What is a head injury
A head injury is any trauma to the scalp, skull, or brain. Head injury may be only a minor bump on the skull or a serious brain injury. Some common causes of head injuries are falls, motor vehicle accidents, violence, and sports injuries.
Head injury can be open or closed:
- A closed head injury means you received a hard blow to the head from striking an object, but the object did not break the skull.
- With an open head injury or penetrating injury, an object pierces the skull and enters the brain. This is more likely to happen when you move at high speed, such as going through the windshield during a car accident. It can also happen from a gunshot to the head.
Closed head injuries are not always less severe than open head injuries.
Head injuries include:
- Concussion, in which the brain is shaken, is the most common type of traumatic brain injury (TBI) that alters the way the brain functions. Concussion is a minor head injury caused by force to the head. Concussion may or may not be associated with loss of consciousness (blackout). Effects of concussion are usually temporary, but can include altered levels of consciousness, headaches, confusion, dizziness, memory loss of events surrounding the injury, and visual disturbance. Most people who have concussion will recover on their own within 2 weeks, but complications can occur. It is important that people with concussion rest and that their recovery is monitored.
- Scalp wounds.
- Skull fractures.
Loss of consciousness – when a person is unable to open their eyes, speak or follow commands. They have no awareness of stimulation from outside their body and cannot remember the immediate periods before and after the injury.
Head injuries may cause bleeding:
- In the brain tissue
- In the layers that surround the brain (subarachnoid hemorrhage, subdural hematoma, extradural hematoma)
Head injury is a common reason for an emergency room visit. A large number of people who suffer head injuries are children. Traumatic brain injury (TBI) accounts for over 1 in 6 injury-related hospital admissions each year.
Most head injury is minor because your skull is hard and it protects your brain. But other head injuries can be more severe, such as a skull fracture, concussion, or traumatic brain injury.
The most common causes of serious head injuries are:
- car accidents
- sports injuries
- accidents at home, such as slips, falls or trips
- accidents at work, such as falls or being hit on the head
- assaults.
Even in a mild head injury there is a small risk of you developing serious complications so you should be watched closely by another adult for 24 hours after the accident. If you show any of these symptoms or signs after your head injury, or you get worse, go to the nearest hospital, doctor or telephone an ambulance immediately.
Learning to recognize a serious head injury and give basic first aid can save someone’s life. For a moderate to severe head injury, your local emergency services number and ask for an ambulance.
It is important to know the warning signs of a moderate or severe head injury. Get help immediately if the injured person has:
- A constant headache that gets worse or does not go away
- Repeated vomiting or nausea
- Convulsions or seizures
- An inability to wake up
- Dilated (enlarged) pupil in one or both eyes
- Slurred speech
- Weakness or numbness in the arms or legs
- Loss of coordination
- Increased confusion, restlessness, or agitation
- Fainting or drowsiness – or you can’t wake up
- Acting strange, saying things that do not make sense (change in behavior)
- Cannot remember new events, recognize people or places (increased confusion)
- Pass out or have a blackout or a seizure (any jerking of the body or limbs)
- Cannot move parts of your body or clumsiness
- Blurred vision or slurred speech
- Continual fluid or bleeding from the ear or nose
- There is severe head or face bleeding.
- The person is confused, tired, or unconscious.
- The person stops breathing.
- You suspect a serious head or neck injury, or the person develops any signs or symptoms of a serious head injury.
Doctors use a neurologic exam and imaging tests to make a diagnosis. Treatment depends on the type of injury and how severe it is.
A serious head injury can cause anything from nausea to concussion to bleeding to death.
If you have a fit or seizure or fall unconscious, even if its only for a second, you should call your local emergency services number and ask for an ambulance.
If you are bleeding and it won’t stop, or if you have fluid coming from your nose or ears, you should call your local emergency services number and ask for an ambulance.
Head Injury in Children
Children who have had a head injury may develop symptoms at various times. Some of the symptoms may begin minutes or hours after the initial injury, while others may take days or weeks to show up.
- Call an ambulance immediately if you have any difficulty waking your child.
If your child experiences any of the following symptoms, take them to the doctor or nearest hospital emergency department immediately:
- vomiting more than once
- bleeding or any discharge from the ear or nose
- fits/seizures/twitching/convulsions
- blurred or double vision
- poor coordination or clumsiness
- any new arm or leg weakness, or any existing weakness that gets worse or does not improve
- difficulty swallowing or coughing when eating or drinking
- sensitivity to noise
- slurred or unclear speech
- unusual or confused behavior
- severe or persistent headache that is not relieved by paracetamol.
If your child has had a head injury, they should return to school and sport gradually. For moderate to severe head injuries, your doctor will advise you.
First Aid
After calling your local emergency services number and ask for an ambulance. Then take the following steps:
- Check the person’s airway, breathing, and circulation. If necessary, begin rescue breathing and CPR.
- If the person’s breathing and heart rate are normal, but the person is unconscious, treat as if there is a spinal injury. Stabilize the head and neck by placing your hands on both sides of the person’s head. Keep the head in line with the spine and prevent movement. Wait for medical help.
- Stop any bleeding by firmly pressing a clean cloth on the wound. If the injury is serious, be careful not to move the person’s head. If blood soaks through the cloth, do not remove it. Place another cloth over the first one.
- If you suspect a skull fracture, do not apply direct pressure to the bleeding site, and do not remove any debris from the wound. Cover the wound with sterile gauze dressing.
- If the person is vomiting, to prevent choking, roll the person’s head, neck, and body as one unit onto their side. This still protects the spine, which you must always assume is injured in the case of a head injury. Children often vomit once after a head injury. This may not be a problem, but call a doctor for further guidance.
- Apply ice packs to swollen areas.
Follow these precautions
DO NOT
- DO NOT wash a head wound that is deep or bleeding a lot.
- DO NOT remove any object sticking out of a wound.
- DO NOT move the person unless absolutely necessary.
- DO NOT shake the person if he or she seems dazed.
- DO NOT remove a helmet if you suspect a serious head injury.
- DO NOT pick up a fallen child with any sign of head injury.
- DO NOT drink alcohol within 48 hours of a serious head injury.
A serious head injury that involves bleeding or brain damage must be treated in a hospital.
For a mild head injury, no treatment may be needed. However, watch for symptoms of a head injury, which can show up later.
Your health care provider will explain what to expect, how to manage any headaches, how to treat your other symptoms, when to return to sports, school, work, and other activities, and signs or symptoms to worry about.
- Children will need to be watched and make activity changes.
- Adults also need close observation and activity changes.
Both adults and children must follow the provider’s instructions about when it will be possible to return to sports.
Key points to remember
- Head injuries can be mild, moderate or severe.
- Call an ambulance if you or your child has had head injury involving high speeds or heights, or if after a knock to the head they lose consciousness or vomit more than once.
- Your child may develop a number of different symptoms in the weeks after a head injury. Many of these require immediate medical attention.
- Children with cognitive fatigue need complete rest to recover.
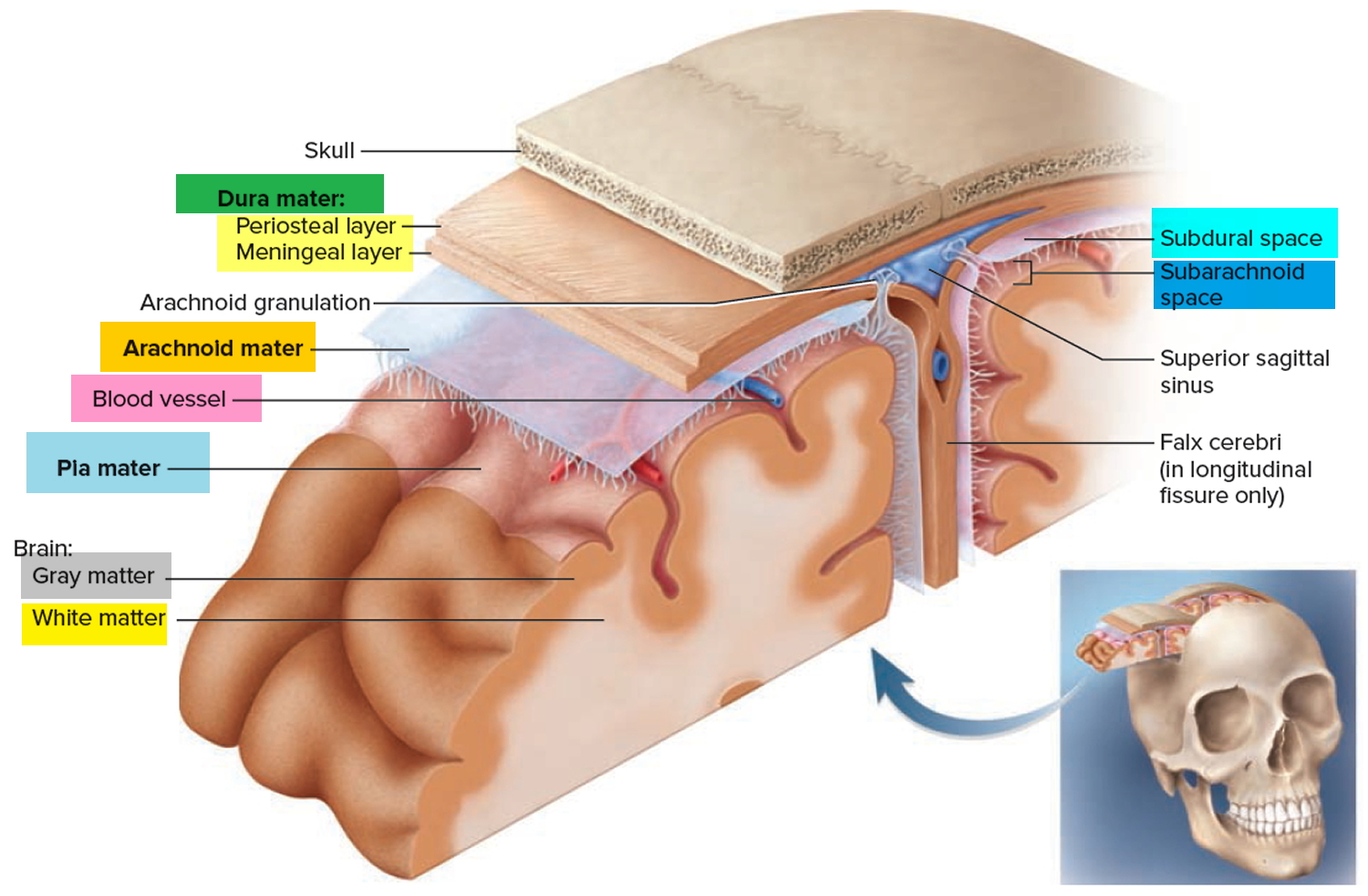
Figure 1. Skull and human brain
Types of head injury
The following are some of the different types of head injuries:
Concussion. A concussion is an injury to the head area that may cause instant loss of awareness or alertness for a few minutes up to a few hours after the traumatic event.
Skull fracture. A skull fracture is a break in the skull bone. There are four major types of skull fractures, including the following:
- Linear skull fractures. This is the most common type of skull fracture. In a linear fracture, there is a break in the bone, but it does not move the bone. These patients may be observed in the hospital for a brief amount of time, and can usually resume normal activities in a few days. Usually, no interventions are necessary.
- Depressed skull fractures. This type of fracture may be seen with or without a cut in the scalp. In this fracture, part of the skull is actually sunken in from the trauma. This type of skull fracture may require surgical intervention, depending on the severity, to help correct the deformity.
- Diastatic skull fractures. These are fractures that occur along the suture lines in the skull. The sutures are the areas between the bones in the head that fuse when we are children. In this type of fracture, the normal suture lines are widened. These fractures are more often seen in newborns and older infants.
- Basilar skull fracture. This is the most serious type of skull fracture, and involves a break in the bone at the base of the skull. Patients with this type of fracture frequently have bruises around their eyes and a bruise behind their ear. They may also have clear fluid draining from their nose or ears due to a tear in part of the covering of the brain. These patients usually require close observation in the hospital.
Intracranial hematoma (ICH). There are several types of ICH, or blood clots, in or around the brain. The different types are classified by their location in the brain. These can range from mild head injuries to quite serious and potentially life-threatening injuries. The different types of ICH include the following:
- Epidural hematoma. Epidural hematomas occur when a blood clot forms underneath the skull, but on top of the dura, the tough covering that surrounds the brain. They usually come from a tear in an artery that runs just under the skull called the middle meningeal artery. Epidural hematomas are usually associated with a skull fracture.
- Subdural hematoma. Subdural hematomas occur when a blood clot forms underneath the skull and underneath the dura, but outside of the brain. These can form from a tear in the veins that go from the brain to the dura, or from a cut on the brain itself. They are sometimes, but not always, associated with a skull fracture.
- Contusion or intracerebral hematoma. A contusion is a bruise to the brain itself. A contusion causes bleeding and swelling inside of the brain around the area where the head was struck. Contusions may occur with skull fractures or other blood clots such as a subdural or epidural hematoma. Bleeding that occurs inside the brain itself (also called intraparenchymal hemorrhage) can sometimes occur spontaneously. When trauma is not the cause, the most common causes are long-standing, high blood pressure in older adults, bleeding disorders in either children or adults, or the use of medications that cause blood thinning or certain illicit drugs.
- Diffuse axonal injury. These injuries are fairly common and are usually caused by shaking of the brain back and forth, which can happen in car accidents, from falls or shaken baby syndrome. Diffuse injuries can be mild, such as with a concussion, or may be very severe, as in diffuse axonal injury. In diffuse axonal injury, the patient is usually in a coma for a prolonged period of time, with injury to many different parts of the brain.
Head injury in children and babies
Children and adolescence often bump or bang their heads, and it can be difficult to tell whether a head injury is serious or not. Any knock to the head is considered a head injury.
Head injuries are classified as mild, moderate or severe. Many head injuries are mild, and simply result in a small lump or bruise. Mild head injuries can be managed at home, but if your child has received a moderate or severe injury to the head, they need to see a doctor.
When there is a direct blow to the head, shaking of the child (as seen in many cases of child abuse), or a whiplash-type injury (as seen in motor vehicle accidents), the bruising of the brain and the damage to the internal tissue and blood vessels is due to a mechanism called coup-countrecoup. A bruise directly related to trauma, at the site of impact, is called a coup lesion. As the brain jolts backwards, it can hit the skull on the opposite side and cause a bruise called a countrecoup lesion. The jarring of the brain against the sides of the skull can cause tearing of the internal lining, tissues, and blood vessels that may cause internal bleeding, bruising, or swelling of the brain.
Also it’s always best to see a doctor if you’re unsure. Sometimes, a child might look normal, but be behaving abnormally. Sometimes symptoms can take 24-48 hours to appear.
Most head injuries are mild and not associated with brain injury or long-term complications. Very rarely, children with more significant injuries may develop serious complications (e.g, brain injury or bleeding around the brain).
A brain injury or head trauma happens when the brain is swollen, torn, stretched, shaken, compressed, bruised or pierced. These injuries range from very mild to life-threatening. Having brain damage can cause a range of disabilities, affecting how a child moves, thinks, feels or behaves.
The parent(s) of a child/adolescent with a head injury should work with their child’s healthcare provider to determine if the child needs to be evaluated, how to monitor for signs or symptoms of worsening, and develop a plan for minimizing the risk of future injuries.
Head injury causes in children and babies
Falls are the most common cause of minor head injury in children and adolescents, followed by motor vehicle crashes, pedestrian and bicycle accidents, sports-related trauma, and child abuse. The risk of brain injury varies with the severity of the trauma.
Low force injuries (e.g, short falls, hit by low speed or soft object such as toy or ball) have a low risk of brain injury.
In comparison, incidents that have a higher risk of brain injury include:
- High speed motor vehicle accidents
- Falls from great heights
- Being hit by a high speed, heavy, or sharp object (eg, baseball bat, golf club, bullet, knife)
- Inflicted injury (abuse), such as vigorous shaking, typically causes severe injury
Head injury symptoms in children and babies
A child’s behavior and symptoms after a head injury depend upon the type and extent of the head injury. The most common signs and symptoms include:
- Scalp swelling – Scalp swelling is common because there are many blood vessels in the scalp. If the skin is not broken, it is common to develop a large lump from bleeding or swelling under the skin.
- Loss of consciousness – Only about 5 percent of children/adolescents with a mild head injury pass out (lose consciousness), usually just for a brief period (less than one minute).
- Headache – Headache occurs in about 45 percent of children/adolescents after head injury. In children who are too young to speak, irritability may be an indication of headache or other discomfort.
- Vomiting – Approximately 10 percent of children/adolescents have at least one episode of vomiting after a head injury. Children who vomit after a head injury do not necessarily have a serious brain injury.
- Seizures – Less than one percent of children/adolescents have a seizure immediately after a head injury. A few of these children have a serious head injury. A CT scan of the head is usually recommended in this situation.
- Concussion – The term concussion is used to describe a mild form of traumatic brain injury. Common symptoms of a concussion include confusion, amnesia (not being able to remember events around the time of the injury), headache, vomiting, and dizziness. Loss of consciousness may occur but is uncommon, occurring in about 10 percent of young athletes with concussions.
Some closed (internal) head injuries can be serious and possibly life-threatening. These include a broken skull bone, torn blood vessels, or damage to the brain itself.
- However, it can be hard to know how serious a head injury is, even for experienced physicians, so it’s always wise to call your local emergency services number and ask for an ambulance.
Call your local emergency services number and ask for an ambulance if your child is an infant; has lost consciousness, even briefly; or if a child of any age has any of these symptoms:
- won’t stop crying
- complains of head and neck pain (younger or nonverbal children may be more fussy)
- vomits several times
- won’t awaken easily
- becomes hard to console
- isn’t walking or talking normally
- unconsciousness for more than a few seconds
- abnormal breathing
- obvious serious wound
- bleeding or clear fluid from the nose, ear, or mouth
- disturbance of speech or vision
- pupils of unequal size
- weakness or paralysis
- weak, numb or tingling arms, legs or face
- neck pain or stiffness
- seizure
- seeming confused or acting oddly
- a loss of memory
- persistent or recurrent headache
- losing balance or feeling dizzy
- you’re concerned
If your child is UNCONSCIOUS:
- DO NOT try to move your child in case there is a neck or spine injury.
- Call for help.
- Turn a child who is vomiting or having a seizure onto his or her side while trying to keep the head and neck straight. This will help prevent choking and provide protection in case of neck and spine injury.
If your child is conscious:
- Do your best to keep your child calm and still.
- If there’s bleeding, apply a clean or sterile bandage.
- Do not attempt to cleanse the wound, which can make bleeding worse and/or cause serious complications if the skull is fractured.
- Do not apply direct pressure to the wound if you suspect the skull is fractured.
- Do not remove any object that’s stuck in the wound.
If your child is not an infant, has not lost consciousness, and is alert and behaving normally after the fall or blow:
- Apply an ice pack or instant cold pack to the injured area for 20 minutes every 3 to 4 hours. If you use ice, always wrap it in a washcloth or sock; ice applied directly to bare skin can injure it.
- Watch your child carefully for the next 24 hours. If you notice any of the signs of internal injury, call your doctor right away.
- If the incident happens close to bedtime or naptime and your child falls asleep soon afterward, check in a few times while he or she sleeps.
- If color and breathing are normal, and you don’t sense a problem, let your child sleep (unless the doctor has advised otherwise). There’s no need to keep a child awake after a head injury.
- Trust your instincts. If you aren’t comfortable with your child’s appearance, partly awaken your child by sitting him or her up. Your child should fuss a bit and attempt to resettle. If he or she still seems very drowsy, try to awaken your child fully. If your child can’t be awakened or shows any signs of internal injury, call the doctor or call your local emergency services number for an ambulance.
Head injury tests
Many parents wonder if their child/adolescent needs medical attention after a head injury. The American Academy of Pediatrics recommends that parents contact their child’s healthcare provider for advice for anything more than a light bump on the head.
Children with any of the following symptoms need to be evaluated by a healthcare provider since these symptoms may indicate a higher risk of complications. Depending upon the particular circumstances, this may be done at the pediatrician’s office or in an emergency department:
- If the child has recurrent vomiting
- If the child has a seizure (convulsion)
- If the child loses consciousness after the injury
- If the child develops a headache that is severe or worsens with time
- If there are changes in the child’s behavior (eg, lethargic, difficult to wake, extremely irritable, or exhibiting other abnormal behavior)
- If the child stumbles, or difficulty walking, clumsiness, or lack of coordination
- If the child is confused or has slurred speech
- If the child has dizziness that does not resolve or recurs repeatedly
- If blood or watery fluid oozes from the nose or ears
- If the child is younger than six months of age
- If a cut will not stop bleeding after applying pressure for 10 minutes
- If the child fell from a height greater than three to five feet, was hit with a high speed object, or was hit with great force
- If the parent/caregiver is concerned about how the child is acting
The goal of the evaluation is to determine if there is serious brain injury. The evaluation can also determine if the child needs immediate treatment, close follow up, or further testing (e.g, computed tomography of the head or a “CAT scan”).
Medical history and physical examination — Parents should try to describe how the injury occurred, if possible, including what the child was doing before the injury and how he/she responded after the injury. If there is any reason to suspect that another adult or child intentionally injured the child, this should be discussed with the healthcare provider.
Imaging tests — Many parents assume that their child will undergo imaging tests after a head injury. The purpose of imaging tests, such as a head CT (computed tomography), is to determine if there is bleeding inside or around the brain, if there is a skull fracture, or if there are other serious brain injuries. Most children with a minor head injury do not require an imaging test because the risk of a serious brain injury is small.
When is a head CT needed?
A head CT should be performed when there is concern about a serious brain injury. However, unnecessary use of CT exposes children to radiation and should be avoided 1.
A head CT may be recommended if there are concerning signs or symptoms of brain injury during the examination. These include the following 2:
- Prolonged loss of consciousness
- Persistent or severe memory loss, confusion
- Persistent vomiting
- Seizure
- Severe, persistent, or worsening headache
- Suspicion of intentional injury (abuse)
- Behavioral changes (e.g, lethargy, decreased alertness, extreme irritability)
- Signs of a skull fracture or bulging fontanel (soft spot on an infant’s head)
- Abnormal neurologic examination
- Significant scalp bruise or swelling in a very young infant
- Bloody or clear fluid oozing from the ears or nose
- Incident with a higher risk of brain injury (see ‘Head injury causes’ above)
Why is head CT scan best?
Head CT is recommended to evaluate head injuries because it is fast, available in most hospitals, and is good at identifying recent, severe injuries. Young children may need to be sedated briefly (less than 15 minutes in most cases) to obtain the best results.
MRI (Magnetic resonance imaging) of the brain is not the test of choice for recent brain injury. In addition, in most hospitals, it is not usually available quickly. MRI requires the child to remain completely still for at least 30 minutes, which often requires prolonged sedation or general anesthesia.
Observation
In some cases, it is not clear initially if a head CT is needed. In studies, some children with vomiting, headache, or a brief loss of consciousness (without other symptoms) have a traumatic brain injury while others do not.
In these cases, one reasonable strategy is to observe the child closely for four to six hours after the injury, usually in the emergency department. If the child develops any other symptoms, a CT scan could be done at that time. If no further symptoms occur, the child does not usually need a CT scan. Children who are well more than 12 hours after a head injury have a very low risk of brain injury that requires surgical intervention, although there is always a very small chance. Observation has been shown to decrease the number of children undergoing CT scans without missing important injuries.
Head injury treatment at home
If the child/adolescent’s injury is mild and there are no worrisome signs or symptoms, he or she can be treated and monitored at home. However, if there is any evidence that the injury is more serious, the child should be evaluated in their doctor’s office or an emergency department. (See ‘Head injury tests’ above.)
- Rest — Encourage the child to lie down or choose a quiet activity. Allow the child to sleep if desired. It is not dangerous to sleep after a minor head injury (especially if it is nap time), although the parent should monitor the child. (See ‘Monitoring after a head injury’ below.)
- A mild headache, nausea, and dizziness are common, especially during the first few hours after the injury. If the child is nauseous or has vomited, try offering clear liquids (e.g, soda, clear juice, gelatin).
- Bleeding — If the head is bleeding, clean the area with soap and water and apply pressure to the area with a clean cloth (sterile gauze, if available). Bleeding should stop within 10 minutes. If bleeding does not stop or the cut is large, the child should be evaluated to determine if stitches are needed.
- Swelling — Swelling (a large lump or “goose egg”) is also common after a head injury. To reduce swelling, an ice or a cold pack can be applied to the area for 20 minutes. Swelling usually begins to improve within a few hours, but may take one week to completely resolve.
- Pain — Acetaminophen (e.g, Tylenol®) may be given for a headache. If the child’s headache is severe or worsens, the child should be evaluated by a healthcare provider.
Monitoring after a head injury
Parents of a child with a head injury are usually instructed to observe their child at home for signs of worsening injury. The parent(s) should call the pediatrician and/or take the child to the emergency department immediately if the child does any of the following:
- Vomits twice or continues to vomit four to six hours after the injury
- Develops a severe or worsening headache
- Becomes more and more drowsy or is hard to awaken
- Is confused or not acting normally
- Has a hard time walking, talking, or seeing
- Develops a stiff neck
- Has a seizure (convulsion) or any abnormal movements or behaviors that worry you
- Cannot stop crying or looks sicker
- Has weakness or numbness involving any part of the body
Waking from sleep — It is not usually necessary to wake the child/adolescent from sleep after a minor head injury. If the healthcare provider recommends waking the child, he or she should be able to wake up and recognize his or her surroundings and parent/caretaker.
Follow-up visit — Most healthcare providers recommend a follow up visit or phone call within 24 hours after the injury. This is to ensure that the child is behaving normally, feeling well, and that there are no signs of brain injury.
Return to play — Children and adolescents who have sustained a concussion are at risk for a serious or even fatal complication if they have a second head injury within a short time after the first injury. This is called second impact syndrome.
Any child/adolescent who is suspected of having a concussion should be removed from play (e.g, if playing a team sport) and monitored for signs of brain injury. The child should follow up with a physician before returning to play.
What is concussions?
Concussions — the temporary loss of normal brain function due to an injury — are also a type of internal head injury. Repeated concussions can permanently damage the brain.
In many cases, a concussion is mild and won’t cause long-term damage. Kids who get a concussion usually recover within a week or two without lasting health problems by following certain precautions and taking a break from sports and other activities that make symptoms worse.
Children and adolescents with concussion can take up to four weeks to recover, but most concussions will get better on their own over several days. Following a mild head injury, your child will need to get plenty of rest and sleep, particularly in the first 24 to 48 hours.
Your child may have a headache after a head injury. Give them paracetamol (not ibuprofen or aspirin) every six hours if needed to relieve pain.
There is no need to wake your child during the night unless you have been advised to do so by a doctor. Call an ambulance immediately if you have any difficulty waking your child.
Playing sports is one of the most common causes of concussions. To help protect your kids, make sure that they wear the proper protective gear, and don’t let them continue to play if they’ve had a head injury.
If your child sustains an injury to the head, watch for these signs of a possible concussion:
- “seeing stars” and feeling dazed, dizzy, or lightheaded
- memory loss, such as trouble remembering what happened right before and after the injury
- vomiting
- headaches
- blurred vision and sensitivity to light
- slurred speech or saying things that don’t make sense
- problems concentrating, thinking, or making decisions
- difficulty with coordination or balance (such as being unable to catch a ball or other easy tasks)
- feeling anxious or irritable for no apparent reason
If you suspect a concussion, call your doctor right away.
Key points to remember
- The majority of concussions will get better on their own over several days.
- Follow the return to school and return to sport steps carefully, ensuring at least 24 hours for each return-to-sport step.
- Only move onto the next step if your child is not experiencing any symptoms of concussion.
- Talk to your doctor if you are unsure whether your child is ready for the next stage or if they can fully return to playing sport.
- Seek urgent medical attention if your child’s symptoms get worse or they develop new symptoms of concussion.
What to expect at home
Healing from a concussion takes days to weeks or even months as the brain gradually heals itself. Your child’s condition will slowly improve.
Some children experience cognitive fatigue, meaning that their brain gets tired from thinking more quickly than usual. Your doctor will probably want your child to rest at home and avoid sports or activities that put them at risk of another injury. Talk to your doctor about when your child can return to school or childcare.
Most people with a mild traumatic brain injury recover fully within a few weeks or months.
Your child may use acetaminophen (Tylenol) for a headache. DO NOT give aspirin, ibuprofen (Motrin, Advil, Naproxen), or other non-steroidal anti-inflammatory drugs.
Feed your child foods that are easy to digest. Light activity around the home is okay. Your child needs rest but does not need to stay in bed. It is very important that your child does not do anything that results in another, or similar, head injury.
Have your child avoid activities that need concentration, such as reading, homework, and complex tasks.
When you go home from the emergency room, it is OK for your child to sleep:
- For the first 12 hours, you may want to wake up your child briefly every 2 or 3 hours.
- Ask a simple question, such as your child’s name, and look for any other changes in the way your child looks or acts.
- Make sure the pupils of your child’s eyes are the same size and get smaller when you shine a light in them.
- Ask your health care provider how long you need to do this for.
Returning to School
As long as your child has symptoms, your child should avoid sports, hard play at recess, being overly active, and physical education class. Ask the doctor when your child can return to their normal activities.
Make sure your child’s teacher, physical education teacher, coaches, and school nurse are aware of the recent injury.
Talk to teachers about helping your child catch up on school work. Also ask about timing of tests or major projects. Teachers should also understand that your child may be more tired, withdrawn, easily upset, or confused. Your child may also have a hard time with tasks that require remembering or concentrating. Your child may have mild headaches and be less tolerant of noise. If your child has symptoms in school, have your child stay home until feeling better.
Talk with teachers about:
- Not having your child make up all of their missed work right away
- Reducing the amount of homework or class work your child does for a while
- Allowing rest times during the day
- Allowing your child to turn assignments in late
- Giving your child extra time to study and complete tests
- Being patient with your child’s behaviors as they recover
Based on how bad the head injury was, your child may need to wait 1 to 3 months before doing the following activities. Ask your child’s provider about:
- Playing contact sports, such as football, hockey, and soccer
- Riding a bicycle, motorcycle, or off-road vehicle
- Driving a car (if they are old enough and licensed)
- Skiing, snowboarding, skating, skateboarding, gymnastics, or martial arts
- Participating in any activity where there is a risk of hitting the head or of a jolt to the head
Some organizations recommend that your child stay away from sports activities that could produce a similar head injury, for the rest of the season.
Talk to your doctor if you are unsure about your child’s progress at any step.
Following repeated concussions, your doctor may recommend your child avoid contact sports and any activities with increased risk of head injury for a period of time. This is because after a head injury, your child’s reaction times and thinking may be slower, and this can put them further at risk.
At-risk sports and activities include:
- tackle football
- soccer and hockey
- basketball and netball
- horse riding
- riding motorbikes or BMX bikes
- skiing, snowboarding and surfing
- riding a bike, scooter, skateboard or skates
- playing on a trampoline
climbing trees or other high structures.
Make sure your child always wears a helmet when bike riding or skateboarding.
When to call your doctor
If symptoms do not go away or are not improving a lot after 2 or 3 weeks, follow-up with your child’s doctor.
Call the doctor if your child has:
- A stiff neck
- Fluid or blood leaking from the nose or ears
- Any change in awareness, a hard time waking up, or has become more sleepy
- A headache that is getting worse, lasts a long time, or is not relieved by acetaminophen (Tylenol)
- Fever
- Vomiting more than 3 times
- Problems walking or talking
- Changes in speech (slurred, difficult to understand, does not make sense)
- Problems thinking straight
- Seizures (jerking arms or legs without control)
- Changes in behavior or unusual behavior
- Double vision
- Changes in nursing or eating patterns
Head injury outcome
Children with a minor head trauma who do not have brain injury usually recover completely without any long term complications. Children with mild traumatic brain injury usually recover completely as well, but must be monitored closely and allowed to fully recover before returning to sports 3.
Head injury prevention
It’s impossible to prevent kids from ever being injured, but there are ways to help prevent head blows.
The following tips can help to prevent head injuries, as well as other types of injuries.
Make sure that:
- your home is childproofed to prevent household accidents
- your kids always wear the proper headgear and safety equipment when biking, in-line skating, skateboarding, snowboarding or skiing, and playing contact sports
- kids always use a seatbelt or child safety seat
- your child takes it easy after a head injury, especially if there is a concussion
- your child doesn’t go back to rough play or sports until the doctor says it’s OK. If your child reinjures the brain while it’s still healing, it will take even longer to completely heal.
Bicycle safety — The majority of bicycle-related deaths and hospital admissions are caused by head injuries. Bicycle helmets reduce the risk of head, and brain injuries for bicyclists of all ages. Thus, all bicycle riders and passengers of all ages should wear a helmet every time they ride a bicycle.
- Only bicycle helmets that meet US Consumer Product Safety Commission (CPSC) standards should be used; helmets that have been involved in a crash should be thrown away.
- Bicycle helmets should fit properly and be worn in the proper position.
- Children younger than one year should not ride in bicycle-mounted carriers or trailers.
- When used, mounted carriers should be securely mounted, should have a spoke guard and seat with a high back, shoulder harness, and lap belt. Mounted carriers are not recommended once the child approaches four years of age since the weight of the child makes the bicycle unstable and difficult to handle.
- For child passengers, bicycle trailers are a safer alternative to bicycle mounted carriers. Children who ride in bicycle trailers should wear a helmet.
Bicycle skills — It is important for children to have the developmental skills needed to ride a bike.
- Children younger than three years often do not have the developmental skills necessary to ride a tricycle.
- Children aged four to five can typically ride a bicycle with training wheels and foot-operated brakes; they should not ride in traffic and must be supervised at all times.
- Children aged six and older can usually operate hand brakes and ride a bicycle without training wheels.
- Children should not be permitted to ride in traffic until they have demonstrated that they can control the bicycle, understand and follow the rules of the road, and exercise good judgment. The age at which a child has these skills is variable. Until this point, the child should be closely supervised by an adult and should not ride in the street.
General safety tips
Install car seats and booster seats correctly, and use the seat every time the child rides in a car. A booster seat is needed until the shoulder belt can be worn across the shoulder (rather than the face or neck), when the child is at least 4 feet 9 inches (142.5 cm) tall. Individual states may have additional regulations regarding the need for booster seats.
Many fire and police departments in the United States can determine if the seat is installed correctly. More information is available here: https://www.nhtsa.gov/equipment/car-seats-and-booster-seats
Use gates on stairways and doors to prevent injuries in infants and young children. Install window guards on all windows above the first floor. Do not use wheeled baby walkers.
Teach children to safely cross the street by stopping at the curb and looking both ways (left, right, left). Young children should never cross the street alone.
Discuss sports safety with your child’s healthcare provider. Be sure that the child or adolescent has the appropriate protective equipment for biking, skating, skateboarding, skiing, snowboarding, or contact sports. Protective equipment often includes a helmet, mouthguard, wrist guards, eye protection, and knee and shin pads.
Head injury prevention
Not all head injuries can be prevented. The following simple steps can help keep you and your child safe:
- Always use safety equipment during activities that could cause a head injury. These include seat belts, bicycle or motorcycle helmets, and hard hats.
- Learn and follow bicycle safety recommendations.
- Do not drink and drive, and do not allow yourself to be driven by someone who you know or suspect has been drinking alcohol or is impaired in another way.
Head injury signs and symptoms
The symptoms experienced straight after a head injury are used to determine how serious the head injury is. The information below is a guideline.
Head injuries may cause bleeding in the brain tissue and the layers that surround the brain (subarachnoid hemorrhage, subdural hematoma, epidural hematoma).
Symptoms of a head injury can occur right away. Or symptoms can develop slowly over several hours or days. Even if the skull is not fractured, the brain can hit the inside of the skull and be bruised. The head may look fine, but problems could result from bleeding or swelling inside the skull.
The spinal cord is also likely to be injured in any serious trauma.
Mild head injury
A mild head injury or concussion is when you or your child:
- May display altered level of consciousness at the time of the injury
- Is now alert and interacts with you
- May have vomited, but only once
- May have bruises or cuts on their head
- Raised, swollen area from a bump or a bruise
- Small, superficial (shallow) cut in the scalp
- Headache
- Sensitivity to noise and light
- Irritability
- Confusion
- Lightheadedness and/or dizziness
- Problems with balance
- Nausea
- Problems with memory and/or concentration
- Change in sleep patterns
- Blurred vision
- “Tired” eyes
- Ringing in the ears (tinnitus)
- Alteration in taste
- Fatigue or lethargy
- Is otherwise normal.
You should seek medical advice if you or your child has any of the above symptoms of mild head injury, and you are worried about them. Otherwise, continue to observe your child for any of the signs and symptoms listed under care at home (see above).
Moderate to severe head injury
You should call an ambulance immediately if you or your child has a moderate or severe head injury. Always consult your doctor for a diagnosis.
If you or your child has a moderate or severe head injury, they may:
- Lose consciousness
- Be drowsy and not respond to your voice
- Be dazed or shocked
- Not cry straight after the knock to the head (younger children)
- Be confused, have memory loss or loss of orientation about place, time or the people around them
- Experience visual disturbance
- Have unequally sized pupils or weakness in their arm or leg
- Have something stuck in their head, or a cut causing bleeding that is difficult to stop, or a large bump or bruise on their head
- Have a seizure, convulsion or fit
- Repeated nausea and vomiting more than once
- Severe headache that does not go away
- Loss of short-term memory, such as difficulty remembering the events that led right up to and through the traumatic event
- Slurred speech
- Difficulty with walking
- Weakness in one side or area of the body
- Sweating
- Pale skin color
- Behavior changes including irritability
- Blood or clear fluid draining from the ears or nose
- One pupil (dark area in the center of the eye) is dilated, or looks larger, than the other eye and doesn’t constrict, or get smaller, when exposed to light
- Deep cut or laceration in the scalp
- Open wound in the head
- Foreign object penetrating the head
- Coma (a state of unconsciousness from which a person cannot be awakened; responds only minimally, if at all, to stimuli; and exhibits no voluntary activities)
- Vegetative state (a condition of brain damage in which a person has lost his thinking abilities and awareness of his surroundings, but retains some basic functions such as breathing and blood circulation)
- Locked-in syndrome (a neurological condition in which a person is conscious and can think and reason, but cannot speak or move)
Some head injuries cause changes in brain function. This is called a traumatic brain injury. Concussion is a mild traumatic brain injury. Symptoms of a concussion can range from mild to severe.
Concussion signs and symptoms
People who have concussion may have:
- headache
- nausea
- dizziness
- problems with balance
- problems with attention
- loss of consciousness (30 minutes or less)
- confusion
- sensitivity to noise and light
- brief convulsions
- temporary memory loss
Head injury assessment
The full extent of the problem may not be completely understood immediately after the injury, but may be revealed with a comprehensive medical evaluation and diagnostic testing. The diagnosis of a head injury is made with a physical examination and diagnostic tests. During the examination, the doctor obtains a complete medical history of the patient and family and asks how the injury occurred. Trauma to the head can cause neurological problems and may require further medical follow up.
How to assess severity of head injury:
| Minor head injury
|
|
| Moderate head injury
|
|
| Severe head injury
|
|
Glasgow Coma Scale (GCS) – level of consciousness
Glasgow Coma Scale 15-point test helps a doctor or other emergency medical personnel assess the initial severity of a brain injury by checking a person’s ability to follow directions and move their eyes and limbs. The coherence of speech also provides important clues.
Abilities are scored from 3 to 15 in the Glasgow Coma Scale. Higher scores mean less severe injuries (Total Normal Glasgow Coma Score is 15 out of 15).
| Under 4 years of age | Above 4 years of age | ||
| Response | Score | Response | Score |
| Eye opening | Eye opening | ||
| Spontaneously | 4 | Spontaneously | 4 |
| To verbal stimuli | 3 | To verbal stimuli | 3 |
| To painful stimuli | 2 | To painful stimuli | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best verbal response | Best verbal response | ||
| Orientated and converses | 5 | Appropriate words or social smile, fixes, follows | 5 |
| Confused and converses | 4 | Cries but consolable; less than usual words | 4 |
| Inappropriate words | 3 | Persistently irritable | 3 |
| Incomprehensible sounds | 2 | Moans to pain | 2 |
| No response to pain | 1 | No response to pain | 1 |
| Best motor response | Best motor response | ||
| Obeys verbal commands | 6 | Spontaneous or obeys verbal commands | 6 |
| Localises to stimuli | 5 | Localizes to stimuli | 5 |
| Withdraws to stimuli | 4 | Withdraws to stimuli | 4 |
| Abnormal flexion to pain (decorticate) | 3 | Abnormal flexion to pain (decorticate) | 3 |
| Abnormal extension to pain (decerebrate) | 2 | Abnormal extension to pain (decerebrate) | 2 |
| No response to pain | 1 | No response to pain | 1 |
Imaging tests
- Computerized tomography (CT) scan. This test is usually the first performed in an emergency room for a suspected traumatic brain injury. A CT scan uses a series of X-rays to create a detailed view of the brain. A CT scan can quickly visualize fractures and uncover evidence of bleeding in the brain (hemorrhage), blood clots (hematomas), bruised brain tissue (contusions), and brain tissue swelling.
- Magnetic resonance imaging (MRI). An MRI uses powerful radio waves and magnets to create a detailed view of the brain. This test may be used after the person’s condition stabilizes, or if symptoms don’t improve soon after the injury.
Intracranial pressure monitor
Tissue swelling from a traumatic brain injury can increase pressure inside the skull and cause additional damage to the brain. Doctors may insert a probe through the skull to monitor this pressure.
Neuroimaging Definite indications:
- Any sign of basal skull fracture on secondary survey (see above)
- Focal neurological deficit
- Suspicion of open or depressed skull fracture
- Unresponsive or only responding non-purposefully to pain
- Glasgow Coma Score (GCS) persistently < 8
- Respiratory irregularity/loss of protective laryngeal reflexes
Relative indications:
- Loss of consciousness lasting more than 5 minutes (witnessed)
- Amnesia (antegrade or retrograde) lasting more than 5 minutes
- Persistent vomiting
- Clinical suspicion of non-accidental injury
- Post-traumatic seizures (except a brief ( <2 min) convulsion occurring at time of the impact)
- Glasgow Coma Score (GCS) persistently less than 14, or for a baby under 1 year Glasgow Coma Score (GCS) (pediatric) persistently less than 15, on assessment in the emergency department
- If under 1 year, presence of bruise, swelling or laceration of more than 5 cm on the head
- Dangerous mechanism of injury (high-speed road traffic accident either as pedestrian, cyclist or vehicle occupant, fall from a height).
- Known bleeding tendency
Head injury treatment
If you have a fit or seizure or fall unconscious, even if its only for a second, you should call your local emergency services number and ask for an ambulance.
If you are bleeding and it won’t stop, or if you have fluid coming from your nose or ears, you should go to your nearest emergency department immediately.
You should seek medical advice if you:
- vomit
- have trouble seeing, hearing or speaking properly
- having a headache which is getting worse or won’t go away
- having difficulty seeing or hearing
- being confused or acting strangely
- having difficulty staying awake
- having pupils which are a different size to each other
- losing your balance or feeling dizzy
- losing your memory.
You should also see your doctor if:
- you develop any other new symptoms
- you become increasingly concerned
Otherwise, sit quietly and use an ice pack. You need someone with you to watch you closely for 24 hours (or 48 hours for children or older people). You can take paracetamol, but not other painkillers.
There is no need to stay awake following a head injury. The injured person needs to be woken gently every 4 hours to make sure they respond normally. If they don’t, they should go to the nearest emergency department.
Head injury – general advice
Ensure the parents or responsible adults have clear instructions regarding the management of their child at home especially to return to hospital immediately if their child:
- becomes unconscious or difficult to rouse
- becomes confused
- has a fit
- develops a persistent headache
- vomits more than once
- develops any bleeding or watery discharge from the ears to nose
Minor Head Injury
Mild traumatic brain injuries usually require no treatment other than rest and over-the-counter pain relievers to treat a headache. However, a person with a mild traumatic brain injury usually needs to be monitored closely at home for any persistent, worsening or new symptoms. He or she may also have follow-up doctor appointments.
The doctor will indicate when a return to work, school or recreational activities is appropriate. It’s best to limit physical or thinking (cognitive) activities that make things worse until your doctor advises that it’s OK. Most people return to normal routines gradually.
- The patient may be discharged from the Emergency Department to the care of their parents or responsible adults
- If there is any doubt as to whether there has been loss of consciousness or not, assume there has been and treat as for moderate head injury.
- Adequate analgesia
Moderate Head Injury
- If, on the history from the patient, eyewitnesses, parents and ambulance officers, the patient is not neurologically deteriorating they may be observed in the Emergency Department for a period of up to 4 hours after trauma with 30 minutely neurological observations (conscious state, pulse rate, respiratory rate, BP, pupils and limb power).
- The patient may be discharged home if there is improvement to normal conscious state, no further vomiting and patient is able to tolerate oral fluids.
- A persistent headache, large hematoma or possible penetrating wound may need further investigation, discuss with consultant.
- Adequate analgesia
- Consider anti-emetics, but consider a longer period of observation if anti-emetics are given.
When to consider consultation with pediatric neurosurgical team:
- Moderate head injury with:
- Ongoing drowsiness or vomiting
- Unexplained confusion lasting for more than 4 hours
Severe Head Injury
The initial aim of management of a patient with a serious head injury is prevention of secondary brain damage. The key aims are to maintain oxygenation, ventilation and circulation, and to avoid rises in intracranial pressure (ICP).
Urgent CT of head and cervical spine. Ensure early neurosurgical and intensive care unit (ICU) intervention.
Cervical spine immobilisation should be maintained even if cervical spine imaging is normal.
Intubation and ventilation:
- Child unresponsive or not responding purposefully to pain
- GCS (Glasgow Coma Score) persistently <8
- Loss of protective laryngeal reflexes
- Respiratory irregularity
Intracranial pressure (ICP) is measured in two ways. One way is to place a small hollow tube (catheter) into the fluid-filled space in the brain (ventricle). Other times, a small hollow device (bolt) is placed through the skull into the space just between the skull and the brain. Both devices are inserted by the doctor either in the intensive care unit or in the operating room. The ICP device is then attached to a monitor that gives a constant reading of the pressure inside the skull. If the pressure goes up, it can be treated right away. While the ICP device is in place your child will be given medicine to stay comfortable. When the swelling has gone down and there is little chance of more swelling, the device will be removed.
In consultation with the neurosurgeon consider measures to decrease intracranial pressure:
- Nurse 20-30 degrees head up (after correction of shock) and head in midline position to help venous drainage.
- Ventilate to a pCO2 35mmHg 4-4.5 kPa (consider arterial catheter).
- Ensure adequate blood pressure with crystalloid infusion or inotropes (e.g. noradrenaline) if necessary.
- Consider mannitol (0.5-1 g/kg over 20-30 min i.v.) or hypertonic saline (NaCl 3% 3 ml/kg over 10-20 min i.v.).
- Consider phenytoin loading dose (20 mg/kg over 20 min i.v.).
- Control seizures
- Correct hypoglycaemia
- Analgesia: sufficient analgesia should be administered by careful titration. Head injured children are often more sensitive to opioids.
Medications
Medications to limit secondary damage to the brain immediately after an injury may include:
- Diuretics. These drugs reduce the amount of fluid in tissues and increase urine output. Diuretics, given intravenously to people with traumatic brain injury, help reduce pressure inside the brain.
- Anti-seizure drugs. People who’ve had a moderate to severe traumatic brain injury are at risk of having seizures during the first week after their injury. An anti-seizure drug may be given during the first week to avoid any additional brain damage that might be caused by a seizure. Continued anti-seizure treatments are used only if seizures occur.
- Coma-inducing drugs. Doctors sometimes use drugs to put people into temporary comas because a comatose brain needs less oxygen to function. This is especially helpful if blood vessels, compressed by increased pressure in the brain, are unable to supply brain cells with normal amounts of nutrients and oxygen.
Surgery
Emergency surgery may be needed to minimize additional damage to brain tissues. Surgery may be used to address the following problems:
- Removing clotted blood (hematomas). Bleeding outside or within the brain can result in a collection of clotted blood (hematoma) that puts pressure on the brain and damages brain tissue.
- Repairing skull fractures. Surgery may be needed to repair severe skull fractures or to remove pieces of skull in the brain.
- Bleeding in the brain. Head injuries that cause bleeding in the brain may need surgery to stop the bleeding.
- Opening a window in the skull. Surgery may be used to relieve pressure inside the skull by draining accumulated cerebral spinal fluid or creating a window in the skull that provides more room for swollen tissues.
Rehabilitation
Most people who have had a significant brain injury will require rehabilitation. They may need to relearn basic skills, such as walking or talking. The goal is to improve their abilities to perform daily activities.
Therapy usually begins in the hospital and continues at an inpatient rehabilitation unit, a residential treatment facility or through outpatient services. The type and duration of rehabilitation is different for everyone, depending on the severity of the brain injury and what part of the brain was injured.
Rehabilitation specialists may include:
- Physiatrist, a doctor trained in physical medicine and rehabilitation, who oversees the entire rehabilitation process, manages medical rehabilitation problems and prescribes medication as needed
- Occupational therapist, who helps the person learn, relearn or improve skills to perform everyday activities
- Physical therapist, who helps with mobility and relearning movement patterns, balance and walking
- Speech and language pathologist, who helps the person improve communication skills and use assistive communication devices if necessary
- Neuropsychologist, who assesses cognitive impairment and performance, helps the person manage behaviors or learn coping strategies, and provides psychotherapy as needed for emotional and psychological well-being
- Social worker or case manager, who facilitates access to service agencies, assists with care decisions and planning, and facilitates communication among various professionals, care providers and family members
- Rehabilitation nurse, who provides ongoing rehabilitation care and services and who helps with discharge planning from the hospital or rehabilitation facility
- Traumatic brain injury nurse specialist, who helps coordinate care and educates the family about the injury and recovery process
- Recreational therapist, who assists with time management and leisure activities
- Vocational counselor, who assesses the ability to return to work and appropriate vocational opportunities and who provides resources for addressing common challenges in the workplace
Coping and support
A number of strategies can help a person with traumatic brain injury cope with complications that affect everyday activities, communication and interpersonal relationships. Depending on the severity of injury, a family caregiver or friend may need to help implement the following approaches:
- Join a support group. Talk to your doctor or rehabilitation therapist about a support group that can help you talk about issues related to your injury, learn new coping strategies and get emotional support.
- Write things down. Keep a record of important events, people’s names, tasks or other things that are difficult to remember.
- Follow a routine. Keep a consistent schedule, keep things in designated places to avoid confusion and take the same routes when going to frequently visited destinations.
- Take breaks. Make arrangements at work or school to take breaks as needed.
- Alter work expectations or tasks. Appropriate changes at work or school may include having instructions read to you, allowing more time to complete tasks or breaking down tasks into smaller steps.
- Avoid distractions. Minimize distractions such as loud background noise from a television or radio.
- Stay focused. Work on one task at a time.
Concussion treatment
If you have had concussion, it is important to see a doctor. Do not drive and don’t take medicines like aspirin, anti-inflammatories, sleeping tablets and sedating pain medications until your doctor tells you it’s ok. Your doctor may order a head scan. Some people are kept in hospital for observation. It is important that, after concussion, you are with other people until you recover.
If you have had concussion, you need to rest, both physically and mentally. Children should stay home from school and not use a computer or play video games. The return to school might need to be gradual. You can slowly return to normal mental and physical activities when you have had a minimum of 24 hours without any symptoms.
If you have had concussion, you should not play sport until you are fully recovered as the brain is more vulnerable to a more serious brain injury if another blow occurs. Anybody who is suspected of having concussion while they’re playing sport should sit out the rest of the game.
Most people recover fully within 2 weeks. Some people have symptoms for longer.
A small number of people have longer-term complications. Some have symptoms that last a long time. Some get repeated concussions. People in these situations should see a doctor.
- Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001; 176:289.[↩]
- Schutzman SA, Barnes P, Duhaime AC, et al. Evaluation and management of children younger than two years old with apparently minor head trauma: proposed guidelines. Pediatrics 2001; 107:983.[↩]
- Carroll LJ, Cassidy JD, Peloso PM, et al. Prognosis for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med 2004; :84.[↩]