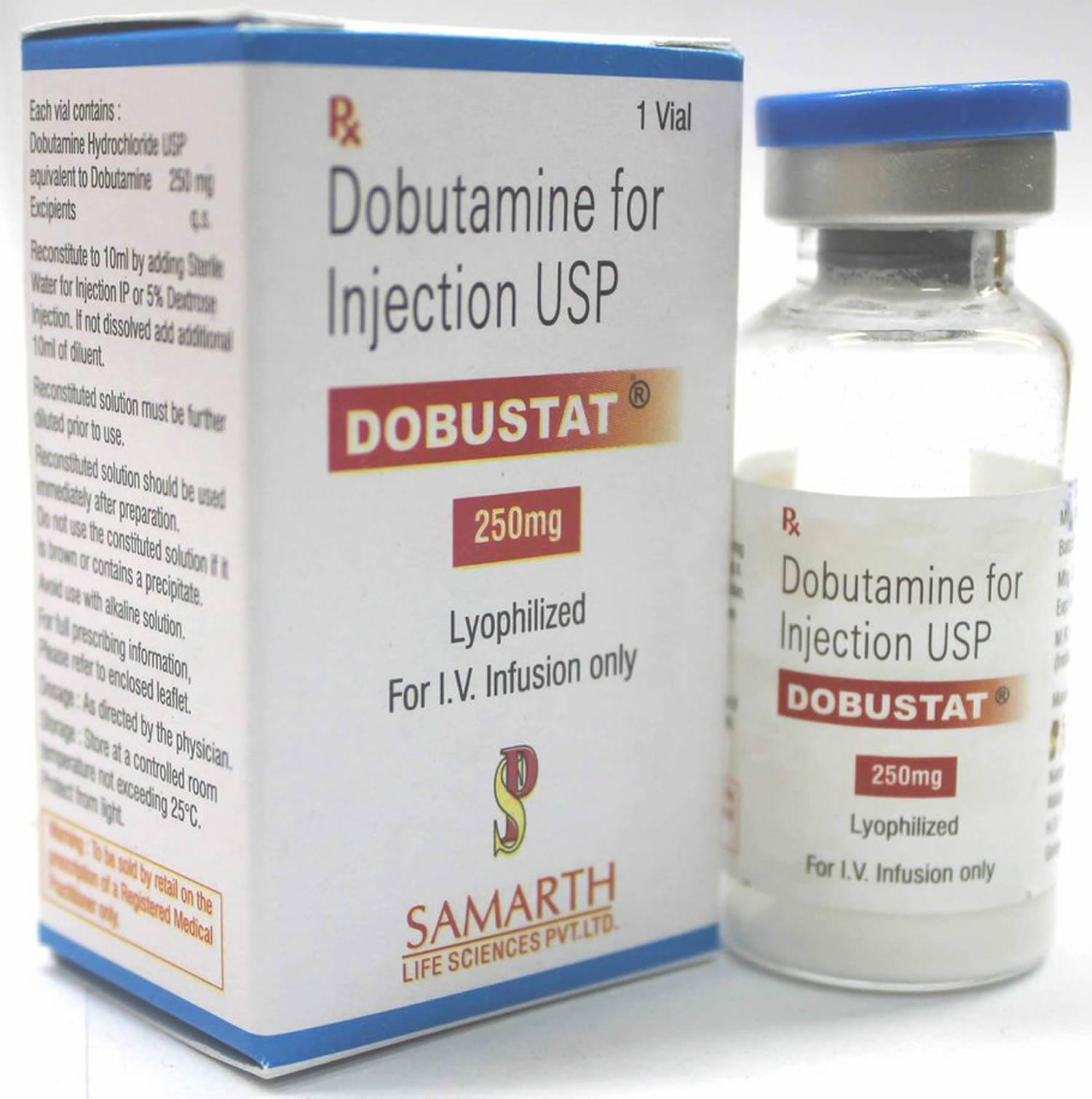
What is dobutamine
Dobutamine is a synthetic catecholamine with sympathomimetic activity that is often used to stimulate your heart muscle and improves blood flow by helping your heart pump better. Dobutamine is a direct-acting inotropic agent and an adrenergic agonist that stimulates primarily the beta-1 adrenoceptor, with lesser effect on beta-2 or alpha receptors. Via beta-1 adrenoceptor of the heart, Dobutamine induces positive inotropic effect with minimal changes in chronotropic activities or systemic vascular resistance. Dobutamine also causes vasodilation by stimulating beta-2 adrenergic receptors in blood vessels, augmented by reflex vasoconstriction resulting in increased cardiac output.
Dobutamine is used short-term to treat cardiac decompensation due to weakened heart muscle.
Dobutamine is usually given after other heart medicines have been tried without success.
Dobutamine may also be used for purposes not listed in this medication guide.
Dobutamine Contraindications
Dobutamine hydrochloride is contraindicated in patients with idiopathic hypertrophic subaortic stenosis and in patients who have shown previous manifestations of hypersensitivity to dobutamine injection. Dobutamine is contraindicated in patients with idiopathic hypertrophic subaortic stenosis because Dobutamine’s strong inotropic effect is potentially harmful in the presence of such severe mechanical obstruction.
Dobutamine Warnings
Dobutamine administration may produce symptomatic benefits in patients with acute decompensated heart failure, however, routine use of intermittent inotropic infusions has been shown to increase mortality in patients with chronic heart failure. The American Heart Association guidelines for management of chronic heart failure recommend that intermittent intravenous positive inotropic therapy has no proven value in patients with Stage C chronic heart failure; however, the guidelines suggest that continuous intravenous inotrope infusions may be considered for palliation of symptoms in patients with end-stage heart failure (e.g., Stage D).
Increase in Heart Rate or Blood Pressure
Dobutamine hydrochloride may cause a marked increase in heart rate or blood pressure, especially systolic pressure. Approximately 10% of patients in clinical studies have had rate increases of 30 beats/minute or more, and about 7.5% have had a 50 mm Hg or greater increase in systolic pressure. Usually, reduction of dosage promptly reverses these effects. Because Dobutamine hydrochloride facilitates atrioventricular conduction, patients with atrial fibrillation are at risk of developing rapid ventricular response. Patients with pre-existing hypertension appear to face an increased risk of developing an exaggerated pressor response.
Ectopic Activity
Dobutamine hydrochloride may precipitate or exacerbate ventricular ectopic activity, but it rarely has caused ventricular tachycardia.
Hypersensitivity
Reactions suggestive of hypersensitivity associated with administration of Dobutamine injection, including skin rash, fever, eosinophilia, and bronchospasm, have been reported occasionally.
Dobutamine injection contains sodium metabisulfite, a sulfite that may cause allergic-type reactions, including anaphylactic symptoms and life-threatening or less severe asthmatic episodes, in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
Corn hypersensitivity and sulfite hypersensitivity
Dobutamine is contraindicated in patients with a hypersensitivity to dobutamine or any of its components. Formulations containing dextrose (e.g., premixed bags) may be contraindicated in patients with a known corn hypersensitivity. Some preparations of dobutamine contain sulfites; use these preparations with caution in individuals with sulfite hypersensitivity because these antioxidant compounds can cause allergic reactions, including anaphylaxis. This reaction appears to be more common in patients with asthma than non-asthmatic patients.
Dobutamine Injection Precautions
General
- During the administration of Dobutamine injection, as with any adrenergic agent, ECG and blood pressure should be continuously monitored. In addition, pulmonary wedge pressure and cardiac output should be monitored whenever possible to aid in the safe and effective infusion of Dobutamine hydrochloride.
- Hypovolemia should be corrected with suitable volume expanders before treatment with Dobutamine hydrochloride is instituted.
- No improvement may be observed in the presence of marked mechanical obstruction, such as severe valvular aortic stenosis.
Usage Following Acute Myocardial Infarction
Clinical experience with Dobutamine hydrochloride following myocardial infarction has been insufficient to establish the safety of the drug for this use. There is concern that any agent that increases contractile force and heart rate may increase the size of an infarction by intensifying ischemia, but it is not known whether Dobutamine hydrochloride does so.
Hypovolemia
Do not administer dobutamine to patients with uncorrected hypovolemia; correct hypovolemia with volume expanders before initiating dobutamine.
Geriatric hypotension
Geriatric patients may have a variable dose-response to dobutamine. In general, the initial dose for an elderly patient should start at the low end of the dosing range. Reported clinical experience with dobutamine suggests that the incidence of significant hypotension is a function of both dose and age, with elderly patients having a greater incidence of hypotension.
Atrial fibrillation, cardiac arrhythmias, ventricular arrhythmias
Use dobutamine with caution in patients with cardiac arrhythmias such as atrial fibrillation and ventricular arrhythmias. Dobutamine increases atrioventricular conduction; patients with atrial fibrillation should be adequately digitalized before administration of dobutamine. Dobutamine may precipitate or exacerbate ventricular ectopic activity. Dobutamine may be associated with sinus tachycardia or premature ventricular contractions (PVCs) due to its stimulatory effect on cardiac conduction. Dobutamine rarely induces ventricular tachycardia; however it can cause a marked increase in heart rate in susceptible patients.
Acute myocardial infarction, angina, coronary artery disease, hypertension
Use dobutamine with caution in patients with certain types of cardiac disease including acute myocardial infarction, unstable angina, or severe coronary artery disease because dobutamine can intensify or extend myocardial ischemia. Use dobutamine with caution in patients with hypertension as these patients are at risk for developing an exaggerated pressor response.
Laboratory Tests
Dobutamine, like other β2-agonists, can produce a mild reduction in serum potassium concentration, rarely to hypokalemic levels. Accordingly, consideration should be given to monitoring serum potassium.
Drug Interactions
Animal studies indicate that Dobutamine may be ineffective if the patient has recently received a β-blocking drug. In such a case, the peripheral vascular resistance may increase.
Preliminary studies indicate that the concomitant use of Dobutamine and nitroprusside results in a higher cardiac output and, usually, a lower pulmonary wedge pressure than when either drug is used alone.
There was no evidence of drug interactions in clinical studies in which Dobutamine was administered concurrently with other drugs, including digitalis preparations, furosemide, spironolactone, lidocaine, nitroglycerin, isosorbide dinitrate, morphine, atropine, heparin, protamine, potassium chloride, folic acid, and acetaminophen.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies to evaluate the carcinogenic or mutagenic potential of Dobutamine hydrochloride, or its potential to affect fertility, have not been conducted.
Pregnancy – Teratogenic Effects
Dobutamine is classified as FDA pregnancy risk category B. Animal studies have revealed no toxicities; however, no adequate or well-controlled pregnancy studies have been done in humans. Use of dopamine during pregnancy should be avoided unless the potential benefits outweigh the unknown potential risks to the fetus.
Reproduction studies performed in rats at doses up to the normal human dose (10 mcg/kg/min for 24 h, total daily dose of 14.4 mg/kg), and in rabbits at doses up to twice the normal human dose, have revealed no evidence of harm to the fetus due to Dobutamine hydrochloride. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery
The effect of Dobutamine hydrochloride on labor and delivery is unknown.
Breastfeeding Mothers
According to the manufacturer, it is not known whether dobutamine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when administering dobutamine to a breast-feeding woman. If a mother requires dobutamine therapy, the manufacturer recommends that breast-feeding be discontinued for the duration of drug administration. Consider the benefits of breast-feeding, the risk of potential infant drug exposure, and the risk of an untreated or inadequately treated condition. If a breast-feeding infant experiences an adverse effect related to a maternally administered drug, healthcare providers are encouraged to report the adverse effect to the FDA.
Pediatric Use
The safety and effectiveness of Dobutamine injection for use in pediatric patients have not been studied.
Premature neonates
Dobutamine has been shown to increase cardiac output and systemic pressure in pediatric patients of every age group. In premature neonates, however, dobutamine is less effective than dopamine in raising systemic blood pressure without causing undue tachycardia, and dobutamine has not been shown to provide any added benefit when given to such infants already receiving optimal infusions of dopamine. In addition, because of variation in development, there is significant interpatient variability in response to dobutamine in neonates. Very preterm neonates are likely to have an attenuated reduction in systemic vascular resistance (SVR) compared to term neonates and therefore, experience a more pronounced increase in blood pressure. Titrate dosage carefully with close monitoring.
Renal failure
Monitor patients with renal failure carefully during dobutamine administration. Reports indicate that the continuous infusion of dobutamine in patients with end stage renal disease may produce myoclonia (e.g., muscle spasms). Although etiology of this reaction remains unclear, proposed mechanisms include an increase in dobutamine uptake by the central nervous system secondary to renal failure and an increase in the permeability of the blood-brain barrier caused by P-glycoprotein inhibition of concomitant medications.
Dobutamine mechanism of action
Dobutamine hydrochloride is a direct-acting inotropic agent whose primary activity results from stimulation of the β receptors of the heart while producing comparatively mild chronotropic, hypertensive, arrhythmogenic, and vasodilative effects. Dobutamine directly stimulates beta-1 receptors of the heart to increase myocardial contractility and stroke volume, resulting in increased cardiac output. Dobutamine does not cause the release of endogenous norepinephrine, as does dopamine. In animal studies, Dobutamine hydrochloride produces less increase in heart rate and less decrease in peripheral vascular resistance for a given inotropic effect than does isoproterenol.
In patients with depressed cardiac function, both Dobutamine hydrochloride and isoproterenol increase the cardiac output to a similar degree. In the case of Dobutamine hydrochloride, this increase is usually not accompanied by marked increases in heart rate (although tachycardia is occasionally observed), and the cardiac stroke volume is usually increased. In contrast, isoproterenol increases the cardiac index primarily by increasing the heart rate while stroke volume changes little or declines.
Facilitation of atrioventricular conduction has been observed in human electrophysiologic studies and in patients with atrial fibrillation.
Systemic vascular resistance is usually decreased with administration of Dobutamine hydrochloride. Occasionally, minimum vasoconstriction has been observed.
Most clinical experience with Dobutamine hydrochloride is short-term − not more than several hours in duration. In the limited number of patients who were studied for 24, 48, and 72 hours, a persistent increase in cardiac output occurred in some, whereas output returned toward baseline values in others.
The onset of action of Dobutamine is within 1 to 2 minutes; however, as much as 10 minutes may be required to obtain the peak effect of a particular infusion rate.
The plasma half-life of Dobutamine hydrochloride in humans is 2 minutes. The principal routes of metabolism are methylation of the catechol and conjugation. In human urine, the major excretion products are the conjugates of Dobutamine and 3-O-methyl Dobutamine. The 3-O-methyl derivative of Dobutamine is inactive.
Alteration of synaptic concentrations of catecholamines with either reserpine or tricyclic antidepressants does not alter the actions of Dobutamine in animals, which indicates that the actions of Dobutamine hydrochloride are not dependent on presynaptic mechanisms.
Dobutamine uses
Dobutamine injection is indicated when parenteral therapy is necessary for inotropic support in the short-term treatment of adults with cardiac decompensation due to depressed contractility resulting either from organic heart disease, congestive heart failure, cardiogenic shock, septic shock (off-label use) or from cardiac surgical procedures.
In patients who have atrial fibrillation with rapid ventricular response, a digitalis preparation should be used prior to institution of therapy with Dobutamine hydrochloride.
Dobutamine stress echo
Dobutamine stress echocardiography is a non-invasive method with established accuracy for diagnosing coronary artery disease 1. Dobutamine infusion in combination with radionuclide myocardial perfusion imaging is an alternative pharmacological stress test for detection of myocardial ischemia in patient who is not able to tolerate dipyridamole or adenosine infusion. It is commonly used in patients with chronic obstructive pulmonary disease (COPD) 2.
As a catecholamine with predominant β1 receptor against, dobutamine increases heart rate, systolic blood pressure and myocardial contractility. Consequently, myocardial oxygen demand increases. Although its hemodynamic effect is similar to physical exercise, dobutamine stress test is not a substitute for exercise stress test. Serious side effects may occur during dobutamine stress test including myocardial infarction (heart attack), ventricular arrhythmia, hypotension and prolonged ischemia 3. However ST-segment elevation with chest pain is a rare event in dobutamine stress test with myocardial perfusion imaging.
Numerous studies have demonstrated that dobutamine stress test in association with radionuclide or echocardiographic imaging is sensitive and specific diagnostic test for coronary artery disease. In order to maintain sensitivity of dobutamine stress test, it is important to reach target heart rate during the test. Atropine is usually combined with dobutamine infusion to increase heart rate. It has been demonstrated that β-agonists treatment shortly prior to dobutamine stress test reduced amounts and duration of dobutamine infusion as well as requirement of atropine 4.
The mechanism of dobutamine induced vasospasm with or without β-agonists is complex. Dobutamine primarily stimulates cardiomyocyte sarcolemma β1-adrenergic receptors, but also has effect on β2- and α1-receptors. Increase in myocardial oxygen demand and coronary flow causes α-adrenergic mediated vasoconstriction that has been observed during exercise. In fact exercise-induced coronary spasm is a result of α1 receptor stimulation. Higher doses of dobutamine, as in dobutamine stress test, generate more α1-adrenergic effect that may induce coronary spasm, particularly in the presence of endothelial dysfunction 5. Moreover, dobutamine-induced coronary vasoconstriction is mediated through postjunctional α2-adrenergic receptors 6.
β-agonists cause cardiovascular side effects including angina, tachyarrhythmias, hypertension and myocardial injury by increasing myocardial oxygen consumption. Albuterol activates β2-adrenergic receptors particularly in coronary resistant vessels that are partially mediated by the endothelium at the microcirculatory level. Endothelial function plays important role in β2-agonist effect on vascular tone. Intracoronary infusion of salbutamol induces vasoconstriction in stenotic coronary arteries without increase in heart rate and blood pressure 7.
Albuterol pre-treatment with dobutamine stress test may induce coronary spasm in association with chest pain and ST-segment elevation. This clinical condition may lead to invasive procedures like cardiac catheterization and possible complications. Although the true incidence of coronary vasospasm with ST-segment elevation during dobutamine stress test with albuterol pre-treatment is not known, nuclear cardiologist must be aware of this potentially life threatening complication of this non-invasive diagnostic test. Coronary spasm should be considered in all patients with ST-segment elevation and chest pain during dobutamine stress test, particularly following β-agonist treatment. The safety of this combination must be re-examined. Thus, the patients should not be subjected to the dobutamine stress test if they are treated with β-agonist before the test 2.
Dobutamine dose
Applies to the following dobutamine strengths: 12.5 mg/mL; 1 mg/mL-dextrose5%; 2 mg/mL-dextrose5%; 4 mg/mL-dextrose5%; 500 mcg/mL-dextrose5%
Administration advice:
- Administer through a suitable IV catheter or needle.
- A calibrated electronic infusion device is recommended for controlling the rate of flow.
Storage requirements: Do not freeze.
Reconstitution/preparation techniques: The manufacturer product information should be consulted.
IV compatibility:
- Do not administer solutions containing dextrose through the same administration set as blood.
- Do not add supplementary medications to this drug; do not administer this drug simultaneously with strong alkaline solutions, solutions containing sodium bicarbonate, or other agents or diluents containing both sodium bisulfite and ethanol.
General: Dobutamine Injection USP is a clear, practically colorless, sterile, nonpyrogenic solution of Dobutamine hydrochloride for intravenous use only. Each milliliter contains 12.5 mg (41.5 µmol) Dobutamine, as the hydrochloride and sodium metabisulfite, 0.2 mg added as antioxidant. May contain hydrochloric acid and/or sodium hydroxide for pH adjustment. pH is 3.3 (2.5 to 5.5).
Dobutamine Hydrochloride USP is chemically designated (±)-4-[2-[[3-(ρ-hydroxyphenyl)-1-methylpropyl] amino]ethyl]-pyrocatechol hydrochloride.
Dobutamine may exhibit a pink color that, if present, will increase with time. This color change indicates slight oxidation but no significant loss of potency.
Monitoring:
- Cardiovascular: ECG and blood pressure should be monitored continuously; pulmonary wedge pressure and cardiac output should be monitored whenever possible.
- Metabolic: Consider monitoring serum potassium.
Usual Adult Dose for Congestive Heart Failure
- Initial dose: 0.5 to 1 mcg/kg/min IV infusion
- Maintenance dose: 2 to 20 mcg/kg/min IV infusion
- Maximum dose: 40 mcg/kg/min IV infusion
Initially 0.5 to 1 mcg/kg/minute as a continuous IV infusion, then titrated every few minutes. The usual dosage range is 2 to 20 mcg/kg/minute IV. Another manufacturer recommends a usual dosage range of 2.5 to 15 mcg/kg/minute IV. Titrate dosage based on hemodynamic response, including systemic blood pressure, urine flow, frequency of ectopic activity, heart rate, and (whenever possible) measurements of cardiac output, central venous pressure, and/or pulmonary capillary wedge pressure. Infusion rates higher than 20 mcg/kg/minute may produce tachycardia or ventricular ectopy. On rare occasions, infusion rates up to 40 mcg/kg/minute IV have been required to obtain the desired clinical response. Septic shock clinical practice guidelines recommend dobutamine in patients who show evidence of persistent hypoperfusion despite adequate fluid loading and the use of vasopressors. Titrate to an endpoint reflecting perfusion; reduce rate or discontinue if worsening hypotension or arrhythmias occur.
Comments:
- Rate of administration and duration of therapy should be based on blood pressure, heart rate, frequency of ectopic activity, and urine flow; cardiac output, central venous pressure, and pulmonary capillary wedge pressure should also be considered whenever possible.
- Concentrations up to 5000 mcg/mL have been administered to humans. Determine final volume based on fluid requirements of the patient.
- No controlled-trial experience exists beyond 48 hours of repeated boluses and/or continuous infusions.
Use:
- Inotropic support when parenteral therapy is needed in the short-term treatment of patients with cardiac decompensation due to depressed contractility resulting from organic heart disease or cardiac surgical procedures.
Usual Infants, Children, and Adolescents Dose for Congestive Heart Failure
- Initial dose: 0.5 to 1 mcg/kg/min IV infusion
- Maintenance dose: 2 to 20 mcg/kg/min IV infusion
- Maximum dose: 40 mcg/kg/min IV infusion
0.5 to 1 mcg/kg/minute as a continuous IV infusion, then titrated every few minutes to clinical response. The usual dosage range is 2 to 20 mcg/kg/minute IV. Infusion rates higher than 20 mcg/kg/minute may produce tachycardia or ventricular ectopy. On rare occasions, infusion rates up to 40 mcg/kg/minute IV have been required to obtain the desired clinical response. If IV access is not available during hypotensive states post-cardiopulmonary resuscitation, the same dobutamine dosage listed for IV use may be administered using the intraosseous route.
Neonates
0.5 to 1 mcg/kg/minute as a continuous IV infusion initially, then titrated every few minutes to clinical response. The usual dosage range is 2 to 20 mcg/kg/minute IV. Infusion rates higher than 20 mcg/kg/minute may produce tachycardia or ventricular ectopy. Because of variation in development, there is significant interpatient variability in response to dobutamine in neonates. Very preterm neonates are likely to have an attenuated reduction in systemic vascular resistance (SVR) compared to term neonates and, therefore, experience a more pronounced increase in blood pressure.
Comments:
- Certain container systems of this drug may be inappropriate for the dosage requirements of pediatric patients less than 30 kg.
- Rate of administration and duration of therapy should be based on systemic blood pressure, heart rate, frequency of ectopic activity urine flow; cardiac output, central venous pressure, and pulmonary capillary wedge pressure should also be considered whenever possible.
- Concentrations up to 5000 mcg/mL have been administered to humans. Determine final volume based on fluid requirements of the patient.
- No controlled-trial experience exists beyond 48 hours of repeated boluses and/or continuous infusions.
Use:
- Inotropic support when parenteral therapy is needed in the short-term treatment of patients with cardiac decompensation due to depressed contractility resulting from organic heart disease or cardiac surgical procedures.
Renal Dose Adjustments
Specific guidelines for dosage adjustments are not available; it appears that no dosage adjustments are needed. Titrate the dobutamine infusion rate to attain clinical goals.
Liver Dose Adjustments
Specific guidelines for dosage adjustments are not available; it appears that no dosage adjustments are needed. Titrate the dobutamine infusion rate to attain clinical goals.
Dialysis
It is unknown whether dobutamine is dialyzable. Titrate the dobutamine infusion rate to attain clinical goals.
Injectable Administration
Visually inspect parenteral products for particulate matter and discoloration prior to administration whenever solution and container permit.
Premixed bags of dobutamine in 5% Dextrose Injection solutions may exhibit a pink color that, if present, will increase with time. This color change is due to slight oxidation of the drug, but there is no significant loss of potency.
Intravenous Administration
Dilution
Concentrate for injection must be diluted with a compatible IV solution (e.g., 5% Dextrose Injection, 10% Dextrose Injection, 0.9% Sodium Chloride Injection, 5% Dextrose and 0.9% Sodium Chloride Injection, 5% Dextrose and 0.45% Sodium Chloride Injection, Lactated Ringer’s Injection) prior to administration.
Institute for Safe Medication Practices (ISMP)/Vermont Oxford Network (VON) Recommended Standard Concentration for Neonatal Infusions: 2,000 mcg/mL
Maximum concentration should not exceed 5,000 mcg/mL.
Intravenous Infusion Administration
Administer diluted solution by IV infusion using a controlled infusion device.
Infuse into a large vein whenever possible.
Use caution to avoid inadvertent bolus administration or inadvertent interruption of the infusion, particularly during line changes, when flushing the line, or during syringe/bag changes.
Do not administer dobutamine simultaneously with solutions containing sodium bicarbonate or strong alkaline solutions (incompatible). Solutions containing dextrose should not be administered through the same administration set as blood, as this may cause pseudoagglutination or hemolysis.
Initiate infusion at a low rate and titrate every few minutes to reach the optimal dosage based on patient response. Dosage titration is guided by the patient’s response, including systemic blood pressure, urine flow, frequency of ectopic activity, heart rate, and (whenever possible) measurements of cardiac output, central venous pressure, and/or pulmonary capillary wedge pressure.
Other Injectable Administration
Intraosseous infusion
NOTE: Dobutamine is not approved by the FDA for intraosseous administration.
During cardiopulmonary resuscitation, the same dosage may be given via the intraosseous route when IV access is not available.
Dobutamine side effects
Get emergency medical help if you have any of these signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Common side effects include:
- ectopic heartbeats,
- increased heart rate,
- elevations in BP (hypertension),
- hypotension (low blood pressure),
- phlebitis,
- local inflammatory changes,
- leg cramps,
- headache,
- fever,
- tingly feeling,
- nausea and vomiting.
The most common adverse reaction was heart rate increased by 30 beats per minute or more.
Tell your caregiver right away if you have:
- shortness of breath (even with mild exertion), swelling, rapid weight gain;
- chest pain, fast or pounding heartbeats;
- a light-headed feeling, like you might pass out;
- wheezing, chest tightness;
- dangerously high blood pressure-severe headache, blurred vision, buzzing in your ears, anxiety, confusion, uneven heartbeats, seizure; or
- signs of infection in your catheter–pain, swelling, warmth, redness, oozing, or skin changes where the medicine is injected.
Increased Heart Rate, Blood Pressure, and Ventricular Ectopic Activity − A 10 to 20 mm increase in systolic blood pressure and an increase in heart rate of 5 to 15 beats/minute have been noted in most patients. Approximately 5% of patients have had increased premature ventricular beats during infusions. These effects are dose related.
Hypotension − Precipitous decreases in blood pressure have occasionally been described in association with Dobutamine therapy. Decreasing the dose or discontinuing the infusion typically results in rapid return of blood pressure to baseline values. In rare cases, however, intervention may be required and reversibility may not be immediate.
Reactions at Sites of Intravenous Infusion − Phlebitis has occasionally been reported. Local inflammatory changes have been described following inadvertent infiltration. Isolated cases of cutaneous necrosis (destruction of skin tissue) have been reported.
Miscellaneous Uncommon Effects − The following adverse effects have been reported in 1% to 3% of patients: nausea, headache, anginal pain, nonspecific chest pain, palpitations, and shortness of breath. Isolated cases of thrombocytopenia have been reported.
Administration of Dobutamine hydrochloride, like other catecholamines, can produce a mild reduction in serum potassium concentration, rarely to hypokalemic levels.
Longer-Term Safety − Infusions of up to 72 hours have revealed no adverse effects other than those seen with shorter infusions.
Severe side effects
- ventricular tachycardia / Early / Incidence not known
- arrhythmia exacerbation / Early / Incidence not known
- pulmonary edema / Early / Incidence not known
- skin necrosis / Early / Incidence not known
- bronchospasm / Rapid / Incidence not known
- anaphylactoid reactions / Rapid / Incidence not known
Moderate side effects
- hypertension / Early / 7.5-7.5
- angina / Early / 1.0-3.0
- palpitations / Early / 1.0-3.0
- dyspnea / Early / 1.0-3.0
- thrombocytopenia / Delayed / 0-1.0
- sinus tachycardia / Rapid / Incidence not known
- premature ventricular contractions (PVCs) / Early / Incidence not known
- chest pain (unspecified) / Early / Incidence not known
- hypotension / Rapid / Incidence not known
- hypokalemia / Delayed / Incidence not known
- myoclonia / Delayed / Incidence not known
- phlebitis / Rapid / Incidence not known
- eosinophilia / Delayed / Incidence not known
Mild side effects
- headache / Early / 1.0-3.0
- nausea / Early / Incidence not known
- injection site reaction / Rapid / Incidence not known
- fever / Early / Incidence not known
- rash / Early / Incidence not known
Cardiovascular
- Very common (10% or more): Heart rate increased by 30 beats per minute (bpm) or more (10%)
- Common (1% to 10%): Systolic blood pressure increased by 50 mmHg or more, premature ventricular beats increased, anginal pain, palpitations, blood pressure decreased, ventricular dysrhythmia, dose-dependent ventricular extrasystoles, ventricular frequency increased in patients with atrial fibrillation, vasoconstriction in patients previously treated with beta blockers, supraventricular extrasystoles, ventricular tachycardia
- Uncommon (0.1% to 1%): Ventricular fibrillation
- Very rare (less than 0.01%): Bradycardia, myocardial ischemia, myocardial infarction, cardiac arrest, second degree atrioventricular block, coronary vasospasms, hypertensive/hypotensive blood pressure decompensation, intracavitary pressure gradients
- Frequency not reported: Systolic blood pressure increased by 10 to 20 mmHg, heart rate increased by 5 to 15 bpm, blood pressure decreased precipitously, pulmonary capillary pressure decreased, pectoral anginal discomfort, stress cardiomyopathy, eosinophilic myocarditis, fatal cardiac rupture
Dermatologic
- Common (1% to 10%): Exanthema, skin rash
- Very rare (less than 0.01%): Petechial bleeding
- Frequency not reported: Pruritus of the scalp
Local reactions
- Common (1% to 10%): Phlebitis, inflammation
- Very rare (less than 0.01%): Cutaneous necrosis
Hematologic
- Common (1% to 10%): Eosinophilia, thrombocyte aggregation inhibited when continuing infusion over a number of days
- Frequency not reported: Thrombocytopenia
Other
Common (1% to 10%): Nonspecific chest pain, fever
Frequency not reported: Feeling of heat and anxiety
Respiratory
Common (1% to 10%): Shortness of breath, bronchospasm
Nervous system
Common (1% to 10%): Headache
Frequency not reported: Paresthesia, tremor
Genitourinary
Common (1% to 10%): Urgency increased at high doses of infusion
Frequency not reported: Urinary urgency
Gastrointestinal
Common (1% to 10%): Nausea
Metabolic
Very rare (less than 0.01%): Hypokalemia
Frequency not reported: Serum potassium decreased
Immunologic
Frequency not reported: Hypersensitivity
Musculoskeletal
Frequency not reported: Myoclonic spasm
Psychiatric
Frequency not reported: Restlessness, anxiety
Dobutamine Overdose
Overdoses of dobutamine have been reported rarely. The following is provided to serve as a guide if such an overdose is encountered.
Signs and Symptoms– Toxicity from dobutamine hydrochloride is usually due to excessive cardiac β receptor stimulation. The duration of action of dobutamine hydrochloride is generally short (T1/2 = 2 minutes) because it is repidly metabolized by catechol-0-methyltransferase. The symptoms of toxicity may include anorexia, nausea, vomiting, tremor, anxiety, palpitations, headache, shortness of breath, and anginal and nonspecific chest pain. The positive inotropic and chronotropic effects of dobutamine on the myocardium may cause hypertension, tachyarrhythmias, myocardial ischemia, and ventricular fibrillation.
Hypotension may result from vasodilation.
Treatment
To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center. Telephone numbers of certified poison control centers are listed in the Physicians’ Desk Reference. In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in your patient.
The initial actions to be taken in a dobutamine hydrochloride overdose are discontinuing administration, establishing and airway, and ensuring oxygenation and ventilation. Resuscitative measures should be initiated promptly. Severe ventricular tachyarrhythmias may be successfully treated with propranolol or lidocaine. Hypertension usually responds to a reduction in dose or discontinuation of therapy.
Protect the patient’s airway and support ventilation and perfusion. If needed, meticulously monitor and maintain, within acceptable limits, the patient’s vital signs, blood gases, serum electrolytes, etc. If the product is infested, unpredictable absorption may occur from the mouth and the gastrointestinal tract. Absorption of drugs from the gastrointestinal tract may be decreased by giving activated charcoal, which, in many cases, is more effective than emesis of labage; consider charcoal instead of or in addition to gastric emptying. Repeated doses of charcoal over time may hasten eliminiation of some drugs that have been absorbed. Safeguard the patient’s airway when employing gastirc emptying or charcoal.
Forced diuresis, peritoneal dialysis, hemodialysis, or charcoal hemoperfusion have not been established as beneficial for an overdose of dobutamine hydrochloride.
References- Two-dimensional speckle tracking for the assessment of coronary artery disease during dobutamine stress echo: clinical tool or merely research method. Cardiovasc Ultrasound. 2015; 13: 43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4619392/
- Ozcan C, Zaret BL. Dobutamine stress test and beta-agonist – a potential concern for nuclear cardiology testing: a case report. Cases Journal. 2009;2:7466. doi:10.4076/1757-1626-2-7466. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740317/
- Lubitz SA, Duvall WL, Kim MC, Henzlova MJ. Dobutamin-induced myocardial infarction with normal coronary arteries during stress SPECT myocardial perfusion imaging. J Nucl Cardiol. 2007;14:613–616. doi: 10.1016/j.nuclcard.2007.05.004
- Desai MY, De la Pena-Almaguer E, Mannting F. Can pre-treatment with B-agonists reduce stress test time and the use of atropine in dobutamine stress testing. Cardiology. 2001;95:156–160. doi: 10.1159/000047363
- Kawano H, Fujii H, Motoyama T, Kugiyama K, Ogawa H, Yasue H. Myocardial ischemia due to coronary artery spasm during dobutamin stress echocardiography. Am J Cardiol. 2000;85:26–30. doi: 10.1016/S0002-9149(99)00600-1
- Dai XZ, Chen DG, Bache RJ. Alpha-adrenergic effects of dopamine and dobutamine on the coronary circulation. J Cardiovasc Pharmacol. 1989;14:82–87. doi: 10.1097/00005344-198907000-00015
- Barbato E, Piscione F, Bartunek J, Galasso G, Cirillo P, De Luca G, Iaccarino G, De Bruyne B, Chiariello M, Wijns W. Role of B2 adrenergic receptors in human atherosclerotic coronary arteries. Circulation. 2005;111:288–294. doi: 10.1161/01.CIR.0000153270.25541.72