Fowler’s position
Fowler’s position is a standard patient position in which the patient is seated in a semi-sitting position (45 to 60 degrees) with knees either straight or slightly bent 1. Fowler’s position includes angles between 30 and 90 degrees. Fowler’s position is used in nursing to promote oxygenation to allow for maximum chest expansion, minimizing abdominal muscular tension and minimizing the effects of gravity on the chest wall, therefore, a useful maneuver for patients in mild to moderate respiratory distress. Respiratory changes result in increased oxygenation by maximizing chest expansion. Fowler’s position is usually implemented in cases of respiratory distress. Fowler’s position increases comfort during eating and other activities, is used in postpartum women to improve uterine drainage, and in infants when signs of respiratory distress are present. Fowler’s position is also frequently used when feeding a patient with feeding precautions, during breathing treatments, to perform activities of daily living, for dependent drainage after abdominal surgery, pneumonectomy or other such surgeries. High Fowler’s position with the head of the bed between 60 and 90 degrees is useful during placement of orogastric and nasogastric feeding tubes as it decreases the risk of aspiration. Peristalsis and swallowing are aided by the effect of gravitational pull.
There are several Fowler’s positions 2:
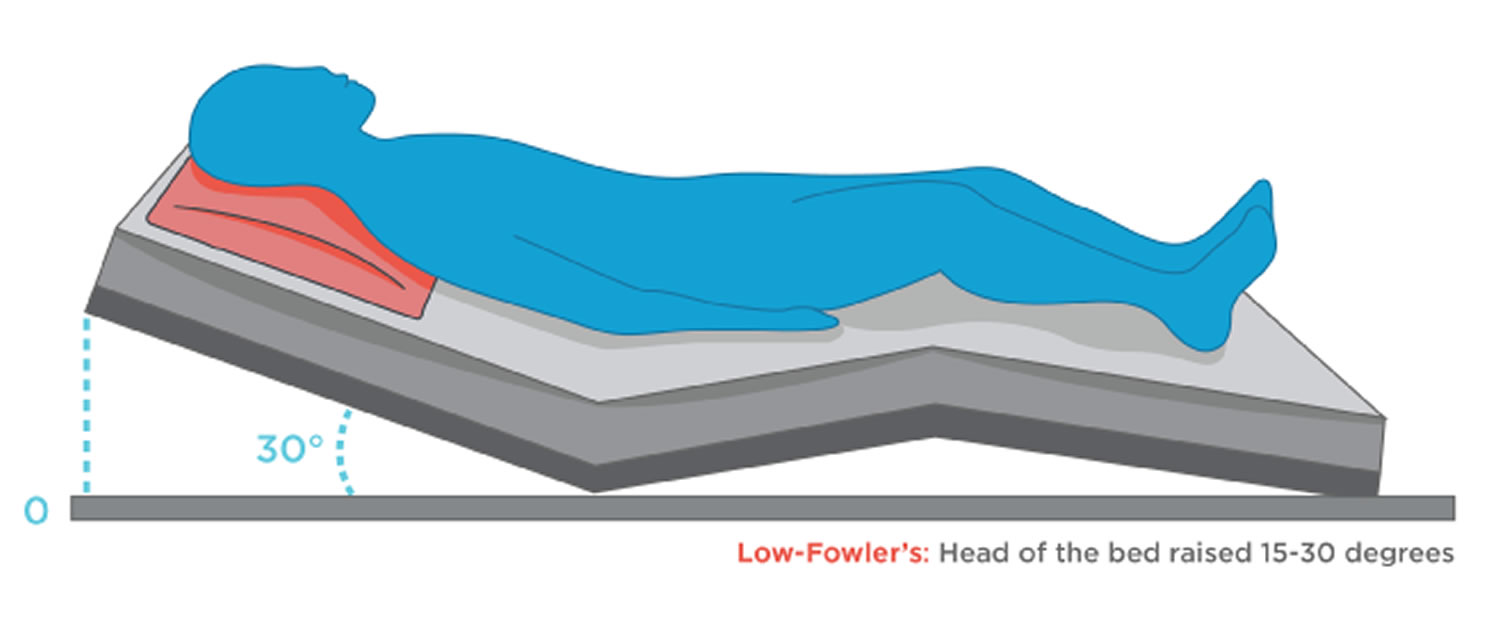
- Low Fowler’s position: head of the bed raised 15-30 degrees
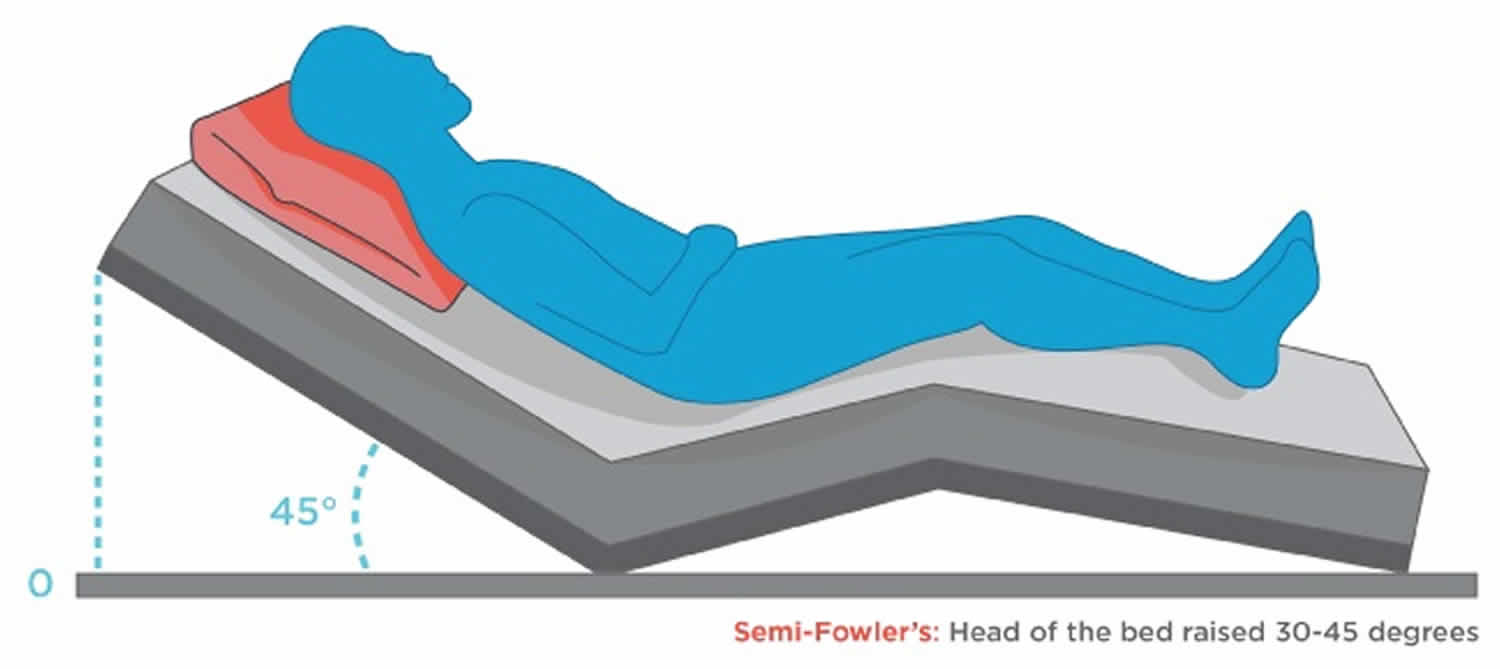
- Semi Fowler’s position: head of the bed raised 30-45 degrees
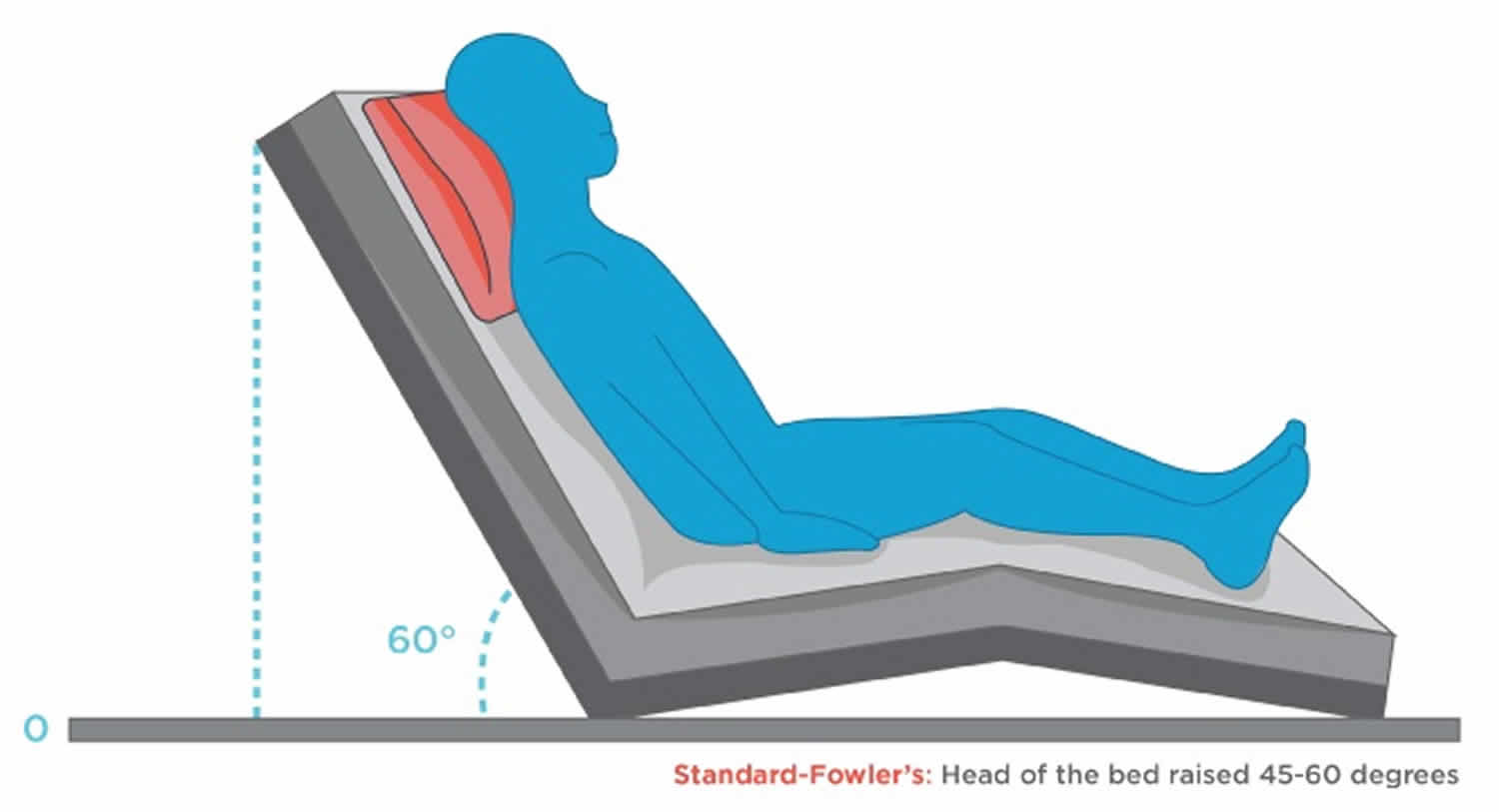
- Standard Fowler’s position: head of the bed raised 45-60 degrees
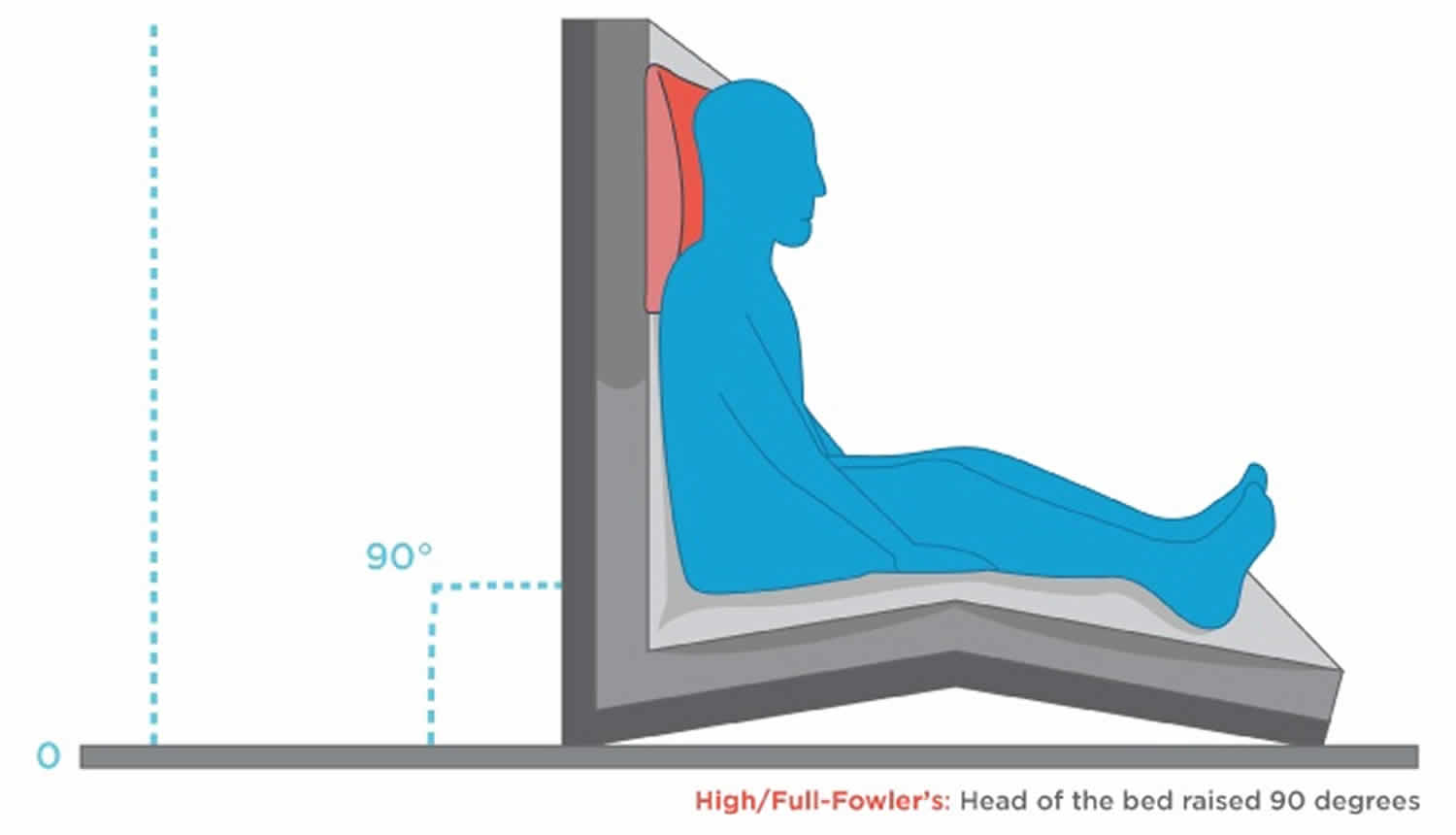
- High Fowler’s position (Full Fowler’s position): head of the bed raised between 60 and 90 degrees.
The upright head and trunk in Fowler’s position are more essential for the quality of life of patients who are confined to bed or frail and it is clinically applied most frequently at inclinations between 30° and 60° 3. Patients who are confined to bed or frail are frequently placed in Fowler’s position instead of remaining supine to assist ambulation, monitor hemodynamics and facilitate breathing as well as routine activities such as eating or conversation 4. On the other hand, such patients develop orthostatic hypotension because they cannot physically compensate quickly for the downward fluid shift caused by assuming an upright position 5. Thus, to understand the most effective posture required to counteract the downward fluid shift while in Fowler’s position should be clinically meaningful. Some studies have described a relationship between the angle of Fowler’s position and the accuracy of hemodynamic measurements among patients in intensive care units 6 and Driscoll et al. 7 reported that cardiac output is decreased in patients under intensive care who are in the Fowler’s position, compared with those who are supine. A study of young healthy individuals has shown that blood pressure in Fowler’s position is intermediate between the seated and supine positions 8 and a cross-sectional study of hypertensive patients found the same tendency 9. Kubota et al 10 found that slight differences in trunk posture while in Fowler’s position affect hemodynamics. An upright upper trunk results in higher stroke volume and preload and a lower heart rate compared with an upright whole trunk in Fowler’s position.
Figure 1. Low Fowler’s position
Figure 2. Semi Fowler’s position
Figure 3. Standard Fowler’s position
Figure 4. High Fowler’s position
- Armstrong M, Moore RA. Anatomy, Patient Positioning. [Updated 2019 Feb 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513320[↩]
- LaFleur Brooks, Myrna and Danielle (2018). Exploring Medical Language: A Student Directed Approach (10th Ed). Elsevier. p. 68.[↩]
- P.A. Potter. Chapter 39 Hygiene & Chapter 47 Mobility and Immobility, Fundamentals of Nursing (7th edition) (2009), (Mosby, St. Louis) pp. 898-1253[↩]
- C.A. Rauen, M.B.F. Makic, E. Bridges. Evidence-based practice habits: transforming research into bedside practice. Crit. Care Nurse, 29 (2009), pp. 46-59[↩]
- M. Bundgaard-Nielsen, C.C. Jørgensen, T.B. Jørgensen, B. Ruhnau, N.H. Secher, H. Kehlet. Orthostatic intolerance and the cardiovascular response to early postoperative mobilization. Br. J. Anaesth., 102 (2009), pp. 756-762[↩]
- F.J. Shih. Patient positioning and the accuracy of pulmonary artery pressure measurements (180f). Int. J. Nurs. Stud., 36 (1999), pp. 497-505[↩]
- A. Driscoll, A. Shanahan, L. Crommy, S. Foong, A. Gleeson. The effect of patient position on the reproducibility of cardiac output measurements. Heart Lung, 24 (1995), pp. 38-44[↩]
- G. Cicolini, G. Gagliardi, E. Ballone. Effect of Fowler’s body position on blood pressure measurement. J. Clin. Nurs., 19 (2010), pp. 3581-3583[↩]
- G. Cicolini, C. Pizzi, E. Palma, M. Bucci, F. Schioppa, A. Mezzetti, L. Manzoli. Differences in blood pressure by body position (supine, Fowler’s, and sitting) in hypertensive subjects. Am. J. Hypertens., 24 (2011), pp. 1073-1079[↩]
- Effects of trunk posture in Fowler’s position on hemodynamics. Autonomic Neuroscience Volume 189, May 2015, Pages 56-59 https://doi.org/10.1016/j.autneu.2015.01.002[↩]