What is haptoglobin
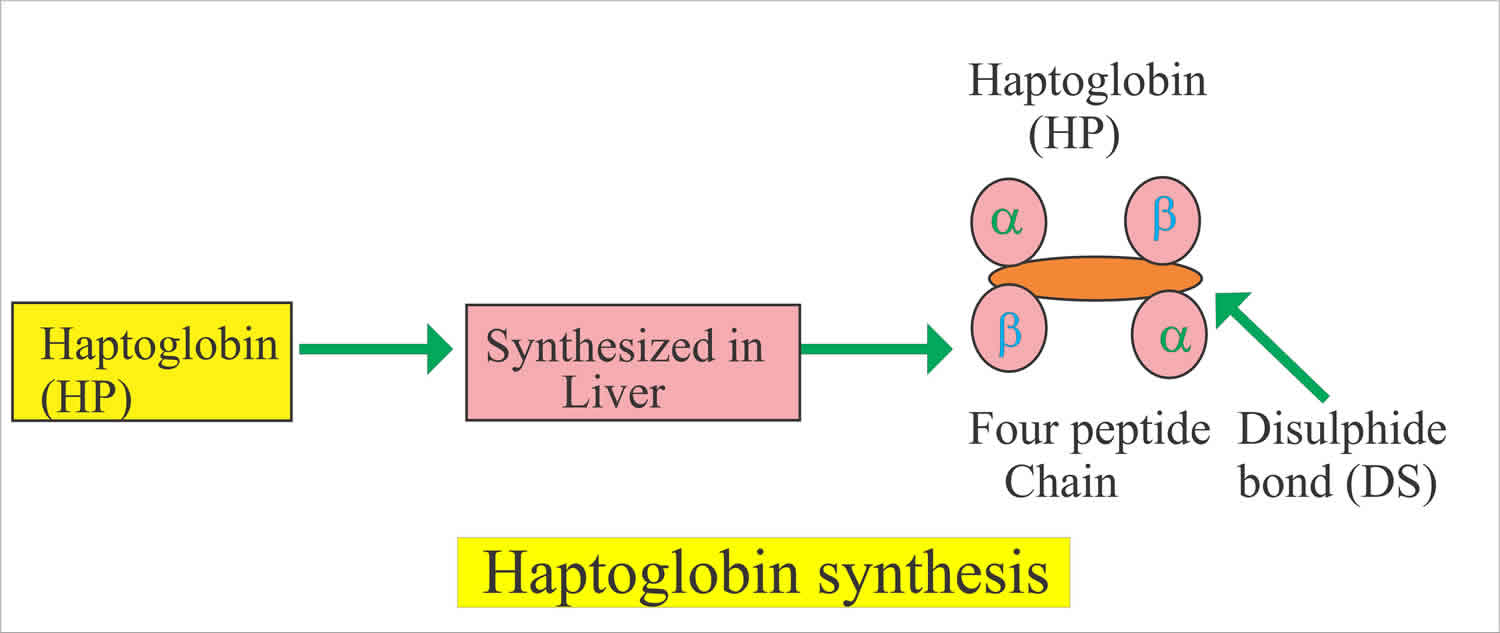
Haptoglobin is an immunoglobulin-like plasma protein produced by the liver that the body uses to clear free hemoglobin (found outside of red blood cells) from circulation. Haptoglobin is a plasma proteins with the highest binding affinities for hemoglobin (Hb) 1. Plasma-purified haptoglobin has been marketed in Japan since 1985, with primary indications for use in conjunction with extracorporeal circulation, massive transfusion, and thermal injury. The primary therapeutic effect of haptoglobin in disease states is protection of the kidneys from hemoglobin (Hb)-induced toxicity 2. Several United States– and European-based pharmaceutical companies have commenced development projects to fractionate haptoglobin (and hemopexin) from human plasma for use as therapeutics during hemolytic diseases 3. In 2011, a human plasma–derived haptoglobin was given orphan drug status for the treatment of sickle cell disease in the European Union 3. However, to date, preclinical proof of concept for haptoglobin (and hemopexin) has been studied within a general context of hemoglobin- and hemolysis-driven pathophysiology and not with the intention of treating a specific disease.
Hemoglobin is the iron-containing protein complex that transports oxygen throughout the body. Hemoglobin is normally found within red blood cells and very little is found free circulating in the blood. Haptoglobin binds to free hemoglobin in the blood. This forms a haptoglobin-hemoglobin complex that is rapidly removed from plasma by macrophages for degradation, the hemoglobin is catabolized and iron recycling. Haptoglobin renders hemoglobin (Hb) and heme relatively nonreactive 4 and deliver hemoglobin (Hb) to CD163 receptors on macrophages 5, for endocytosis and degradation of their heme moieties by heme oxygenase-1 (HO-1) 6. When the hemoglobin-binding capacity of haptoglobin is exceeded, hemoglobin passes through the renal glomeruli, resulting in hemoglobinuria.
When an increased number of red blood cells are damaged and/or break apart (hemolysis), they release their hemoglobin into the blood, increasing the amount of free hemoglobin in circulation. When large numbers of red blood cells are destroyed, haptoglobin concentrations in the blood will temporarily decrease as the haptoglobin is used up faster than the liver can produce it. A decrease in the amount of haptoglobin may be a sign that a person has a condition that is causing red blood cells to be destroyed or break apart. When the binding capacity of haptoglobin is exceeded, free hemoglobin level in circulation goes up and may cause tissue damage and organ dysfunction.
When hemoglobin is released from red blood cells within the physiologic range of haptoglobin, the potential deleterious effects of hemoglobin are prevented. However, during hyper-hemolytic conditions or with chronic hemolysis, haptoglobin is depleted and hemoglobin readily distributes to tissues where it might be exposed to oxidative conditions. In such conditions, heme can be released from ferric hemoglobin. The free heme can then accelerate tissue damage by promoting peroxidative reactions and activation of inflammatory cascades. Hemopexin is another plasma glycoprotein able to bind heme with high affinity. Hemopexin is a heme-binding plasma glycoprotein that forms the second line of defense against intravascular hemolysis associated with heme release from hemoglobin-Fe3+. Hemopexin sequesters heme in an inert, non-toxic form and transports it to the liver for catabolism and excretion. Like haptoglobin levels, hemopexin plasma levels are generally depleted in conditions with intravascular hemolysis, suggesting that supplementation of the plasma protein might provide some benefit to patients 7. However, no hemopexin product is available at a quality that would allow more extensive in vivo studies beyond murine models. Therefore, expanded studies with hemopexin treatment may not be possible in the near future for larger animal models of relevant clinical conditions such as blood transfusion or coronary artery bypass grafting and extracorporeal circulation.
Figure 1. Summary of intravascular/extravascular hemoglobin/heme clearance and cellular/tissue distribution
 Footnote: The main components of the hemoglobin (Hb)/heme detoxification system are haptoglobin (Hp), which sequesters hemoglobin (Hb) in the oxidatively protected Hb-Hp complex and hemopexin (Hx). The haptoglobin-hemoglobin complex is cleared and metabolized by CD163+ macrophages. Alternatively, during more severe hemolysis, free heme—after release from ferric hemoglobin (Hb)—can be detoxified by the hemopexin (Hx) rescue pathway. In all scenarios heme is finally detoxified by the heme oxygenases, which provide free iron for export by ferroportin or, alternatively, storage in the ferritin complex. The physiologic clearance and detoxification organs for hemoglobin (Hb)/heme are the liver and spleen, respectively, while the primary targets of hemoglobin (Hb)/heme toxic activities are the vascular endothelium and the kidney.
[Source 8 ]
Footnote: The main components of the hemoglobin (Hb)/heme detoxification system are haptoglobin (Hp), which sequesters hemoglobin (Hb) in the oxidatively protected Hb-Hp complex and hemopexin (Hx). The haptoglobin-hemoglobin complex is cleared and metabolized by CD163+ macrophages. Alternatively, during more severe hemolysis, free heme—after release from ferric hemoglobin (Hb)—can be detoxified by the hemopexin (Hx) rescue pathway. In all scenarios heme is finally detoxified by the heme oxygenases, which provide free iron for export by ferroportin or, alternatively, storage in the ferritin complex. The physiologic clearance and detoxification organs for hemoglobin (Hb)/heme are the liver and spleen, respectively, while the primary targets of hemoglobin (Hb)/heme toxic activities are the vascular endothelium and the kidney.
[Source 8 ]Increased red blood cell destruction may be due to inherited or acquired conditions. Some examples include transfusion reactions, certain drugs, and mechanical breakage, such as may be seen with some prosthetic heart valves. The destruction may be mild or severe, occurring suddenly (acute) or developing and lasting over a long period of time (chronic), and it can lead to hemolytic anemia. People with hemolytic anemia may experience symptoms such as fatigue, weakness, and shortness of breath and their skin may be pale or jaundiced.
Liver disease may also result in decreased haptoglobin concentrations as liver damage may inhibit both the production of haptoglobin and the clearing of the haptoglobin-free hemoglobin complexes.
Haptoglobin is considered an “acute-phase” protein; this means that haptoglobin will be elevated in many inflammatory diseases, such as ulcerative colitis, acute rheumatic disease, heart attack, and severe infection. Of a person has one of these conditions, it can complicate the interpretation of the haptoglobin results. Haptoglobin testing is not generally used to help diagnose or monitor these conditions.
Figure 2. Haptoglobin and hemolysis
Figure 3. Summary of the hemoglobin (Hb) clearance compartments and the main acute and chronic pathologies that can be associated with intravascular hemolysis. The availability of the hemoglobin (Hb) and heme scavenger proteins haptoglobin (Hp) and hemopexin (Hx) shifts the physiologic balance from tissue damage toward protection.
[Source 9 ]Haptoglobin function
Haptoglobin fundamentally changes the biochemical and physiologic profile of free hemoglobin (Hb) 10. When bound within the large molecular size haptoglobin:hemoglobin complex (> 150 kDa), Hemoglobin (Hb) remains sequestered within the intravascular space and its translocation into the kidney and across the endothelial layer appears to be prevented. This simple mechanism keeps potentially adverse biochemical reactions of the free hemoglobin (Hb) with nitric oxide and/or peroxides away from the most susceptible anatomic sites such as the vascular wall. Intravascular sequestration appears to be the most effective way by which haptoglobin prevents hemoglobin (Hb)-induced hypertension and renal damage. In addition, hemoglobin (Hb) remains contained within the reducing (i.e., antioxidant-rich) environment of the blood plasma until monocyte and macrophage clearance is complete.
Recent in vitro experiments suggest that haptoglobin may also alter hemoglobin’s oxidative reactions. Haptoglobin decreases the redox potential of bound hemoglobin-Fe3+, stabilizes the higher oxidation state of hemoglobin-Fe4+, and prevents radical transfer to non-hemoglobin (Hb) molecules in the presence of oxidants 11. The recently resolved crystal structure of the porcine haptoglobin-hemoglobin complex provided some structural basis for the protection of critical amino acids that are primary targets of globin oxidation 12. As a result of this protection, globin oxidation with subsequent protein degradation does not occur when hemoglobin (Hb) is sequestered in the haptoglobin-hemoglobin complex 13. The structural stability of the complex may prevent accumulation of proinflammatory hemoglobin (Hb)-degradation products that can evade clearance by scavenger receptors 14. In addition, hemin resides firmly in the haptoglobin-hemoglobin complex, it cannot transfer to hemin acceptors such as haptoglobinx, lipoproteins, and albumin 15. Therefore, the prevention of heme transfer is another essential mechanism by which haptoglobin protects against hemoglobin (Hb)-driven oxidation of membrane lipids and plasma lipoproteins, preventing the accumulation of free heme.
A human plasma–derived haptoglobin product was developed by the Japanese Green Cross (now Benesis Corporation) and was approved in 1985 for the treatment of hemolysis due to extracorporeal circulation, burn injuries, and trauma with massive blood transfusions 9. Subsequent findings of several small-scale studies indicated that haptoglobin supplementation could prevent renal tubular damage during open-heart surgery with cardiopulmonary bypass, HELLP (hemolysis elevated liver enzymes low platelets) syndrome, and after hemolysis complicating endoscopic injection sclerotherapy of esophageal varices with ethanolamine-oleate 9. Case reports and studies in a limited number of patients further support the successful use of haptoglobin in patients with hemolytic anemias (i.e., thalassemia and glucose-6-phosphate dehydrogenase deficiency [G6PD]), severe burn injury, in patients with hemolysis resulting from accidental ABO-incompatible red blood cell transfusion, and as a prophylaxis or treatment for hemolysis after ABO-mismatched bone marrow transplantation. The primary clinical criteria for haptoglobin administration and dosing in these studies were the appearance and reversal of hemoglobinuria with the intent of limiting renal injury. The reported doses of haptoglobin that were administered for treating acute hemolytic conditions were approximately 2 g to > 10 g per patient, with dosing schedules of repeated 2 g (children) or 4 g (adults) boluses. The cost for the haptoglobin therapeutic in Japan is currently at $540 USD per 2-g bolus. There is so far no reported use of haptoglobin in chronic hemolytic conditions in which repeated dosing over a longer treatment period might be necessary to effectively suppress free plasma hemoglobin (Hb) levels.
Haptoglobin test
Haptoglobin test measures the amount of haptoglobin in the blood. Haptoglobin testing is used primarily to help detect and evaluate hemolytic anemia and to distinguish it from anemia due to other causes. Haptoglobin testing is used to help determine whether red blood cells (RBCs) are breaking apart or being destroyed prematurely. Haptoglobin test may be used in conjunction with other laboratory tests such as a complete blood count (CBC, including red blood cell count, hemoglobin, hematocrit), reticulocyte count, lactate dehydrogenase, bilirubin, direct antiglobulin test, and blood smear.
Hemolytic anemia is an uncommon cause of anemia. The condition can be inherited or may develop during a person’s lifetime (acquired) due to various factors and may develop suddenly or develop over time.
Though the haptoglobin test is a sensitive test for hemolytic anemia, it cannot be used to diagnose the cause of the condition. Other laboratory tests may be needed to help determine the cause, such as tests for autoantibodies to detect autoimmune causes, sickle cell tests, G6PD, or a hemoglobin evaluation.
A haptoglobin test may be ordered along with a direct antiglobulin test to help determine whether someone who has received a blood transfusion has had a transfusion reaction.
If a haptoglobin level is low, then testing may be repeated at a later time to evaluate changes in concentration and help determine whether the increased destruction of red blood cells is no longer occurring or continues.
Should everyone have a haptoglobin test?
No, this is not a test that is used for general screening. Most people will never need to have a haptoglobin test performed.
Can I have the haptoglobin test done in my healthcare practitioner’s office?
In most cases, no. This test is typically either performed in a hospital laboratory or sent to a reference laboratory.
When is haptoglobin test ordered?
The haptoglobin test is ordered when someone has symptoms and signs associated with hemolytic anemia. Some signs and symptoms include:
- Fatigue, weakness
- Pale skin (pallor)
- Fainting
- Shortness of breath
- A rapid heart rate
- Jaundice
- Red or brown urine (from the presence of blood/hemoglobin)
Haptoglobin testing may also be done when other laboratory test results are consistent with hemolytic anemia. These may show increased bilirubin concentrations (bulirubinemia), hemoglobin in the urine (hemoglobinuria), decreased red blood cell count, and increased reticulocyte count and lactate dehydrogenase levels.
Haptoglobin level
Normal haptoglobin level
- 30-200 mg/dL
- A low level of haptoglobin is normal for newborns and infants of less than 6 months old.
What does abnormal haptoglobin test result mean?
Haptoglobin levels may be affected by massive blood loss and by conditions associated with kidney dysfunction as well as liver disease. Results are interpreted carefully and in conjunction with results of other tests, such as a reticulocyte count, red blood cell (RBC) count, hemoglobin (Hb), hematocrit (Hct), or complete blood count (CBC).
When a haptoglobin level is significantly decreased, along with an increased reticulocyte count and a decreased red blood cell count, hemoglobin, and hematocrit, then it is likely that the person has some degree of hemolytic anemia with red blood cells destroyed in the circulation (so-called intravascular hemolysis).
If the haptoglobin is normal or borderline normal and the reticulocyte count is increased, then red blood cell destruction is likely occurring in organs such as the spleen and liver (so-called extravascular hemolysis). Because the freed hemoglobin is not released into the blood, the haptoglobin is not consumed and so is at a normal level. However, in severe extravascular hemolysis, haptoglobin level can be low because excess hemolysis can release some free hemoglobin into circulation.
If the haptoglobin concentration is normal and the reticulocyte count is not increased, then it is likely that the anemia present is not due to red blood cell breakdown.
Table 1. Haptoglobin levels that may be seen:
| Haptoglobin | Reticulocyte count | RBC count, Hemoglobin, Hematocrit | Possible interpretation |
| Significantly decreased | Increased | Decreased | Red blood cells are being destroyed within blood vessels (i.e., intravascular hemolysis) |
| Normal or slightly decreased | Increased | Decreased | Red blood cells destruction likely within organs such as spleen and liver (i.e., extravascular hemolysis) |
| Normal | Not increased | Decreased | Anemia due to a cause other than red blood cell destruction (e.g., decrease in red blood cell production in the bone marrow) |
Low haptoglobin
Low levels of plasma haptoglobin may indicate intravascular hemolysis. Absence of plasma haptoglobin may therefore indicate intravascular hemolysis. However, congenital anhaptoglobinemia is common, particularly in African-Americans. For this reason, it may be difficult or impossible to interpret a single measurement of plasma haptoglobin. If the haptoglobin value is low, the haptoglobin test should be repeated after 1 to 2 weeks following an acute episode of hemolysis. If all the plasma haptoglobin is removed following an episode of intravascular hemolysis, and if hemolysis ceases, the haptoglobin concentration should return to normal in a week.
Chronic intravascular hemolysis causes persistently low haptoglobin concentration. Regular strenuous exercise may cause sustained low haptoglobin, presumably from low-grade hemolysis. Low serum haptoglobin may also be due to severe liver disease.
Neonatal plasma or serum specimens usually do not contain measurable haptoglobin. Low haptoglobin is normal for the first 3 to 6 months of life. Adult levels are achieved by 6 months.
If haptoglobin is decreased without any signs of hemolytic anemia, then it is possible that the liver is not producing adequate amounts of haptoglobin. This may be seen with liver disease, although haptoglobin is not typically used to diagnose or monitor liver disease.
Drugs that can decrease haptoglobin concentrations include isoniazid, quinidine, streptomycin, and birth control pills.
If haptoglobin levels are decreased, when will they return to normal?
It depends on the cause of low haptoglobin. If they are due to acute hemolysis, such as may be seen with a transfusion reaction, then they will return to normal once the donor blood has been cleared from the system. If they are due to chronic hemolysis, then the concentration should return to normal if and when the underlying condition can be resolved. If the underlying condition cannot be resolved or if the decreased concentrations of haptoglobin are due to decreased production due to liver disease, then levels may continue to be lower than normal.
Elevated haptoglobin
Haptoglobin is an acute-phase reactant and increases with inflammation or tissue necrosis. Increase in plasma haptoglobin concentration occurs as an acute-phase reaction. Levels may appear to be increased in conditions such as burns and nephrotic syndrome. An acute-phase response may be confirmed and monitored by assay of other acute-phase reactants such as alpha-1-antitrypsin and C-reactive protein (CRP).
Drugs that can increase haptoglobin levels include androgens and corticosteroids.
- Belcher JD, Chen C, Nguyen J, et al. Haptoglobin and hemopexin inhibit vaso-occlusion and inflammation in murine sickle cell disease: Role of heme oxygenase-1 induction. PLoS One. 2018;13(4):e0196455. Published 2018 Apr 25. doi:10.1371/journal.pone.0196455 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5919001/[↩]
- Hashimoto K, Nomura K, Nakano M, Sasaki T, Kurosawa H. Pharmacological intervention for renal protection during cardiopulmonary bypass. Heart Vessels 1993;8(4):203-210.[↩]
- Schaer, D. J., Buehler, P. W., Alayash, A. I., Belcher, J. D., & Vercellotti, G. M. (2013). Hemolysis and free hemoglobin revisited: exploring hemoglobin and hemin scavengers as a novel class of therapeutic proteins. Blood, 121(8), 1276-1284. Accessed November 06, 2018. https://doi.org/10.1182/blood-2012-11-451229.[↩][↩]
- Smith A, McCulloh RJ. Hemopexin and haptoglobin: allies against heme toxicity from hemoglobin not contenders. Front Physiol. 2015;6:187 Epub 2015/07/16. doi: 10.3389/fphys.2015.00187[↩]
- Kristiansen, M., Graversen, J. H., Jacobsen, C., Sonne, O., Hoffman, H. J., Law, S. K., et al. (2001). Identification of the haemoglobin scavenger receptor. Nature 409, 198–201. doi: 10.1038/35051594[↩]
- Thomsen JH, Etzerodt A, Svendsen P, Moestrup SK. The haptoglobin-CD163-heme oxygenase-1 pathway for hemoglobin scavenging. Oxid Med Cell Longev. 2013;2013:523652 Epub 2013/06/20. doi: 10.1155/2013/523652[↩]
- Muller-Eberhard U, Javid J, Liem HH, Hanstein A, Hanna M. Concentrations of hemopexin, haptoglobin and heme in patients with various hemolytic diseases. Blood 1968;32(5):811-815.[↩]
- Haptoglobin, hemopexin, and related defense pathways—basic science, clinical perspectives, and drug development. Front. Physiol., 28 October 2014 https://www.frontiersin.org/articles/10.3389/fphys.2014.00415/full[↩]
- Schaer, D. J., Buehler, P. W., Alayash, A. I., Belcher, J. D., & Vercellotti, G. M. (2013). Hemolysis and free hemoglobin revisited: exploring hemoglobin and hemin scavengers as a novel class of therapeutic proteins. Blood, 121(8), 1276-1284. Accessed November 06, 2018. https://doi.org/10.1182/blood-2012-11-451229[↩][↩][↩]
- Boretti FS, Buehler PW, D’Agnillo F, et al. Sequestration of extracellular hemoglobin within a haptoglobin complex decreases its hypertensive and oxidative effects in dogs and guinea pigs. J Clin Invest 2009;119(8):2271-2280.[↩]
- Cooper CE, Schaer DJ, Buehler PW, et al. Haptoglobin binding stabilizes hemoglobin ferryl iron and the globin radical on tyrosine beta145 [published online ahead of print August 2012]. Antioxid Redox Signal. doi:10.1089/ars.2012.457[↩]
- Andersen CB, Torvund-Jensen M, Nielsen MJ, et al. Structure of the haptoglobin-haemoglobin complex. Nature 2012;489(7416):456-459.[↩]
- Pimenova T, Pereira CP, Gehrig P, Buehler PW, Schaer DJ, Zenobi R. Quantitative mass spectrometry defines an oxidative hotspot in hemoglobin that is specifically protected by haptoglobin. J Proteome Res 2010;9(8):4061-4070.[↩]
- Buehler PW, Vallelian F, Mikolajczyk MG, et al. Structural stabilization in tetrameric or polymeric hemoglobin determines its interaction with endogenous antioxidant scavenger pathways. Antioxid Redox Signal 2008;10(8):1449-1462.[↩]
- Bunn HF, Jandl JH. Exchange of heme among hemoglobins and between hemoglobin and albumin. J Biol Chem 1968;243(3):465-475.[↩]