What is genetic testing
Genetic testing uses laboratory methods to look at your genes, which are the DNA instructions you inherit from your mother and your father. Genetic tests may be used to identify increased risks of health problems, to choose treatments, or to assess responses to treatments.
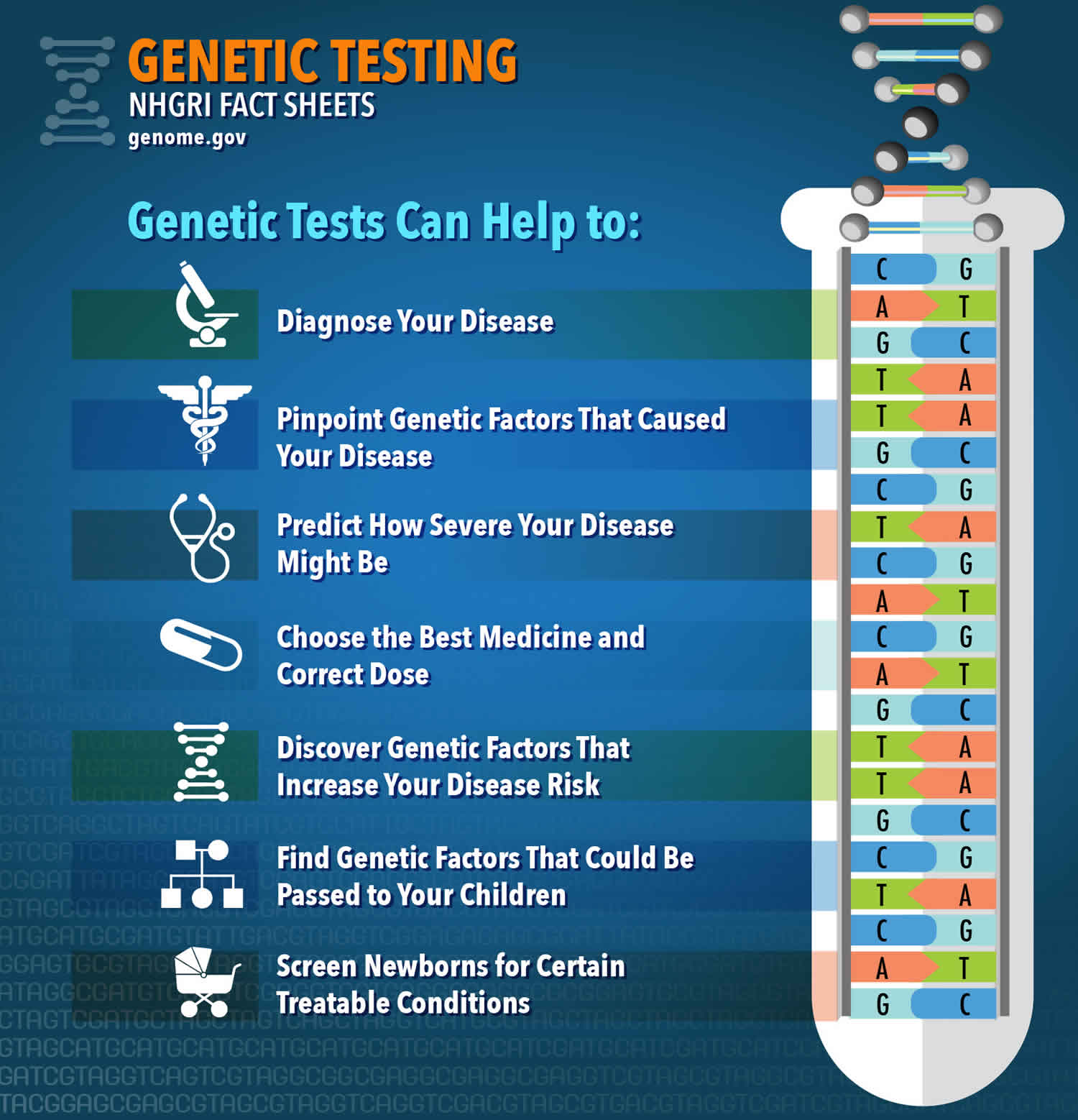
There are many different types of genetic tests. Genetic tests can help to:
- Diagnose disease
- Identify gene changes that are responsible for an already diagnosed disease
- Determine the severity of a disease
- Guide doctors in deciding on the best medicine or treatment to use for certain individuals
- Identify gene changes that may increase the risk to develop a disease
- Identify gene changes that could be passed on to children
- Screen newborn babies for certain treatable conditions
Genetic test results can be hard to understand, however specialists like geneticists and genetic counselors can help explain what results might mean to you and your family. Because genetic testing tells you information about your DNA, which is shared with other family members, sometimes a genetic test result may have implications for blood relatives of the person who had testing.
It is also important to remember that genetic testing is different from other types of laboratory testing. Results of genetic tests may have implications not only for you the patient, but also for your family members, who may need to be tested as well. In addition, genetic education and counseling is often advised to help understand and cope with the results of genetic tests. Genetic counselors are trained professionals who can help those with family members who have a genetic disorder as well as those at risk to better understand the science behind inherited conditions. They can identify families at risk of certain genetic disorders and offer support and counseling as well as serve as patient advocates. For more information on genetic counselors and to find one near you, visit the National Society of Genetic Counselors web site (https://www.nsgc.org/).
What is DNA?
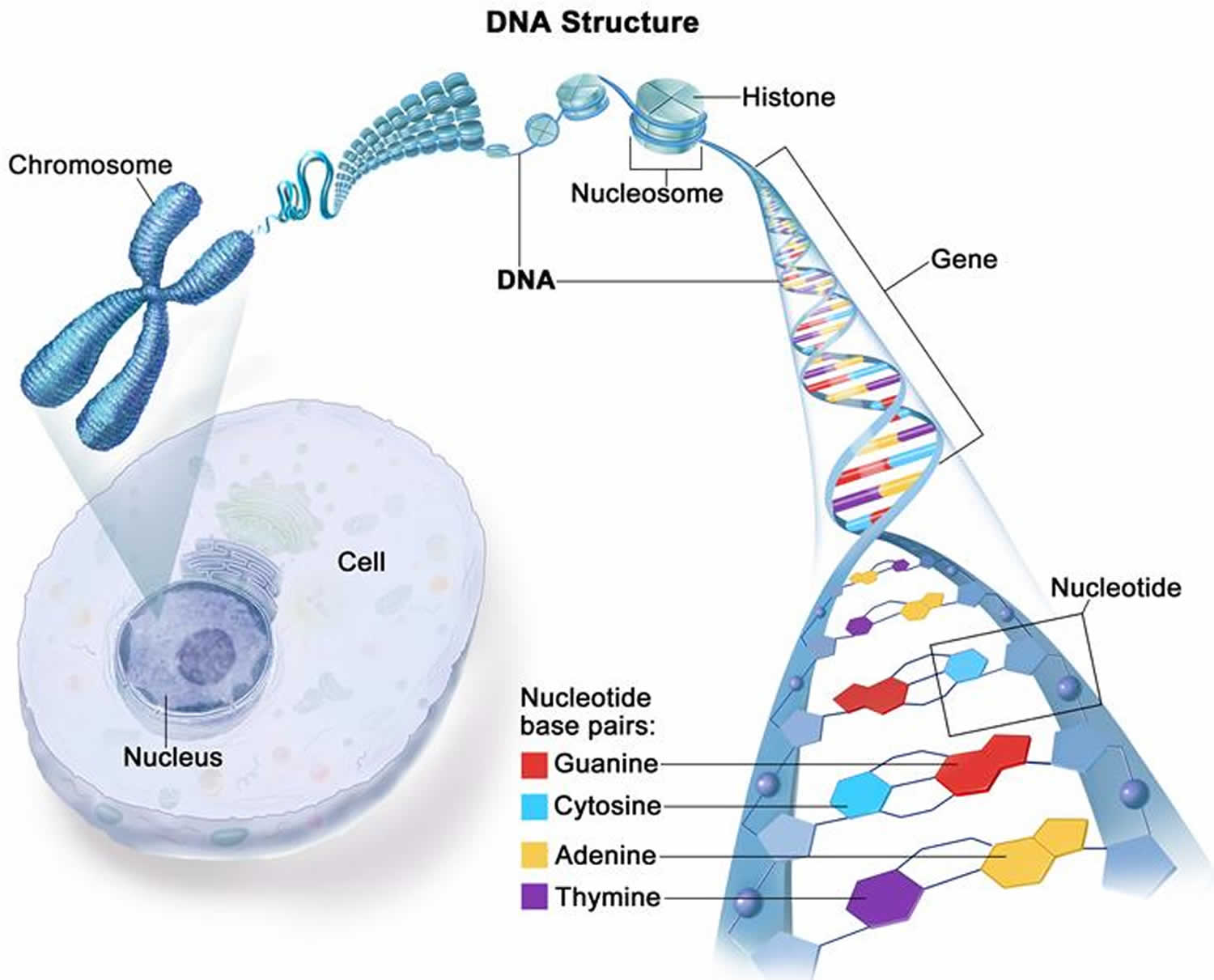
DNA is short for deoxyribonucleic acid, is the hereditary material in humans and almost all other organisms. Nearly every cell in a person’s body has the same DNA. Most DNA is located in the cell nucleus (where it is called nuclear DNA), but a small amount of DNA can also be found in the mitochondria, where it is called mitochondrial DNA or mtDNA 1. Mitochondria are are very important cellular structures within cells that convert the energy from food into a form that cells can use. Mitochondrial DNA is also called “extra-nuclear DNA” and it in part makes the proteins that are needed by the mitochrondria to function properly.
The information in DNA is stored as a code made up of four chemical bases: adenine (A), guanine (G), cytosine (C), and thymine (T). Human DNA consists of about 3 billion bases, and more than 99 percent of those bases are the same in all people. The order, or sequence, of these bases determines the information available for building and maintaining an organism, similar to the way in which letters of the alphabet appear in a certain order to form words and sentences.
DNA bases pair up with each other, A with T and C with G, to form units called base pairs. Each base is also attached to a sugar molecule and a phosphate molecule. Together, a base, sugar, and phosphate are called a nucleotide. Nucleotides are arranged in two long strands that form a spiral called a double helix. The structure of the double helix is somewhat like a ladder, with the base pairs forming the ladder’s rungs and the sugar and phosphate molecules forming the vertical sidepieces of the ladder.
An important property of DNA is that it can replicate, or make copies of itself. Each strand of DNA in the double helix can serve as a pattern for duplicating the sequence of bases. This is critical when cells divide because each new cell needs to have an exact copy of the DNA present in the old cell.
Figure 1. DNA structure
Footnote: Most DNA is found inside the nucleus of a cell (nuclear DNA), where it forms the chromosomes. Chromosomes have proteins called histones that bind to DNA. DNA has two strands that twist into the shape of a spiral ladder called a helix. DNA is made up of four building blocks called nucleotides: adenine (A), thymine (T), guanine (G), and cytosine (C). The nucleotides attach to each other (A with T, and G with C) to form chemical bonds called base pairs, which connect the two DNA strands. Genes are short pieces of DNA that carry specific genetic information.
[Source 2 ]What is a gene?
A gene is the basic physical and functional unit of inheritance. Genes are passed from parents to offspring and contain the information needed to specify traits. Genes are pieces of DNA and most genes contain the information for making a specific protein. Some genes act as instructions to make molecules called proteins. However, many genes do not code for proteins. In humans, genes vary in size from a few hundred DNA bases to more than 2 million bases. Genes are arranged, one after another, on structures called chromosomes. Each chromosome contains many genes. A chromosome contains a single, long DNA molecule, only a portion of which corresponds to a single gene. The Human Genome Project estimated that humans have between 20,000 and 25,000 genes arranged on their chromosomes.
Every person has two copies of each gene, one inherited from each parent. Most genes are the same in all people, but a small number of genes (less than 1 percent of the total) are slightly different between people. Alleles are forms of the same gene with small differences in their sequence of DNA bases. These small differences contribute to each person’s unique physical features.
Scientists keep track of genes by giving them unique names. Because gene names can be long, genes are also assigned symbols, which are short combinations of letters (and sometimes numbers) that represent an abbreviated version of the gene name. For example, a gene on chromosome 7 that has been associated with cystic fibrosis is called the cystic fibrosis transmembrane conductance regulator; its symbol is CFTR.
What is a chromosome?
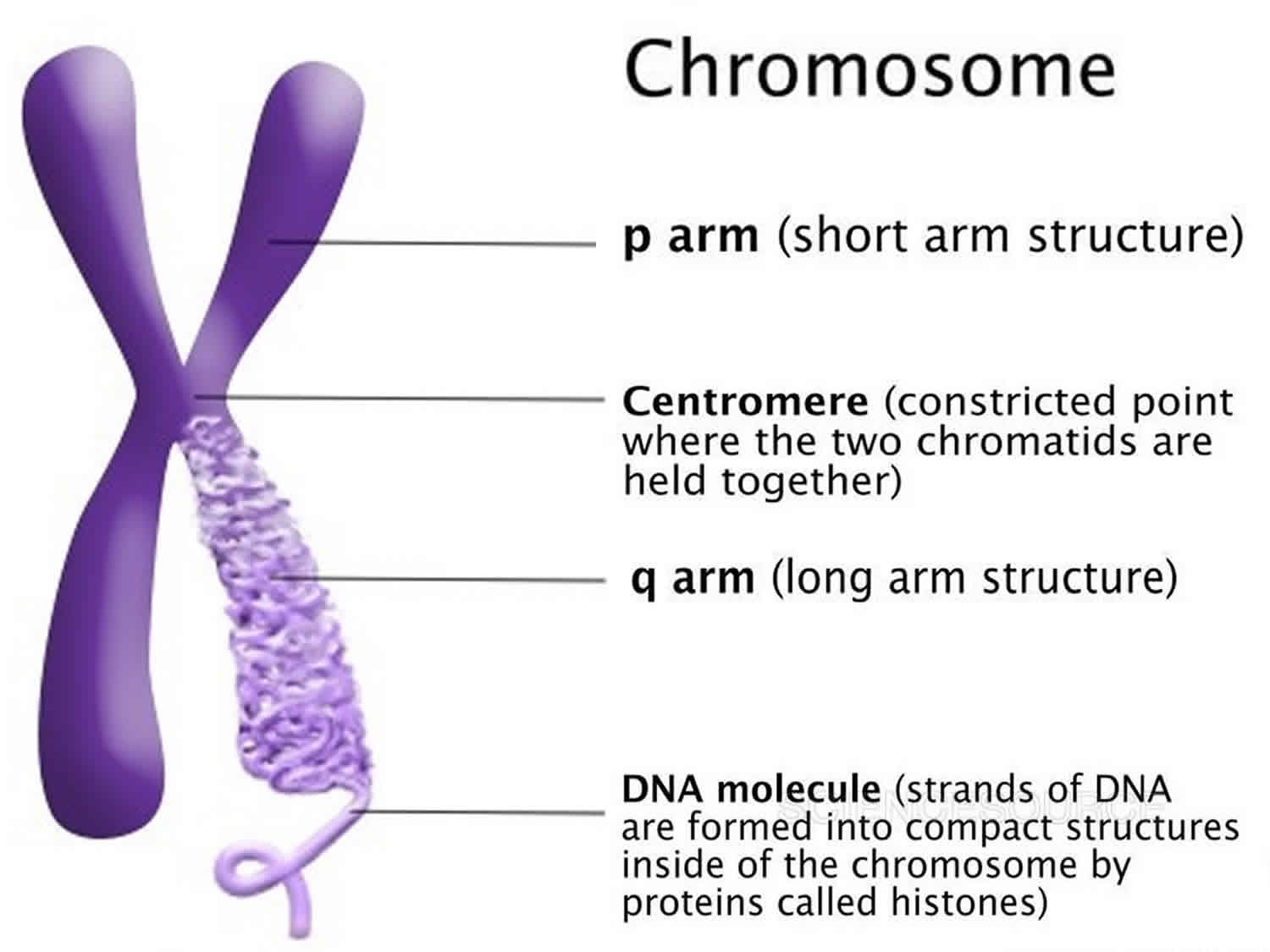
The total of an individual’s genetic information is called their genome. The genome consists of structures called chromosomes that are composed of very long double strands of DNA. In the nucleus of each cell, the DNA molecule is packaged into thread-like structures called chromosomes. Each chromosome is made up of DNA tightly coiled many times around proteins called histones that support its structure.
Chromosomes are not visible in the cell’s nucleus—not even under a microscope—when the cell is not dividing. However, the DNA that makes up chromosomes becomes more tightly packed during cell division and is then visible under a microscope. Most of what researchers know about chromosomes was learned by observing chromosomes during cell division.
Each chromosome has a constriction point called the centromere, which divides the chromosome into two sections, or “arms.” The short arm of the chromosome is labeled the “p arm.” The long arm of the chromosome is labeled the “q arm.” The location of the centromere on each chromosome gives the chromosome its characteristic shape, and can be used to help describe the location of specific genes.
Figure 2. Chromosome structure
How many chromosomes do people have?
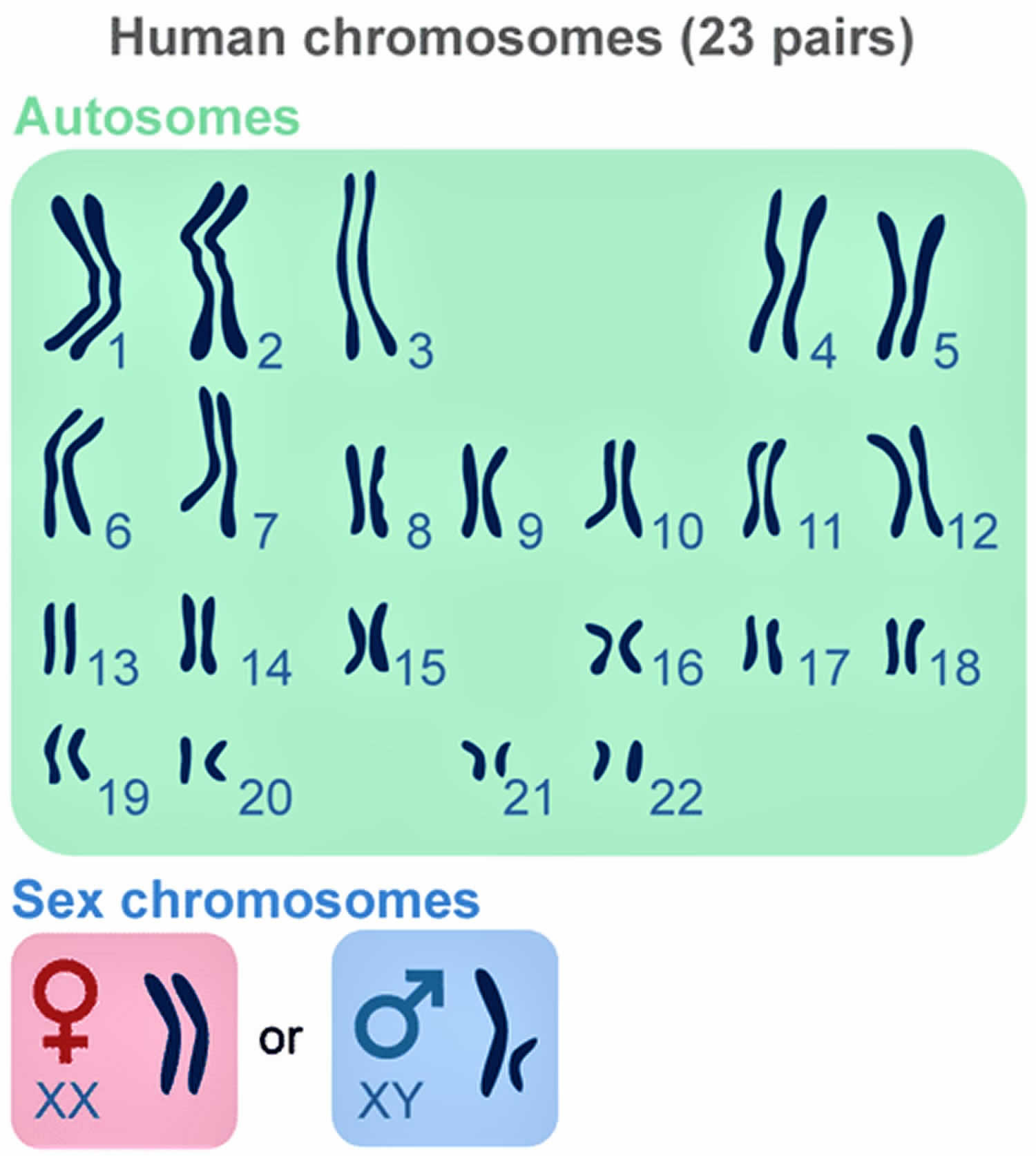
In humans, each cell normally contains 23 pairs of chromosomes, for a total of 46 chromosomes. One-half of each pair of chromosomes is inherited from an individual’s mother and the other half of the pair is inherited from an individual’s father. Twenty-two of the 23 pairs of chromosomes are called autosomes, look the same in both males and females. The 23rd pair, are the sex chromosomes, differ between males and females. Females have two copies of the X chromosome (XX), while males have one X and one Y chromosome (XY). The sex chromosomes determine a person’s sex; normal males have one X and one Y chromosome (XY) while normal females have two X chromosomes (XX).
The 22 autosomes are numbered by size. The other two chromosomes, X and Y, are the sex chromosomes. This picture of the human chromosomes lined up in pairs is called a karyotype.
Figure 3. Human chromosomes
What is noncoding DNA?
Only about 1 percent of DNA is made up of protein-coding genes; the other 99 percent is noncoding. Noncoding DNA does not provide instructions for making proteins. Scientists once thought noncoding DNA was “junk,” with no known purpose. However, it is becoming clear that at least some of it is integral to the function of cells, particularly the control of gene activity 3. For example, noncoding DNA contains sequences that act as regulatory elements, determining when and where genes are turned on and off. Such elements provide sites for specialized proteins (called transcription factors) to attach (bind) and either activate or repress the process by which the information from genes is turned into proteins (transcription). Noncoding DNA contains many types of regulatory elements:
- Promoters provide binding sites for the protein machinery that carries out transcription. Promoters are typically found just ahead of the gene on the DNA strand.
- Enhancers provide binding sites for proteins that help activate transcription. Enhancers can be found on the DNA strand before or after the gene they control, sometimes far away.
- Silencers provide binding sites for proteins that repress transcription. Like enhancers, silencers can be found before or after the gene they control and can be some distance away on the DNA strand.
- Insulators provide binding sites for proteins that control transcription in a number of ways. Some prevent enhancers from aiding in transcription (enhancer-blocker insulators). Others prevent structural changes in the DNA that repress gene activity (barrier insulators). Some insulators can function as both an enhancer blocker and a barrier.
Other regions of noncoding DNA provide instructions for the formation of certain kinds of RNA molecules. RNA is a chemical cousin of DNA. Examples of specialized RNA molecules produced from noncoding DNA include transfer RNAs (tRNAs) and ribosomal RNAs (rRNAs), which help assemble protein building blocks (amino acids) into a chain that forms a protein; microRNAs (miRNAs), which are short lengths of RNA that block the process of protein production; and long noncoding RNAs (lncRNAs), which are longer lengths of RNA that have diverse roles in regulating gene activity.
Some structural elements of chromosomes are also part of noncoding DNA. For example, repeated noncoding DNA sequences at the ends of chromosomes form telomeres. Telomeres protect the ends of chromosomes from being degraded during the copying of genetic material. Repetitive noncoding DNA sequences also form satellite DNA, which is a part of other structural elements. Satellite DNA is the basis of the centromere, which is the constriction point of the X-shaped chromosome pair. Satellite DNA also forms heterochromatin, which is densely packed DNA that is important for controlling gene activity and maintaining the structure of chromosomes.
Some noncoding DNA regions, called introns, are located within protein-coding genes but are removed before a protein is made. Regulatory elements, such as enhancers, can be located in introns. Other noncoding regions are found between genes and are known as intergenic regions.
The identity of regulatory elements and other functional regions in noncoding DNA is not completely understood. Researchers are working to understand the location and role of these genetic components.
Genetic Variation and Mutation
All genetic variations or polymorphisms originate from the process of mutation. Genetic variations occur sometimes during the process of somatic cell division (mitosis). Other genetic variations can occur during meiosis, the cycle of division that a sperm cell or an ovum goes through. Some variations are passed along through the generations, adding more and more changes over the years. Sometimes these mutations lead to disease; other times there is no noticeable effect. Genetic variations can be classified into different categories: stable genetic variations, unstable genetic variations, silent genetic variations, and other types.
Stable genetic variations are caused by specific changes in single nucleotides. These changes are called single nucleotide polymorphisms (SNPs) and can include:
- Substitutions, in which one nucleotide is replaced by another
- Deletions, in which a single nucleotide is lost
- Insertions, in which one or more nucleotides are inserted into a gene
If the single nucleotide polymorphism causes a new amino acid to be made, it is called a “missense mutation.” An example of this is in sickle cell anemia, in which one nucleotide is substituted for another. The genetic variation in the gene causes a different amino acid to be added to a protein, resulting in a protein that doesn’t do its job properly and causes cells to form sickle shapes and not carry oxygen.
Unstable genetic variations occur when a nucleotide sequence repeats itself over and over. This is called a “repeat” and is usually normal; however, if the number of repeats increases too greatly, it is called an “expanded repeat” and has been found to be the cause of many genetic disorders. An example of a disease caused by an expanded repeat is Huntington disease, a severe disorder of a part of the brain that is marked by dementia, hydrocephalus, and unusual movements.
Silent genetic variations are those mutations or changes in a gene that do not change the protein product of the gene. These mutations rarely result in a disease.
Other types of variations occur when an entire gene is duplicated somewhere in a person’s genome. When this occurs, extra copies of the gene are present and make extra protein product. This is seen in a disorder that effects peripheral nerves and is called Charcot-Marie-Tooth disease type 1. Some variations occur in a special part of the gene that controls when DNA is copied to RNA. When the timing of protein production is thrown off, it results in decreased protein production. Other variations include a defect in a gene that makes a protein that serves to repair broken DNA in our cells. This variation can result in many types of diseases, including colorectal cancer and a skin disease called xeroderma pigmentosum.
The Future
With the completion of the Human Genome Project, scientists have learned that the word “normal” no longer has meaning when it comes to a person’s genetic makeup. Genetic variations occur in great numbers in your genome (your total genetic makeup). You are unique, not only in your personalities and appearance, but in your genotype as well.
Scientists continue to work on ways to better understand the structure of your genetic makeup, which could allow for important advances in the prevention and treatment of many diseases. There are promising new screening tests on the horizon, such as one for ovarian cancer or Alzheimer disease that researchers are trying to replicate in other disorders as well.
Gene therapy is an approach to treating potentially lethal and disabling diseases that are caused by single gene deficiencies. With specialized techniques, gene expression can be manipulated to correct the problem in the particular patient, although the correction will not be passed along to offspring of that patient. That is, corrections are made at the DNA molecule level to compensate for the abnormal gene so that the detrimental symptoms of the disease are not expressed in the patient. It is still highly experimental. Clinical trials are being conducted to see if this can be used to develop treatments for other diseases, including cancer, heart disease, and AIDS.
Further advances in technology and molecular biology lab techniques have led to a recent invention – the “gene chip” or microarray – which allows many genes to be examined together instead of one at a time as is done now. Using these gene chips, researchers can look for molecular indicators of disease even before the disease presents itself and the patient becomes symptomatic. Gene chips are still being developed and tested for clinical use.
Further advances in genetic testing will eventually replace older methods of predicting prognosis, helping to treat only those patients who will respond to therapy and by helping to guide further research into these therapies. Recent advances are also helping to increase our understanding of some complex cancers, such as multiple myeloma and lymphoma. Without a doubt, there will be more and more advances in genetic research that will impact the laboratory tests available to all patients for detection and treatment of a variety of diseases.
How can I find a genetics professional in my area?
To find a genetics professional in your community, you may wish to ask your doctor for a referral. If you have health insurance, you can also contact your insurance company to find a medical geneticist or genetic counselor in your area who participates in your plan.
Several organizations have tips for finding a healthcare professional:
- The Genetic and Rare Diseases Information Center (https://rarediseases.info.nih.gov/guides/pages/25/how-to-find-a-disease-specialist), a service of the National Institutes of Health, provides a guide to finding specialists in particular genetic and rare conditions.
- The Tuberous Sclerosis Alliance provides advice on finding and choosing a doctor. Although this advice is written for adults with tuberous sclerosis, much of it applies to people with any chronic health condition (https://www.tsalliance.org/individuals-families/adults/how-to-find-a-doctor-a-guide-for-adults-with-tsc/).
Additional resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counsellors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
- The National Cancer Institute provides a Cancer Genetics Services Directory (https://www.cancer.gov/about-cancer/causes-prevention/genetics/directory), which lists professionals who provide services related to cancer genetics. You can search by type of cancer or syndrome, location, and/or provider name.
If you have a health condition that has not been diagnosed, you may be interested in the Undiagnosed Diseases Network (https://undiagnosed.hms.harvard.edu/). They have information about how to apply for this multicenter research study.
Types of genetic testing
Diagnostic genetic testing
Diagnostic testing is used to precisely identify or rule out a specific genetic or chromosomal condition (disease) that is making a person ill. The results of a diagnostic test may help you make choices about how to treat or manage your health.
In many cases, genetic testing is used to confirm a diagnosis when a particular condition is suspected based on physical signs and symptoms. Diagnostic testing can be performed before birth or at any time during a person’s life, but is not available for all genes or all genetic conditions. The results of a diagnostic test can influence a person’s choices about health care and the management of the disorder.
Predictive and pre-symptomatic genetic tests
Predictive and pre-symptomatic genetic tests are used to find gene mutations that increase a person’s likelihood of developing diseases that appear after birth, often later in life. The results of these tests provide you with information about your risk of developing a specific disease. Such information may be useful in decisions about your lifestyle and healthcare.
These tests can be helpful to people who have a family member with a genetic disorder, but who have no features of the disorder themselves at the time of testing. Predictive testing can identify mutations that increase a person’s risk of developing disorders with a genetic basis, such as certain types of cancer. Presymptomatic testing can determine whether a person will develop a genetic disorder, such as hereditary hemochromatosis (an iron overload disorder), before any signs or symptoms appear. The results of predictive and presymptomatic testing can provide information about a person’s risk of developing a specific disorder and help with making decisions about medical care.
Carrier testing
Carrier testing is used to find people who “carry” one copy of a gene mutation that is linked to disease (when present in two copies). Carriers may show no signs of the disease (genetic disorder); however, they have the ability to pass on the gene mutation to their children, who may develop the disease or become carriers themselves. Some diseases require a gene mutation to be inherited from both parents for the disease to occur. This type of testing usually is offered to people who have a family history of a specific inherited disease or who belong to certain ethnic groups that have a higher risk of specific inherited diseases.
If both parents are tested, the test can provide information about a couple’s risk of having a child with a genetic condition.
Prenatal testing
Prenatal testing is offered during pregnancy to help identify fetuses that have certain diseases. Prenatal testing is used to detect changes in a fetus’s genes or chromosomes before birth. This type of testing is offered during pregnancy if there is an increased risk that the baby will have a genetic or chromosomal disorder. In some cases, prenatal testing can lessen a couple’s uncertainty or help them make decisions about a pregnancy. It cannot identify all possible inherited disorders and birth defects, however.
Newborn screening
Newborn screening is used to test babies one or two days after birth to find out if they have certain diseases (genetic disorders) known to cause problems with health and development, so the baby can be treated early in life.
Millions of babies are tested each year in the United States. All states currently test infants for phenylketonuria [PKU] (a genetic disorder that causes intellectual disability if left untreated) and congenital hypothyroidism (a disorder of the thyroid gland). Most states also test for other genetic disorders.
Genetic testing for medication
Pharmacogenomic testing gives information about how certain medicines are processed by an individual’s body. This type of testing can help your healthcare provider choose the medicines that work best with your genetic makeup.
There have been cases regarding individuals who are given a certain therapeutic drug to treat symptoms or to keep symptoms from occurring in which the individual has a very violent reaction to the drug or feels no affect whatsoever. Many times this happens because of the genetic makeup of the individual. The study of this phenomenon is called “pharmacogenomics” or “pharmacogenetics.”
As an example, a woman had surgery to remove a tumor and was given codeine as a pain reliever. Although she was doing well after the surgery, as soon as she began treatment with codeine she developed a full-body rash, difficulty breathing, and an irregular heartbeat. When she was taken off the codeine, her reaction disappeared. Upon further study, it was found that she lacked the enzyme in her blood that metabolized (broke it down into different components) the codeine into morphine and other substances, so she was essentially being overdosed with codeine. The lack of the enzyme was directly related to a variation in the gene that produced it. This genetic variation is a polymorphism between normal individuals and those who carry it. Sometimes these polymorphisms can cause a very serious reaction in an individual that could lead to death.
In some cases, individuals “hypermetabolize” drugs. This occurs when there is too much of an enzyme present that breaks down the helpful drug too quickly, leading to a lack of response to the drug. This can happen when too many copies of the gene are made and too much enzyme is produced. In other cases, the special receptor that the drug binds to on cells or tissues is missing, again because of a variation in the gene that makes the receptor protein. When there is no receptor to bind the drug, the drug may not have any affect on the cells or tissues that it should.
Genetic testing to determine the polymorphisms that play a role in our response to a drug is typical of basic genetic analyses. DNA is removed from cells, manipulated to find a specific area on a specific chromosome, and compared to “normal” DNA. In this way, genetic variations can be seen that may play a role in the over- or under-responsiveness to a therapeutic drug. This testing can also determine an individual’s resistance or sensitivity to the effectiveness of certain drugs used in viral therapy (HIV or hepatitis C drugs, for example).
There are many, many enzymes in your blood that act to metabolize or break down specific drugs, allowing them to be excreted in urine or by other means. At present, there are comprehensive testing programs in place that can give you an overall picture of your specific genetic variations that may cause you to be unresponsive or over-responsive to a therapeutic drug.
Preimplantation testing
Preimplantation testing, also called preimplantation genetic diagnosis, is a specialized technique that can reduce the risk of having a child with a particular genetic or chromosomal disorder. It is used to detect genetic changes in embryos that were created using assisted reproductive techniques such as in-vitro fertilization. In-vitro fertilization (IVF) involves removing egg cells from a woman’s ovaries and fertilizing them with sperm cells outside the body. To perform preimplantation testing, a small number of cells are taken from these embryos and tested for certain genetic changes. Only embryos without these changes are implanted in the uterus to initiate a pregnancy.
Forensic testing
Forensic testing uses DNA sequences to identify an individual for legal purposes and is sometimes referred to as “identity testing”. Unlike the tests described above, forensic testing is not used to detect gene mutations associated with disease. This type of testing can identify crime or catastrophe victims, rule out or implicate a crime suspect, or establish biological relationships between people (for example, paternity).
Identity testing focuses on the identification of an individual through the analysis of either nuclear or mitochondrial DNA extracted from some material: blood, tissue, hair, bone, etc. Any material that contains cells with nuclei can be used for nuclear DNA extraction and eventual identity testing. Mitochondrial DNA, which is “extra-nuclear,” is used when a sample is severely degraded or if only hair shafts with no attached cells are available.
Increasingly, identity testing is used to identify a suspect in a criminal investigation by comparing the DNA found at a crime scene to that of the suspected individual. If a suspected individual is convicted of the crime, his or her DNA polymorphisms are put into a data bank system that is accessible by law enforcement officials. This system is referred to as CODIS or “Combined DNA Index System.” This system has helped to solve many crimes and also to clear those wrongfully accused of a crime.
Other uses of identity testing are to identify individuals whose identity cannot be distinguished by other means, as with decomposed bodies. In this type of genetic testing, specific parts of DNA are examined for polymorphisms (differences) that are unique to the individual. These parts of the DNA strand are referred to as microsatellites or minisatellites and are composed of repeated subunits of the DNA strand. Sometimes these repeated units are called short tandem repeats or variable number of tandem repeats. In forensics, these unique sequences are given the name “DNA fingerprint.”
Other types of identity testing include the determination of an individual’s parent or parents, often called “parentage testing,” and identifying organ donors by using genetic testing for tissue transplantation, called “tissue typing.”
Parentage testing
The primary goal of parentage testing is to identify the biological parent of a given child. It is done to determine an individual’s parent or parents in, for example, cases of adoption or alleged paternity. This determination must be looked at very carefully and must identify the alleged parent with at least 99% certainty.
Many different types of laboratory tests can be done to assess parentage, including examination of red blood cell antigens (blood typing), examination of polymorphic serum protein genes, and assessment of short tandem repeats. The DNA testing techniques used are similar to those used in identity testing for a criminal investigation, that is, extracting DNA from cells and manipulating it in such a way as to be able to examine the individual uniqueness of it.
If, after testing multiple systems, the parent in dispute is not excluded as a possible parent, a mathematical estimate of the possibility that the tested person could be the biological parent must be calculated. This mathematical testing combines the results of the genetic tests with other “non-genetic events” (location of the alleged parent at the time of conception, phenotype of the parent and child, etc.) and results in a “parentage index.” This index is a percentage of the likelihood of parentage. Results of these tests are admissible as evidence in court.
Tissue typing
In the past, it was difficult to tell exactly whether an organ or tissue, such as a kidney, lung or bone marrow, was an exact match for the transplant between a donor and recipient. If it was not, a serious rejection reaction could sometimes occur between the recipient patient and the transplanted organ.
Basic laboratory testing for tissue transplantation involves mixing the white blood cells (leukocytes) from the donor (or the donor tissue) and the recipient together and observing whether an immune response occurs. Proliferation of a specific population of leukocytes signals the onset of an immune response and the likely rejection of the tissue by the recipient’s body. Although this technique is still commonly used, analysis of the DNA in both the donor and the recipient (tissue typing) is used to diminish the likelihood of rejection in the case of tissue transplantation. In bone marrow transplants, DNA testing is done to determine whether the leukocytes and their precursors repopulating a recipient’s bone marrow are his own or those of the donor.
A very specific set of genes is examined when DNA testing is used for tissue typing. On chromosome 6, a large set of genes called the “Major Histocompability Complex” or MHC, resides. These genes are very polymorphic (different) between individuals, and they code for the production of specific glycoprotein antigens located on the surface of many cells. It is these antigens that “recognize” our own organs and tissues from those of another individual. These antigens have the ability to begin an immune system response that results in organ or tissue rejection if the tissue looks foreign.
A distinct region within the MHC on chromosome 6 is used in the DNA analysis of tissue that could be used for transplantation. This region is called the human leukocyte antigen, or HLA-D, region, and sets of genes located there are further subdivided into HLA-DR, HLA-DQ, and HLA-DP depending on the type of glycoprotein antigen for which they code. Polymorphisms in these genes are carefully compared between donor and recipient to determine the appropriateness of the transplant.
The exact techniques used to test DNA for tissue typing are similar to those mentioned in the previous sections. DNA is extracted from donor and recipient cells, then manipulated and fragmented in such a way as to isolate a specific region on a chromosome and within a gene. The fragments are subjected to further analysis that allows for comparison of the polymorphisms in the HLA-DP between the donor’s tissue and the recipient’s blood. This careful analysis of genetic material results in fewer rejection reactions and the chance for a successful transplant.
Cytogenetics
Everyone has 23 pairs of chromosomes, 22 pairs of autosomes and one pair of sex chromosomes. The science that relates to the study of these chromosomes is referred to as “cytogenetics.” Persons who look at chromosome preparations on slides are cytogenetic technologists or cytogeneticists. A trained cytogeneticist examines the number, shape, and staining pattern of these structures using special technologies. In this way, extra chromosomes, missing chromosomes, or rearranged chromosomes can be detected.
Studies of chromosomes begin with the extraction of whole chromosomes from the nuclei of cells. These chromosomes are then placed on glass slides, stained with special stains, and examined under a microscope. Sometimes, pictures are taken of the chromosomes on the slides, and the picture is cut into pieces so the chromosome pairs can be matched. Each chromosome pair is assigned a special number (from 1 to 22, then X and Y) that is based on their staining pattern and size.
There are many disorders that can be diagnosed by examining a person’s whole chromosomes. Down syndrome, in which an individual has an extra chromosome 21, can be determined by cytogenetic studies. When there are three chromosomes in one group instead of a pair, it is referred to as a “trisomy.” Missing chromosomes can also be detected, as in the case of Turner’s syndrome, in which a female has only a single X chromosome. When there is only one chromosome instead of a pair, it is referred to as a “monosomy.”
Abnormalities in chromosome structure are also observed with cytogenetic staining techniques. The Fragile X syndrome, the most common inherited cause of mental retardation, takes its name from the appearance of the stained X chromosome under a microscope. There is a site near the end of this chromosome that does not stain, indicating its fragility. The gene in the fragile region is important in making a special protein needed by developing brain cells.
Sometimes, pieces of a chromosome will break off and attach to another chromosome somewhere in a person’s genome. When this happens, it is referred to as a “translocation.” An example of a disease caused by a translocation would be chronic myelogenous leukemia (CML), in which a part of chromosome 9 breaks off and attaches itself to chromosome 22. Another example would be Burkitt lymphoma, in which a piece of chromosome 8 attaches to chromosome 14. These chromosomal translocations cause disease because the broken piece usually attaches to the new chromosome near a special gene that then becomes activated and produces tumor cells. Translocations can sometimes be seen under the microscope if a special stain is used (via conventional cytogenetic analysis).
A special technique called fluorescence in situ hybridization (FISH) can be used to view changes in chromosomes that result from genetic variations. An aberrant gene segment in a chromosome can be made to “light up” or fluoresce when it is bound by a special probe. Genetic changes in some cancers can be detected using this method. For instance, FISH is one of the methods used to determine increased copy number (amplification) of the gene ERBB2 (also known as HER2/neu) in breast cancer. There are many other applications of FISH technology as well, such as chromosome microdeletions, in which a certain part of a chromosome is completely missing. In this case, the chromosome segment will not fluoresce compared to a normal set of chromosomes.
Infectious disease testing
When you hear the term “infectious disease,” you usually think of something that can infect you and cause a disease process to begin. That “something” can be a bacteria, virus, parasite, or fungus obtained from many different sources (other infected individuals, poor hygiene, transfusion with infected blood, shared needles between drug users, etc.). Disease-causing bacteria and viruses are known as infectious agents, and some of them can be quickly identified by using genetic testing techniques; however, common infectious agents, such as certain bacteria and viruses, are much less expensive to identify using standard laboratory methods that don’t involve genetic testing techniques.
Bacteria are one-celled organisms that contain their own DNA and in some cases can cause serious disease. Even those bacteria that harmlessly live inside your bodies and are involved in beneficial chemical processes can become mutated under unusual conditions and cause you to be very sick. By isolating the DNA from bacteria, breaking it into small pieces, and amplifying them, the bacteria can be identified very quickly. Some of the bacteria that can be quickly identified using these genetic testing techniques include: Chlamydia trachomitis, which is an organism that causes the sexually-transmitted disease chlamydia; Neisseria gonorrhea, which causes gonorrhea, Borrelia burgdorferi which causes Lyme Disease, Legionella pneumophilia which causes Legionnaire’s disease, Mycoplasma pneumoniae which leads to “walking pneumonia,” Mycopbacterium tuberculosis which can cause tuberculosis, and Bordetella pertussis which causes whooping cough. Specimens that might contain these bacteria include urine, blood, sputum, cerebrospinal fluid, and others.
Viruses are unusual organisms that sometimes insert their DNA into a host’s genome. The viral RNA or DNA utilizes the host’s cells to produce proteins and make more viruses. Viruses such as hepatitis C virus (HCV) and human immunodeficiency virus (HIV) are examples of RNA viruses.
Other disease-causing viruses that contain DNA instead of RNA include Herpes simplex virus, cytomegalovirus, Epstein-Barr virus, parvovirus, and varicella-zoster viruses. All of these viruses can be identified by first removing the suspected viral DNA or RNA from a patient specimen and then using it to provide a “fingerprint” of the suspected virus. Specimens usually include blood, cerebrospinal fluid, sputum, other body fluids, amniotic fluid, tissue, or bone marrow. Much of the testing on donor blood that will be used in a blood transfusion utilizes genetic testing to inspect the blood for viral contamination.
Determining how many copies of a virus’ RNA are present in an individual’s blood is another use of infectious disease genetic testing techniques. The number of copies present is typically referred to as the “viral load” or “viral burden.” This testing is usually done after a drug therapy is initiated to assess whether it is working to remove or decrease the viral RNA load. The most common viral load tests are for hepatitis C virus (HCV) or human immunodeficiency virus (HIV), and the tests require a sample of blood.
A parasite is a complex multi-cellular organism. Parasites usually infect an individual through the saliva of a biting insect, such as a mosquito, or through infected material. An example of a parasite that can be identified using genetic tests is Toxoplasma gondii, which can cause encephalitis or congenital infections that lead to severe damage of a fetus (fetal toxoplasmosis).
Research genetic testing
Research genetic testing is used to learn more about the contributions of genes to health and to disease. Sometimes the results may not be directly helpful to participants, but they may benefit others by helping researchers expand their understanding of the human body, health, and disease.
What is direct-to-consumer genetic testing?
Most of the time, genetic testing is done through healthcare providers such as physicians, nurse practitioners, and genetic counselors. Healthcare providers determine which test is needed, order the test from a laboratory, collect and send the DNA sample, interpret the test results, and share the results with the patient. Often, a health insurance company covers part or all of the cost of testing.
Direct-to-consumer genetic testing is different: these genetic tests are marketed directly to customers via television, print advertisements, or the Internet, and the tests can be bought online or in stores. Customers send the company a DNA sample and receive their results directly from a secure website or in a written report. Direct-to-consumer genetic testing provides people access to their genetic information without necessarily involving a healthcare provider or health insurance company in the process.
Dozens of companies currently offer direct-to-consumer genetic tests for a variety of purposes. The most popular tests use genetic variations to make predictions about health, provide information about common traits, and offer clues about a person’s ancestry. The number of companies providing direct-to-consumer genetic testing is growing, along with the range of health conditions and traits covered by these tests. Because there is currently little regulation of direct-to-consumer genetic testing services, it is important to assess the quality of available services before pursuing any testing.
Other names for direct-to-consumer genetic testing include DTC genetic testing, direct-access genetic testing, at-home genetic testing, and home DNA testing. Ancestry testing (also called genealogy testing) is also considered a form of direct-to-consumer genetic testing.
What kinds of direct-to-consumer genetic tests are available?
With so many companies offering direct-to-consumer genetic testing, it can be challenging to determine which tests will be most informative and helpful to you. When considering testing, think about what you hope to get out of the test. Some direct-to-consumer genetic tests are very specific (such as paternity tests), while other services provide a broad range of health, ancestry, and lifestyle information.
Major types of direct-to-consumer genetic tests include:
Disease risk and health
The results of these tests estimate your genetic risk of developing several common diseases, such as celiac disease, Parkinson disease, and Alzheimer disease. Some companies also include a person’s carrier status for less common conditions, including cystic fibrosis and sickle cell disease. A carrier is someone who has one copy of a gene mutation that, when present in two copies, causes a genetic disorder. The tests may also look for genetic variations related to other health-related traits, such as weight and metabolism (how a person’s body converts the nutrients from food into energy).
Ancestry or genealogy
The results of these tests provide clues about where a person’s ancestors might have come from, their ethnicity, and genetic connections between families. For more information, see What is genetic ancestry testing?
Kinship
The results of these tests can indicate whether tested individuals are biologically related to one another. For example, kinship testing can establish whether one person is the biological father of another (paternity testing). The results of direct-to-consumer kinship tests, including paternity tests, are usually not admissible in a court of law.
Lifestyle
The results of these tests claim to provide information about lifestyle factors, such as nutrition, fitness, weight loss, skincare, sleep, and even your wine preferences, based on variations in your DNA. Many of the companies that offer this kind of testing also sell services, products, or programs that they customize on the basis of your test results.
Before choosing a direct-to-consumer genetic test, find out what kinds of health, ancestry, or other information will be reported to you. Think about whether there is any information you would rather not know. In some cases, you can decline to find out specific information if you tell the company before it delivers your results.
What is genetic ancestry testing?
Genetic ancestry testing, or genetic genealogy, is a way for people interested in family history (genealogy) to go beyond what they can learn from relatives or from historical documentation. Examination of DNA variations can provide clues about where a person’s ancestors might have come from and about relationships between families. Certain patterns of genetic variation are often shared among people of particular backgrounds. The more closely related two individuals, families, or populations are, the more patterns of variation they typically share.
Three types of genetic ancestry testing are commonly used for genealogy:
Y chromosome testing
Variations in the Y chromosome, passed exclusively from father to son, can be used to explore ancestry in the direct male line. Y chromosome testing can only be done on males, because females do not have a Y chromosome. However, women interested in this type of genetic testing sometimes recruit a male relative to have the test done. Because the Y chromosome is passed on in the same pattern as are family names in many cultures, Y chromosome testing is often used to investigate questions such as whether two families with the same surname are related.
Mitochondrial DNA testing
This type of testing identifies genetic variations in mitochondrial DNA. Although most DNA is packaged in chromosomes within the cell nucleus, cell structures called mitochondria also have a small amount of their own DNA (known as mitochondrial DNA). Both males and females have mitochondrial DNA, which is passed on from their mothers, so this type of testing can be used by either sex. It provides information about the direct female ancestral line. Mitochondrial DNA testing can be useful for genealogy because it preserves information about female ancestors that may be lost from the historical record because of the way surnames are often passed down.
Single nucleotide polymorphism testing
These tests evaluate large numbers of variations (single nucleotide polymorphisms or SNPs) across a person’s entire genome. The results are compared with those of others who have taken the tests to provide an estimate of a person’s ethnic background. For example, the pattern of SNPs might indicate that a person’s ancestry is approximately 50 percent African, 25 percent European, 20 percent Asian, and 5 percent unknown. Genealogists use this type of test because Y chromosome and mitochondrial DNA test results, which represent only single ancestral lines, do not capture the overall ethnic background of an individual.
Genetic ancestry testing has a number of limitations. Test providers compare individuals’ test results to different databases of previous tests, so ethnicity estimates may not be consistent from one provider to another. Also, because most human populations have migrated many times throughout their history and mixed with nearby groups, ethnicity estimates based on genetic testing may differ from an individual’s expectations. In ethnic groups with a smaller range of genetic variation due to the group’s size and history, most members share many SNPs, and it may be difficult to distinguish people who have a relatively recent common ancestor, such as fourth cousins, from the group as a whole.
Genetic ancestry testing is offered by several companies and organizations. Most companies provide online forums and other services to allow people who have been tested to share and discuss their results with others, which may allow them to discover previously unknown relationships. On a larger scale, combined genetic ancestry test results from many people can be used by scientists to explore the history of populations as they arose, migrated, and mixed with other groups.
What are the pros and cons of direct-to-consumer genetic testing?
Direct-to-consumer genetic testing has both benefits and limitations, although they are somewhat different than those of genetic testing ordered by a healthcare provider.
Benefits
- Direct-to-consumer genetic testing promotes awareness of genetic diseases.
- It provides personalized information about your health, disease risk, and other traits.
- It may help you be more proactive about your health.
- It does not require approval from a healthcare provider or health insurance company.
- It is often less expensive than genetic testing obtained through a healthcare provider.
- DNA sample collection is usually simple and noninvasive, and results are available quickly.
- Your data is added to a large database that can be used to further medical research. Depending on the company, the database may represent up to several million participants.
Risks and limitations
- Tests may not be available for the health conditions or traits that interest you.
- This type of testing cannot tell definitively whether you will or will not get a particular disease.
- Unexpected information that you receive about your health, family relationships, or ancestry may be stressful or upsetting.
- People may make important decisions about disease treatment or prevention based on inaccurate, incomplete, or misunderstood information from their test results.
- There is currently little oversight or regulation of testing companies.
- Unproven or invalid tests can be misleading. There may not be enough scientific evidence to link a particular genetic variation with a given disease or trait.
- Genetic privacy may be compromised if testing companies use your genetic information in an unauthorized way or if your data is stolen.
- The results of genetic testing may impact your ability to obtain life, disability, or long-term care insurance.
Direct-to-consumer genetic testing provides only partial information about your health. Other genetic and environmental factors, lifestyle choices, and family medical history also affect the likelihood of developing many disorders. These factors would be discussed during a consultation with a doctor or genetic counselor, but in many cases they are not addressed when using at-home genetic tests.
Genetic testing during pregnancy
Prenatal genetic testing gives parents-to-be information about whether their fetus has certain genetic disorders. They help your health care provider find out how you and your baby are doing.
You get some prenatal tests several times during pregnancy at your prenatal care checkups. You get other tests at certain times during pregnancy or if you have certain problems that may affect your health and your baby’s health. For example, some prenatal tests check for health conditions in your baby, including:
- Birth defects. These are health conditions that are present at birth. They change the shape or function of one or more parts of the body. Birth defects can cause problems in overall health, how the body develops or how the body works.
- Genetic and chromosomal conditions. These conditions are caused by changes in genes and chromosomes. A gene is part of your body’s cells that stores instructions for the way your body grows and works. A chromosome is the structure in cells that holds genes. Genetic conditions include cystic fibrosis (CF), sickle cell disease and heart defects. A common chromosomal condition is Down syndrome. Sometimes these conditions are passed from parent to child, and sometimes they happen on their own.
If certain health conditions run in your family, you may want to talk with a genetic counselor. A genetic counselor has training to help you understand about genes, birth defects and other medical conditions that run in families, and how they can affect your health and your baby’s health.
Types of prenatal genetic tests
There are two general types of prenatal tests for genetic disorders:
- Prenatal screening tests: These tests can tell you the chances that your fetus has an aneuploidy and a few additional disorders. These tests check if your baby is more likely than others to have a health condition, but they don’t tell you for sure if you baby has a condition. There are no risks to you or your baby when you have a screening test.
- Prenatal diagnostic tests: If a screening test shows your baby is at high risk of a health condition, your provider may recommend a diagnostic test to confirm the results. These tests can tell you whether your fetus actually has certain disorders. These tests are done on cells from the fetus or placenta obtained through amniocentesis or chorionic villus sampling (CVS). Diagnostic tests may have some risks for your baby, like miscarriage. Miscarriage is when a baby dies in the womb before 20 weeks of pregnancy.
Both screening and diagnostic testing are offered to all pregnant women. Screening test results can help you decide if you want to have a diagnostic test. You may or may not want to know if your baby has a health condition. If you decide to have a diagnostic test, you can learn more about your baby’s condition and how to care for your baby after he’s born. You also can make plans to give birth in a hospital that can give your baby special medical care.
What are the different types of prenatal genetic screening tests?
Screening tests can tell you your risk of having a baby with certain disorders. They include carrier screening and prenatal genetic screening tests:
- Carrier screening is done on parents (or those just thinking about becoming parents) using a blood sample or tissue sample swabbed from inside the cheek. These tests are used to find out whether a person carries a gene for certain inherited disorders. Carrier screening can be done before or during pregnancy.
- Prenatal genetic screening tests of the pregnant woman’s blood and findings from ultrasound exams can screen the fetus for aneuploidy; defects of the brain and spine called neural tube defects; and some defects of the abdomen, heart, and facial features. They include first-trimester screening, second-trimester screening, combined first- and second-trimester screening, and cell-free DNA testing.
What prenatal tests are done in the first trimester?
You can have several tests in your first trimester (months 1, 2 and 3). Talk to your provider to find out which tests are right for you.
- Carrier screening for genetic conditions. This screening test checks your blood or saliva to see if you’re a carrier of certain genetic conditions that could affect your baby. If you’re a carrier, you don’t have the condition yourself, but you have a gene change (a change in a gene) for it that you can pass to your baby. If both you and your partner are carriers of the same condition, the risk that your baby has the condition increases. Carrier screening can be done before pregnancy or during the early weeks of pregnancy. If results show that you or your partner is a carrier, you may be able to find out if your baby has the condition or is a carrier of the condition. All women can have carrier screening for CF (cystic fibrosis), spinal muscular atrophy (also called SMA), thalassemias and hemoglobinopathies. Cystic fibrosis is a condition that affects breathing and digestion. Spinal muscular atrophy attacks nerve cells in the spinal cord. It weakens muscles and can affect movement, breathing and swallowing. Thalassemias and hemoglobinopathies are blood conditions that affect red blood cells. Some women get carrier screening for conditions, like Fragile X syndrome and Tay Sachs disease. These conditions run in families or ethnic groups. An ethnic group is a group of people, often from the same country, who share language or culture.
- Cell-free fetal DNA testing (also called noninvasive prenatal screening or testing). This screening test checks your blood for your baby’s DNA to see if he may have certain genetic conditions, like Down syndrome. This test is done after 9 weeks of pregnancy. Your provider may recommend the test if an ultrasound shows that your baby may have a birth defect or if you’ve already had a baby with a birth defect. It’s not recommended if you’re not at risk for having a baby with a birth defect or if you’re pregnant with multiples (more than one baby, like twins or triplets). The test is called noninvasive because it’s a simple blood test that doesn’t require any other tools that break the skin or enter your body. If you have this test, your provider may recommend you have a diagnostic test, like amniocentesis, to confirm the results.
- Chorionic villus sampling (also called CVS). This diagnostic test checks tissue from the placenta to see if your baby has a genetic condition, like Down syndrome. Chorionic villus sampling (CVS) is done at 10 to 13 weeks of pregnancy. Your provider may want you to have CVS if you’re older than 35, if genetic conditions run in your family, or if your first-trimester screening shows that your baby is at increased risk for birth defects.
- Early ultrasound (also called first-trimester ultrasound). Ultrasound uses sound waves and a computer screen to make a picture of your baby inside the womb. Your provider may use early ultrasound exam, called a nuchal translucency screening, that measures the thickness of a space at the back of the fetus’s neck. An abnormal measurement means there is an increased risk that the fetus has Down syndrome or another type of aneuploidy. It also is linked to physical defects of the heart, abdominal wall, and skeleton.
- First-trimester screening. This screening test includes a blood test and an ultrasound to see if your baby may be at risk for some birth defects, like Down syndrome and heart defects. The test usually is done at 11 to 14 weeks of pregnancy.
What tests are done in the second trimester?
Your provider may offer you these prenatal tests in your second trimester (months 4, 5 and 6 of pregnancy):
- Maternal blood screening (also called quad screen). This screening test checks your blood to see if your baby may be at risk for some birth defects, like Down syndrome. It’s called a quad screen because it measures four substances in your blood: alpha-fetoprotein (AFP), estriol, human chorionic gonadotropin (hCG) and inhibin A. The test is done at 15 to 22 weeks of pregnancy.
- Amniocentesis (also called amnio). Amnio is a diagnostic test of the amniotic fluid from around your baby to see if he has a birth defect or genetic condition, like Down syndrome. The test usually is done at 15 to 20 weeks of pregnancy. Your provider may want you to have an amnio for the same reasons as for chorionic villus sampling (CVS). You also may have amnio later in pregnancy to check your baby’s lungs or to see if he has certain infections.
- Ultrasound. Your provider uses ultrasound to check for major physical defects in the brain and spine, facial features, abdomen, heart, and limbs. It’s usually done at 16 to 20 weeks of pregnancy.
- Glucose screening. This screening test checks to see if you may have gestational diabetes. This is a kind of diabetes that some women get during pregnancy. You get this test at 24 to 28 weeks of pregnancy.
What is combined first- and second-trimester screening?
The results from first- and second-trimester tests can be combined in various ways. Combined test results are more accurate than a single test result. If you choose combined screening, keep in mind that final results often are not available until the second trimester.
What is cell-free DNA testing?
Cell-free DNA is the small amount of DNA that is released from the placenta into a pregnant woman’s bloodstream. The cell-free DNA in a sample of a woman’s blood can be screened for Down syndrome, trisomy 13, trisomy 18, and problems with the number of sex chromosomes. This test can be done starting at 10 weeks of pregnancy. It takes about 1 week to get the results. A positive cell-free DNA test result should be followed by a diagnostic test with amniocentesis or CVS.
The cell-free DNA screening test works best for women who already have an increased risk of having a baby with a chromosome disorder. For a woman at low risk of having a baby with a chromosome disorder, conventional screening remains the most appropriate choice. Cell-free DNA testing is not recommended for a woman carrying more than one fetus.
What do the different results of prenatal screening tests mean?
Results of blood screening tests for aneuploidy are reported as the level of risk that the disorder might be present:
- A positive screening test result for aneuploidy means that your fetus is at higher risk of having the disorder compared with the general population. It does not mean that your fetus definitely has the disorder.
- A negative result means that your fetus is at lower risk of having the disorder compared with the general population. It does not rule out the possibility that your fetus has the disorder.
Diagnostic testing with CVS or amniocentesis that gives a more definite result is an option for all pregnant women. Your obstetrician or other health care professional, such as a genetic counselor, will discuss what your screening test results mean and help you decide the next steps.
How accurate are prenatal genetic screening tests?
With any type of testing, there is a possibility of false-positive results and false-negative results. A screening test result that shows there is a problem when one does not exist is called a false-positive result. A screening test result that shows there is not a problem when one does exist is called a false-negative result. Your health care professional can give you information about the rates of false-positive and false-negative results for each test.
What should I consider when deciding whether to have prenatal genetic testing?
It is your choice whether to have prenatal testing. Your personal beliefs and values are important factors in the decision about prenatal testing.
It can be helpful to think about how you would use the results of prenatal screening tests in your pregnancy care. Remember that a positive screening test tells you only that you are at higher risk of having a baby with Down syndrome or another aneuploidy. A diagnostic test should be done if you want to know a more certain result. Some parents want to know beforehand that their baby will be born with a genetic disorder. This knowledge gives parents time to learn about the disorder and plan for the medical care that the child may need. Some parents may decide to end the pregnancy in certain situations.
Other parents do not want to know this information before the child is born. In this case, you may decide not to have follow-up diagnostic testing if a screening test result is positive. Or you may decide not to have any testing at all. There is no right or wrong answer.
Genetic testing for cancer
Cancer is a genetic disease—that is, cancer is caused by certain changes to genes that control the way our cells function, especially how they grow and divide. Genes carry the instructions to make proteins, which do much of the work in our cells. Certain gene changes can cause cells to evade normal growth controls and become cancer. For example, some cancer-causing gene changes increase production of a protein that makes cells grow. Others result in the production of a misshapen, and therefore nonfunctional, form of a protein that normally repairs cellular damage.
Genetic changes that promote cancer can be inherited from your parents if the changes are present in germ cells, which are the reproductive cells of the body (eggs and sperm). Such changes, called germline changes, are found in every cell of the offspring.
Cancer-causing genetic changes can also be acquired during one’s lifetime, as the result of errors that occur as cells divide or from exposure to carcinogenic substances that damage DNA, such as certain chemicals in tobacco smoke, and radiation, such as ultraviolet rays from the sun. Genetic changes that occur after conception are called somatic (or acquired) changes.
There are many different kinds of DNA changes. Some changes affect just one unit of DNA, called a nucleotide. One nucleotide may be replaced by another, or it may be missing entirely. Other changes involve larger stretches of DNA and may include rearrangements, deletions, or duplications of long stretches of DNA.
Sometimes the changes are not in the actual sequence of DNA. For example, the addition or removal of chemical marks, called epigenetic modifications, on DNA can influence whether the gene is “expressed”—that is, whether and how much messenger RNA is produced. Messenger RNA in turn is translated to produce the proteins encoded by the DNA.
In general, cancer cells have more genetic changes than normal cells. But each person’s cancer has a unique combination of genetic alterations. Some of these changes may be the result of cancer, rather than the cause. As the cancer continues to grow, additional changes will occur. Even within the same tumor, cancer cells may have different genetic changes.
Genetic mutations that are harmful may increase a person’s chance, or risk, of developing a disease such as cancer. Overall, inherited mutations are thought to play a role in about 5 to 10 percent of all cancers 4.
Cancer can sometimes appear to “run in families” even if it is not caused by an inherited mutation. For example, a shared environment or lifestyle, such as tobacco use, can cause similar cancers to develop among family members. However, certain patterns—such as the types of cancer that develop, other non-cancer conditions that are seen, and the ages at which cancer typically develops—may suggest the presence of a hereditary cancer syndrome.
The genetic mutations that cause many of the known hereditary cancer syndromes have been identified, and genetic testing can confirm whether a condition is, indeed, the result of an inherited syndrome. Genetic testing is also done to determine whether family members without obvious illness have inherited the same mutation as a family member who is known to carry a cancer-associated mutation.
Inherited genetic mutations can increase a person’s risk of developing cancer through a variety of mechanisms, depending on the function of the gene. Mutations in genes that control cell growth and the repair of damaged DNA are particularly likely to be associated with increased cancer risk.
What genetic tests are available for cancer risk?
More than 50 hereditary cancer syndromes have been described. The majority of these are caused by highly penetrant mutations that are inherited in a dominant fashion. The list below includes some of the more common inherited cancer syndromes for which genetic testing is available, the gene(s) that are mutated in each syndrome, and the cancer types most often associated with these syndromes.
Hereditary breast cancer and ovarian cancer syndrome
- Genes: BRCA1, BRCA2
- Related cancer types: Female breast, ovarian, and other cancers, including prostate, pancreatic, and male breast cancer
Li-Fraumeni syndrome
- Gene: TP53
- Related cancer types: Breast cancer, soft tissue sarcoma, osteosarcoma (bone cancer), leukemia, brain tumors, adrenocortical carcinoma (cancer of the adrenal glands), and other cancers
Cowden syndrome (PTEN hamartoma tumor syndrome)
- Gene: PTEN
- Related cancer types: Breast, thyroid, endometrial (uterine lining), and other cancers
Lynch syndrome (hereditary nonpolyposis colorectal cancer)
- Genes: MSH2, MLH1, MSH6, PMS2, EPCAM
- Related cancer types: Colorectal, endometrial, ovarian, renal pelvis, pancreatic, small intestine, liver and biliary tract, stomach, brain, and breast cancers
Familial adenomatous polyposis
- Gene: APC
- Related cancer types: Colorectal cancer, multiple non-malignant colon polyps, and both non-cancerous (benign) and cancerous tumors in the small intestine, brain, stomach, bone, skin, and other tissues
Retinoblastoma
- Gene: RB1
- Related cancer types: Eye cancer (cancer of the retina), pinealoma (cancer of the pineal gland), osteosarcoma, melanoma, and soft tissue sarcoma
Multiple endocrine neoplasia type 1 (Wermer syndrome)
- Gene: MEN1
- Related cancer types: Pancreatic endocrine tumors and (usually benign) parathyroid and pituitary gland tumors
Multiple endocrine neoplasia type 2
- Gene: RET
- Related cancer types: Medullary thyroid cancer and pheochromocytoma (benign adrenal gland tumor)
Von Hippel-Lindau syndrome
- Gene: VHL
- Related cancer types: Kidney cancer and multiple noncancerous tumors, including pheochromocytoma
Who should consider genetic testing for cancer risk?
Many experts recommend that genetic testing for cancer risk should be strongly considered when all three of the following criteria are met:
- The person being tested has a personal or family history that suggests an inherited cancer risk condition
- The test results can be adequately interpreted (that is, they can clearly tell whether a specific genetic change is present or absent)
- The results provide information that will help guide a person’s future medical care
The features of a person’s personal or family medical history that, particularly in combination, may suggest a hereditary cancer syndrome include:
- Cancer that was diagnosed at an unusually young age
- Several different types of cancer that have occurred independently in the same person
- Cancer that has developed in both organs in a set of paired organs, such as both kidneys or both breasts
- Several close blood relatives that have the same type of cancer (for example, a mother, daughter, and sisters with breast cancer)
- Unusual cases of a specific cancer type (for example, breast cancer in a man)
- The presence of birth defects, such as certain noncancerous (benign) skin growths or skeletal abnormalities, that are known to be associated with inherited cancer syndromes
- Being a member of a racial/ethnic group that is known to have an increased chance of having a certain hereditary cancer syndrome and having one or more of the above features as well
It is strongly recommended that a person who is considering genetic testing speak with a professional trained in genetics before deciding whether to be tested. These professionals can include doctors, genetic counselors, and other health care providers (such as nurses, psychologists, or social workers). Genetic counseling can help people consider the risks, benefits, and limitations of genetic testing in their particular situation. Sometimes the genetic professional finds that testing is not needed.
Genetic counseling includes a detailed review of the individual’s personal and family medical history related to possible cancer risk. Counseling also includes discussions about such issues as:
- Whether genetic testing is appropriate, which specific test(s) might be used, and the technical accuracy of the test(s)
- The medical implications of a positive or a negative test result (see below)
- The possibility that a test result might not be informative—that is, that the information may not be useful in making health care decisions (see below)
- The psychological risks and benefits of learning one’s genetic test results
- The risk of passing a genetic mutation (if one is present in a parent) to children
Learning about these issues is a key part of the informed consent process. Written informed consent is strongly recommended before a genetic test is ordered. People give their consent by signing a form saying that they have been told about, and understand, the purpose of the test, its medical implications, the risks and benefits of the test, possible alternatives to the test, and their privacy rights.
Unlike most other medical tests, genetic tests can reveal information not only about the person being tested but also about that person’s relatives. The presence of a harmful genetic mutation in one family member makes it more likely that other blood relatives may also carry the same mutation. Family relationships can be affected when one member of a family discloses genetic test results that may have implications for other family members. Family members may have very different opinions about how useful it is to learn whether they do or do not have a disease-related genetic mutation. Health discussions may get complicated when some family members know their genetic status while other family members do not choose to know their test results. A conversation with genetics professionals may help family members better understand the complicated choices they may face.
Breast cancer genetic testing
About 5% to 10% of breast cancer cases are thought to be hereditary, meaning that they result directly from gene defects (called mutations) passed on from a parent 5.
BRCA1 and BRCA2 genes
The most common cause of hereditary breast cancer is an inherited mutation in the BRCA1 or BRCA2 gene. In normal cells, these genes help make proteins that repair damaged DNA. Mutated versions of BRCA1 or BRCA2 genes can lead to abnormal cell growth, which can lead to cancer.
- If you have inherited a mutated copy of either gene from a parent, you have a higher risk of breast cancer.
- On average, a woman with a BRCA1 or BRCA2 gene mutation has about a 7 in 10 chance of getting breast cancer by age 80. This risk is also affected by how many other family members have had breast cancer. (It goes up if more family members are affected.)
- Women with one of these mutations are more likely to be diagnosed with breast cancer at a younger age, as well as to have cancer in both breasts. They also have a higher risk of developing some other cancers, mainly ovarian cancer.
- In the United States, BRCA mutations are more common in Jewish people of Ashkenazi (Eastern Europe) origin than in other racial and ethnic groups, but anyone can have them.
In 1990, BRCA1 gene for breast cancer was mapped by genetic linkage to the long arm of chromosome 17, in the interval 17q12-21 6. BRCA2, was localized to the long arm of chromosome 13 through linkage studies of 15 families with multiple cases of breast cancer that were not linked to BRCA1.
Changes in other genes
Other gene mutations can also lead to inherited breast cancers. These gene mutations are much less common, and most of them do not increase the risk of breast cancer as much as the BRCA genes.
- ATM: The ATM gene normally helps repair damaged DNA (or helps kill the cell if the damaged can’t be fixed). Inheriting 2 abnormal copies of this gene causes the disease ataxia-telangiectasia. Inheriting one abnormal copy of this gene has been linked to a high rate of breast cancer in some families.
- TP53: The TP53 gene gives instructions for making a protein called p53 that helps stop the growth of abnormal cells. Inherited mutations of this gene cause Li-Fraumeni syndrome. People with this syndrome have an increased risk of breast cancer, as well as some other cancers such as leukemia, brain tumors, and sarcomas (cancers of bones or connective tissue). This mutation is a rare cause of breast cancer.
- CHEK2: The CHEK2 gene is another gene that normally helps with DNA repair. A CHEK2 mutation can increase breast cancer risk about 2-fold.
- PTEN: The PTEN gene normally helps regulate cell growth. Inherited mutations in this gene can cause Cowden syndrome, a rare disorder that puts people at higher risk for both non-cancer and cancer tumors in the breasts, as well as growths in the digestive tract, thyroid, uterus, and ovaries.
- CDH1: Inherited mutations in this gene cause hereditary diffuse gastric cancer, a syndrome in which people develop a rare type of stomach cancer. Women with mutations in this gene also have an increased risk of invasive lobular breast cancer.
- STK11: Defects in this gene can lead to Peutz-Jeghers syndrome. People affected with this disorder have pigmented spots on their lips and in their mouths, polyps (abnormal growths) in the urinary and digestive tracts, and a higher risk of many types of cancer, including breast cancer.
- PALB2: The PALB2 gene makes a protein that interacts with the protein made by the BRCA2 gene. Mutations in this gene can lead to a higher risk of breast cancer.
Mutations in several other genes have also been linked to breast cancer, but these account for only a small number of cases.
Genetic testing
Genetic testing can be done to look for mutations in the BRCA1 and BRCA2 genes (or less commonly in other genes such as PTEN or TP53). While testing can be helpful in some cases, not every woman needs to be tested, and the pros and cons need to be considered carefully.
One concern is that some genetic tests are promoted to doctors and the public without giving full information. For example, a test for a small number of BRCA1 and BRCA2 gene mutations has been approved by the FDA. However, there are more than 1,000 known BRCA mutations, and the ones included in the approved test are not the most common ones. This means there are many BRCA mutations that would not be detected by this test.
If you’re thinking about genetic testing, it’s strongly recommended that you first talk to a genetic counselor, nurse, or doctor who can explain these tests. It’s very important to understand what genetic testing can and can’t tell you, and to carefully weigh the benefits and risks of genetic testing before these tests are done. Testing costs a lot and might not be covered by some health insurance plans.
How does DNA testing work
Once a person decides to proceed with genetic testing, a medical geneticist, primary care doctor, specialist, or nurse practitioner can order the test. Genetic testing is often done as part of a genetic consultation.
Genetic tests are performed on a sample of blood, hair, skin, amniotic fluid (the fluid that surrounds a fetus during pregnancy), or other tissue. For example, a procedure called a buccal smear uses a small brush or cotton swab to collect a sample of cells from the inside surface of the cheek. The sample is sent to a laboratory where technicians look for specific changes in chromosomes, DNA, or proteins, depending on the suspected disorder. The laboratory reports the test results in writing to a person’s doctor or genetic counselor, or directly to the patient if requested.
Newborn screening tests are done on a small blood sample, which is taken by pricking the baby’s heel. Unlike other types of genetic testing, a parent will usually only receive the result if it is positive. If the test result is positive, additional testing is needed to determine whether the baby has a genetic disorder.
Before a person has a genetic test, it is important that he or she understands the testing procedure, the benefits and limitations of the test, and the possible consequences of the test results. The process of educating a person about the test and obtaining permission is called informed consent.
Informed consent
Before a person has a genetic test, it is important that he or she fully understands the testing procedure, the benefits and limitations of the test, and the possible consequences of the test results. The process of educating a person about the test and obtaining permission to carry out testing is called informed consent. “Informed” means that the person has enough information to make an educated decision about testing; “consent” refers to a person’s voluntary agreement to have the test done.
In general, informed consent can only be given by adults who are competent to make medical decisions for themselves. For children and others who are unable to make their own medical decisions (such as people with impaired mental status), informed consent can be given by a parent, guardian, or other person legally responsible for making decisions on that person’s behalf.
Informed consent for genetic testing is generally obtained by a doctor or genetic counselor during an office visit. The healthcare provider will discuss the test and answer any questions. If the person wishes to have the test, he or she will then usually read and sign a consent form.
Several factors are commonly included on an informed consent form:
- A general description of the test, including the purpose of the test and the condition for which the testing is being performed.
- How the test will be carried out (for example, a blood sample).
- What the test results mean, including positive and negative results, and the potential for uninformative results or incorrect results such as false positives or false negatives.
- Any physical or emotional risks associated with the test.
- Whether the results can be used for research purposes.
- Whether the results might provide information about other family members’ health, including the risk of developing a particular condition or the possibility of having affected children.
- How and to whom test results will be reported and under what circumstances results can be disclosed (for example, to health insurance providers).
- What will happen to the test specimen after the test is complete.
- Acknowledgement that the person requesting testing has had the opportunity to discuss the test with a healthcare professional.
- The individual’s signature, and possibly that of a witness.
The elements of informed consent may vary, because some states have laws that specify factors that must be included. (For example, some states require disclosure that the test specimen will be destroyed within a certain period of time after the test is complete.)
Informed consent is not a contract, so a person can change his or her mind at any time after giving initial consent. A person may choose not to go through with genetic testing even after the test sample has been collected. A person simply needs to notify the healthcare provider if he or she decides not to continue with the testing process.
Testing genetic material
Testing of genetic material is performed on a variety of specimens including blood, urine, saliva, stool, body tissues, bone, or hair. Cells in these samples are isolated and the nucleic acids (DNA or sometimes RNA) within them is extracted and examined for possible mutations or alterations. Looking at small portions of the DNA within a gene requires specialized and specific laboratory testing. This is done to pinpoint the exact location of genetic errors. This section will focus on the examination of a person’s genes to look for the one(s) responsible for a particular disease.
There are four basic reasons that genetic material is tested for clinical reasons.
- Presymptomatic testing identifies the presence of variant genes that cause disease even if the physical abnormalities associated with the disease are not yet present in an individual.
- Diagnostic genetic testing is performed on a symptomatic individual with symptoms sufficiently suggestive of a genetic disorder. This assists the individual’s physician in making a clear diagnosis.
- Testing of genetic material can also be performed as a prenatal screening tool to assess whether two individuals who wish to become parents have an autosomal or X-linked recessive gene that, when combined in a child, will produce a serious disorder in that child. This type of genetic testing is referred to as carrier screening.
- Fetuses developing in the uterus can also have their genetic material tested to assess their health status if it is thought to be in jeopardy.
To test DNA for medical reasons, some type of cellular material is required. This material can come from blood, urine, saliva, body tissues, bone marrow, hair, amniotic fluid (amniocentesis) or the placenta (chorionic villus sampling). The material can be submitted in a tube, on a swab, in a container, or frozen. If the test requires RNA, the same materials can be used. Once received in the laboratory, the cells are removed from the substance they are in, broken apart, and the DNA in the nuclei is isolated and extracted.
The laboratory professionals who perform and interpret these tests are specially trained physicians and scientists. The extracted DNA is manipulated in different ways in order for the molecular pathologist or genetic technologist to see what might be missing or mutated in such a way as to cause disease. One type of manipulation is “cutting” the DNA into small pieces using special enzymes. These small pieces are much easier to test than the long strands of uncut DNA and they contain the genes of interest. Another manipulation is to apply the extracted and cut DNA to an agarose gel, apply an electrical field to the gel, and see how the DNA moves on the gel. This can indicate differences in the size of the pieces of the cut DNA that might be caused by specific mutations.
Other manipulations to DNA include amplification, sequencing, or a special procedure called hybridization. When the results of these tests are examined and compared with results from a normal person, it is possible to see differences in the genes that might cause a disease.
Testing for products of genetic expression
Many inherited disorders are identified indirectly by examining abnormalities in the genetic end products (proteins or metabolites) that are present in abnormal forms or quantities. As a reminder, genes code for the production of thousands of proteins and, if there is an error in the code, changes can occur in the production of those proteins. So, rather than detecting the problem in the gene, some types of testing look for unusual findings related to the pertinent proteins, such as their absence.
An example of testing for genetic products includes those widely used to screen newborns for a variety of disorders. For example, newborns are tested for phenylketonuria (PKU), an inherited autosomal recessive metabolic disorder caused by a variation in a gene that makes a special enzyme that breaks down phenylalanine, an amino acid. When too much of this substance builds up in blood, it can lead to mental retardation if not treated early in life with a special, restricted diet. The test uses a blood sample from a baby’s heel to look for the presence of extra phenylalanine, rather than looking for the mutated gene itself. Other examples include blood tests for congenital hypothyroidism, diagnosed by low blood levels or absence of thyroid hormone, and congenital adrenal hyperplasia, a genetic disease that causes the hormone cortisol to be decreased in blood. Frequently, abnormal blood screening tests in the newborn may be augmented by genetic testing when appropriate (in cystic fibrosis, for example).
Risks
Generally genetic tests have little physical risk. Blood and cheek swab tests have almost no risk. However, prenatal testing such as amniocentesis or chorionic villus sampling has a small risk of pregnancy loss (miscarriage).
Genetic testing can have emotional, social and financial risks as well. Discuss all risks and benefits of genetic testing with your doctor, a medical geneticist or a genetic counselor before you have a genetic test.
How you prepare
Before you have genetic testing, gather as much information as you can about your family’s medical history. Then, talk with your doctor or a genetic counselor about your personal and family medical history to better understand your risk. Ask questions and discuss any concerns about genetic testing at that meeting. Also, talk about your options, depending on the test results.
If you’re being tested for a genetic disorder that runs in families, you may want to consider discussing your decision to have genetic testing with your family. Having these conversations before testing can give you a sense of how your family might respond to your test results and how it may affect them.
Not all health insurance policies pay for genetic testing. So, before you have a genetic test, check with your insurance provider to see what will be covered.
In the United States, the federal Genetic Information Nondiscrimination Act of 2008 (GINA) helps prevent health insurers or employers from discriminating against you based on test results. Under GINA, employment discrimination based on genetic risk also is illegal. However, this act does not cover life, long-term care or disability insurance. Most states offer additional protection.
What you can expect
Depending on the type of test, a sample of your blood, skin, amniotic fluid or other tissue will be collected and sent to a lab for analysis.
- Blood sample. A member of your health care team takes the sample by inserting a needle into a vein in your arm. For newborn screening tests, a blood sample is taken by pricking your baby’s heel.
- Cheek swab. For some tests, a swab sample from the inside of your cheek is collected for genetic testing.
- Amniocentesis. In this prenatal genetic test, your doctor inserts a thin, hollow needle through your abdominal wall and into your uterus to collect a small amount of amniotic fluid for testing.
- Chorionic villus sampling. For this prenatal genetic test, your doctor takes a tissue sample from the placenta. Depending on your situation, the sample may be taken with a tube (catheter) through your cervix or through your abdominal wall and uterus using a thin needle.
Genetic test results
The amount of time it takes for you to receive your genetic test results depends on the type of test and your health care facility. Talk to your doctor, medical geneticist or genetic counselor before the test about when you can expect the results and have a discussion about them.
Positive results
If the genetic test result is positive, that means the genetic change that was being tested for was detected. The steps you take after you receive a positive result will depend on the reason you had genetic testing.
If the purpose is to:
- Diagnose a specific disease or condition, a positive result will help you and your doctor determine the right treatment and management plan.
- Find out if you are carrying a gene that could cause disease in your child, and the test is positive, your doctor, medical geneticist or a genetic counselor can help you determine your child’s risk of actually developing the disease. The test results can also provide information to consider as you and your partner make family planning decisions.
- Determine if you might develop a certain disease, a positive test doesn’t necessarily mean you’ll get that disorder. For example, having a breast cancer gene (BRCA1 or BRCA2) means you’re at high risk of developing breast cancer at some point in your life, but it doesn’t indicate with certainty that you’ll get breast cancer. However, with some conditions, such as Huntington’s disease, having the altered gene does indicate that the disease will eventually develop.
Talk to your doctor about what a positive result means for you. In some cases, you can make lifestyle changes that may reduce your risk of developing a disease, even if you have a gene that makes you more susceptible to a disorder. Results may also help you make choices related to treatment, family planning, careers and insurance coverage.
In addition, you may choose to participate in research or registries related to your genetic disorder or condition. These options may help you stay updated with new developments in prevention or treatment.
Negative results
A negative result means a mutated gene was not detected by the test, which can be reassuring, but it’s not a 100 percent guarantee that you don’t have the disorder. The accuracy of genetic tests to detect mutated genes varies, depending on the condition being tested for and whether or not the gene mutation was previously identified in a family member.
Even if you don’t have the mutated gene, that doesn’t necessarily mean you’ll never get the disease. For example, the majority of people who develop breast cancer don’t have a breast cancer gene (BRCA1 or BRCA2). Also, genetic testing may not be able to detect all genetic defects.
Inconclusive results
In some cases, a genetic test may not provide helpful information about the gene in question. Everyone has variations in the way genes appear, and often these variations don’t affect your health. But sometimes it can be difficult to distinguish between a disease-causing gene and a harmless gene variation. These changes are called variants of uncertain significance. In these situations, follow-up testing or periodic reviews of the gene over time may be necessary.
Genetic counseling
No matter what the results of your genetic testing, talk with your doctor, medical geneticist or genetic counselor about questions or concerns you may have. This will help you understand what the results mean for you and your family.
A genetic counseling or consultation is a health service that provides information and support to people who have, or may be at risk for, genetic disorders. During a consultation, a genetics professional meets with an individual or family to discuss genetic risks or to diagnose, confirm, or rule out a genetic condition.
Genetics professionals include medical geneticists (doctors who specialize in genetics) and genetic counselors (certified healthcare workers with experience in medical genetics and counseling). Other healthcare professionals such as nurses, psychologists, and social workers trained in genetics can also provide genetic consultations.
Consultations usually take place in a doctor’s office, hospital, genetics center, or other type of medical center. These meetings are most often in-person visits with individuals or families, but they are occasionally conducted in a group or over the telephone.
How can consumers be sure a genetic test is valid and useful?
Before undergoing genetic testing, it is important to be sure that the test is valid and useful. A genetic test is valid if it provides an accurate result. Two main measures of accuracy apply to genetic tests: analytical validity and clinical validity. Another measure of the quality of a genetic test is its usefulness, or clinical utility.
- Analytical validity refers to how well the test predicts the presence or absence of a particular gene or genetic change. In other words, can the test accurately detect whether a specific genetic variant is present or absent?
- Clinical validity refers to how well the genetic variant being analyzed is related to the presence, absence, or risk of a specific disease.
- Clinical utility refers to whether the test can provide information about diagnosis, treatment, management, or prevention of a disease that will be helpful to a consumer.
All laboratories that perform health-related testing, including genetic testing, are subject to federal regulatory standards called the Clinical Laboratory Improvement Amendments (CLIA) or even stricter state requirements. Clinical Laboratory Improvement Amendments (CLIA) standards cover how tests are performed, the qualifications of laboratory personnel, and quality control and testing procedures for each laboratory. By controlling the quality of laboratory practices, Clinical Laboratory Improvement Amendments (CLIA) standards are designed to ensure the analytical validity of genetic tests.
Clinical Laboratory Improvement Amendments (CLIA) standards do not address the clinical validity or clinical utility of genetic tests. The Food and Drug Administration (FDA) requires information about clinical validity for some genetic tests. Additionally, the state of New York requires information on clinical validity for all laboratory tests performed for people living in that state. Consumers, health providers, and health insurance companies are often the ones who determine the clinical utility of a genetic test.
It can be difficult to determine the quality of a genetic test sold directly to the public. Some providers of direct-to-consumer genetic tests are not CLIA-certified, so it can be difficult to tell whether their tests are valid. If providers of direct-to-consumer genetic tests offer easy-to-understand information about the scientific basis of their tests, it can help consumers make more informed decisions. It may also be helpful to discuss any concerns with a health professional before ordering a direct-to-consumer genetic test.
Pros and Cons of genetic testing
Benefits of genetic testing
Genetic testing may be beneficial whether the test identifies a mutation or not. For some people, test results serve as a relief, eliminating some of the uncertainty surrounding their health. These results may also help doctors make recommendations for treatment or monitoring, and give people more information for making decisions about their and their family’s health, allowing them to take steps to lower his/her chance of developing a disease. For example, as the result of such a finding, someone could be screened earlier and more frequently for the disease and/or could make changes to health habits like diet and exercise. Such a genetic test result can lower a person’s feelings of uncertainty, and this information can also help people to make informed choices about their future, such as whether to have a baby.
Drawbacks of genetic testing
Genetic testing has a generally low risk of negatively impacting your physical health. However, it can be difficult financially or emotionally to find out your results. Clinical genetic tests are not just descriptive as many laboratory tests are (such as describing the glucose level in your blood), but they are predictive as well. Predictive tests will not give a yes/no answer, but instead will tell what the chances are of developing a particular genetic condition. Such results are not definitive and may leave a person wondering what to do with those results, particularly if available treatments or therapies limit the course of action.
Emotional: Learning that you or someone in your family has or is at risk for a disease can be scary. Some people can also feel guilty, angry, anxious, or depressed when they find out their results.
Financial: Genetic testing can cost anywhere from less than $100 to more than $2,000. Health insurance companies may cover part or all of the cost of testing.
Many people are worried about discrimination based on their genetic test results. In 2008, Congress enacted the Genetic Information Nondiscrimination Act (GINA) to protect people from discrimination by their health insurance provider or employer. GINA does not apply to long-term care, disability, or life insurance providers.
Limitations of testing: Genetic testing cannot tell you everything about inherited diseases. For example, a positive result does not always mean you will develop a disease, and it is hard to predict how severe symptoms may be. Geneticists and genetic counselors can talk more specifically about what a particular test will or will not tell you, and can help you decide whether to undergo testing.
- A particular genetic test will only tell if there is specific genetic variant, or mutation; it cannot guarantee whether the disease will develop nor can the test provide information about other genetic diseases not being specifically looked for by that test.
- While genetic test may detect a particular problem gene, it cannot predict how severely the person carrying that gene will be affected. Again with cystic fibrosis, symptoms may be mild bronchial abnormalities or they may range to severe lung, pancreatic, and intestinal problems depending on the specific mutation present.
- Many genetic tests cannot detect all of the variations that can cause a particular disease. For instance, with genetic testing for cystic fibrosis, most genetic testing panels only look for the more common variants, not all of those that are associated with this disease.
- Many diseases are the result of an interaction between one’s genes and one’s environment. The way in which these interactions cause disease is not clearly understood. Examples of these diseases include coronary heart disease, type 2 diabetes, obesity, and Alzheimer disease.
Legal issues, such as patient privacy, use of genetic testing to determine insurance coverage, and the use of archived patient samples are some of the broader social issues to be considered.
Because of these limitations, genetic test results can be a mixed blessing. An absolutely essential component of clinical genetics testing is giving your informed consent to do the tests and knowing what you want to do with the results of these tests. Know your legal rights as well. Make certain that your privacy is respected. Educate yourself about genetic tests, and talk to your medical provider if you think you should have genetic testing performed. This is especially important as more genetic testing becomes available directly to consumers.
How do I decide whether to be tested?
There are many reasons that people might get genetic testing. Doctors might suggest a genetic test if patients or their families have certain patterns of disease. Genetic testing is voluntary and the decision about whether to have genetic testing is complex.
A geneticist or genetic counselor can help families think about the benefits and limitations of a particular genetic test. Genetic counselors help individuals and families understand the scientific, emotional, and ethical factors surrounding the decision to have genetic testing and how to deal with the results of those tests.
How do I find a genetic professional?
Your health care provider may refer you to a genetic professional. Universities and medical centers also often have affiliated genetic professionals, or can provide referrals to a genetic professional or genetics clinic.
As more has been learned about genetics, genetic professionals have grown more specialized. For example, they may specialize in a particular disease (such as cancer genetics), an age group (such as adolescents) or a type of counseling (such as prenatal).
How do I decide whether I need to see a geneticist or other specialist?
Your health care provider may refer you to a geneticist – a medical doctor or medical researcher – who specializes in your disease or disorder. A medical geneticist has completed a fellowship or has other advanced training in medical genetics. While a genetic counselor or genetic nurse may help you with testing decisions and support issues, a medical geneticist will make the actual diagnosis of a disease or condition. Many genetic diseases are so rare that only a geneticist can provide the most complete and current information about your condition.
Along with a medical geneticist, you may also be referred to a physician who is a specialist in the type of disorder you have. For example, if a genetic test is positive for colon cancer, you might be referred to an oncologist. For a diagnosis of Huntington disease, you may be referred to a neurologist.
- What is DNA? https://ghr.nlm.nih.gov/primer/basics/dna[↩]
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/gene[↩]
- What is noncoding DNA? https://ghr.nlm.nih.gov/primer/basics/noncodingdna[↩]
- Genetic Testing for Hereditary Cancer Syndromes. https://www.cancer.gov/about-cancer/causes-prevention/genetics/genetic-testing-fact-sheet[↩]
- Breast Cancer Risk Factors You Cannot Change. https://www.cancer.org/cancer/breast-cancer/risk-and-prevention/breast-cancer-risk-factors-you-cannot-change.html[↩]
- Hall JM, Lee MK, Newman B, et al.: Linkage of early-onset familial breast cancer to chromosome 17q21. Science 250 (4988): 1684-9, 1990.[↩]