What is discitis
Discitis is an inflammation or infection of the intervertebral disc or intervertebral disc space. Discitis can be caused by bacteria, virus, or fungus. Discitis must be considered with vertebral osteomyelitis or spondylodiscitis; these conditions are almost always present together, and they share much of the same pathophysiology, symptoms, and treatment 1. Spondylodiscitis is an infection of the vertebral bodies. Although discitis and associated vertebral osteomyelitis are uncommon conditions, they are often the causes of debilitating neurologic injury. Discitis and spondylodiscitis can be a serious disease because of diagnostic delay and inadequate treatment 2. Discitis may lead to intervertebral disk erosion. Until recently, discitis has been defined as a nonbacterial inflammation and has been attributed to aseptic processes (e.g., chemical reaction to an injected substance). However, recent studies provide evidence that infection may be the initial cause, but perhaps not the promoter, of most cases of discitis. Discitis has been diagnosed in patients following discography, myelography, lumbar puncture, paravertebral injection, and obstetrical epidural anesthesia.
Discitis can occur in the neck, but it is more common in the low back. Although low back pain is the most common symptom of low back pain, discitis is an unusual cause of low back pain. The pain usually starts slowly and increases gradually over time. Three or more weeks often go by before someone with discitis may present for care. Nerve symptoms such as numbness, tingling and weakness can also be seen. A person with discitis may also feel generally unwell. You may have a fever or feel tired. You may also lose your appetite, become nauseated, and lose weight. The area over the infected disc may be tender to touch. It is important to remember that all of these symptoms are nonspecific, and may be seen with many other causes.
Discitis most commonly occurs when bacteria directly invade the discs from other parts of the body. This can occur when a person has had surgery or some kind of trauma. Other medical conditions can also put a person at risk for discitis. The most common of these is a bacterial heart infection called endocarditis. Other factors that raise a person’s risk for discitis include IV drug use, diabetes, older age, poor nutrition, and others. The most common “bug” that causes discitis is usually Staphylococcus aureus.
Discitis is an infection, and identifying the source of infection is important.. If no obvious reason for the infection is identified, your doctor may recommend getting your heart checked out for endocarditis with a test called an echocardiogram (“echo”).
In the United States, the incidence of discitis ranges from 1 in 100,000 population to 1 in 250,000 population. In other developed nations, the incidence of discitis is similar; however, in less developed nations, infectious discitis is much more common. In some areas of Africa, it has been reported that 11% of all patients seen for back pain were diagnosed with discitis.
A bimodal distribution of ages occurs with discitis. Childhood discitis affects patients with a mean age of 7 years. The incidence of discitis then decreases until middle age, when a second peak in incidence is observed at approximately 50 years of age. Some authors argue that childhood discitis is a separate disease entity and should be considered independently.
The predominance of discitis in males is more pronounced in adults, with male-to-female ratios ranging from 2:1 to as high as 5:1. Childhood discitis has a slight male prevalence, with a male-to-female ratio of 1.4:1.
No specific racial predilection has been noted.
Unfortunately, adult discitis has a slow, insidious onset, which can cause diagnosis to be delayed for months. Neck or back pain with localized tenderness is the initial presenting complaint. Movement exacerbates these symptoms, which are not alleviated with conservative treatment (eg, analgesics or bed rest).
In patients who are chronically ill, a high incidence of epidural extension of the infection exists, causing lower-extremity weakness or plegia. Fever, chills, weight loss, and symptoms of systemic disease may be present, but they are not common.
In postoperative patients, symptoms usually begin days to weeks after surgery. Symptoms are similar to those experienced by patients with spontaneous discitis, consisting of pain without neurologic abnormality. Limited movement and localized tenderness also occur; however, superficial signs of infection are rare (only 10% of cases). Diagnosis is rarely delayed in postoperative patients, which is the main reason that neurologic deficit is uncommon in these cases.
The disease has a more acute course in children. A sudden onset of back pain, refusal to walk, and irritability are the most common symptoms. Fever is often present, accompanied by local tenderness and limited back motion.
Figure 1. Intervertebral disc
Discitis causes
Discitis is thought to spread to the involved intervertebral disk via hematogenous spread of a systemic infection (e.g., urinary tract infection [UTI]). Many sites of origin have been implicated, but UTI (urinary tract infection), pneumonia, and soft-tissue infection seem to be the most common. Direct trauma has not been conclusively shown to be related to discitis. Intravenous (IV) drug use with contaminated syringes offers direct access to the bloodstream for a variety of organisms. Often, no other site of infection is discovered.
Staphylococcus aureus is the organism most commonly found; however, Escherichia coli and Proteus species are more common in patients with UTIs. Pseudomonas aeruginosa and Klebsiella species are other gram-negative organisms observed in IV drug abusers, although they are not seen as commonly as Staphylococcus aureus. Not surprisingly, medical conditions that predispose patients to infections elsewhere in the body are associated with discitis. Diabetes, AIDS, steroid use, cancer, and chronic renal insufficiency are common comorbidities 3.
Although rare, infection of the disk space can also occur following surgical intervention at the site. The infection rate after anterior cervical diskectomy has been quoted at 0.5% of cases; the infection rate for lumbar diskectomy is half that. In such cases, infection is transmitted through direct inoculation of the operative site. As in spontaneous discitis, the most common organism is Staphylococcus aureus, but Staphylococcus epidermidis and Streptococcus species also should be considered.
Childhood discitis has not been consistently associated with an initial causative infection elsewhere in the body. Staphylococcus aureus is the most common organism found.
Pathophysiology
An infection does not ordinarily originate in the vertebra or disk space; rather, it typically spreads there from other sites via the bloodstream. Spinal arteries form two lateral anastomotic chains and one median anastomotic chain along the posterior surface of the vertebral bodies. The spinal arteries are the origins of the periosteal arteries, which in turn give rise to metaphyseal arteries.
In children, anastomoses between metaphyseal arteries are made by the intermetaphyseal arteries; however, in adults, the intermetaphyseal arteries degenerate, causing direct diffusion from the adjacent endplate to be the only source of nutrients for the disk. Septic emboli traveling through this arterial system enter the metaphyseal arteries, which have become end arteries in the adult, causing a large area of infarction. Infarction of the vertebral endplates is followed by localized infection that subsequently spreads through the vertebral body and into the poorly vascularized disk space. Infection can then spread to the epidural space or paraspinal soft tissues.
The other anastomotic vascular system of the spine is the venous system. The venous system of the spine, like the arterial system, forms an anastomotic plexus (Batson plexus) in the epidural space. This plexus drains each segmental level and is continuous with the pelvic veins. Retrograde flow through this plexus during periods of high intra-abdominal pressure has been postulated to allow the spread of infection from the pelvic organs.
Support for this hypothesis comes from the observation that pelvic disease is one of the most common primary sites of infection in patients with diskitis. Other authors take issue with this hypothesis, citing animal studies that show retrograde flow through the epidural venous plexus only at extremely high intra-abdominal pressures that are not physiologic.
Discitis symptoms
Discitis can occur in the neck, but it is more common in the low back. Although low back pain is the most common symptom of low back pain, discitis is an unusual cause of low back pain. The pain usually starts slowly and increases gradually over time. Three or more weeks often go by before someone with discitis may present for care. Nerve symptoms such as numbness, tingling and weakness can also be seen. A person with discitis may also feel generally unwell. You may have a fever or feel tired. You may also lose your appetite, become nauseated, and lose weight. The area over the infected disc may be tender to touch. It is important to remember that all of these symptoms are nonspecific, and may be seen with many other causes.
Localized tenderness over the involved area with concomitant paraspinal muscle spasm is the most common physical sign. If the cervical or lumbar segments are involved, restricted mobility secondary to pain occurs. Reported rates of neurologic deficit (eg, radiculopathy, myelopathy) vary widely, ranging from 2% to 70%. Cervical disease is associated with a much higher rate of neurologic deficit.
Discitis complications
Neurologic deficits develop in 13-40% of patients, especially those with diabetes or other systemic illnesses. Transfer to an institution with neurosurgical or orthopedic spinal care is warranted for any patient demonstrating neurologic decline for decompression and possible stabilization.
Long-term antibiotic therapy may lead to ototoxicity or renal toxicity.
Discitis diagnosis
Discitis is rare, so first and foremost, consult with a spine doctor for an evaluation. The most important part of your evaluation will be your doctor taking your medical history and inquiring about risk factors for discitis. Your doctor will also examine you to look for any signs of infection, as well as test you for any nerve damage.
Your doctor’s evaluation may be enough to say that you do not have it and will not need any further testing. If more testing is needed, your doctor may request blood testing for infection and inflammation. Again, discitis is an infection, and your doctor may check for various sources of infection. They may even check you for tuberculosis or HIV. Disc biopsy is generally the gold standard in making the diagnosis.
A biopsy is done to take a small sample from the disc. This sample can be tested for the presence of bacteria. If bacteria are found, they can be tested further to see what kind of antibiotics will work. Unless absolutely necessary, antibiotics should not be given until testing is completed, and an appropriate antibiotic is identified.
A biopsy for discitis is usually done with a needle. The needle is hollow to allow removing a small sample of the disc. The needle can be inserted with CT Scan guidance, or X-ray guidance.
Plain x-rays and CAT scans can be done, but the best imaging study to look for discitis is an MRI. Doing an MRI with and without contrast is even more helpful. Not everyone can have an MRI, or can have contrast, and your doctor will consider this when deciding what kind of scan you need.
Laboratory tests
Elevations in the erythrocyte sedimentation rate (ESR) and the C-reactive protein (CRP) level are the most consistent laboratory abnormalities seen in cases of discitis. The mean ESR for patients with discitis is 85-95 mm/hr. The utility of the ESR can be extended by performing serial measurements during treatment. A 50% decline in the ESR can usually be expected with successful treatment, and the ESR often continues to decline after treatment. Frequently, the ESR may not return to normal levels despite adequate therapy.
Leukocytosis is often present in systemic disease but is frequently absent in discitis cases. discitis is generally accompanied by a normal peripheral white blood cell (WBC) count if the primary site of infection has been treated.
Procalcitonin (PCT) has been evaluated as a diagnostic tool and monitoring parameter for spondylodiscitis and for discrimination between bacterial infection and aseptic inflammation of the spine, but a study by Maus et al did not find it to be useful for these purposes 4. A study by Jeong et al found serum PCT to be less sensitive than serum CRP in patients with spinal infection 5.
Blood cultures must be obtained on a frequent basis for any patient suspected of harboring an infected disk. Appropriate therapy may be instituted for positive blood cultures without the need for invasive tests. Unfortunately, blood cultures are positive in only one third to one half of discitis cases.
Sputum and urine cultures are necessary to locate any other sources of infection, including respiratory and genitourinary sites.
Imaging Studies
Plain radiography
Although radiographic films of the spine can be very useful in diagnosing discitis, abnormalities are visible only after several weeks following the onset of disease. The most common early finding on plain films is disk-space narrowing, followed by irregularities and erosion of the adjacent endplates and calcification of the anulus around the affected disk. As osteomyelitis progresses, bone density decreases, with loss of the normal trabeculation of the vertebra. If bone destruction continues, subluxation (with possible instability of the spine) becomes evident.
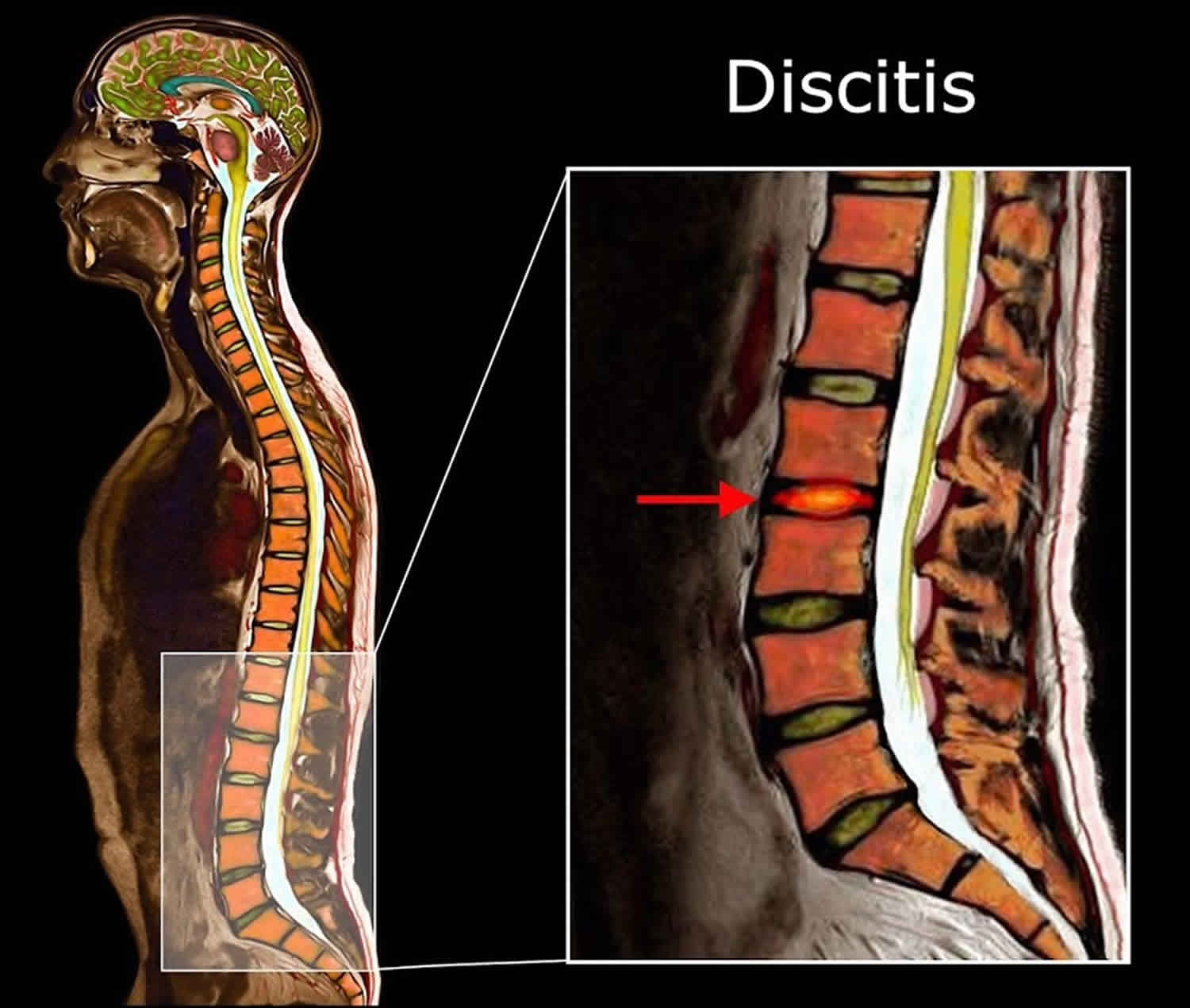
Magnetic resonance imaging (MRI)
The most sensitive and specific test for discitis is magnetic resonance imaging (MRI). T1-weighted images (see the image below) show narrowing of the disk space and low signals consistent with edema in the marrow of adjacent vertebral bodies. T2-weighted images show increased signals in both the disk space and the surrounding vertebral bodies.
MRI is very useful in helping distinguish between infectious discitis, neoplasia, and tuberculosis. Diffusion-weighted imaging is useful in distinguishing between degenerative and infectious endplate abnormalities. Compared with positron emission tomography (PET), diffusion-weighted MRI costs less, has faster imaging times, and lacks ionizing radiation 6.
Disk-space involvement directs attention toward infection; it only is involved late in tuberculosis and very rarely in neoplasia.
With the use of intravenous (IV) contrast (see the image below), MRI, like computed tomography (CT), can detect paraspinal disease (eg, paraspinal phlegmon or epidural abscess). A large amount of paraspinal soft-tissue swelling and a psoas abscess are often associated with spinal tuberculosis.
Computed tomography
CT has the ability to detect discitis earlier than plain radiography does. Findings include hypodensity of the intervertebral disk and destruction of the adjacent endplate and bone (see the image below), with edematous surrounding tissues.
Certain bacterial organisms can also produce gas in the site that is easily detected on CT scans. However, this is not pathognomonic, because as it can be present in degenerative spine disease.
The advantage of CT over radiography is that it can also detect associated paraspinal disease, especially when combined with IV contrast or myelography. CT can serve as a supplement to MRI, in that it is better able to distinguish between bone and soft tissue than MRI. CT can help monitor successful treatment, which is accompanied by increased bone density and sclerosis.
Nuclear medicine
Gallium-67 and technetium-99m have been utilized in the detection of discitis with similar results. Radionuclide scanning has demonstrated a high degree of sensitivity shortly after the onset of symptoms. Diffuse initial uptake is followed by more focal uptake on delayed scans. Technetium-99m has been recommended more often because of its lower cost and smaller radiation dose.
Because of the availability and sensitivity of other tests, radionuclide scans may be most useful in the workup of patients with fever of unknown origin.
Indium-111 WBC scintigraphy has been shown to have a low sensitivity for discitis and is not the test of choice.
Bone scans are not specific for infection over inflammation; therefore, they are ineffective in postoperative patients.
Echocardiography
Echocardiography can detect bacterial endocarditis, which is a common source of discitis and embolic infection throughout the body.
Discitis treatment
Discitis is an infection. If it is a bacterial infection, which is usually the case, antibiotics are required. Antibiotics may need to be given through an IV, and for as long as 3 months.
Discitis is usually quite painful, and pain control is a critical component of discitis treatment as well. This is a complex process requiring detailed discussions with the treating physician regarding various options.
Surgery is usually not necessary to treat discitis. It only becomes necessary if antibiotic treatment does not work. Occasionally discitis can affect the spine’s alignment. In this case, surgery may be necessary to fix alignment issues, if there is nerve compromise and extremity symptoms in the arms or legs. Also, hardware may need to be removed until the discitis is cleared up.
Antibiotics
Antibiotic treatment must be tailored to the isolated organism and any other sites of infection. Broad-spectrum antibiotics must be used if no organism is isolated; however, this is very rare, and other disease processes (eg, spinal tuberculosis) must be considered in the face of persistently negative cultures.
Parenteral antibiotics are a requirement, even for outpatients. They are usually administered for 6-8 weeks. Before parenteral therapy is discontinued, the erythrocyte sedimentation rate (ESR) should have dropped by one half to one third, the patient should have no pain on ambulation, and there should be no neurologic deficits 7.
The use of oral antibiotics after intravenous (IV) treatment has not been shown to be of added benefit.
Any laboratory or clinical sign of persistent infection should prompt another biopsy and continued antibiotic therapy.
Immobilization
Immobilization is necessary, especially in the initial stages of the disease. The goal of immobilization is to provide the opportunity for the affected vertebrae to fuse in an anatomically aligned position.
Two weeks of bed rest should be followed by external immobilization with a brace when the patient gets out of bed. Any pain on ambulation is an indication for continued bed rest. Generally, bracing is used for 3-6 months following initiation of treatment; however, even with the use of appropriate antibiotics and bracing, collapse of the vertebral segments and kyphos formation may occur.
Surgical therapy
Indications for surgery beyond open biopsy include the following:
- Neurologic deficit
- Spinal deformity
- Disease progression
- Noncompliance
- Antibiotic toxicity
The goal of surgery are as follows:
- To remove diseased tissue
- To decompress neural structures
- To ensure spinal stability
Although in most cases the vertebrae fuse spontaneously after discitis and osteomyelitis, operative fusion can be a useful adjunct by allowing earlier mobilization of the patient. Despite early concerns, use of a fusion plug and metallic instrumentation in an infected field has not been shown to impede successful treatment.
Discitis recovery time
Most patients are cured by a treatment protocol of antibiotics, either alone or in combination with surgery. Only 15% of patients experience permanent neurologic deficits. Recurrence of infection occurs in 2-8% of patients.
Mortality associated with discitis occurs from the spread of infection, either through the nervous system or through other organs. Mortality has been reported to be 2-12%.
Karadimas et al. 8 retrospectively analyzed the outcomes of a large series of patients treated for spondylodiscitis. Patients were divided into three groups: 70 who received nonoperative treatment (group A), 56 who underwent posterior decompression alone (group B), and 37 who underwent decompression and stabilization (group C). At 12-month follow-up, treatment had failed in eight of the group A patients. Reoperation was necessary in 24 of the group B patients and in six of the group C patients. None of the group A patients had neurologic symptoms; 11 of the group B patients had neurologic deficits, five of whom benefited from surgery; and 11 of the group C patients had altered neurologic deficits.
Long-term monitoring
Once the correct treatment is implemented, monitor patients to rule out progressive neurologic deficit.
A falling ESR is consistent with successful treatment. Although ESR values should fall by at least one third to one half, rarely do they return to preinfection levels. Reduction of C-reactive protein (CRP) levels has been shown to be more sensitive than ESR in some studies.
Serial radiographic examination is a necessity to detect bony collapse or deformity. Successful treatment is accompanied by appropriate changes, including sclerosis of the endplates, on plain radiography and computed tomography (CT). Nevertheless, radiographic findings are significantly slower than clinical response and cannot be used to assess eradication of infection.
- Diskitis. https://emedicine.medscape.com/article/1263845-overview[↩]
- Spondylodiscitis associated with multiple level involvement and negative microbiological tests: an unusual case. Spine (Phila Pa 1976). 2010 Sep 1;35(19):E1006-9. doi: 10.1097/BRS.0b013e3181c52d56. https://www.ncbi.nlm.nih.gov/pubmed/20395882[↩]
- Conaughty JM, Chen J, Martinez OV, Chiappetta G, Brookfield KF, Eismont FJ. Efficacy of linezolid versus vancomycin in the treatment of methicillin-resistant Staphylococcus aureus discitis: a controlled animal model. Spine (Phila Pa 1976). 2006 Oct 15. 31 (22):E830-2.[↩]
- Maus U, Andereya S, Gravius S, Ohnsorge JA, Miltner O, Niedhart C. [Procalcitonin (PCT) as diagnostic tool for the monitoring of spondylodiscitis]. Z Orthop Unfall. 2009 Jan-Feb. 147 (1):59-64[↩]
- Jeong DK, Lee HW, Kwon YM. Clinical Value of Procalcitonin in Patients with Spinal Infection. J Korean Neurosurg Soc. 2015 Sep. 58 (3):271-5.[↩]
- Eguchi Y, Ohtori S, Yamashita M, Yamauchi K, Suzuki M, Orita S, et al. Diffusion magnetic resonance imaging to differentiate degenerative from infectious endplate abnormalities in the lumbar spine. Spine (Phila Pa 1976). 2011 Feb 1. 36 (3):E198-202.[↩]
- Walters R, Rahmat R, Fraser R, Moore R. Preventing and treating discitis: cephazolin penetration in ovine lumbar intervertebral disc. Eur Spine J. 2006 Sep. 15 (9):1397-403.[↩]
- Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, et al. Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop. 2008 Oct. 79 (5):650-9.[↩]