What is epidermodysplasia verruciformis
Epidermodysplasia verruciformis is a very rare, autosomal recessive inherited skin disorder characterized by chronic infection with human papillomavirus (HPV) leading to polymorphous cutaneous lesions and high risk of developing non melanoma skin cancer. This genodermatosis manifests mainly as verrucous cutaneous lesions such as multiple persistent verrucae, pityriasis versicolor-like lesions, and other verrucous or “warty” cutaneous lesions as well as the development of Bowen disease and squamous cell carcinoma 1.
The most commonly identified human papillomavirus (HPV) types found in epidermolysis verruciformis related cancers are HPV5 and HPV8. These 2 types have been found to be present in up to 90% of epidermolysis verruciformis-related skin cancers 2. Other types of HPV that are alternatively commonly found include 9, 12, 14, 15, 17, 19, 20, 21, 22, 23, 24, 25, 36, 38, 47, and 50 3. One study showed that HPV5 was the most common single type isolated, and contrary to other literature results, HPV3, HPV14, and HPV20 were more commonly isolated than HPV8 4. This autosomal recessive condition in its primary (in other words, inherited) form is caused by a mutation of TMC6/EVER1 or TMC8/EVER2, which is believed to impart a defect in the ability to mount an immune response to certain HPV types within keratinocytes 5. Interestingly, these patients with typical epidermolysis verruciformis do not generally display reduced immune capabilities against other infectious pathogens. The beta-HPV types identified in patients with epidermolysis verruciformis who develop skin malignancies are found throughout the general population, and in persons without the EVER mutations or epidermolysis verruciformis, these HPV types have not been shown to produce dysplasia or malignancy otherwise 6.
Malignant transformation of cutaneous epidermal lesions in epidermolysis verruciformis is usually observed in association with HPV5, HPV8, HPV17, HPV20, and HPV47. These lesions usually develop in patients in their 30s, decades after the initial presentation 7.
There are broadly 2 forms of epidermolysis verruciformis, the classic form being the inherited or primary type, inherited in an autosomal recessive pattern, while a separate acquired or secondary type is a clinically almost indistinguishable condition that is observed mainly in HIV-infected, immunocompromised, or immunosuppressed individuals 8.
In patients with the acquired or secondary type of epidermolysis verruciformis, also known as an atypical form, there is usually a history of some form of immunodeficiency, often treatment related. This occurrence of epidermolysis verruciformis in relation to immunodeficiency (other than as occurs in the inherited type) is thought to be specifically due to T-cell mediated immunodeficiency in patients with pre-disposing genetic mutations such as in RHOH and STK4, among others. Not all patients with these mutations who are immunosuppressed will develop epidermolysis verruciformis-like disease. This is much different than typical epidermolysis verruciformis, wherein characteristic mutations are inherited display full penetrance 9. Interestingly, a case has been reported of a patient who developed epidermolysis verruciformis lesions in an acquired fashion due to trauma from Brazilian hot wax hair removal of the pubic region. The patient had a history of renal transplant 5 years earlier and a pancreatic transplant 3 years earlier. The area was denuded from the hot wax treatment, and as it healed, a brownish red cutaneous plaque developed that when biopsied was diagnosed as an epidermolysis verruciformis lesion. The patient denied family or personal history of epidermolysis verruciformis lesions. The lesion was successfully treated with topical 0.1% tretinoin and showed better resolution of lesion and less post-inflammatory increased pigmentation as compared with cryotherapy of another portion of the lesion treated concurrently 10.
Epidermodysplasia verruciformis is a very rare condition. A review of literature performed by Imahorn et al. in 2017 found about 500 patients with epidermodysplasia verruciformis reported in the literature worldwide 11. Patients with typical epidermolysis verruciformis develop epidermolysis verruciformis lesions early in childhood and continue to develop new lesions throughout life 12. These cutaneous lesions persistently infected with beta-HPV may progress to non-melanoma skin cancer, and between 30% to 70% of patients with epidermolysis verruciformis will develop squamous cell carcinoma within their lifetime 13. No bias for gender or specific geographical distribution has been identified 14.
Epidermodysplasia verruciformis usually manifests during infancy (7.5% of cases), childhood (61.5% of cases) or puberty (22% of cases) with a progressive development of hyperpigmented or hypopigmented flat wart-like papules, irregular reddish brown plaques, seborrheic keratosis-like lesions and pityriasis versicolor-like macules on the trunk, neck, face, dorsal hands and feet (sun-exposed skin). Various HPV subtypes (HPV5 and HPV8 are found in 80% of cases) can be detected in the cutaneous lesions. Thirty to 60% of patients develop non-melanoma skin cancers, especially squamous cell carcinomas (SCC), during the fourth or fifth decades of life, mainly on sun-exposed areas. Black-skinned patients have a much lower incidence of skin cancer. Most squamous cell carcinomas remain local; metastases are uncommon.
Although permanent cure of epidermolysis verruciformis cannot be achieved by any therapy at present, described treatment modalities include cryotherapy, topical imiquimod and 5-fluorouracil, systemic retinoids, interferon alpha, and 5-aminolevulinic acid photodynamic therapy. Surgical excision is the treatment of choice for squamous cell carcinoma (SCC). Preventive measures, in particular sun exposure avoidance and photoprotection, are crucial for proper management.
Epidermodysplasia verruciformis causes
Epidermodysplasia verruciformis is caused by a reduced ability by the immune system to fend off and eradicate human papillomavirus (HPV) infection 1.
Epidermolysis verruciformis can be caused by loss-of-function mutations in either of the 2 adjacent genes epidermolysis verruciformisER1/TMC6 or epidermolysis verruciformisER2/TMC8 (17q25.3) coding for membrane proteins that form a complex with the Zinc transporter protein ZnT-1 in the endoplasmic reticulum (ER) membrane of keratinocytes. The mutations in these genes lead to susceptibility to infection with specific HPV subtypes belonging to the beta genus, including HPV5, 8, 9, 12, 14, 15, 17, 19-25, 36-38, 47 and 49, which are ubiquitous and harmless to healthy individuals.
Each epidermodysplasia verruciformis patch is caused by an infection with a subtype of human papillomavirus (HPV).
HPV has numerous subtypes, which cause a wide range of viral warts. Some subtypes of HPV have minimal or no clinical effect in most people yet the same subtypes result in the clinical features of epidermodysplasia verruciformis in people with an impaired immune response to the virus. More than 30 subtypes of HPV have been implicated.
Epidermolysis verruciformis inheritance pattern
In most epidermodysplasia verruciformis cases, transmission is autosomal recessive but sex-linked and autosomal dominant inheritance patterns have also been reported.
Epidermodysplasia verruciformis autosomal recessive inherited disorder means that the individual has gained an abnormal epidermolysis verruciformis gene from each parent. The parents of about 10% of patients with epidermodysplasia verruciformis are blood relatives (ie, the parents share a common ancestor). In a few cases, sex-linked and autosomal dominant inheritance patterns have also been reported.
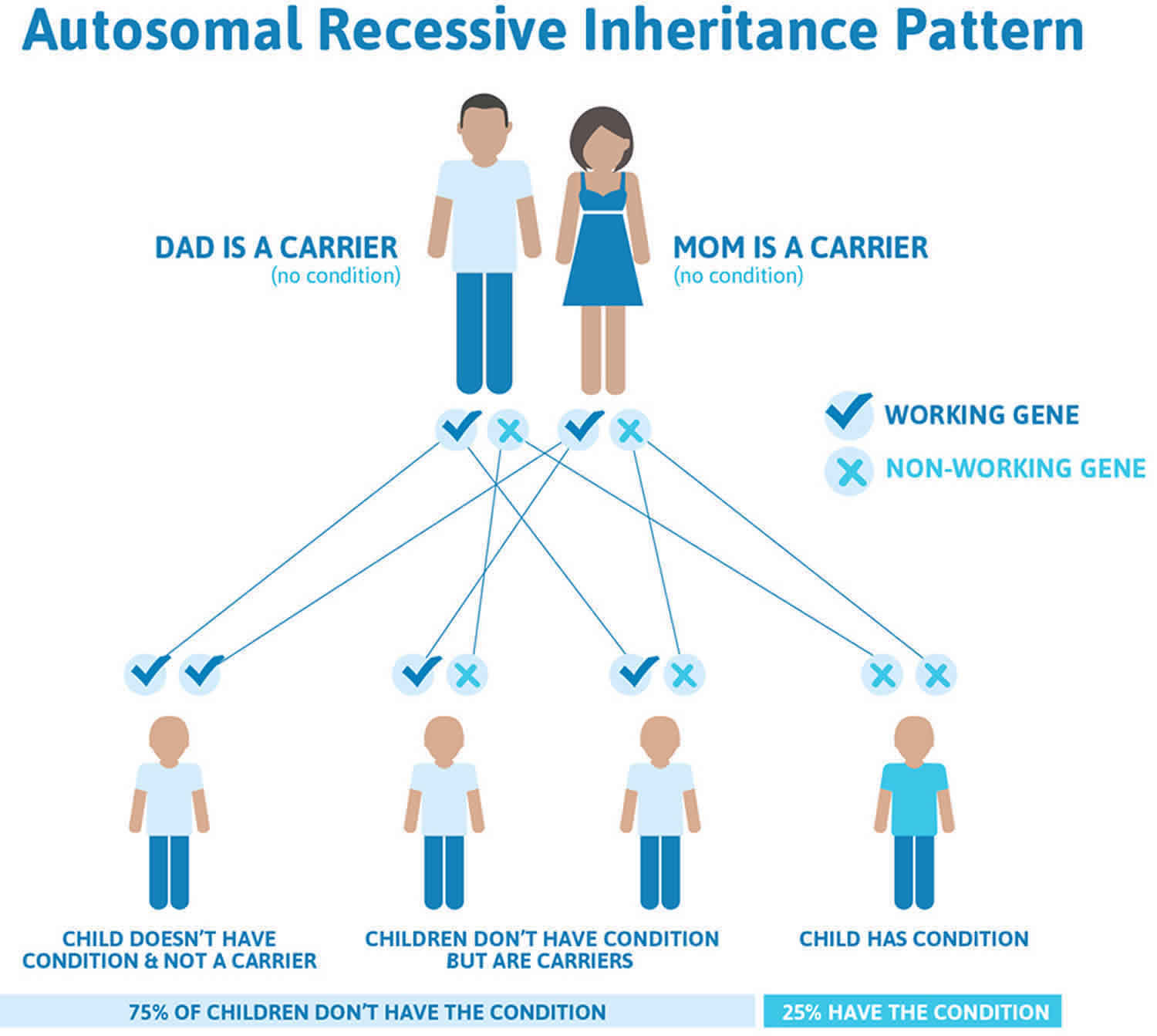
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
Epidermodysplasia verruciformis is often due to mutations in the epidermolysis verruciformis ER1 or epidermolysis verruciformis ER2 genes on chromosome 17q25. The mutation decreases cell capacity to fight HPV infections. In cases that lack this mutation, mutations in RAS homolog gene family member H (RHOH), MST1 deficiency, and splicing deficiency in the gene encoding LCK (lymphocyte specific kinase) have been found.
The lesions usually start to appear during childhood and persist. About 7.5% of cases appear in infancy, 61.5% in children aged 5–11 years and 22.5% in puberty. The disease affects both males and females and people of all races.
Acquired epidermodysplasia verruciformis is a result of HIV infection, organ transplantation or a lymphoma.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 1. Epidermolysis verruciformis autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Epidermodysplasia verruciformis symptoms
Patients with both inherited and acquired epidermolysis verruciformis present with identical lesions, characterized by verruca plana-like sometimes scaly, often flat, lesions and papules usually on the trunk, neck or face, or appearing similar to pityriasis versicolor lesions. These lesions appear in multiple places, and in the case of inherited epidermolysis verruciformis, may begin to appear as early as infancy and continue throughout the patient’s life. They will usually appear on skin areas exposed to ultraviolet (UV) light. A family history of epidermolysis verruciformis would be quite helpful in the diagnosis. For acquired epidermolysis verruciformis, history of HIV or immunosuppression medical therapy would be vital to diagnosis 6.
Two clinical presentations have been described in epidermodysplasia verruciformis.
- White, pink, reddish brown, dark brown or violet flat-topped papules and plaques with a scaly surface and irregular borders.
- Verrucous or seborrheic keratoses-like lesions. These are raised brown warty lesions.
Warts occur in irregular clusters of a few to over a hundred lesions. They are especially prevalent in sun-exposed areas such as the hands, feet, face, and earlobes. Plaque-like lesions usually appear on the trunk, neck, arms and legs. The palms, soles, armpits and external genitals may also be involved.
Epidermolysis verruciformis complications
A major concern for patients with epidermodysplasia verruciformis is that in 30-60% of epidermolysis verruciformis patients the lesions may transform into skin cancers; these are mostly cutaneous squamous cell carcinoma and intraepidermal squamous cell carcinoma. Basal cell carcinoma and adnexal tumours are less common. Malignant tumours are usually found in patients 30–50 years of age.
Over 90% of epidermolysis verruciformis-associated skin cancers contain HPV types 5, 8, 10, and 47. epidermolysis verruciformis lesions caused by HPV 14, 20, 21, and 25 usually remain benign. Exposure to sunlight or ultraviolet radiation increases the chance that a benign wart will develop into skin cancer.
Epidermodysplasia verruciformis diagnosis
Epidermolysis verruciformis diagnosis is based on clinical and histological findings. Epidermodysplasia verruciformis is suspected when there are a large number of treatment-resistant viral warts. Skin biopsy shows verruca plana-like lesions with mild hyperkeratosis, hypergranulosis and acanthosis of the epidermis. Keratinocytes of the upper epidermal layers are enlarged with perinuclear vacuolization and a typical blue-gray pallor. HPVs can be detected in keratinocytes using in situ hybridization or immunohistochemistry with anti-HPV antibodies. Some laboratories can report the subtype of HPV by polymerase chain reaction (PCR).
Epidermodysplasia verruciformis treatment
Epidermodysplasia verruciformis is a lifelong disease. There is no definitively effective treatment for epidermolysis verruciformis exists. Even though lesions can be treated or removed as they appear, the lesions develop throughout life.
Currently there is no treatment to prevent new lesions from occurring. The management of epidermolysis verruciformis involves a combination of medical and surgical treatments alongside patient counseling, education and regular surveillance (especially if immunocompromised).
- Stress the importance of following sun protection strategies especially if living at high altitude and/or working outdoors. Exposure to sunlight (UVB and UVA) has been shown to increase the rate of epidermolysis verruciformis lesions turning into skin cancers.
- Encourage smoking cessation.
- Treat and remove the lesions in the same way as other viral warts, using a chemical treatment, cryotherapy, electrosurgery or laser ablation.
- Oral and topical retinoids (isotretinoin and acitretin), fluorouracil and imiquimod may be helpful.
- Experimental therapies for epidermodysplasia verruciformis and skin tumours include intralesional interferon, a combination of isotretinoin and interferon alpha or cholecalciferol (vitamin D) analogues.
- Surgical excision and reconstruction are used for invasive skin cancers.
Patients with epidermolysis verruciformis will require annual or more frequent check-ups with dermatologists to evaluate for development of new worrisome lesions 15. Although radiation therapy is used often in non-epidermolysis verruciformis patients with conjunctival squamous cell carcinoma, it is contraindicated in patients with epidermolysis verruciformis as this has been observed to cause the development of more invasive and serious lesions 16. In non-conjunctival cases of squamous cell carcinoma which have metastasized, radiation therapy may be a consideration as an adjunct to other treatments 17.
Epidermolysis verruciformis prognosis
Epidermolysis verruciformis prognosis is favorable since skin tumors appear progressively and metastases are uncommon.
- Myers DJ, Fillman EP. Epidermodysplasia Verruciformis. [Updated 2019 Jan 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534198[↩][↩]
- Patel T, Morrison LK, Rady P, Tyring S. Epidermodysplasia verruciformis and susceptibility to HPV. Dis. Markers. 2010;29(3-4):199-206.[↩]
- Gewirtzman A, Bartlett B, Tyring S. Epidermodysplasia verruciformis and human papilloma virus. Curr. Opin. Infect. Dis. 2008 Apr;21(2):141-6.[↩]
- Imahorn E, Yüksel Z, Spoerri I, Gürel G, Imhof C, Saraçoğlu ZN, Koku Aksu AE, Rady PL, Tyring SK, Kempf W, Itin PH, Burger B. Novel TMC8 splice site mutation in epidermodysplasia verruciformis and review of HPV infections in patients with the disease. J Eur Acad Dermatol Venereol. 2017 Oct;31(10):1722-1726[↩]
- Ramoz N, Rueda LA, Bouadjar B, Montoya LS, Orth G, Favre M. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat. Genet. 2002 Dec;32(4):579-81.[↩]
- de Jong SJ, Imahorn E, Itin P, Uitto J, Orth G, Jouanguy E, Casanova JL, Burger B. Epidermodysplasia Verruciformis: Inborn Errors of Immunity to Human Beta-Papillomaviruses. Front Microbiol. 2018;9:1222.[↩][↩]
- Nindl I, Gottschling M, Stockfleth E. Human papillomaviruses and non-melanoma skin cancer: basic virology and clinical manifestations. Dis. Markers. 2007;23(4):247-59.[↩]
- Gül U, Kiliç A, Gönül M, Cakmak SK, Bayis SS. Clinical aspects of epidermodysplasia verruciformis and review of the literature. Int. J. Dermatol. 2007 Oct;46(10):1069-72.[↩]
- Crequer A, Troeger A, Patin E, Ma CS, Picard C, Pedergnana V, Fieschi C, Lim A, Abhyankar A, Gineau L, Mueller-Fleckenstein I, Schmidt M, Taieb A, Krueger J, Abel L, Tangye SG, Orth G, Williams DA, Casanova JL, Jouanguy E. Human RHOH deficiency causes T cell defects and susceptibility to EV-HPV infections. J. Clin. Invest. 2012 Sep;122(9):3239-47.[↩]
- Kirchhof MG, Au S. Brazilian waxing and human papillomavirus: a case of acquired epidermodysplasia verruciformis. CMAJ. 2015 Feb 03;187(2):126-8.[↩]
- Imahorn E, Yüksel Z, Spoerri I, Gürel G, Imhof C, Saraçoğlu ZN, Koku Aksu AE, Rady PL, Tyring SK, Kempf W, Itin PH, Burger B. Novel TMC8 splice site mutation in epidermodysplasia verruciformis and review of HPV infections in patients with the disease. J Eur Acad Dermatol Venereol. 2017 Oct;31(10):1722-1726.[↩]
- de Jong SJ, Imahorn E, Itin P, Uitto J, Orth G, Jouanguy E, Casanova JL, Burger B. Epidermodysplasia Verruciformis: Inborn Errors of Immunity to Human Beta-Papillomaviruses. Front Microbiol. 2018;9:1222[↩]
- Gubinelli E, Posteraro P, Cocuroccia B, Girolomoni G. Epidermodysplasia verruciformis with multiple mucosal carcinomas treated with pegylated interferon alfa and acitretin. J Dermatolog Treat. 2003 Sep;14(3):184-8.[↩]
- Pereira de Oliveira WR, Carrasco S, Neto CF, Rady P, Tyring SK. Nonspecific cell-mediated immunity in patients with epidermodysplasia verruciformis. J. Dermatol. 2003 Mar;30(3):203-9.[↩]
- de Oliveira WR, Neto CF, Rivitti EA. The lack of a clinical effect of cimetidine in the treatment of epidermodysplasia verruciformis. J. Am. Acad. Dermatol. 2004 Jun;50(6):e14; author reply e15[↩]
- Rajabi MT, Ghasemi H, Safizadeh M, Jamshidi S, Asadi-Amoli F, Abrishami Y, Oestreicher JH. Conjunctival squamous cell carcinoma with intraocular invasion after radiotherapy in epidermodysplasia verruciformis. Can. J. Ophthalmol. 2014 Apr;49(2):e43-6[↩]
- Vohra S, Sharma NL, Shanker V, Mahajan VK, Jindal N. Autosomal dominant epidermodysplasia verruciformis: a clinicotherapeutic experience in two cases. Indian J Dermatol Venereol Leprol. 2010 Sep-Oct;76(5):557-61[↩]