What is enophthalmos
Enophthalmos is the sinking of the eyeball towards the back part of the eye socket. Enophthalmos becomes clinically obvious if the anterior globe projection is less than 12 mm or differs from the opposite side by 3 mm or more as measured by a Hertel exophthalmometer. The anterior projection of the eye is most commonly measured relative to the outer edge of the orbit, the orbital rim, but may also be assessed relative to the frontal and maxillary prominences, or the contralateral eye.
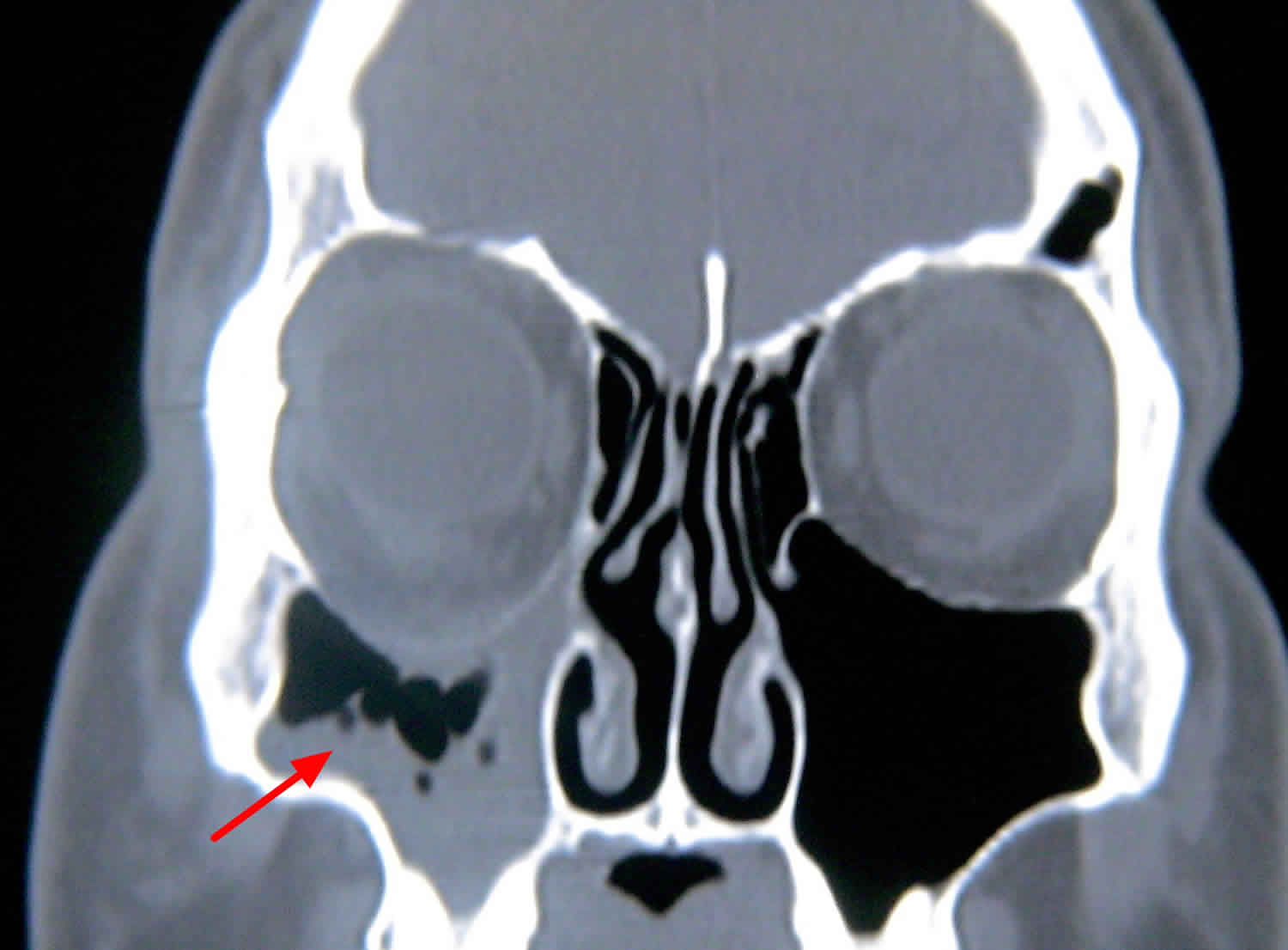
Primary enophthalmos indicates a congenital or developmental cause. Some degree of facial asymmetry is common, but congenital relative enophthalmos or ocular retrusion may occur with in utero maldevelopment (eg, plagiocephaly, microphthalmos). Secondary enophthalmos is due to an acquired change in volumetric relationship between the rigid bone cavity, the orbit, and its contents (predominantly the orbital fat, the extraocular muscles, and the eye). Expansion of the orbital cavity without change in the volume of orbital contents (ie, a blow-out fracture) leads to enophthalmos 1. Acute posttraumatic enophthalmos, in absence of direct injuries of the globe is generally due to blowout fractures with herniation of the orbital soft tissues in the adjacent paranasal sinuses. It can be associated with visual deficits, diplopia, eye movement defects, hemosinus, and locoregional sensibility defect. In patients with radiologic evidence of orbital soft tissue herniation in the paranasal sinuses or increases in significant orbital volume, enophthalmos can be clinically recognized immediately or several days after periorbital swelling and/or emphysema reduction 2. In the absence of these radiological findings, enophthalmos is rare and may be attributed to volumetric orbital content reduction induced by ischemic liponecrosis or posttraumatic fibrotic scarring of orbital soft tissues 3. An example of a blow-out fracture is shown in the image below. The arrow points to the downward displacement of the orbital floor bone into the blood-filled maxillary sinus.
Spontaneous enlargement of the orbit may also occur in silent sinus syndrome, as depicted in the figure 2 below, where a negative pressure develops within the maxillary sinus, thinning the orbital floor and drawing it downward. Silent sinus syndrome is a rare disease characterized by spontaneous enophthalmos and hypoglobus (an abnormal lowering of the globe usually due to a deficient anterior orbital floor) secondary to collapse of the orbital floor in patients with asymptomatic maxillary sinusitis. Radiographic findings include ipsilateral maxillary sinus opacification, lateralization of the uncinate and middle turbinate, and infundibular occlusion. The maxillary sinus is filled with mucoid material, not blood, in silent sinus syndrome (Figure 3).
Alternatively, scarring contracture of the orbital fat and extraocular muscles may decrease soft tissue volume, making the orbital cavity less full and causing enophthalmos. Several disorders may cause this, including metastatic sclerosing or scirrhous breast carcinoma.
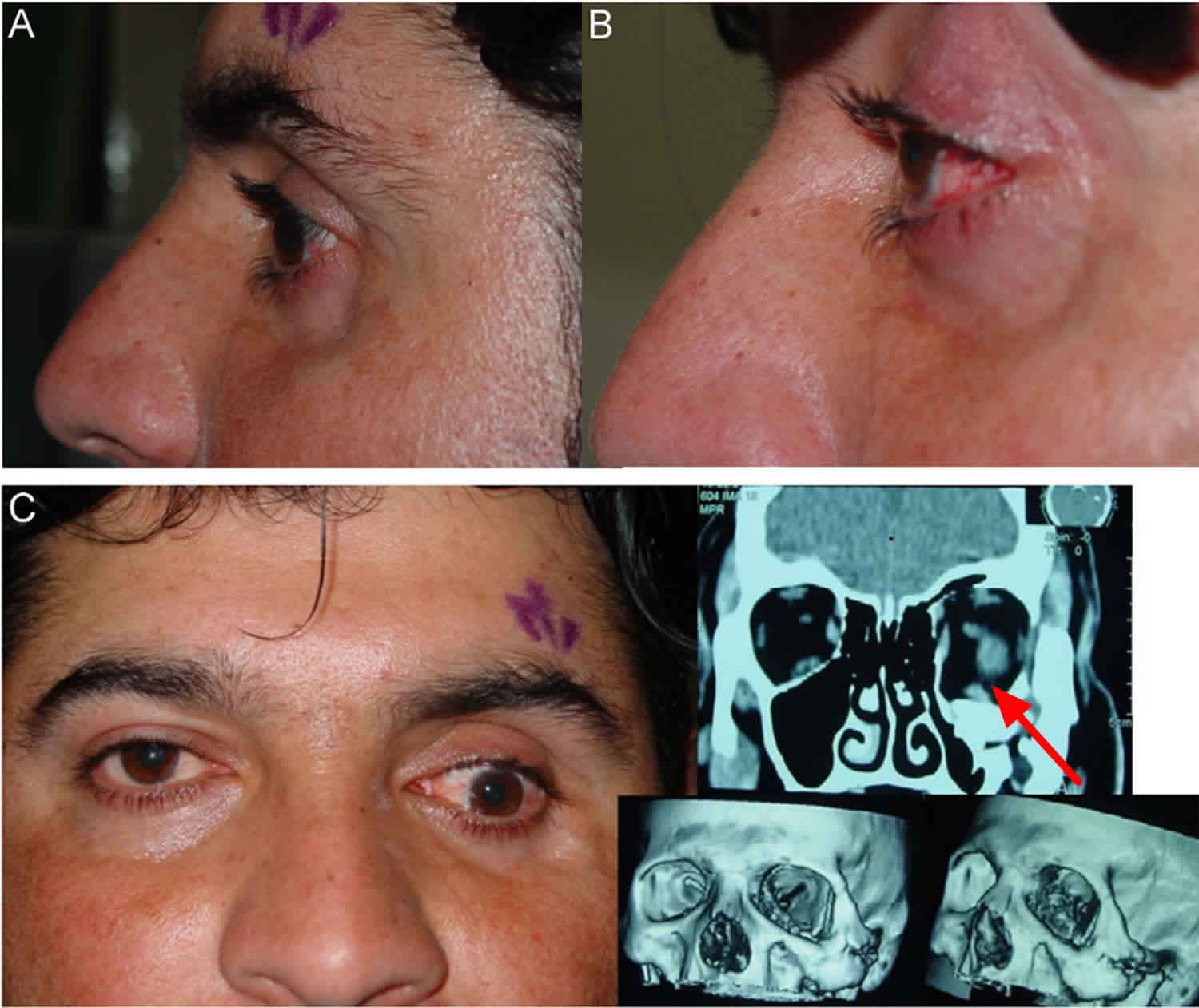
Figure 1. Enophthalmos due to blow-out fracture
Footnote:A 30-year-old Iraqi male with a history of blast injury to the face reported a left sunken eye. (A) Side picture preoperative assessment. Patient has significant enophthalmos in the left eye. (B) Postoperative picture. Patient has improvement in enophthalmos. (C) Patient’s preoperative CT scan showing severe medial, inferior, and lateral orbital wall fractures.
Figure 2. Enophthalmos due to silent sinus syndrome
Figure 3. Silent sinus syndrome CT scan
Enophthalmos causes
Causes of secondary enophthalmos include the following:
- Postnatal, inadequate, orbital cavity development
- Bone growth arrest (eg, ionizing radiation for retinoblastoma)
- Inadequate local tissue stimulation of orbital bone growth
- Intraorbital (eg, phthisis bulbi, anophthalmos, fat atrophy in childhood)
- Extraorbital (eg, maxillary bone growth problems)
- Orbital cavity expansion
- Outward fracture of orbital bones: In order of frequency, fracture sites are as follows: floor, medial wall, lateral wall, and roof.
- Surgical expansion of the orbit (as in orbital decompression or expansion for thyroid orbitopathy)
- Silent sinus syndrome (ie, spontaneous, asymptomatic collapse of the maxillary sinus and orbital floor associated with negative sinus pressures)
- Orbital varix with presumed slow bone erosion when the varix fills during recumbent position
- Volumetric loss of orbital contents
- Orbital fat atrophy
- Following concussive trauma
- Following severe inflammation or infection
- Following external beam irradiation
- Associated with wasting disorders (eg, Parry-Romberg hemifacial atrophy, linear scleroderma)
- Contraction of orbital fat – Scirrhous carcinomas (most commonly metastatic breast, but pulmonary, prostate, and gastrointestinal cancers may cause fat and globe retraction as well) 4
- Following surgery (as in resection of a mass lesion associated with local fat atrophy)
- Phthisis bulbi or prephthisis bulbi
- Orbital fat atrophy
- Pseudoenophthalmos
- Unilateral blepharoptosis
- Horner syndrome
- Contralateral exophthalmos
- Contralateral pseudoexophthalmos
- Contralateral high myopia
- Contralateral buphthalmos or megaloglobus
- Contralateral eyelid retraction
Enophthalmos symptoms
Enophthalmos may be sudden and static, non-changing (as may occur with trauma) or progressive. Sudden appreciation of enophthalmos does not necessarily imply sudden development. Depending on the cause, enophthalmos may progress over any time frame, ranging from minutes to years. Most causes of enophthalmos are progressive, including trauma and congenital deformities, because inflammation and swelling immediately after trauma may prevent achievement of the total final degree of enophthalmos, and congenital enophthalmos may progress as certain parts of the face continue to develop while others do not.
Mild degrees of bilateral enophthalmos may be difficult to determine without radiographic studies or old photographs for comparison, but unilateral enophthalmos is often obvious when comparing one eye with the other. Specific changes include the following:
- Narrowed vertical eyelid fissure (vertical fissure may be widened or normal if associated with downward displacement of the eye, also known as hypoglobus or globe ptosis)
- Superior sulcus deformity (deepened upper eyelid crease)
- Lost fullness of fat bulge in upper and lower eyelids
- Can be associated with hypoglobus (downward displaced eye), usually without significant associated diplopia (double vision) [2]
- Other physical findings, depending on cause:
- Skin and eyelids
- Thinned skin, muscle, fat, or even bone in a linear array may suggest Parry-Romberg syndrome or linear scleroderma.
- Thickened indurated skin may suggest metastatic scirrhous carcinoma.
- Blue, boggy skin might indicate associated vascular malformation with varix.
- Fifth nerve function
- Decreased function of second division may suggest nerve entrapment in fracture.
- Decreased function of either of the first 2 divisions may suggest tumor infiltration or cavernous sinus involvement.
- Exophthalmometry measurement: This is important to establish progression or stability.
- Ocular motility: Dysmotility might suggest a mass (orbital tumor) or restrictive process (fracture).
- Skin and eyelids
Enophthalmos complications
Long-standing enophthalmos, especially associated with very extensive orbital trauma, may be associated with severe orbital scarring, and correction can be very difficult or impossible.
Complications of enophthalmos are mostly aesthetic, but certain problems may be associated with a posterior position of the eye, including the following:
- Upper eyelid ptosis and lower eyelid reverse ptosis
- Upper eyelid retraction if the enophthalmos is due to cicatricial problems or associated with hypoglobus, downward displacement of the eye
- Ocular dysmotility and diplopia due to abnormal vectors induced upon the oblique muscles
- Upper eyelid “standoff” from the globe with inadequate blink-induced lubrication if the eye lies posterior to the Whitnall ligament
- Ocular surface irritation and drying due to air spaces at the lateral and medial canthi, where the eyelids remain attached to the orbital rim, but the globe is much more posterior.
- Diminished visual field due to the relative prominent projection of the brow, lateral orbital rim, cheek, and nose
- Enlarged tear lakes with inadequate tear mobilization down the lacrimal system and resulting vision blur and epiphora
Other complications may be associated with the development of enophthalmos, but not caused by the enophthalmos. Examples might include other facial trauma or systemic malignancy.
Enophthalmos diagnosis
Neuroimaging is the most essential laboratory study in patients with enophthalmos. Other tests are determined by the specific suspected disease process. For example, in the case of suspected contralateral orbital tumor, systemic evaluation for a primary malignancy and metastatic disease should be performed. Open biopsy may be indicated. Needle biopsy is rarely helpful in the diagnosis of enophthalmos.
The degree of enophthalmos is often appreciated and measured using an exophthalmometer, of which several varieties are available. However, exophthalmometer measurements are highly position– and applied pressure–dependent, and the reliability of measurements, especially as performed by different examiners, may be low.
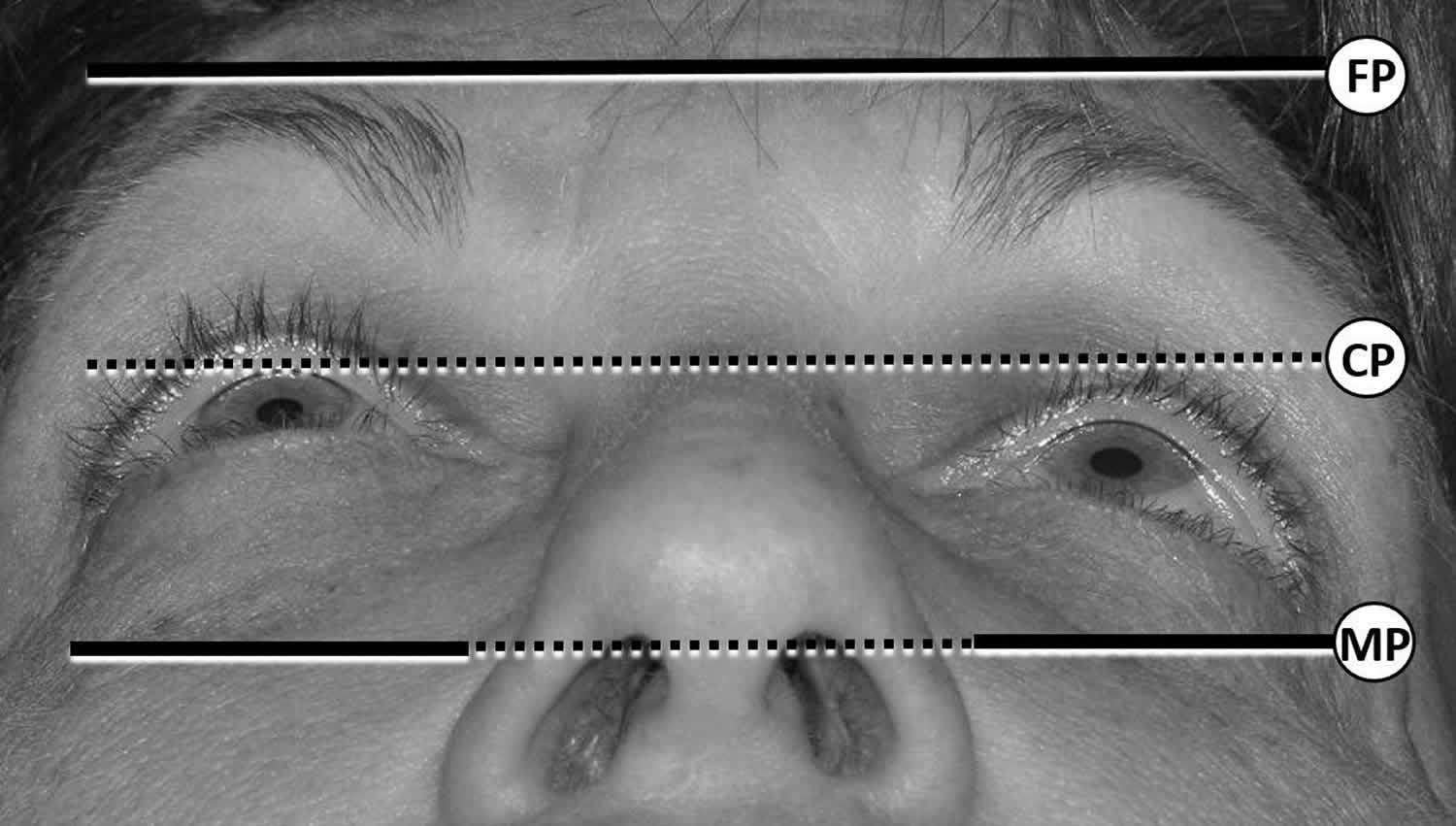
“Worms’ eye” photographs, such as that shown in the image below, can be very helpful in documenting and monitoring enophthalmos. The photographs are taken at a standardized angle of head tilt, for example placing the tragus of the ear and the projection of the chin in a line parallel to the floor. An assessment of the anterior corneal projection, marked “CP” below, may be compared to the frontal process projection “FP” and the maxillary process projection “MP.” In this photograph, the left eye is enophthalmic. If the lateral orbital rim is posteriorly displaced or the maxilla is hypoplastic or in-fractured, the more common exophthalmometers will provide inaccurate measurements. The degree of enophthalmos is usually measured in millimeters relative to the contralateral eye and documented as millimeters of relative enophthalmos.
Figure 4. Worms’ eye photographs (Worms’ eye view showing left enophthalmos)
Imaging Studies
The following imaging studies might be considered:
- CT scan of the orbits:
- This is often the best first imaging study.
- Coronal images are best to evaluate blow-out fractures and changes associated with the maxillary sinus.
- Axial images best demonstrate orbital fat atrophy.
- Rapid spin or spiral technology is useful for demonstrating varix during a Valsalva maneuver.
- MRI with fat suppression, surface coils, and contrast enhancement is best for characterizing neoplastic infiltrations.
- Bone scans are infrequently helpful to identify areas of bone inflammation seen with osteomyelitis or inflammatory wasting disorders.
- Plain films may provide gross assessment relative orbit sizes but do not provide adequate information about soft-tissue volume.
- Old photographs can help to determine the rate of progression of the problem or an unrecognized congenital facial asymmetry.
Enophthalmos treatment
Medical treatments in patients with enophthalmos are directed at specific diseases and may include chemotherapy or ionizing radiation for metastatic disease or immunosuppressive treatments for inflammatory disorders. Once the disease process is stabilized, nonsurgical management may include camouflage glasses (hyperopic [magnifying] correction over myopic contact lens).
Enophthalmos surgery
Once medical or surgical treatment of the underlying process is achieved, correction of enophthalmos begins with approximating normal orbital bone positions before addressing soft tissue volume loss 5.
Orbital fracture repair includes the following 6:
- Maintain the convexity of the posterior, medial orbital floor 7.
- Stabilize floor implants posteriorly on intact floor ledge.
- Release any major adhesions or scar bands to allow mobilization of soft tissues. In late posttraumatic cases, sharp rather than blunt dissection is often required 8.
- If using bone grafts rather than synthetic materials, allow for 15-30% resorption.
- Overcorrect to obtain 1-2 mm of exophthalmos intraoperatively.
- Perform forced duction testing of the globe prior to closure.
In replacing lost orbital soft tissue volume, perform the following:
- A forward traction test on the globe to determine the amount of correction possible
- Augment from the orbital walls inward with bone or synthetic materials. For pure enophthalmos correction without hypoglobus, inferolateral and retrobulbar mass effect is desirable.
- He Y, Zhang Y, An JG. Correlation of types of orbital fracture and occurrence of enophthalmos. J Craniofac Surg. 2012 Jul. 23(4):1050-3.[↩]
- Hamedani M, Pournaras J A, Goldblum D. Diagnosis and management of enophthalmos. Surv Ophthalmol. 2007;52(5):457–473[↩]
- Gagnon M R, Yeatts R P, Williams Z, Matthews B. Delayed enophthalmos following a minimally displaced orbital floor fracture. Ophthal Plast Reconstr Surg. 2004;20(3):241–243.[↩]
- [Guideline] Children’s Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. Sections 38-91: radiation. Bethesda (MD): Children’s Oncology Group; 2006 Mar.[↩]
- Kang SJ, Kim JW. Surgical treatment of enophthalmos using an endoscope and T-shaped porous polyethylene fabricated with a mirror image. Int J Oral Maxillofac Surg. 2012 Oct. 41(10):1186-91.[↩]
- Cole P, Kaufman Y, Hollier L. Principles of facial trauma: orbital fracture management. J Craniofac Surg. 2009 Jan. 20(1):101-4.[↩]
- Kim HS, Kim SE, Evans GR, Park SH. The usability of the upper eyelid crease approach for correction of medial orbital wall blowout fracture. Plast Reconstr Surg. 2012 Oct. 130(4):898-905.[↩]
- Hazani R, Yaremchuk MJ. Correction of posttraumatic enophthalmos. Arch Plast Surg. 2012 Jan. 39(1):11-7.[↩]