Functional residual capacity
Functional Residual Capacity (FRC) is the volume of air present in your lungs at the end of passive natural exhalation. However, there is still air left in your lungs 1. Functional residual capacity (FRC) is the sum of Expiratory Reserve Volume (ERV) and Residual Volume (RV) and measures approximately 2400 mL in an average sized person with no lung pathology. At functional residual capacity, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium and there is no exertion by the diaphragm or other respiratory muscles. Functional residual capacity (FRC) cannot be estimated through spirometry, since it includes the residual volume (RV). Residual Volume (RV) is the amount of air an individual never physiologically expires. The residual volume (RV) is the volume remaining in the lungs after expelling as much air from your lungs as possible. The amount of air between residual volume (RV) and functional residual capacity (FRC) is the expiratory reserve volume (ERV). Therefore:
- Functional Residual Capacity (FRC) = Expiratory Reserve Volume (ERV) + Residual Volume (RV)
Functional Residual Capacity (FRC) is the total amount of air in a person’s lungs at the lowest point of their tidal volume (TV). Tidal volume (TV) is the volume of air a person normally inspires and expires. So, after normal expiration, functional residual capacity (FRC) is equal to the amount of air left in the lungs.
In order to measure residual volume (RV) precisely, you would need to perform a test such as nitrogen washout, helium dilution or body plethysmography 2. Gas dilution method uses an inert gas (poorly soluble in alveolar blood and lung tissues), either nitrogen or helium. The subject breathes a gas mixture until equilibrium is achieved. The volume and mixture of gas exhaled after the equilibrium have been achieved permit the calculation of functional residual capacity (FRC). In body plethysmography, the subject sits inside a body box and breathes against a shutter valve. Functional residual capacity (FRC) is calculated using Boyle Law (at a given temperature, the product of gas volume and pressure is constant). Functional residual capacity (FRC) calculated by body plethysmography is usually larger in subjects with obstructive lung disease and air trapping than functional residual capacity calculated using gas dilution methods. Body plethysmography is considered the gold standard for lung volumes measurement 2.
The predicted value of functional residual capacity was measured for large populations and published in several studies 3. Functional residual capacity was found to vary by a patient’s age, height, and sex. Functional residual capacity is directly proportional to height and indirectly proportional with obesity. It is reduced in the setting of obesity primarily due to a reduction in chest wall compliance. An online calculator exists (https://dynamicmt.com/dataform3.html) that will calculate functional residual capacity for a patient using these references.
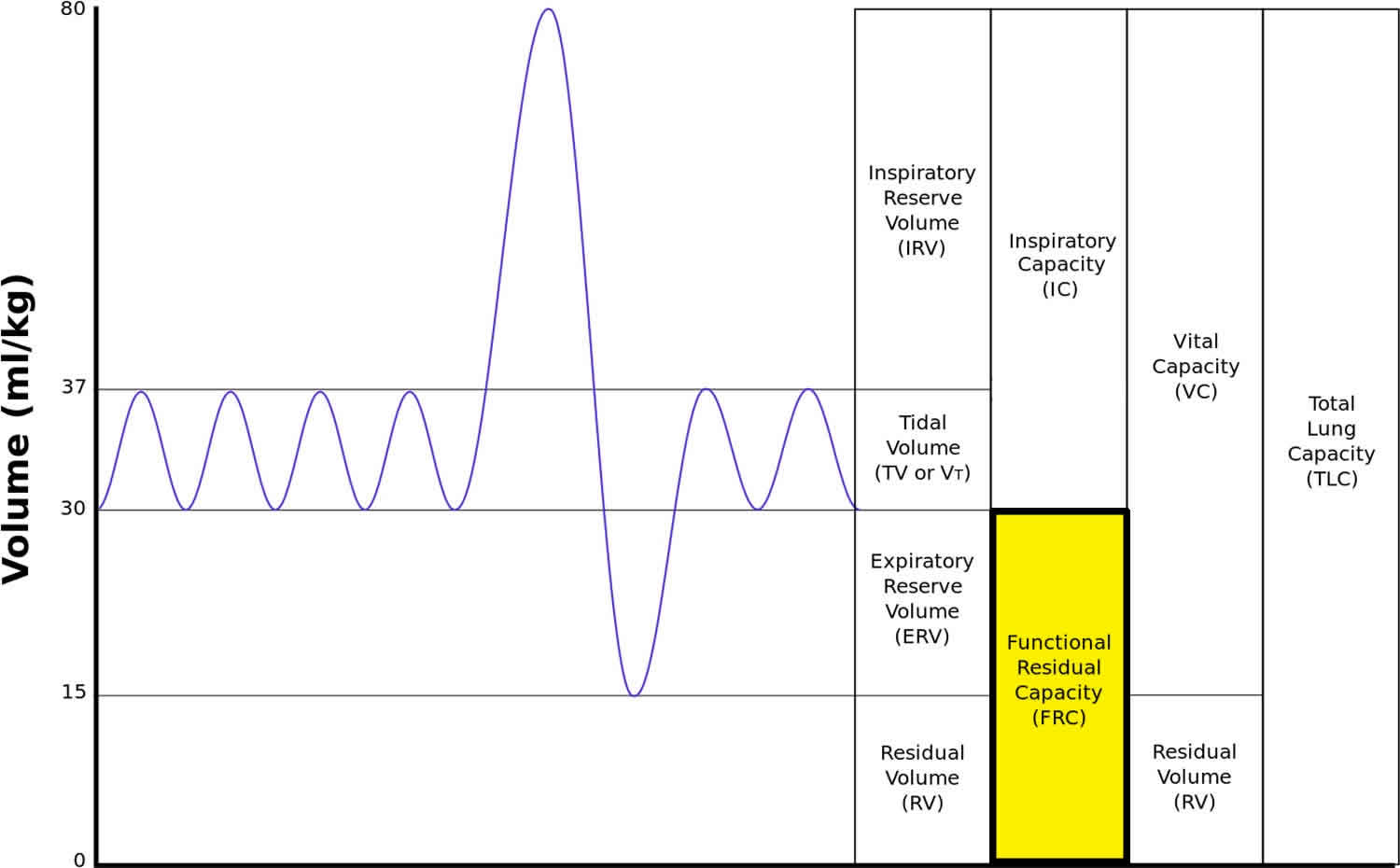
Capacities are the sum of 2 or more volumes (Figure 1). Total lung capacity (TLC) the volume in the lungs at maximal inflation, the sum of vital capacity (VC) the volume of air breathed out after the deepest inhalation and residual volume (RV) the volume of air remaining in the lungs after a maximal exhalation. Total lung capacity (TLC) is the gold standard for diagnosis of restrictive lung disease. Total lung capacity (TLC) less than 5 percentile of predicted or less than 80% predicted are diagnostic of a restrictive ventilatory defect 4.
An important aspect of understanding functional residual capacity (and the respiratory cycle in general) is knowledge of the forces involved. There are 2 main mechanical forces throughout the breathing cycle: the force of the chest wall and the force of the lungs. Without the necessary physiological pressures, the chest wall would expand outward, and the lungs would collapse. This is what occurs when the vacuum is disrupted such as with a stab wound leading to a pneumothorax. functional residual capacity is the point at which these forces are at equilibrium; that is, the difference between the inner recoil forces of the lungs and the outer recoil forces of the chest wall are balanced 2.
A lowered or elevated functional residual capacity is often an indication of some form of respiratory disease. For instance, in emphysema, functional residual capacity is increased, because the lungs are more compliant and the equilibrium between the inward recoil of the lungs and outward recoil of the chest wall is disturbed. As such, patients with emphysema often have noticeably broader chests due to the relatively unopposed outward recoil of the chest wall. Total lung capacity also increases, largely as a result of increased functional residual capacity. In healthy humans, functional residual capacity changes with body posture. Obese patients will have a lower functional residual capacity in the supine position due to the added tissue weight opposing the outward recoil of the chest wall.
Positioning plays a significant role in altering functional residual capacity. It is highest when in an upright position and decreases as one moves from upright to supine/prone or Trendelenburg position. The greatest decrease in functional residual capacity occurs when going from 60° to totally supine at 0°. Interestingly, there is no significant change in functional residual capacity as position changes from 0° to Trendelenburg of up to -30°. However, beyond -30°, the drop in functional residual capacity is considerable 5.
Once Functional Residual Capacity (FRC) is measured, the clinician may calculate Residual Volume (RV), and with that value may calculate the patient’s Total Lung Capacity (TLC). This is possible due to the following equations:
- TLC = RV + ERV + IRV + TV + IRV
- TLC = FRC + TV + IRV
- FRC = RV + ERV
- RV = FRC – ERV
- RV = TLC – (IRV + TV + ERV)
*TLC= total lung capacity, RV= residual volume, ERV= expiratory reserve volume, IRV= inspiratory reserve volume, FRC= functional residual capacity
The Expiratory Reserve Volume (ERV) can be measured. So, if a clinician measures the Functional Residual Capacity (FRC), the Expiratory Reserve Volume (ERV) can also be obtained and subtracted from FRC to calculate the Residual Volume (RV). The Total Lung Capacity (TLC) can be obtained by adding all of the lung volumes together after Residual Volume (RV) has been calculated or by adding Functional Residual Capacity (FRC), Tidal Volume (TV), and Inspiratory Reserve Volume (IRV) [Inspiratory Reserve Volume is the maximal volume that can be inhaled from the end-inspiratory level are needed] (third equation).
If whole body plethysmograph is utilized, other informative values may be distinguished including the specific airway resistance (sRaw), airway resistance (Raw), and shift volume. All of these values together, when obtained, paint a detailed clinical picture of a patient’s lung function.
Years of studying patients’ various lung volumes led to the realization that by analyzing gathered data, equations could be used to predict the person’s likely lung volumes/capacities. Equations such as these are how clinicians can compare a patient’s lung function to what is considered normal for that patient 6.
Figure 1. Functional residual capacity
Functional residual capacity function
As previously mentioned, Functional Residual Capacity (FRC) contains both the Expiratory Reserve Volume (ERV) and Residual Volume (RV).
Expiratory Reserve Volume (ERV)
While sitting quietly or performing normal activities, the only air a person with no respiratory pathology breathes is their Tidal Volume (TV). However, when a person exerts energy, more oxygen is needed and the volume of air ventilated increases in both directions; more air is inspired, and more air is expired. Think of someone running a race. Their energy expenditure increases and more oxygen is needed to continue at an acceptable pace. This is one reason both Expiratory Reserve Volume (ERV) and Inspiratory Reserve Volume (IRV) [Inspiratory Reserve Volume is the maximal volume that can be inhaled from the end-inspiratory level are needed].
Residual Volume (RV)
Residual Volume (RV) is the amount of air a person may never physiologically expire. Why is Residual Volume (RV) essential? Imagine blowing up a balloon. The most difficult part of inflating a balloon is the first expelling of air. If all of the air left your lungs every time extra lung volume was needed, the work of breathing would increase tremendously. Your lungs would collapse, and any strenuous activity would be not only difficult, but also dangerous.
Functional Residual Capacity (FRC) is dependent upon many factors. Some of these are uncontrollable including age, height, and biological gender. Other elements that are sometimes controllable or reversible include pathological respiratory diseases (often due to smoking), some occupations that lead to lung disease, pregnancy, diseases that cause ascites, and acute changes in position such as laying supine.
Age
As humans age, our pulmonary function also declines; muscle mass, the elasticity of tissue, alveolar surface area, and diffusion capability all decrease. A person’s ability to respond to insults also lessens. The decrease in muscle mass includes the muscles we use to breathe. Loss of elasticity in connective tissue increases the work of breathing; similar to chronic obstructive pulmonary disease (COPD) (but to a lesser extent), the air becomes harder to expel. The lungs do not as readily return to normal size after inspiration.
Height and Gender
If a person is taller, their diaphragm is likely larger, and they need more oxygen to perform the same tasks as do smaller individuals. This means that they need more lung volume to accomplish this and therefore have an increased functional residual capacity. While it is tempting to assume this is the reason for differences of lung volume between genders, research has shown that men and women who are the same height and age still differ in lung volumes. Men tend to have a significantly larger lung volume, and because of this an increased functional residual capacity. This is likely due to structural differences between men and women. Women have ribs that are angled differently than men and a shorter diaphragm length. Due to the difference in rib angle, women have a greater capacity to expand their lungs. While women have a smaller rib cage and a shorter diaphragm length, the angle of a woman’s ribs has shown to lend an increased advantage in inspiratory capacity. This is likely to aid physiological changes that occur during pregnancy.
Pregnancy
Pregnant women need more oxygen to have the necessary energy to fertilize an egg and create a fetus. Physiological hormone changes throughout pregnancy allow a pregnant woman’s respiratory status to change significantly. While spirometry remains within normal limits, structural and volumes/capacities change significantly. The diaphragm relaxes (due to aforementioned hormonal changes), and the growing fetus begins to exert pressure on the thoracic cavity. This causes both the Expiratory Reserve Volume (ERV) and Residual Volume (RV) to decrease, which leads to a decreased functional residual capacity. However, a pregnant female’s oxygen requirements are increased. Tidal Volume (TV) and Inspiratory Reserve Volume (IRV) increase, and a pregnant woman’s ribcage grows in size while the subcostal angle increases. The previously mentioned inspiratory advantage due to rib angle likely helps a pregnant female compensate. Because of the lowered functional residual capacity and pressure on the thorax, a pregnant woman is more susceptible to atelectasis. This likelihood is increased when laying supine. The result is the possibility of a slightly reduced PaO2 if a blood gas is obtained, especially when in this position. It is also important to note that while minute ventilation (MV) increases throughout pregnancy, this is mostly due to the increase in Tidal Volume (TV). Respiratory rate is largely unchanged.
Ascites
Similar to pregnancy, functional residual capacity also changes with ascites, whether caused by liver disease, malignancy, or other pathology. With significant disease of the liver, portal hypertension causes fluid to leak out of the capillaries into the abdomen. Increased abdominal girth yields cephalad pressure on the diaphragm, decreasing functional residual capacity. This is one of the causes of shortness of breath in patients with ascites; unlike in pregnancy, Tidal Volume (TV) and Inspiratory Reserve Volume (IRV) are not increased.
Postoperative Changes
Post-surgical patients also experience a drop in functional residual capacity. Medications given during anesthesia relax the muscles of respiration. When a person breathes, the diaphragm moves inferiorly to help create the negative pressure gradient that brings air into the lungs. When the accessory muscles of respiration are relaxed, and analgesic/anesthetic/paralytic medications have been consumed, the diaphragm experiences superior movement (cephalad) rather than inferior. This reduces functional residual capacity significantly, and some studies have suggested that the length of time that functional residual capacity is reduced is directly proportional to the likelihood of post-surgical pulmonary complications 7.
Functional residual capacity importance
Before discussing specific lung pathologies and their relationship to functional residual capacity (FRC), it is important to have a basic understanding of compliance and elasticity. Compliance and elasticity are defined mathematically as:
- Compliance (C) = change in volume/change in pressure
- Elasticity (E) = 1/C or E= change in pressure/change in volume
Compliance is the change in volume per change in unit pressure. Elasticity is the inverse of compliance: the change in unit pressure per change in volume. Simply stated, compliance is the ease of distension; elasticity is the ease at which a distended structure returns to the original volume. The more compliant an object, the less elastic, and vice versa.
In restrictive respiratory states, the lungs or chest wall are affected in a way that limits lung expansion. While some restrictive states can be due to chest wall issues (such as severe kyphosis), here restrictive pathology of the lung itself will be considered. An example of a restrictive disease of the lung is idiopathic pulmonary fibrosis. An increase in fibrous tissue in the lung causes a decrease in lung compliance; the lungs become more elastic and therefore harder to inflate. This decreases Total Lung Capacity (TLC), and therefore functional residual capacity (FRC), due to the lungs being harder to fill.
With obstructive respiratory pathology of the lungs such as emphysema, there is a reduction in airflow, and the lungs become increasingly compliant. Alveoli are destroyed, air is trapped, and TLC is increased. Consequently, functional residual capacity (FRC) is also increased. The increased volume and compliance causes the chest wall to experience less resistance from the lungs, hence, the typical barrel chest seen in those with emphysema.
The previous paragraphs illustrate the importance of understanding basic principles and definitions in physiology to perceive the pathological conditions that plague patients correctly. Mastering this knowledge can also simplify the process of explaining a disease the patient. If a patient understands their pathology and why pharmacological interventions are important, one can infer that there will be an increase in patient compliance to treatments meant to lengthen life or improve symptoms.
While other lung values are more widely used clinically, functional residual capacity contains utility both in understanding the respiratory cycle and in clinical practice. Since functional residual capacity (FRC) is the equilibrium point for the forces of the chest wall and lung, it is an efficient starting point when learning about the chest wall/lung system. Both clinicians and researchers use methods to calculate functional residual capacity (FRC) to obtain values that cannot be measured by standard spirometry 8.
- Hopkins E, Sharma S. Physiology, Functional Residual Capacity. [Updated 2019 Mar 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500007[↩]
- Ponce MC, Sharma S. Pulmonary Function Tests. [Updated 2019 Mar 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482339[↩][↩][↩]
- P.H. Quanjer. “Lung Volumes and Forced Ventilatory Flows.” Eur Respir J, Vol 6, Suppl 16, pp. 5-40, 1993.[↩]
- Ali NA, Nafees AA, Fatmi Z, Azam SI. Dose-response of Cotton Dust Exposure with Lung Function among Textile Workers: MultiTex Study in Karachi, Pakistan. Int J Occup Environ Med. 2018 Jul;9(3):120-128.[↩]
- Barash, Clinical Anesthesia, 6th edition, pp. 247-248.[↩]
- Lofrese JJ, Lappin SL. Physiology, Residual Volume. [Updated 2019 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493170[↩]
- Hallett S, Ashurst JV. Physiology, Tidal Volume. [Updated 2019 Feb 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482502[↩]
- Hewlett JC, Kropski JA, Blackwell TS. Idiopathic pulmonary fibrosis: Epithelial-mesenchymal interactions and emerging therapeutic targets. Matrix Biol. 2018 Oct;71-72:112-127.[↩]