Dislocated hand
Hand dislocation is a common injury in sports and in occupational settings, often appearing to be minor. However, hand dislocations have real potential for long-term disability in sports and other areas of life if adequate reduction is not performed, if associated injuries are not identified and appropriately treated or referred, and if potential complications of the injury and its treatment are not foreseen. Symptoms and the circumstances of the injury suggest the diagnosis, but doctors take x-rays to confirm it. The judgment of the initial treating physician can be critical in determining the long-term outcome of these injuries.
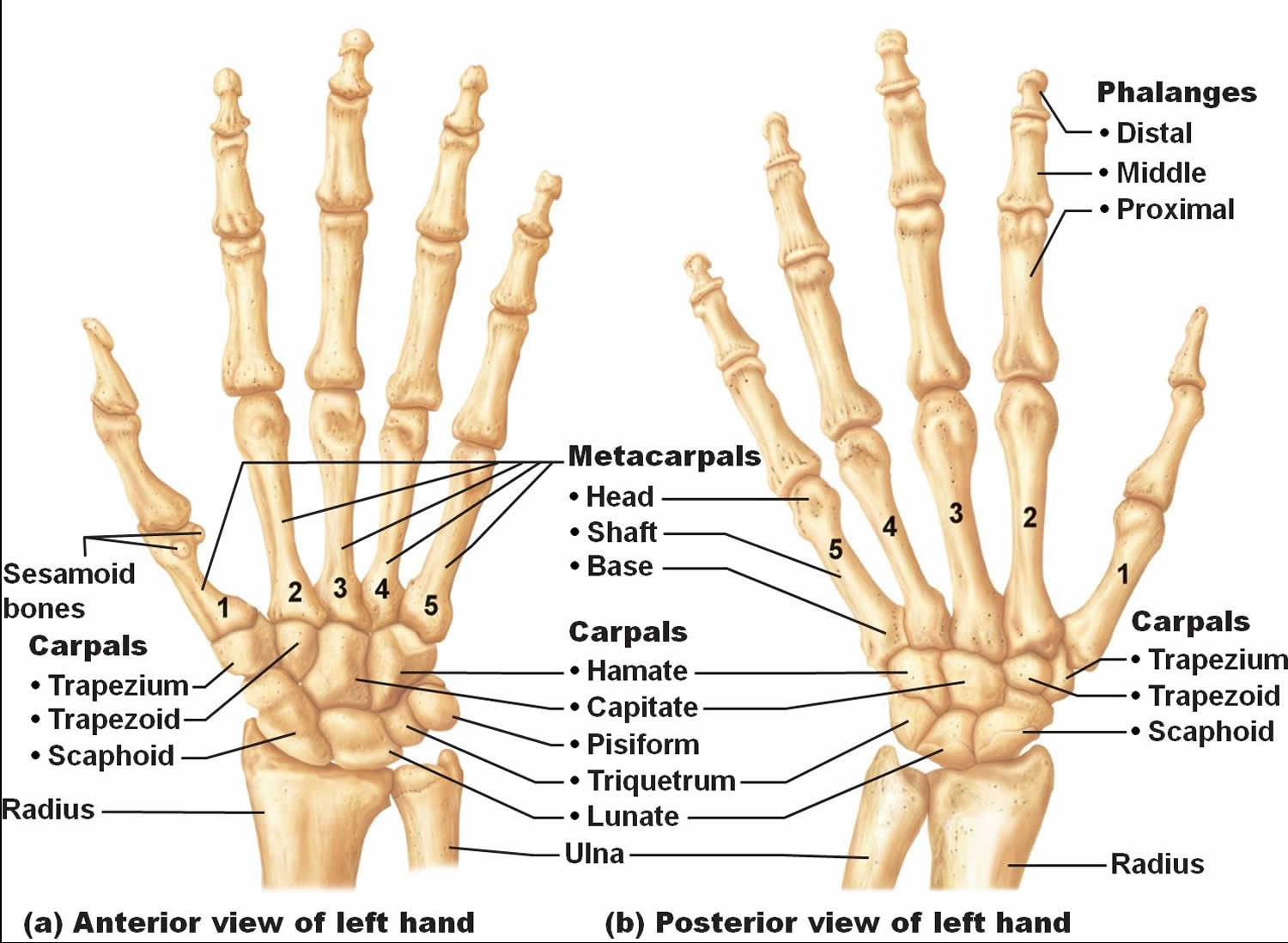
The bones at the base the hand (carpal bones or wrist bones), between the forearm bones (radius and ulna) and the long metacarpal bones of the hand, usually the lunate or the capitate, move out of their normal position. These dislocations usually occur when great force is applied to the wrist and it is bent backward, usually a fall on an outstretched hand or an injury in a car crash.
Two of the carpal bones are commonly dislocated:
- The capitate (which is the largest bone in the hand, located in the middle of the lower palm)
- The lunate (which is located between the capitate and the end of the ulna)
Dislocation of the capitate is called a perilunate dislocation. Perilunate dislocations are more common than lunate dislocations.
The wrist and hand are painful and may look misshapen, and people cannot move them normally.
Many hand dislocations can be effectively treated with closed reduction, traction, or both. Grossly unstable joints and those for which closed reduction has failed typically require surgical intervention. Physical and occupational therapy are key components of treatment throughout. Any long-term complications (usually involving stiffness or instability) that develop must be addressed.
A hand surgeon should see any patient with hand dislocations which require or may require surgery. A hand surgeon should be involved early in the treatment of any complicated proximal interphalangeal or distal interphalangeal injury. The need for such consultation would be indicated if the patient presents late after the injury, was inadequately assessed at initial presentation, or develops an unforeseen complication (eg, recurrent subluxation in a joint that appeared to be stable after reduction).
Most patients with chronic instability or stiffness in a finger (especially if it involves the proximal interphalangeal joint) should be referred for assessment by a hand surgeon.
Treatment of hand dislocation depends on the site and severity of your injury. It might involve:
- Reduction. Your doctor might try gentle maneuvers to help your bones back into position. Depending on the amount of pain and swelling, you might need a local anesthetic or even a general anesthetic before manipulation of your bones.
- Immobilization. After your bones are back in position, your doctor might immobilize your joint with a splint or sling for several weeks. How long you wear the splint or sling depends on the joint involved and the extent of damage to nerves, blood vessels and supporting tissues.
- Surgery. You might need surgery if your doctor can’t move your dislocated bones into their correct positions or if the nearby blood vessels, nerves or ligaments have been damaged. Surgery may also be necessary if you have had recurring dislocations, especially of your shoulder.
- Rehabilitation. After your splint or sling is removed, you’ll begin a gradual rehabilitation program designed to restore your joint’s range of motion and strength.
Figure 1. Hand bones
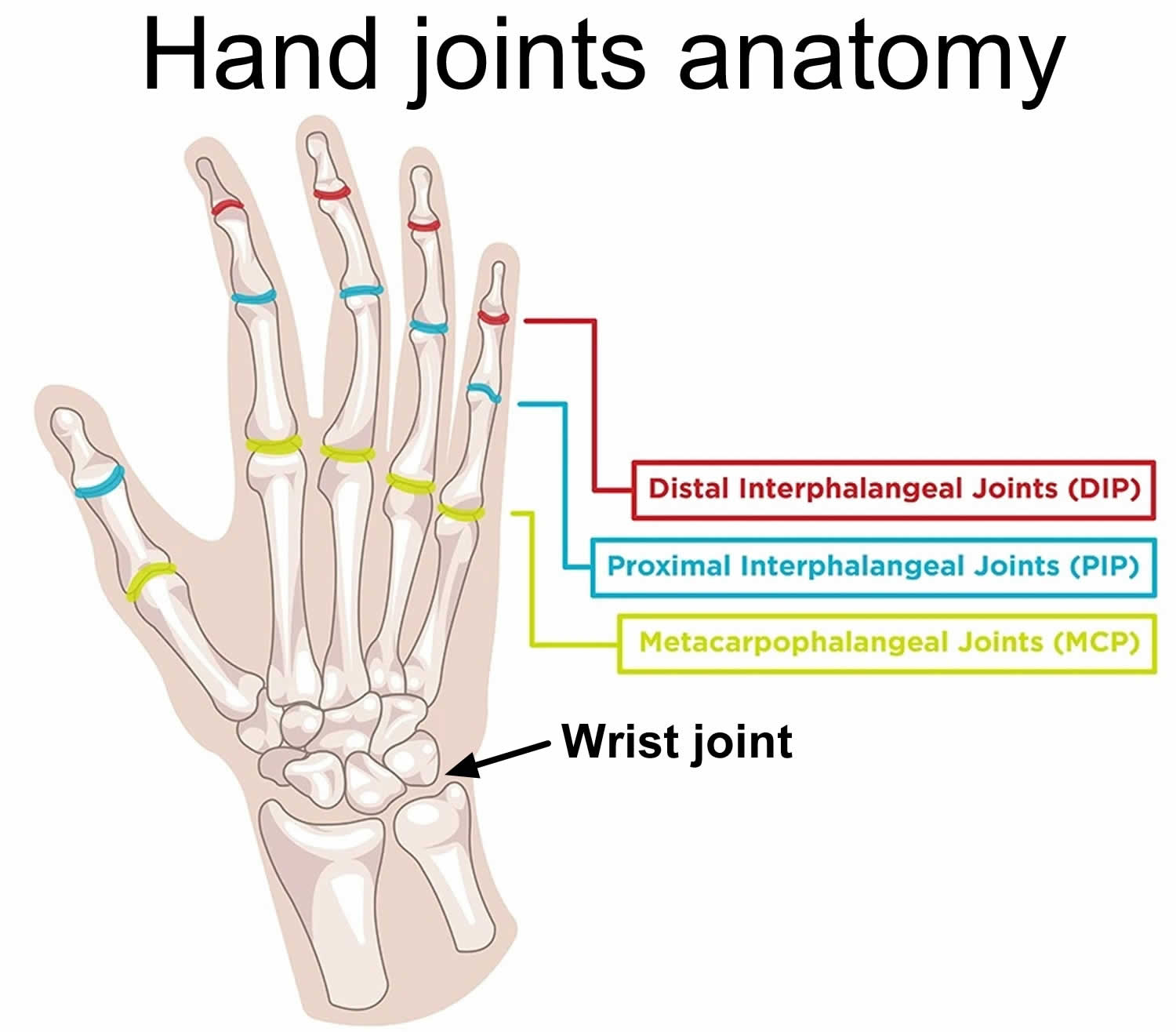
Figure 2. Hand wrist and finger joints
Hand anatomy
Interphalangeal joints
The bony anatomy of the proximal interphalangeal (PIP) joint consists of medial and lateral condyles on the proximal phalanx, with matching concavities on the associated distal phalanx. The joint has a wide range of motion (ROM) in flexion and extension but is relatively rigid in abduction and adduction; thus, it is a hinge (ginglymus) joint functionally. The bony anatomy of the distal interphalangeal (DIP) joint is similar, but the surrounding soft tissue provides more restriction in flexion.
The extrinsic flexors across both joints are at least 4 times stronger than the extensors, allowing flexion contractures to develop very rapidly, especially with immobilization in flexion. Adequate range of motion, especially at the proximal interphalangeal (PIP) joint, is critical for normal hand function.
The proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints are both supported on all 4 sides by similar soft-tissue structures, which include the volar plate on the palmar side (the integrity of which is essential for a stable reduction), collateral ligaments on the radial and ulnar sides, and the extensor complex (central slip, lateral bands, and hood) dorsally (see Figures 1 and 2 above). These structures attach to and reinforce the joint capsule. For a dislocation to occur, at least 1, often 2, and sometimes 3 of these structures must be significantly injured.
The volar plate is a roughly triangular structure with its base oriented distally, attaching to the volar base of the middle phalanx with its tip attaching to the distal aspect of the proximal phalanx. The volar plate functions largely in limiting hyperextension. Thus, it is nearly always injured in dorsal dislocations.
The collateral ligaments restrict the joint from opening to varus or valgus stress and are also commonly injured in dorsal dislocation. Injury to the radial collateral ligament is about 6 times more common than injury to the ulnar collateral ligament.
The extensor complex comprises the central slip, which attaches to the base of the middle phalanx; the lateral bands, which run dorsolaterally on each side; and the transverse retinacular ligament, which connects these structures and extends laterally. It helps limit volar movement of the base of the middle phalanx and thus is commonly injured in volar dislocations at the PIP joint, with the middle phalanx either tearing the central slip from its insertion or buttonholing through the transverse retinacular ligament between the central slip and a lateral band.
Metacarpophalangeal (MCP) joint
The metacarpophalangeal (MCP) joint is thought to be an ellipsoid joint. The head of the metacarpal consists of medial and lateral condyles and is narrower on its dorsal surface than on its palmar surface; it fits into the concavity of the base of the proximal phalanx. The true collateral ligament attaches to a recess created by the junction of the shoulder and head. The collateral ligament is composed of the following 2 parts:
- A dorsally placed cord portion
- A fan-shaped volar portion or accessory collateral ligament, which extends from the metacarpal to the sides of the volar plate
To accomplish flexion and extension at the MCP joint, the anterior and posterior parts of the capsule must be lax. When the joint is extended, the phalanges have considerable lateral play in abduction and adduction; consequently, this joint is not frequently injured. However, if the ligament is torn, dislocation occurs.
The MCP joint of the thumb has radial and ulnar collateral ligaments, which are loose when the joint is extended and tight when flexed. When the joint is extended, the proximal phalanx has the lateral play achieved by the action of the interosseous muscles.
When the thumb is flexed and in a functional position, as in the case of many sports situations (eg, skiing, falls on a gloved hand), the ulnar collateral ligament is the structure at risk and can be ruptured (see Skier’s Thumb). The ulnar collateral ligament can then be displaced so that the adductor aponeurosis is interposed between the ruptured end of the ligament and its site of bony attachment.
Carpometacarpal (CMC) joint
The bony anatomy of the carpometacarpal (CMC) joint consists of the 5 metacarpal bases that articulate with the trapezoid, trapezium, capitate, and hamate (in that order) from the radial aspect of the hand to its ulnar aspect. The carpometacarpal (CMC) joint is a relatively fixed joint segment because of the articular congruity of the joint surfaces, with the metacarpal bases acting like concave receptacles to the distal carpal row, and because of the strong interosseous and extrinsic ligament complex.
The palmar and dorsal ligaments are distinct, with the palmar ligaments being stronger. The scaphoid acts as a link between the proximal and distal carpal rows. The extensor and flexor tendons pass over this articular area but add no strength to the carpometacarpal joint because the bases of the metacarpals dislocate dorsally relative to the distal carpal row.
The first carpometacarpal joint also referred to as the first metacarpotrapezoid joint (thumb joint) is a highly mobile saddle joint, with articular surfaces that are reciprocally concavoconvex. The most important soft-tissue support for this first carpometacarpal joint is the deep ulnar or anterior oblique ligament, which runs from the volar beak of the metacarpal to the tubercle of the trapezium. This ligament can be ruptured, but it tends to be avulsed with a piece of bone (Bennett fracture-dislocation).
Hand dislocation causes
Hand dislocation is caused by the following:
- Sports injuries (usually involving contact sports or a ball forcefully striking the tip of the finger)
- Occupational injuries
- Falls
- Traffic collisions
Dislocations of the proximal interphalangeal and distal interphalangeal joints of the hand probably occur most commonly in basketball and football. In basketball, the usual mechanisms include being struck by the ball, catching a finger on the rim, or contact with another player. In football, the finger may be caught on a jersey, slapped against a helmet, or crushed between some combination of players, equipment, and the ground. Linemen and defensive players are at highest risk. In both sports, return to play almost always requires that the injury can be splinted stably to allow a power grip.
Dislocations of the metacarpophalangeal and basilar carpometacarpal joints occur most commonly with falls on the outstretched hand so-called FOOSH injury or the flexed supinated wrist. With this extension vector, the forces are transmitted up through the carpus.
Injuries and dislocations of the thumb, the metacarpophalangeal joint, and the carpometacarpal basilar joint commonly occur in falls with the thumb in abduction. Examples of this type of injury include a fall on the gloved hand in baseball or application of an abduction force to a flexed thumb while the hand is grasping an object—as in skiing injuries, when the pole impacts the proximal phalanx tearing the radial collateral ligament. This occurs when the wrist is extended at the time of the injury.
Traumatic force applied to the hand can be transmitted to bone, soft tissue, nerves, and vascular structures. Because the structures of the hand are close to the surface and near each other, injury often results in a combination of fractures, dislocations, and soft tissue injury.
The distal interphalangeal and proximal interphalangeal joints both have lateral ligaments and a fibrous volar plate. Common dislocations are posterior or lateral. Typical forces resulting in distal interphalangeal dislocations include a jamming blow to the end of the finger. Forces that commonly lead to proximal interphalangeal joint dislocation include axial loading or hyperextension. Lateral dislocations can result from radial- or ulnar-directed force on the joint.
Dislocations of finger metacarpophalangeal joints are rare and frequently are trapped by the surrounding ligaments, in which case surgical relocation is necessary. metacarpophalangeal or palmar dislocations occur when a hyperextension movement occurs with rotation. The finger is bent back toward the top of the hand and is twisted during the injury. The finger may have been pushed, or compressed, during the injury. metacarpophalangeal dislocations are typically associated with fractures.
In thumb metacarpophalangeal joint dislocations, the mechanism encountered most often is hyperextension that leads to volar dislocations. A significant lateral force can disrupt the collateral ligaments, resulting in instability. Gamekeeper’s (skier’s) thumb often results from a fall onto the hand with the thumb in abduction (as when the hand grips a ski pole) 1.
Carpometacarpal joint dislocation 2 is not always a high-energy injury. Identification involves careful analysis of subtle findings on radiographs and may require additional radiographic views. Missed diagnosis of carpometacarpal dislocation can result in significant morbidity.
Hand dislocation symptoms
When one of these carpal (wrist) bones is dislocated, the wrist and palm of the hand are painful. People cannot move the wrist and hand normally. The wrist usually looks misshapen, and the hand swells.
The fingers may tingle and feel numb because the dislocated bone puts pressure on the carpal tunnel (a narrow passageway of fibrous tissue) and the nerves and blood vessels it contains (causing carpal tunnel syndrome). The blood supply to bones in the wrist may be reduced or disrupted, and bone tissue may die. Over time, the wrist joint may deteriorate, causing disabling arthritis.
Hand dislocation diagnosis
Besides examining your injury, your doctor might order the following
- X-ray. An X-ray of your joint is used to confirm the dislocation and may reveal broken bones or other damage to your joint.
- The following views should be taken:
- Anteroposterior
- Lateral (to check the lateral radiograph for joint congruency or rotation)
- Oblique
- Stress views can be examined if ligamentous laxity is documented or suspected.
- The following views should be taken:
- In rare circumstances, computed tomography (CT) or magnetic resonance imaging (MRI) may be necessary to make a definitive diagnosis 3. MRI can help your doctor assess damage to the soft tissue structures around a dislocated joint.
Swelling, tenderness, or deformity at a joint or along the digit should prompt radiographic evaluation. Findings can be subtle; pain out of proportion to radiographic findings should heighten the physician’s suspicion for significant injury.
If radiographs are obtained and no identifiable fracture is visible, yet the patient remains in a significant amount of discomfort, an occult fracture may be present. Proper splinting and urgent referral may be indicated.
A child or adolescent with open growth plates who remains in pain even though radiographs reveal no fracture may have a growth plate injury. Proper splinting and urgent referral may be indicated.
Postreduction images must follow even the most apparently routine reductions.
Radiographs of the affected finger help further define the anatomy of the dislocation, rule out associated fractures, and assess the adequacy of reduction. For dorsal dislocations at the proximal interphalangeal (PIP) joint, the initial radiographs are often obtained after reduction because the athlete, trainer, or coach commonly reduces the dislocation at the scene. If the finger is still dislocated when the radiographs are obtained, the middle phalanx may be hyperextended and often deviated to the ulnar side.
Common fractures to look for include avulsions and impacted fractures. Avulsions at the volar base of the middle phalanx (or the distal phalanx, in the case of distal interphalangeal [DIP] joint injury) from the volar plate may not affect the treatment plan if they are small. Larger fractures at this location make the injury a fracture-dislocation, which may be unstable in extension.
Avulsions at the dorsal base of the middle phalanx (or the distal phalanx, in the case of DIP joint injury) from the extensor tendon should prompt careful testing of extensor function and probably require splinting in extension; splinting in hyperextension should be avoided. Most central slip injuries, however, involve only soft tissue.
Impacted fractures of the joint surface are often best visualized on a true lateral view, allowing direct comparison of the radial and ulnar articular surfaces.
Key considerations in the radiographic assessment of reduction include the following:
- Congruence of the articular surfaces
- Absence of rotational deformity
- Fractures around the metacarpophalangeal (MCP) and carpometacarpal (CMC) joints
With respect to articular congruence, the head of the more proximal phalanx should form a U shape that fits symmetrically within the U shape of the base of the more distal phalanx. If the joint space is not equal throughout on both views, the examiner should be highly suspicious for persistent subluxation secondary to entrapment of soft-tissue structures within the joint.
A volar proximal interphalangeal dislocation in which the head of the proximal phalanx buttonholes between the central slip and the lateral band has a rotational component. This can be observed on the lateral view, where the radial and ulnar aspects of each joint surface would be superimposed.
To rule out fractures around the metacarpophalangeal and carpometacarpal joints, anteroposterior, lateral, and oblique views of the entire hand are indicated. In the dorsal dislocation patterns, the oblique or lateral view reveals the dorsal prominence of the affected joint. Common fractures to look for include avulsion-type fractures of the metacarpal bases, associated with the carpometacarpal dislocation.
The Breuerton view of the metacarpophalangeal joints may be useful. This view is taken with the fingers flat on the plate, the metacarpals at 65° of inclination to the fingers, and the tube at 15° from the ulnar side of the hand. The Breuerton view demonstrates the metacarpophalangeal bony surface.
Modified lateral views of the metacarpals are sometimes necessary because little of the shaft or head can be observed on a true lateral radiograph of the hand. To study the index and middle finger, the hand should be pronated 30° from the lateral. To study the ring and small fingers, the hand should be supinated 30° from the lateral.
Hand dislocation treatment
Many hand dislocations can be effectively treated with closed reduction, traction, or both. Some of these injuries become subluxated in extension and require extension block splinting. Grossly unstable joints and those for which closed reduction has failed typically require surgical intervention. Most patients needing surgery for hand dislocation injuries are best served by treatment in the acute phase. Steroid injection may rarely be indicated for a chronically swollen, painful joint in those with a hand dislocation.
Active range-of-motion and passive range-of-motion exercises are key components of treatment throughout. Ensure early follow-up for reexamination and repeat radiography in questionable cases. Any long-term complications (usually involving stiffness or instability) that develop must be addressed.
Closed reduction and traction
Dislocations of the distal interphalangeal joint are almost always reducible with longitudinal traction and gentle manipulation in the direction opposite to the deformity. Irreducible dislocations may occur if soft-tissue entrapment develops in the joint or if the patient presents more than a few days out from the injury 4.
Closed reduction is almost always successful for dorsal proximal interphalangeal joint dislocations. Volar dislocations are more problematic, especially if the deformity has a rotational component. For all closed reduction maneuvers, be gentle and limit the number of attempts to 2-3. Irreducible dislocations are usually caused by soft-tissue structures (eg, volar plate, collateral ligament, tendons) trapped in the joint, in which case the patient may need to be referred to a hand surgeon for open reduction (see below).
Most dorsal dislocations of the proximal interphalangeal joint can be easily reduced by placing gentle traction on the finger with the wrist and the metacarpophalangeal joints flexed, then pressing the base of the middle phalanx in a volar direction while holding the proximal phalanx steady. In a sports setting, the athlete, coach, or trainer usually accomplishes this maneuver. If the reduction is performed immediately after the injury, it can usually be accomplished without anesthesia. If the reduction is delayed, a digital block with 1% lidocaine (without epinephrine) is helpful.
To perform a digital block, first cleanse the skin with povidone-iodine solution. Insert a 25-gauge needle near the base of the finger and through its dorsolateral aspect just lateral to the periosteum of the base of the proximal digit. Advance the needle posteriorly so that it slides just past the base of the phalanx. As the needle is advanced, inject 1 mL of anesthetic while observing for protrusion of the palmar dermis directly opposite the needle path. Another 1 mL of solution is injected as the needle is withdrawn.
This technique should block both the dorsal and volar digital nerve branches. For complete anesthesia of the finger, it is performed both on the medial side and on the lateral side (see the image below). It is important not to use lidocaine with epinephrine. The digital arteries are end arteries that can spasm and cause ischemia of the fingertip and, potentially, necrosis. To avoid the mechanical pressure generated by injecting solution into a potentially confined space, volumes of 2-4 mL should not be exceeded.
Volar proximal interphalangeal dislocations without a rotational component are usually reducible with gentle traction. Place the wrist in the neutral position, and press dorsally on the base of the middle phalanx and volarly on the proximal phalanx. Although these injuries are usually treatable with closed reduction, they commonly involve an avulsion of the central slip of the extensor tendon.
Volar proximal interphalangeal dislocations with a rotational component are often difficult to reduce by closed means, because the head of the proximal phalanx becomes trapped between the central slip and one of the lateral bands of the extensor mechanism. Sometimes, these injuries can be reduced by placing the metacarpophalangeal and proximal interphalangeal joints in 90° of flexion with the wrist extended, applying traction, and rotating the middle phalanx in the direction opposite to the deformity.
Metacarpophalangeal dislocations most commonly occur dorsally (simple type). Closed reduction is the treatment of choice and usually is readily accomplished with gentle traction and flexion of the proximal phalanx. A local digital nerve block may facilitate the process.
If closed reduction is not accomplished after several attempts and displacement or subluxation persists, open reduction is indicated. At the time of operation, the capsule has usually impinged between the 2 bones, preventing reduction. In children, the displacement of the proximal phalanx may be more to the ulnar than the dorsal side, and a shearing type of osteocartilaginous fragment often prevents complete reduction.
In early or acute dislocations of the metacarpals, the carpus closed reduction should be attempted and is usually successful. These dislocations occur dorsally, and reduction can be obtained by placing gentle traction on the finger of the associated metacarpal while pressing dorsally on the carpometacarpal joint dislocation through the range from flexion to extension.
The closed reduction can be facilitated with local anesthetic hematoma or intra-articular block at the affected area. After the reduction is accomplished, the wrist and carpometacarpal joint should be flexed acutely to determine stability. If closed reduction is successful but the reduction is unstable, continued reduction can be attempted with a dorsiflexion cobra-type cast or percutaneous Kirschner wire (K-wire) fixation 5.
Figure 3. Buddy strapping
Figure 4. Finger splint
Physical and occupational therapy
Although general guidelines have been developed for the treatment of hand injuries, a review of the literature suggests that return-to-play guidelines are dependent on factors such as the severity of the initial injury, age, hand dominance, and the chronicity of injury, which vary with each individual 6.
Patients with stable distal interphalangeal dislocations may begin immediate active range-of-motion exercises. Unstable dorsal dislocations (which are less common) should be immobilized in 20° of flexion for 2-3 weeks before active range-of-motion exercises are begun. Complete collateral ligament injuries should be protected from lateral stress for at least 4 weeks.
Palmar distal interphalangeal dislocations may involve disruption of the insertion of the terminal extensor tendon as well as collateral ligaments and the palmar plate. Splinting the joint in extension for 8 weeks is required for the extensor tendon to heal. [3, 4, 5, 6, 20, 21, 22, 23, 24]
The duration and position of immobilization of proximal interphalangeal injuries depends on the structures involved and the severity of any disruptions. Dorsal proximal interphalangeal dislocations that are stable after reduction can generally be treated with buddy taping (see the first image below). This limits hyperextension, prevents recurrent dislocation, and allows a combination of active range-of-motion and gentle passive range-of-motion exercises. An alternative is the use of a dorsal aluminum foam splint.
In the case of a significant collateral ligament injury, the finger used as a splint should be on the side of the injured collateral ligament whenever possible. Uncomplicated proximal interphalangeal dislocations are usually immobilized in extension for 7-10 days. More serious injuries may be followed by up to 6 weeks of buddy-taped active range-of-motion. The patient should follow up within 2 weeks to confirm proper splinting and the absence of skin problems.
After closed reduction of dorsal proximal interphalangeal dislocations, immobilize the joint with a dorsally placed splint in 10-15° of flexion. Once the patient is comfortable, he or she can begin active flexion while in the splint. After 2 weeks, the splint can be discontinued and the finger buddy-taped for 2 more weeks.
Dorsal proximal interphalangeal dislocations that are unstable in extension (including fracture-dislocations) should be initially treated with extension block splinting at the angle required to keep the joint and the fracture (if present) reduced. This splint is often placed dorsally as an outrigger splint that is anchored in a short-arm cast and taped to the cast to maintain the flexion angle. The proximal phalanx must be immobilized (taped to the splint) to prevent the patient from achieving too much proximal interphalangeal extension by flexing the metacarpophalangeal joint while the middle and distal phalanges are left free.
A study by Waris et al 7 evaluated the outcomes of extension block pinning used to treat unstable dorsal fracture dislocations of the proximal interphalangeal joint. The study concluded that the extension block pinning technique is a simple and valuable technique for treating unstable dorsal proximal interphalangeal fracture-dislocation injuries producing satisfactory long-term results.
Volar dislocations with an intact extensor mechanism that are stable after reduction can usually be treated with buddy taping. If open reduction is required without extensive surgical repair, the joint can usually be immobilized for a few days and then buddy-taped.
Volar dislocations accompanied by central slip injury require splinting of the proximal interphalangeal joint in extension (with the distal interphalangeal joint left free), usually for 4-6 weeks, followed by daytime dynamic and nighttime static extension splinting for 2 weeks. The distal interphalangeal joint should be actively flexed throughout the entire recovery phase.
All of these injuries should be aggressively treated to minimize swelling. Routine elevation consists of propping the forearm and hand up on a pillow at night, wearing a sling, or consciously holding the arm up during the day. Ice is used as needed, especially during the first few days. Wrapping the finger with Coban tape can also be used to treat edema.
For patients seen early after dorsal metacarpophalangeal dislocations that are stable after reduction, rubber band extension block splinting (about 20°) for 2-3 weeks should be tried to prevent recurrence through hyperextension. Collateral ligament injuries should be immobilized in incomplete flexion (50°) for 3 weeks, followed by active range-of-motion with the digit buddy-taped to protect against lateral deviation stress. Additional physical therapy should be completed with modalities to prevent hand edema and maintain mobilization of all of the joints of the hand.
In carpometacarpal dislocations, the hand and wrist are frequently placed in an extension-type splint or cobra-type (extension) cast. Initial therapy should be directed at elevating the hand, decreasing the swelling, and mobilizing all of the stable joints of the hand.
With almost all of these injuries, early active range-of-motion exercises should be encouraged. This is relatively easy with injuries that have been treated with buddy taping or extension block splinting. In general, passive range-of-motion exercises have a very limited role in the early stages of treatment. The exception involves volar dislocations associated with central slip injuries, which call for aggressive active range-of-motion and passive range-of-motion exercises of the distal interphalangeal joint with the proximal interphalangeal joint in full extension; this helps to minimize both stiffness at the distal interphalangeal joint and adhesions between the 2 flexor tendons.
In the early stages of metacarpophalangeal and carpometacarpal dislocations, the role of occupational therapy is usually limited. However, aggressive mobilization of the fingers of the hand and the wrist joint should be carried out after the dislocation is stable and as early in the course of treatment as possible.
Surgical repair
Surgery is indicated for any open dislocation (irrigation and debridement) and any dislocation that is not reducible by closed means (open reduction).
When reduction by closed methods is unsuccessful, open reduction with removal of the soft tissue in the intra-articular space should be accomplished through a dorsal incision, and the metacarpal base articular surfaces should be fixed in appropriate positions with K-wires after being levered into the normal relationship with the carpus.
In situations where management is delayed and the metacarpal bases cannot be reduced, repositioning of the metacarpal bases is best accomplished by bony resection of the bases that overlap the carpus and pushing the bases into the normal relationship with the carpus.
Any joint that is grossly unstable or that cannot maintain reduction with buddy taping or extension block splinting may require repair of supporting structures (eg, the volar plate or collateral ligaments) to maintain the reduction. Volar dislocations accompanied by complete loss of extension at the proximal interphalangeal joint may require open reattachment of the central slip.
Distal interphalangeal injuries are considered chronic after 3 weeks. Chronically subluxated joints may have to be opened so that scar tissue can be resected to allow tension-free reduction.
Complex fracture-dislocations may require surgery for some combination of open reduction, internal fixation, and repair of supporting structures. External fixation (compass hinge) has been used on some complex proximal interphalangeal fracture-dislocations to provide distraction across the joint, maintain reduction, and allow controlled range of motion (ROM).
A number of procedures are possible to treat instability, stiffness, and fracture nonunions in and around the interphalangeal joints. Severe distal interphalangeal problems may be treated with arthrodesis, depending on the demands placed on the hand. However, this is not a good option for the proximal interphalangeal joint. Any procedure on the proximal interphalangeal joint is likely to result in some loss of range of motion. Therefore, compliance with occupational therapy is critical.
Recovery phase
In the recovery phase, stable hand injuries should continue to be treated with gentle active range-of-motion exercises and should not require extensive formal occupational therapy unless complications develop. Boutonniere injuries should be treated by early occupational therapy to ensure that range of motion exercises are done properly and often, as well as for splint fabrication and more aggressive range of motion when full-time immobilization is discontinued.
Occupational therapy is also important in most postoperative patients, in patients with fracture-dislocations, and in any patient whose injury begins to develop significant stiffness at any point in the course of recovery.
Several complications can arise during the recovery phase. At the first follow-up, the examiner should specifically look for recurrent instability or subluxation in the joint. Early boutonniere deformity (ie, hyperextension at the distal interphalangeal joint with fixed flexion at the proximal interphalangeal joint) is indicative of a central slip injury and often progresses to a disabling deformity without appropriate treatment.
Stiffness can occur in any of these injuries; this can be minimized in most cases by avoidance of excess immobilization and appropriate involvement of occupational therapy and hand surgery at an early stage in high-risk injuries.
In metacarpophalangeal and carpometacarpal dislocations, the same problems that are observed in the acute phase can be observed in the recovery phase. However, stiffness becomes a more predominant complication, and it can occur in any of the joints of the fingers, the metacarpophalangeal joints, and the carpometacarpal joints. Treatment involves aggressive occupational therapy to prevent joint ankylosis.
Follow up care
All patients with hand dislocations should follow up within 1 week to be checked for some of the more common complications 8. Dorsal proximal interphalangeal dislocations that initially appear stable may become subluxated with extension, requiring more aggressive treatment. Volar proximal interphalangeal dislocations may also lose reduction, or they may be associated with an occult central slip injury at initial presentation (usually reflected by tenderness over the insertion) that progresses to a complete rupture over the next few days.
Stiffness is a common complication at all stages of treatment, especially with PIP dislocations. The patient should perform gentle active range-of-motion exercises of any joint that does not require rigid immobilization. Resolution of stiffness and soreness may take as long as 12-18 months, and permanent residual enlargement of the joint is a possibility.
Collateral ligament injuries (usually radial) commonly accompany finger dislocations and usually respond well to closed treatment, with no significant long-term disability. However, the patient should be made aware that the pain from these injuries may take months (or even as long as a year) to resolve completely and that permanent enlargement of the joint is a common sequela.
Complications associated with metacarpophalangeal and carpometacarpal dislocations usually fit into the following 3 categories:
- Skin problems
- Recurrent subluxations or dislocations
- Stiffness or lack of motion of the joints
The patient should be monitored in the week following the dislocation to evaluate whether any posttraumatic skin ulceration, sloughing, or breakdown is present that may have to be treated with wound care or antibiotics. Early on, patients should undergo intermittent repeat radiography to verify that the reduction is maintained.
After appropriate immobilization, patients may show evidence of dislocation or subluxation of the extensor tendon to the radial or ulnar side of the metacarpophalangeal joints occupying a place between the 2 metacarpal heads. This is best treated by surgical intervention and proper repair of the torn extensor expansion with a row of interrupted sutures.
In long-term hand dislocation or recurrences, surgery is suggested to expose the joint dorsally and to perform a capsulectomy on either side of the metacarpophalangeal joint to achieve stable reduction. In some cases of acute metacarpophalangeal joint dislocation, the collateral ligament may rupture where it attaches to the tubercle of the metacarpal.
This collateral ligament rupture may lead to recurrent instability, but it can usually be treated nonoperatively, except when the rupture occurs on the radial side of the metacarpophalangeal joint of the little finger. In this case, the short abductor muscle of the little finger may pull it into ulnar deviation, necessitating operative repair.
Return to activity
In general, athletes with simple dorsal dislocations of the proximal interphalangeal joint may return to play with buddy taping or splinting as soon as the same game if a stable reduction is achieved; exceptions are players whose position places unusual demands on the finger (eg, quarterbacks or pitchers with an injury to the dominant hand).
Athletes with dorsal fracture-dislocations of the proximal interphalangeal joint and dislocations that are unstable in extension require a minimum of 3-4 weeks (the time during which extension block splinting is required) before return to play. Open reduction or volar plate repair necessitates 6 weeks away from sports.
Patients with volar proximal interphalangeal dislocations are more likely to be kept from rapid return by associated injuries and problems with reduction. Injury to the central slip of the extensor tendon is common with volar dislocations and necessitates splinting the distal interphalangeal joint in extension for approximately 6 weeks. If this does not interfere with function, the athlete may return to play, although ball handlers may have some difficulty with the splint.
Patients with volar dislocations requiring open reduction may return to play after a few days of immobilization if the central slip is intact. As with dorsal dislocations, if internal fixation or repair of structures around the joint is required, the athlete may be out for 6 weeks. Most distal interphalangeal dislocations should not require time away from play, except for a few days postoperatively if open reduction or irrigation and debridement is necessary.
Athletes with metacarpophalangeal joint or carpometacarpal joint dislocations generally remain out of sports for 6-8 weeks. This time includes a period for extension block splinting or extension cobra casting, as well a period for regaining full functional mobilization of the fingers, hand, and wrist with appropriate return of grip and wrist flexion and extension strength.
Hand dislocation prognosis
The majority of patients with uncomplicated hand dislocations should recover good function and do not require ongoing treatment in the maintenance phase. Most long-term complications of finger dislocations are related to either stiffness or instability. Stiffness, especially in the proximal interphalangeal joint, is initially best treated with intensive occupational therapy, but a hand surgeon should assess all significant contractures. Even if surgery is planned, the patient benefits the most if range of motion is maximized by means of dynamic splinting and exercise preoperatively.
Lateral instability is usually due to collateral ligament injury, instability in extension to volar plate injury, or a missed fracture 9. Most volar plate injuries heal with immobilization that prevents hyperextension (usually buddy taping); consequently, this complication is often preventable. Depending on the demands of the activity that caused the dislocation, the finger and specific structures involved, and the degree of instability, some of these problems may benefit from surgery.
- Bhargava A, Jennings AG. Simultaneous metacarpophalangeal joint ulnar collateral ligament injury and carpometacarpal dislocation of the thumb in a football player: a case report. Hand Surg. 2009. 14(1):23-4.[↩]
- Lefere M, Dallaudière B, Omoumi P, Cyteval C, Larbi A. Rare carpometacarpal dislocations. Orthop Traumatol Surg Res. 2016 Oct. 102 (6):813-6.[↩]
- Broadbent MR, Bach OS, Johnstone AJ. In situ rotational dislocation of the trapezoid associated with carpal-metacarpal dislocations. Hand Surg. 2009. 14(1):31-3.[↩]
- Inoue G, Maeda N. Irreducible palmar dislocation of the proximal interphalangeal joint of the finger. J Hand Surg [Am]. 1990 Mar. 15(2):301-4.[↩]
- de Haseth KB, Neuhaus V, Mudgal CS. Dorsal fracture-dislocations of the proximal interphalangeal joint: evaluation of closed reduction and percutaneous Kirschner wire pinning. Hand (N Y). 2015 Mar. 10 (1):88-93.[↩]
- Kovacic J, Bergfeld J. Return to play issues in upper extremity injuries. Clin J Sport Med. 2005 Nov. 15(6):448-52.[↩]
- Waris E, Mattila S, Sillat T, Karjalainen T. Extension Block Pinning for Unstable Proximal Interphalangeal Joint Dorsal Fracture Dislocations. J Hand Surg Am. 2016 Feb. 41 (2):196-202.[↩]
- Wilson RL, Liechty BW. Complications following small joint injuries. Hand Clin. 1986 May. 2(2):329-45.[↩]
- Kiefhaber TR, Stern PJ, Grood ES. Lateral stability of the proximal interphalangeal joint. J Hand Surg [Am]. 1986 Sep. 11(5):661-9.[↩]