may explain the lower percentage of hemidesmosomes in cylindromas. Cylindromas also demonstrate low expression of alpha-6-beta-4 integrins. These changes may be the cause the structural abnormalities seen in the basement membranes of cylindromas.
Immunohistochemical analysis has demonstrated myoepithelial, apocrine, eccrine, ductal, and secretory features in both cylindromas and spiradenomas. Alpha-SMA, indicating myoepithelial differentiation, has been shown to be expressed in the basaloid cells of both tumors. Both tumors also demonstrate S-100 protein expression, a marker designating eccrine differentiation and apocrine markers, human milk fat globulin, and lysozyme. In addition, expression of keratin polypeptides 10 and 14, specific for ductal epithelium, and keratins 7, 8, and 18, specific for secretory cells, have been observed in both cylindromas and spiradenomas.
Nerve growth factor, S-100 protein, CD44, and CD34 are other markers that have been found to be expressed in or surrounding eccrine coils and are not expressed in the eccrine duct or apocrine gland. These markers have all been found to varying degrees in cylindromas. Other immunohistochemical studies linking cylindromas to eccrine differentiation include positive expression of cytokeratins 19 and 1/10/11. IKH-4 is a monoclonal antibody specific for the eccrine gland and will not stain apocrine glands. This marker can also be used to differentiate eccrine from apocrine tumors and is positive in eccrine cylindromas and spiradenomas 32.
Immunohistochemical studies linking cylindromas to apocrine differentiation include the expression of alpha-1-antichymotrypsin, alpha smooth muscle actin (1A4), and cytokeratins 8 and 18.
Staining for cytokeratin 15, a marker specific for hair follicle stem cells, has also been shown in some cylindromas and spiradenomas. The expression of follicular, apocrine, and eccrine features in cylindromas suggests that the tumor may be derived from epithelial stem cells of immature differentiation.
Markers expressed in cylindromas and both eccrine and apocrine glands include epithelial membrane antigen, carcinoembryonic antigen, mucinlike carcinoma-associated antigen (B12), laminin, collagen IV, fibronectin, and CD34(QBEND/10).
Cylindroma signs and symptoms
Solitary cylindromas are usually sporadic and not familial, present as slow-growing, painless, round nodular lesions 14. They are sometimes pedunculated. Solitary lesions usually occur in older populations and do not usually grow larger than one centimeter 14. They are rarely painful or tender and may have a pinkish or tan coloring with a smooth surface. Small superficial blood vessels may be visualized. These lesions are most likely to occur on the scalp, and they are seen across the head and neck, with some reports showing the development of these lesions in the nasal area or along ducts, such as the parotid duct; importantly, however, there are reports of these lesions on the trunk and other areas on the body related to apocrine ductal differentiation, which is the presumed source of these neoplastic cells 33, 34
Multiple cylindromas will usually occur in the setting of a familial syndrome and develop much earlier in life 14. When occurring in multiples, these lesions require excisions for treatment and re-excisions later in life as they can recur or progress into cancers 35. Also, in syndromic patients, the cylindromas may exhibit accelerated growth and reach sizes over 20 centimeters in some cases. As they grow this large, they often will ulcerate and become painful 36.
90 percent of cylindromas occur in the head and neck region 1, 14. They also can occur on the trunk and extremities, but the palms and soles are spared 1. A family history of multiple cylindromas should be helpful in aiding the diagnosis 1. The development of multiple lesions should be cautiously suggestive of Brooke-Spiegler syndrome, an autosomal dominant condition involving mutations in the CYLD gene causing multiple tumors 37.
Cylindroma complications
Complications associated with cylindromas typically arise from surgical intervention and include bleeding, scarring, recurrence, pain, and the potential necessity for further procedures 1. In familial cases, where lesions may be large and multiple, there could be disfigurement or pain. However, most studies suggest a low post-removal recurrence rate, indicating that the lesions tend not to recur once excised 38.
Cylindroma diagnosis
Dermatoscopic examination of cylindromas demonstrates arborizing telangiectasia and scattered white globules on a background of white to salmon-pink. The vascular branches appear more pronounced when examined at the periphery. The vascular branches extend from the periphery into the center of the cylindroma 39.
Biopsy is required to confirm the diagnosis and to histologically characterize the neoplasm. Light microscopy with ordinary hematoxylin and eosin (H&E) staining is sufficient for diagnosis of cylindroma. Histologically, angular and ovoid dermal islands composed of an inner larger basaloid polygonal cell population and outer small round cell population are delineated from the stroma by a basement membrane and are arranged in a mosaic or jigsaw pattern. Lobules may contain hyaline deposits and small tubular lumina.
Cylindromas are distinguished microscopically from basal cell carcinomas, which contain irregular basaloid lobules with peripheral palisading of nuclei, often with a connection to the epidermis, that have artifactual retractions from a mucinous stroma on sun-damaged skin. Cylindromas may have similar cytologic features similar to those of spiradenomas; however, the rounded tumor lobules in spiradenomas often contain a vascular stroma containing lymphocytes and lack the mosaic pattern.
A breast cylindroma that displays MYB expression is a benign tumor, with CYLD gene mutations differing from an adenoid cystic carcinoma. In the breast, the diagnosis of a benign cylindroma was made using reverse-transcription polymerase chain reaction, fluorescence in situ hybridization, whole-exome sequencing, immunohistochemistry, and revealing a MYB-NFIB fusion gene absence and decreased levels of expression of MYB protein with a clonal somatic CYLD splice site mutation accompanying a wild-type allele linked with an absence of heterozygosity showing a benign cylindroma 40.
Cylindroma differential diagnosis
Trichoepitheliomas (noncancerous tumors that grow from hair follicles) and spiradenomas (a rare, benign tumor that originates from sweat glands in the skin) appear similar and often occur simultaneously 1.
Trichoepitheliomas are differentiated from cylindromas by the presence of horn cysts 41.
Spiradenomas can prove exceedingly difficult to differentiate from cylindromas in some cases. Within a spiradenoma, populations of basaloid cells may appear indistinguishable from a cylindroma 42. Spiradenomas will often appear more circumscribed and nodular than cylindromas. Spiradenomas are typically solitary lesions that often exhibit intermittent pain and are tender to palpation, as opposed to the majority of cylindromas, which are painless. A thorough histopathological examination of the entire lesion is vital under challenging cases to differentiate between cylindromas and spiradenomas 43.
Cylindromas may transform into malignant versions in rare cases 44. Malignant cylindromas are more frequently associated with Brooke-Spiegler Syndrome. The malignant form exhibits more rapid growth, atypical and asymmetrical architectural features, and an invasive pattern of growth 41. Cytological features may include nuclear pleomorphism and crowding, loss of the characteristic jigsaw puzzle pattern, loss of intervening hyaline sheaths, loss of the biphasic cell population, and development of necrosis. Malignant cylindromas exhibit aggressive local infiltrative growth patterns and have been known to metastasize. Immunohistochemical stains do not help differentiate between benign or malignant lesions 20, 10.
Cylindroma treatment
For solitary lesions, the treatment of choice is surgical excision 44. Large lesions should be imaged before planning treatment to determine vascularity and involvement of surrounding tissues, including underlying osseous structures. Pretreatment embolization is vital in patients with large and multiple cylindromas to minimize intraoperative blood loss, as they can be quite vascular lesions.
Other treatments include electrodesiccation/curettage and cryotherapy 45.
For small cylindromas, the carbon dioxide laser may be used 46. Retamar et al 47 used carbon dioxide laser to treat facial trichoepitheliomas in 2 patients, with good results.
Multiple cylindromas usually require extensive plastic surgery that may be obviated by progressively excising a group of nodules in multiple procedures.
Long-term monitoring
Follow-up care of patients with multiple cylindromas is recommended because of the tendency for new lesions to develop 44. Follow-up care is also recommended because of the risk of malignant degeneration 44. Topical aspirin has been utilized to prevent recurrence after excision 1.
Cylindroma prognosis
Most cylindromas are benign but some are malignant and potentially lethal; at least 14 reports have described malignant transformation 48. Malignant cylindromas are more commonly associated with Brooke-Spiegler Syndrome. The malignant variant typically demonstrates rapid growth, atypical and asymmetrical architectural features, and an invasive growth pattern 48. Malignant cylindromas demonstrate aggressive local infiltrative growth patterns and have been known to metastasize. The prognosis is not good with malignancy because visceral metastasis frequently follows. Immunohistochemical stains do not aid in differentiating between benign and malignant lesions 20, 10.
Multiple cylindromas can cover the entire scalp and cause the disfiguring turban tumor appearance, which necessitates extensive reconstructive surgery.
Additionally, there have been documented cases where cylindromas evolved into adenoid cystic carcinoma or spread to dangerous sites, such as malignant nasal cylindroma, or invasion into the lacrimal sac 16.
Cytological features of malignant cylindromas may include nuclear pleomorphism and crowding, loss of the characteristic jigsaw puzzle pattern, loss of intervening hyaline sheaths, loss of the biphasic cell population, and the development of necrosis 48.
- Myers DJ, Sathe NC, Fillman EP. Cylindroma. [Updated 2024 Mar 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482127[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Sellheyer K. Spiradenoma and cylindroma originate from the hair follicle bulge and not from the eccrine sweat gland: an immunohistochemical study with CD200 and other stem cell markers. J Cutan Pathol. 2015 Feb;42(2):90-101. doi: 10.1111/cup.12406[↩][↩][↩]
- Mahalingam M, Srivastava A, Hoang MP. Expression of stem-cell markers (cytokeratin 15 and nestin) in primary adnexal neoplasms-clues to etiopathogenesis. Am J Dermatopathol. 2010 Dec;32(8):774-9. doi: 10.1097/DAD.0b013e3181dafd8c[↩]
- Revis P, Chyu J, Medenica M. Multiple eccrine spiradenoma: case report and review. J Cutan Pathol. 1988 Aug;15(4):226-9. doi: 10.1111/j.1600-0560.1988.tb00549.x[↩]
- Albores-Saavedra J, Heard SC, McLaren B, Kamino H, Witkiewicz AK. Cylindroma (dermal analog tumor) of the breast: a comparison with cylindroma of the skin and adenoid cystic carcinoma of the breast. Am J Clin Pathol. 2005 Jun;123(6):866-73. doi: 10.1309/CRWU-A3K0-MPQH-QC4W[↩]
- Chauhan DS, Guruprasad Y. Dermal cylindroma of the scalp. Natl J Maxillofac Surg. 2012 Jan;3(1):59-61. doi: 10.4103/0975-5950.102163[↩]
- Löser C, Rütten A, Dippel E. Zylindrome – selten aber eindrucksvoll [Cylindromas-rare but striking]. Hautarzt. 2019 Sep;70(9):677-683. German. doi: 10.1007/s00105-019-4458-9[↩][↩][↩][↩]
- Inherited cylindromas: lessons from a rare tumour. The Lancet Oncology Volume 16, ISSUE 9, Pe460-e469, September 01, 2015 https://doi.org/10.1016/S1470-2045(15)00245-4[↩]
- Kazakov DV. Brooke-Spiegler Syndrome and Phenotypic Variants: An Update. Head Neck Pathol. 2016 Jun;10(2):125-30. doi: 10.1007/s12105-016-0705-x[↩]
- Son JH, Choi YW, Cho YS, Byun YS, Chung BY, Cho HJ, Kim HO, Park CW. A Case of Eccrine Spiradenoma: A Rarely Seen Soft Tissue Tumor on the Extensor Surface of Arm. Ann Dermatol. 2017 Aug;29(4):519-522. doi: 10.5021/ad.2017.29.4.519[↩][↩][↩][↩]
- Massoumi R, Podda M, Fässler R, Paus R. Cylindroma as tumor of hair follicle origin. J Invest Dermatol. 2006 May;126(5):1182-4. doi: 10.1038/sj.jid.5700218[↩][↩]
- Nair SP. Soft pink nodules on the scalp. Indian Dermatol Online J. 2015 Sep-Oct;6(5):373-4. doi: 10.4103/2229-5178[↩]
- Manicketh I, Singh R, Ghosh PK. Eccrine cylindroma of the face and scalp. Indian Dermatol Online J. 2016 May-Jun;7(3):203-5. doi: 10.4103/2229-5178.182355[↩]
- Dubois A, Rajan N. CYLD Cutaneous Syndrome. 2020 Apr 16. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555820[↩][↩][↩][↩][↩][↩]
- Bowen S, Gill M, Lee DA, et al. Mutations in the CYLD gene in Brooke-Spiegler syndrome, familial cylindromatosis, and multiple familial trichoepithelioma: lack of genotype-phenotype correlation. J Invest Dermatol. 2005 May. 124(5):919-20.[↩]
- Schittkowski M, Stropahl G, Timm A, Guthoff R. Tränennasenwegsstenose durch ein Zylindrom – Beschreibung einer ungewöhnlichen Tumormanifestation und Literaturüberblick [Nasolacrimal duct obstruction caused by a cylindroma. Report of an atypical tumor manifestation and review of the literature]. Klin Monbl Augenheilkd. 2002 Aug;219(8):602-8. German. doi: 10.1055/s-2002-34424[↩][↩]
- Dubois A, Hodgson K, Rajan N. Understanding Inherited Cylindromas: Clinical Implications of Gene Discovery. Dermatol Clin. 2017 Jan;35(1):61-71. doi: 10.1016/j.det.2016.08.002[↩]
- Dhir G, Makkar M, Suri V, Dubey V. Familial dermal eccrine cylindromatosis with emphasis on histology and genetic mapping. Ann Med Health Sci Res. 2013 Nov;3(Suppl 1):S3-6. doi: 10.4103/2141-9248.121207[↩]
- Rajan N, Andersson MK, Sinclair N, Fehr A, Hodgson K, Lord CJ, Kazakov DV, Vanecek T, Ashworth A, Stenman G. Overexpression of MYB drives proliferation of CYLD-defective cylindroma cells. J Pathol. 2016 Jun;239(2):197-205. doi: 10.1002/path.4717[↩]
- Borik L, Heller P, Shrivastava M, Kazlouskaya V. Malignant cylindroma in a patient with Brooke-Spiegler syndrome. Dermatol Pract Concept. 2015 Apr 30;5(2):61-5. doi: 10.5826/dpc.0502a09[↩][↩][↩]
- Zhang G, Huang Y, Yan K, et al. Diverse phenotype of Brooke-Spiegler syndrome associated with a nonsense mutation in the CYLD tumor suppressor gene. Exp Dermatol. 2006 Dec. 15(12):966-70[↩]
- Stegmeier F, Sowa ME, Nalepa G, Gygi SP, Harper JW, Elledge SJ. The tumor suppressor CYLD regulates entry into mitosis. Proc Natl Acad Sci U S A. 2007 May 22. 104(21):8869-74.[↩]
- Massoumi R, Paus R. Cylindromatosis and the CYLD gene: new lessons on the molecular principles of epithelial growth control. Bioessays. 2007 Dec. 29(12):1203-14.[↩]
- Fehr A, Kovács A, Löning T, Frierson H Jr, van den Oord J, Stenman G. The MYB-NFIB gene fusion-a novel genetic link between adenoid cystic carcinoma and dermal cylindroma. J Pathol. 2011 Jul. 224(3):322-7[↩]
- Trufant J, Robinson M, Patel R. Brooke-Spiegler syndrome. Dermatol Online J. 2012 Dec 15. 18(12):16.[↩]
- Grossmann P, Vanecek T, Steiner P, et al. Novel and Recurrent Germline and Somatic Mutations in a Cohort of 67 Patients From 48 Families With Brooke-Spiegler Syndrome Including the Phenotypic Variant of Multiple Familial Trichoepitheliomas and Correlation With the Histopathologic Findings in 379 Biopsy Specimens. Am J Dermatopathol. 2013 Feb. 35(1):34-44[↩]
- Hayashi M, Jono H, Shinriki S, Nakamura T, Guo J, Sueta A, et al. Clinical significance of CYLD downregulation in breast cancer. Breast Cancer Res Treat. 2014 Jan 8.[↩]
- Sellheyer K. Spiradenoma and cylindroma originate from the hair follicle bulge and not from the eccrine sweat gland: an immunohistochemical study with CD200 and other stem cell markers. J Cutan Pathol. 2014 Oct 29.[↩]
- Pinho AC, Gouveia MJ, Gameiro AR, Cardoso JC, Gonçalo MM. Brooke-Spiegler Syndrome – an underrecognized cause of multiple familial scalp tumors: report of a new germline mutation. J Dermatol Case Rep. 2015 Sep 30. 9 (3):67-70.[↩]
- Rajan N, Burn J, Langtry J, Sieber-Blum M, Lord CJ, Ashworth A. Transition from cylindroma to spiradenoma in CYLD-defective tumours is associated with reduced DKK2 expression. J Pathol. 2011 Jul;224(3):309-21. doi: 10.1002/path.2896[↩]
- Corda G, Sala A. Cutaneous cylindroma: it’s all about MYB. J Pathol. 2016 Aug;239(4):391-3. doi: 10.1002/path.4746[↩]
- Ishihara M, Mehregan DR, Hashimoto K, et al. Staining of eccrine and apocrine neoplasms and metastatic adenocarcinoma with IKH-4, a monoclonal antibody specific for the eccrine gland. J Cutan Pathol. 1998 Feb. 25(2):100-5[↩]
- Khoury E, Godfrey M, Yeoh CC. Gynaecological cylindroma in association with CYLD gene mutation. Oxf Med Case Reports. 2022 Jan 24;2022(1):omab139. doi: 10.1093/omcr/omab139[↩]
- Casale F, Elwood HR, Tchanque-Fossuo CN. Exophytic growth on nasal ala. JAAD Case Rep. 2021 Nov 17;19:48-50. doi: 10.1016/j.jdcr.2021.10.035[↩]
- Watanabe Y, Mori T, Makino T, Yamamoto T. Giant Vascular Cylindroma in a Case of Brooke-Spiegler Syndrome. Indian Dermatol Online J. 2022 Oct 12;13(6):792-793. doi: 10.4103/idoj.idoj_33_22[↩]
- Bargiel J, Wyszyńska-Pawelec G, Gontarz M, Gąsiorowski K, Marecik T, Szczurowski P, Zapała J. Turban Tumor Syndrome: In Search of a Gold Standard – A Case Report. Skin Appendage Disord. 2021 Jun;7(4):326-328. doi: 10.1159/000514855[↩]
- Luo YY, Chen DG, Ji PZ, Liu B, Yang YL. [Brooke-Spiegler syndrome: report of a case]. Zhonghua Bing Li Xue Za Zhi. 2022 Mar 8;51(3):253-255. Chinese. doi: 10.3760/cma.j.cn112151-20211228-00939[↩]
- Singh DD, Naujoks C, Depprich R, Schulte KW, Jankowiak F, Kübler NR, Handschel J. Cylindroma of head and neck: review of the literature and report of two rare cases. J Craniomaxillofac Surg. 2013 Sep;41(6):516-21. doi: 10.1016/j.jcms.2012.11.016[↩]
- Cohen YK, Elpern DJ. Dermatoscopic pattern of a cylindroma. Dermatol Pract Concept. 2014 Jan 31. 4(1):67-8[↩]
- Fusco N, Colombo PE, Martelotto LG, De Filippo MR, Piscuoglio S, Ng CK, et al. Resolving quandaries: basaloid adenoid cystic carcinoma or breast cylindroma? The role of massively parallel sequencing. Histopathology. 2016 Jan. 68 (2):262-271[↩]
- Merlo G, Pesce M, Borra T, Orejuela I, Pasquali F, Panizza R, Ghiglione M, Grosso F. Malignant eccrine spiradenocylindroma and parotid gland involvement in Brooke Spiegler syndrome. Dermatol Reports. 2022 Jan 26;14(3):9418. doi: 10.4081/dr.2022.9418[↩][↩]
- Herzum A, Russo R, Cozzani E, Paudice M, Guadagno A, Parodi A. Multiple rubbery nodules on the scalp. JAAD Case Rep. 2021 Jan 5;8:80-82. doi: 10.1016/j.jdcr.2020.12.023. Erratum in: JAAD Case Rep. 2021 Mar 04;10:81. doi: 10.1016/j.jdcr.2021.03.005[↩]
- Thomas LW, Pham CT, Coakley B, Lee P. Treatment of Brooke-Spiegler Syndrome Trichoepitheliomas with Erbium: Yttrium-Aluminum-Garnet Laser: A Case Report and Review of the Literature. J Clin Aesthet Dermatol. 2020 Jul;13(7):41-44. https://pmc.ncbi.nlm.nih.gov/articles/PMC7492015[↩]
- Kim KE, Jeong JY, Park TJ, Kim IH. A Case of Malignant Transformation of Solitary Recurrent Cylindroma on Scalp. Ann Dermatol. 2022 Dec;34(6):478-481. doi: 10.5021/ad.20.118[↩][↩][↩][↩]
- Cylindroma Treatment & Management. https://emedicine.medscape.com/article/1056630-treatment[↩]
- Rallan D, Harland CC. Brooke-Spiegler syndrome: treatment with laser ablation. Clin Exp Dermatol. 2005 Jul. 30(4):355-7[↩]
- Retamar RA, Stengel F, Saadi ME, et al. Brooke-Spiegler syndrome – report of four families: treatment with CO2 laser. Int J Dermatol. 2007 Jun. 46(6):583-6.[↩]
- Iyer PV, Leong AS. Malignant dermal cylindromas. Do they exist? A morphological and immunohistochemical study and review of the literature. Pathology. 1989 Oct;21(4):269-74. doi: 10.3109/00313028909061072[↩][↩][↩]