What is heel pain
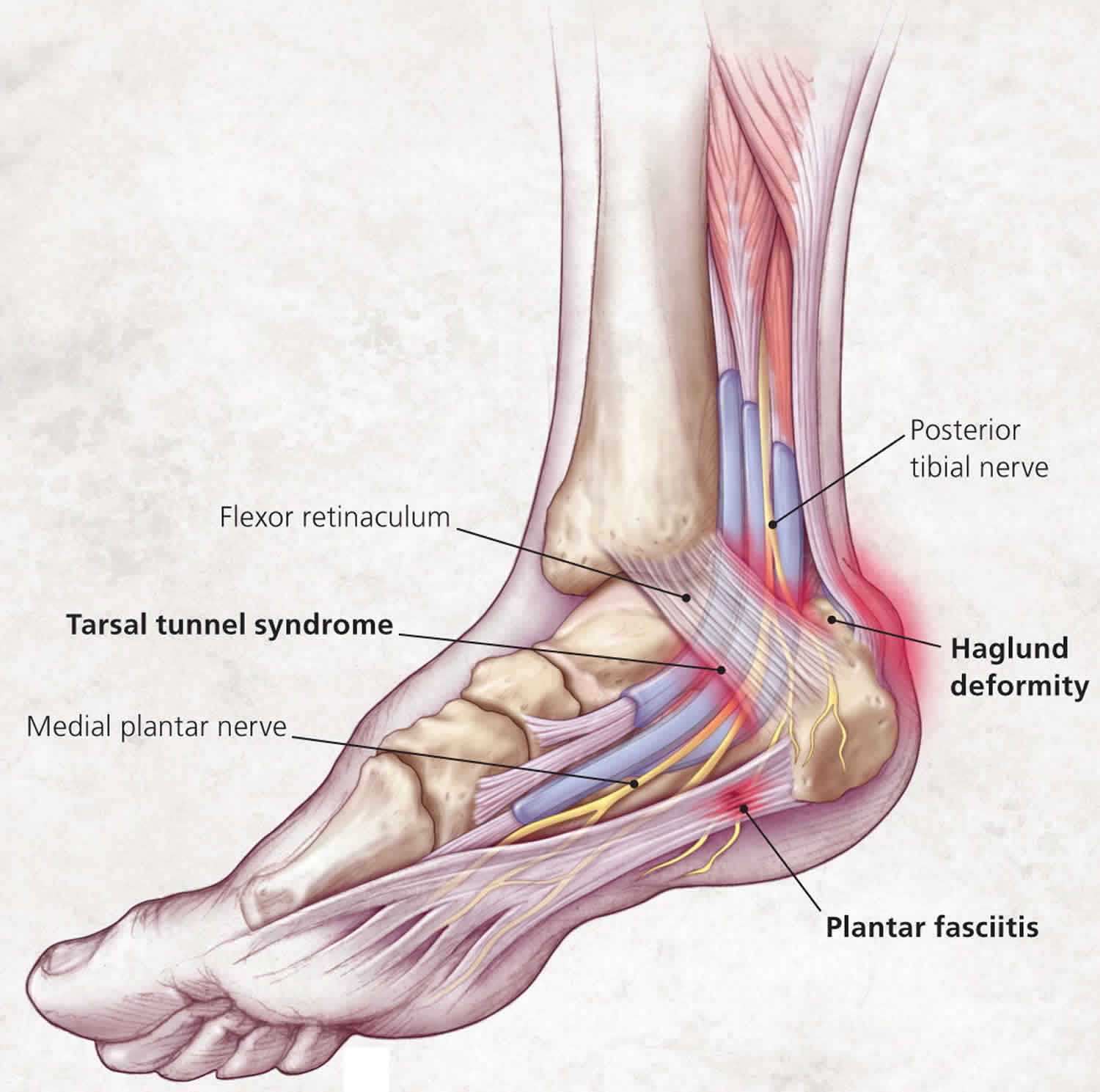
There are many causes of heel pain, but a mechanical cause is the most common. The specific anatomic location of the pain can help guide diagnosis. The most common diagnosis is plantar fasciitis, which leads to medial plantar heel pain, especially with the first weight-bearing steps after rest 1. Other causes of plantar heel pain include calcaneal stress fractures (progressively worsening pain after an increase in activity or change to a harder walking surface), nerve entrapment or neuroma (pain accompanied by burning, tingling, or numbness), heel pad syndrome (deep, bruise-like pain in the middle of the heel), and plantar warts 1. Achilles tendinopathy is a common cause of posterior heel pain; other tendinopathies result in pain localized to the insertion site of the affected tendon. Posterior heel pain can also be attributed to Haglund deformity (a prominence of the calcaneus that may lead to retrocalcaneal bursa inflammation) or Sever disease (calcaneal apophysitis common in children and adolescents) 1. Medial midfoot heel pain, particularly with prolonged weight bearing, may be due to tarsal tunnel syndrome, which is caused by compression of the posterior tibial nerve 1. Sinus tarsi syndrome manifests as lateral midfoot heel pain and a feeling of instability, particularly with increased activity or walking on uneven surfaces 1.
The heel bone is the largest of the 26 bones in the human foot, which also has 33 joints and a network of more than 100 tendons, muscles, and ligaments. Like all bones, it is subject to outside influences that can affect its integrity and its ability to keep you on your feet. Every mile you walk puts 60 tons of stress on each foot. Your feet can handle a heavy load, but too much stress pushes them over their limits. When you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues, you may develop heel pain, the most common problem affecting the foot and ankle.
A sore heel will usually get better on its own without surgery if you give it enough rest. However, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it. When you continue to use a sore heel, it will only get worse and could become a chronic condition leading to more problems. Surgery is rarely necessary.
Common causes of heel pain
Heel pain is most often the result of overuse. However, it may be caused by an injury.
Your heel may become tender or swollen from:
- Shoes with poor support or shock absorption
- Running on hard surfaces, like concrete
- Running too often
- Tightness in your calf muscle or the Achilles tendon
- Sudden inward or outward turning of your heel
- Landing hard or awkwardly on the heel
Your symptoms might give you an idea of what’s causing your heel pain. But don’t self-diagnose – see a doctor if you’re worried.
| Main symptoms | Possible cause |
|---|---|
| Very bad pain taking first steps after waking or after period of not moving, difficulty raising toes off floor | Plantar fasciitis |
| Tenderness and pain at back of heel and along Achilles tendon, pain in calf when standing on tiptoes | Achilles tendonitis |
| Swelling, feels hot, pain on squeezing heel bone, hurts to walk and you’ve had an injury | Heel fracture |
| Pain at back of heel, can raise toes without pain | Bursitis |
| Numbness or tingling in foot when moving or resting | Peripheral neuropathy or tarsal tunnel syndrome |
| Stiff, swollen heel, difficult to move foot | Arthritis |
How you can treat heel pain yourself
You can treat most heel pain yourself at home. If it doesn’t go away, see a doctor.
Try these things:
DO
- Rest – if possible, avoid activities that put stress on your heels, such as running, standing for long periods or walking on hard surfaces.
- Take ibuprofen or paracetamol
- Put an ice pack (or bag of frozen peas) in a towel under the heel for up to 20 minutes every 2 to 3 hours
- Wear shoes with a medium heel (2 to 3cm) – both men and women
- Gentle stretching exercises
- Try heel pads, cups or wedges. Custom-made orthotics usually aren’t needed for heel problems.
DON’T
- put weight on the foot – avoid walking or standing for long periods
- go barefoot or wear flat shoes
See a doctor if:
- you see no improvement after treating at home
- your pain is getting worse despite home treatment.
- you’re finding it difficult to walk
See your doctor immediately if you have:
- Your pain is sudden and severe.
- Severe pain and swelling near your heel
- Inability to bend your foot downward, rise on your toes or walk normally
- Heel pain with fever, numbness or tingling in your heel
- Severe heel pain immediately after an injury
- You have redness or swelling of your heel.
- You cannot put weight on your foot, even after resting.
Figure 1. Heel pain
Heel pain causes
Heel pain has many causes (see Table 1). Most diagnoses stem from a mechanical cause (Table 2). Heel pain is generally the result of faulty biomechanics (walking gait abnormalities) that place too much stress on the heel bone and the soft tissues that attach to it. The stress may also result from injury, or a bruise incurred while walking, running, or jumping on hard surfaces; wearing poorly constructed footwear (such as flimsy flip-flops); or being overweight.
The most common causes of heel pain are plantar fasciitis (bottom of the heel) and Achilles tendinitis (back of the heel).
Causes of heel pain also include:
- Achilles tendinitis
- Achilles tendon rupture
- Bone tumor
- Bursitis (joint inflammation)
- Haglund’s deformity
- Heel spur
- Osteomyelitis (a bone infection)
- Paget’s disease of bone
- Peripheral neuropathy
- Plantar fasciitis
- Reactive arthritis
- Retrocalcaneal bursitis
- Rheumatoid arthritis (inflammatory joint disease)
- Sarcoidosis (collections of inflammatory cells in the body)
- Stress fractures
- Tarsal tunnel syndrome
Table 1. Common causes of heel pain
Arthritic | |
Gout | |
Rheumatoid arthritis | |
Seronegative spondyloarthropathies | |
Infectious | |
Diabetic ulcers | |
Osteomyelitis | |
Plantar warts | |
Mechanical (see Table 2) | |
Neuropathic | |
Lumbar radiculopathy | |
Nerve entrapment (branches of posterior tibial nerve) | |
Neuroma | |
Tarsal tunnel syndrome (posterior tibial nerve) | |
Trauma | |
Tumor (rare) | |
Ewing sarcoma | |
Neuroma | |
Vascular (rare) | |
Table 2. Mechanical causes of heel pain by location
| Etiology | Clinical features | Initial treatment |
|---|---|---|
Plantar heel pain | ||
Plantar fasciitis/fasciosis |
| Relative rest |
Stretching/strengthening exercises | ||
Anti-inflammatory/analgesic medication | ||
Ice | ||
Arch support | ||
Heel spur |
| Decrease pressure to affected area |
Calcaneal stress fracture |
| Decrease in activity level, and occasionally no weight bearing |
Heel pads or walking boots | ||
Nerve entrapment (medial or lateral plantar nerve, nerve to abductor digiti minimi) |
| Rest |
Stretching/strengthening exercises | ||
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Ice | ||
Heel pad syndrome |
| Rest |
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Heel cups | ||
Taping | ||
Posterior heel pain | ||
Achilles tendinopathy |
| Eccentric exercises |
Decrease pressure to affected area | ||
Heel lifts, other orthotic devices | ||
Anti-inflammatory/analgesic medication | ||
Haglund deformity |
| Decrease pressure to affected area |
Anti-inflammatory/analgesic medication | ||
Retrocalcaneal bursitis |
| Decrease pressure to affected area |
Anti-inflammatory/analgesic medication | ||
Corticosteroid injections (preferably ultrasound-guided) | ||
Sever disease (calcaneal apophysitis) |
| Avoid pain-inducing activities |
Anti-inflammatory/analgesic medication | ||
Ice | ||
Stretching/strengthening exercises | ||
Orthotic devices | ||
Midfoot (medial) heel pain | ||
Posterior tibialis tendinopathy |
| Eccentric exercises |
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Flexor digitorum longus tendinopathy |
| Eccentric exercises |
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Flexor hallucis longus tendinopathy |
| Eccentric exercises |
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Tarsal tunnel syndrome |
| Avoid pain-inducing activities |
Orthotic devices | ||
Neuromodulator/anti-inflammatory medication | ||
Corticosteroid injection | ||
Midfoot (lateral) heel pain | ||
Peroneal tendinopathy |
| Eccentric exercises |
Decrease pressure to affected area | ||
Anti-inflammatory/analgesic medication | ||
Sinus tarsi syndrome |
| Orthotics |
Physical therapy | ||
Anti-inflammatory/analgesic medication | ||
Corticosteroid injection | ||
Figure 2. Heel Pain Diagnostic Algorithm
[Source 1 ]Plantar Heel Pain
Plantar fasciitis and heel spurs
Every year, as many as 2 million people present with plantar heel pain 2, with men and women affected equally 3. Plantar fasciitis is the most common cause of plantar heel pain 1. Historically, plantar fasciitis was considered an inflammatory syndrome; however, recent studies have demonstrated a noninflammatory, degenerative process 4, leading some to use the term plantar fasciosis. Regardless, the condition usually stems from multiple causes and can be debilitating for the patient.
Plantar fasciitis causes throbbing medial plantar heel pain that is worse with the first few steps in the morning or after long periods of rest. The pain usually decreases after further ambulation, but can return throughout the day with continued weight bearing. Tenderness is noted on the medial calcaneal tuberosity and along the plantar fascia (Figure 1). Pain often increases with stretching of the plantar fascia, which is achieved by passive dorsiflexion of the foot and toes. Radiography is usually not necessary, although weight-bearing radiography can help rule out other causes of heel pain. Approximately 50 percent of patients with plantar fasciitis have heel spurs 5, but they are most often an incidental finding and do not correlate well with the patient’s symptoms. Ultrasonography can demonstrate a thicker heel aponeurosis of greater than 5 mm 6.
Treatment of plantar fasciitis is typically conservative, although resolution can take months to years 7. First-line therapies include relative rest, stretching before initial weight bearing, strengthening exercises, anti-inflammatory or analgesic medications, and ice. Arch taping, over-the-counter shoe inserts, custom orthotics, or supportive shoes may be helpful 5. Night splints, corticosteroid injections, and formal physical therapy have been used for more recalcitrant cases 8. Extracorporeal shock wave therapy may also be of benefit.9,10 Surgery to transect the plantar aponeurosis is used only when other treatments have been ineffective 5.
Calcaneal stress fracture
Calcaneal stress fracture is the second most common stress fracture in the foot, following metatarsal stress fracture 9. A calcaneal stress fracture is usually caused by repetitive overload to the heel, and most commonly occurs immediately inferior and posterior to the posterior facet of the subtalar joint 7. Patients often report onset of pain after an increase in weight-bearing activity or change to a harder walking surface. The pain initially occurs only with activity, but often progresses to include pain at rest. Examination may reveal swelling or ecchymosis; point tenderness at the fracture site is usually indicative of a calcaneal stress fracture. Because radiography often does not initially reveal the fracture, bone scans or magnetic resonance imaging (Figure 3) may be needed 9.
Early treatment of a calcaneal stress fracture involves decreasing activity level and possibly no weight bearing. Heel pads or walking boots are also used.
Figure 3. Calcaneal stress fracture
Footnote: Magnetic resonance image of calcaneal stress fracture (red arrow).
[Source 10 ]Nerve entrapment
Heel pain that is accompanied by burning, tingling, or numbness may suggest a neuropathic etiology. These symptoms most commonly indicate nerve entrapment caused by overuse, trauma, or injury from previous surgery. Affected nerves leading to plantar heel pain are typically branches of the posterior tibial nerve, including the medial plantar nerve, the lateral plantar nerve, or the nerve to the abductor digiti minimi. Neuropathic heel pain is usually unilateral; therefore, underlying systemic illnesses should be ruled out in those with bilateral pain 7. Lumbar radiculopathy of L4-S2 must also be considered in the diagnosis of neuropathic heel pain.
Initial treatment of heel pain caused by nerve entrapment includes rest, ice, anti-inflammatory or analgesic medications, relief of pressure at the site of pain, and stretching exercises. If conservative measures are ineffective after six to 12 months, surgical decompression should be considered.
Heel pad syndrome
Pain from heel pad syndrome is often erroneously attributed to plantar fasciitis 11. Patients with heel pad syndrome present with deep, bruise-like pain, usually in the middle of the heel, that can be reproduced with firm palpation 11. Walking barefoot or on hard surfaces exacerbates the pain. The syndrome is usually caused by inflammation, but damage to or atrophy of the heel pad can also elicit pain. Decreased heel pad elasticity with aging and increasing body weight can also contribute to the condition 11. Treatment is aimed at decreasing pain with rest, ice, and anti-inflammatory or analgesic medications. Heel cups, proper footwear, and taping can also be used.
Soft tissue causes
Neuromas may develop on the branches of the tibial nerve, causing plantar heel pain. Patients often present with symptoms similar to plantar fasciitis, although pain can sometimes be a more burning or tingling sensation. Palpation may reveal a painful lump at the neuroma site. Neuromas should be considered when treatment for plantar fasciitis is ineffective 12.
Plantar warts are sometimes a source of heel pain. They are raised skin lesions arising from direct contact with human papillomavirus. The lesion is noted on inspection of the heel and is tender to palpation. Plantar warts are usually self-limited; however, patients often need quicker resolution to return to activity. Over-the-counter topical medications, cryotherapy, laser therapy, and shaving the wart have been shown to be beneficial, but may worsen pain.
Posterior Heel Pain
Achilles tendinopathy
Achilles tendinopathy is usually caused by running, wearing high heels, and other activities associated with overuse of the calf muscles. The achilles tendon is formed by the union of the gastrocnemius and soleus muscle tendons 9. The condition can be insertional or within the midsubstance of the tendon, leading to posterior heel pain that is achy, is occasionally sharp, and worsens with increased activity or pressure to the area, such as from contact with shoe backing 7. Fluoroquinolone use has also been shown to precipitate Achilles tendinopathy, particularly in older persons 13. Palpation reveals tenderness along the Achilles tendon and sometimes a palpable prominence from tendon thickening. Passive dorsiflexion of the foot increases the pain. Radiography may demonstrate spurring at the Achilles tendon insertion site or intratendinous calcifications 7, whereas ultrasonography may show thickening of the tendon (Figure 4).
The most beneficial treatment of Achilles tendinopathy is eccentric exercises, which involve lengthening a muscle in response to external resistance 14. Initial treatment should also include reduction of pressure to the area, heel lifts or other orthotic devices, and anti-inflammatory or analgesic medications. Nitroglycerin patches and platelet-rich plasma injections have shown benefit in some studies 15. Surgical debridement may be needed for severe cases.
Figure 4. Achilles tendinopathy
Footnote: Ultrasound image showing (A) normal Achilles tendon (arrow) and (B) thickened Achilles tendon (arrow) from Achilles tendinopathy.
[Source 10 ]Haglund deformity
A Haglund deformity is a prominence of the superior aspect of the posterior calcaneus (Figures 1 and 5). The condition can occur in anyone, but is most common in women who are in their twenties 16. Repeated pressure, from this deformity or from ill-fitting footwear, can cause inflammation and swelling between the calcaneus and Achilles tendon, leading to retrocalcaneal bursitis 7. Patients with bursitis have erythema and swelling over the bursa and tenderness to direct palpation.
Treatment of Haglund deformity, with or without bursitis, targets decreasing the pressure and inflammation with open-heeled shoes, anti-inflammatory or analgesic medications, and corticosteroid injections (ultrasound-guided injections are preferable to avoid disruption of the Achilles tendon). Physical therapy may also help reduce pain. In recalcitrant cases, surgery to remove the Haglund deformity may be necessary 7.
Figure 5. Haglund deformity
Sever disease
Sever disease (calcaneal apophysitis) is the most common cause of heel pain in children and adolescents, usually occurring between five and 11 years of age 17. Bones grow quicker than the muscles and tendons in these patients. The tight Achilles tendon begins to pull on its insertion site with repetitive running or jumping activities, causing microtrauma to the area. There may be swelling and tenderness around the Achilles tendon insertion site, and passive dorsiflexion may increase pain. Radiography is usually normal and therefore does not aid in the diagnosis, but may reveal a fragmented or sclerotic calcaneal apophysis 17. Treatment involves decreasing pain-inducing activities, anti-inflammatory or analgesic medication if needed, ice, stretching and strengthening of the gastrocnemius-soleus complex, and some orthotic devices.
Figure 6. Sever disease (calcaneal apophysitis)
Footnote: Fat-suppressed T2-weighted images show bone marrow edema within the calcaneal apophysis, extending into the adjacent calcaneal tuberosity, and post-contrast fat-supressed T1-weighted images show contrast enhancement in the same locations. There is also edema around the apophysis as seen on fat-suppressed T2-weighted images. The appearances are suggestive of calcaneal apophysitis
[Source 18 ]Midfoot Heel Pain
Tendinopathies
Although less common, other tendinopathies can cause heel pain localized to the insertion site of the affected tendon. Medial heel pain may be triggered by the posterior tibialis, flexor digitorum longus, or flexor hallucis longus tendons 9. Lateral heel pain can originate from the peroneal tendon. Musculoskeletal ultrasonography of these tendons may aid in the diagnosis 19. Treatment is similar to that of Achilles tendinopathy.
Tarsal tunnel syndrome
The tarsal tunnel is a fibroosseous space formed by the flexor retinaculum, medial calcaneus, posterior talus, and medial malleolus 20. Compression of the posterior tibial nerve most commonly occurs as it courses through this tunnel, causing neuropathic pain and numbness in the posteromedial ankle and heel (Figure 7), which may extend into the distal sole and toes 9. Patients often report worsening of pain with standing, walking, or running, and alleviation of pain with rest or loose-fitting footwear. Physical examination may reveal a pes planus deformity, which increases tension of the nerve with weight bearing 9, or muscle atrophy in more severe cases.13 Pain can be reproduced by tapping along the course of the nerve (Tinel sign) and with provocative maneuvers to stretch or compress the nerve (dorsiflexion-eversion test, plantar flexion-inversion test) 9. Electromyography and nerve conduction studies may be useful to confirm the diagnosis 9.
Treatment is mostly conservative, with activity modification, orthotic devices, neuromodulator medications (tricyclics or antiepileptics), or anti-inflammatory medications. Corticosteroid injections into the tarsal tunnel may also be beneficial. Surgery is available if conservative measures are ineffective 12.
Figure 7. Tarsal tunnel syndrome
Sinus tarsi syndrome
The sinus tarsi, or talocalcaneal sulcus, is an anatomic space bound by the calcaneus, talus, talocalcaneonavicular joint, and posterior facet of the subtalar joint. Pain from this location is usually felt in the lateral calcaneus and ankle, and is worse immediately following exercise and when walking on an uneven surface 19. It can arise from repeated lateral ankle sprains or from repeated hyperpronation of the foot 19. Initial treatment includes managing the underlying causes with orthotics or physical therapy, although anti-inflammatory or analgesic medications and corticosteroid injections (Figure 8) may also be beneficial.
Figure 8. Sinus tarsi syndrome
Footnote: Symptoms associated with sinus tarsi syndrome are usually described as deep in the ankle and can be localized by athlete pointing to the sinus tarsi space.
[Source 21 ]Heel pain prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions:
- Wear shoes that fit well—front, back, and sides—and have shock-absorbent soles, rigid shanks, and supportive heel counters
- Wear the proper shoes for each activity
- Do not wear shoes with excessive wear on heels or soles
- Prepare properly before exercising. Warm up and do stretching exercises before and after running.
- Pace yourself when you participate in athletic activities
- Don’t underestimate your body’s need for rest and good nutrition
- If obese or overweight, lose weight
Heel pain diagnosis
Heel pain can have many causes. If your heel hurts, see your doctor right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you’ve had it.
Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel.
Heel pain treatment
The following steps may help relieve your heel pain:
- Use crutches to take weight off your feet.
- Rest as much as possible for at least a week.
- Apply ice to the painful area. Do this at least twice a day for 10 to 15 minutes. Ice more often in the first couple of days.
- Take acetaminophen or ibuprofen for the pain.
- Wear well-fitted and supportive shoes.
- Use a heel cup, felt pads in the heel area, or shoe insert.
- Wear night splints.
Your doctor may recommend other treatments, depending on the cause of your heel pain.
Maintaining flexible and strong muscles in your calves, ankles, and feet can help prevent some types of heel pain. Always stretch and warm-up before exercising.
Wear comfortable and well-fitting shoes with good arch support and cushioning. Make sure there is enough room for your toes.
- Heel Pain: Diagnosis and Management. Am Fam Physician. 2018 Jan 15;97(2):86-93. https://www.aafp.org/afp/2018/0115/p86.html[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Martin JE, Hosch JC, Goforth WP, Murff RT, Lynch DM, Odom RD. Mechanical treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc. 2001;91(2):55–62.[↩]
- Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA. 2002;288(11):1364–1372.[↩]
- Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–237.[↩]
- Cole C, Seto C, Gazewood J. Plantar fasciitis: evidence-based review of diagnosis and therapy. Am Fam Physician. 2005;72(11):2237–2242.[↩][↩][↩]
- McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2009;2:32.[↩]
- Thomas JL, Christensen JC, Kravitz SR, et al.; American College of Foot and Ankle Surgeons Heel Pain Committee. The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg. 2010;49(3 suppl):S1–S19.[↩][↩][↩][↩][↩][↩][↩]
- Dyck DD Jr, Boyajian-O’Neill LA. Plantar fasciitis. Clin J Sport Med. 2004;14(5):305–309.[↩]
- Aldridge T. Diagnosing heel pain in adults [published correction appears in Am Fam Physician. 2006;73(5):776]. Am Fam Physician. 2004;70(2):332–338.[↩][↩][↩][↩][↩][↩][↩][↩]
- Diagnosis of Heel Pain. Am Fam Physician. 2011 Oct 15;84(8):909-916. https://www.aafp.org/afp/2011/1015/p909.html[↩][↩]
- Prichasuk S. The heel pad in plantar heel pain. J Bone Joint Surg Br. 1994;76(1):140–142.[↩][↩][↩]
- Peck E, Finnoff JT, Smith J. Neuropathies in runners. Clin Sports Med. 2010;29(3):437–457.[↩][↩]
- Corrao G, Zambon A, Bertù L, et al. Evidence of tendinitis provoked by fluoroquinolone treatment: a case-control study. Drug Saf. 2006;29(10):889–896.[↩]
- Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med. 2009;19(1):54–64.[↩]
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–1767.[↩]
- Sofka CM, Adler RS, Positano R, Pavlov H, Luchs JS. Haglund’s syndrome: diagnosis and treatment using sonography. HSS J. 2006;2(1):27–29.[↩]
- Cassas KJ, Cassettari-Wayhs A. Childhood and adolescent sports-related overuse injuries. Am Fam Physician. 2006;73(6):1014–1022.[↩][↩]
- Case courtesy of Dr Paulo A Noronha, Radiopaedia.org, rID: 63302 https://radiopaedia.org/cases/63302[↩]
- Choudhary S, McNally E. Review of common and unusual causes of lateral ankle pain [published ahead of print October 24, 2010].[↩][↩][↩]
- Daniels TR, Lau JT, Hearn TC. The effects of foot position and load on tibial nerve tension. Foot Ankle Int. 1998;19(2):73–78.[↩]
- Examination and intervention for sinus tarsi syndrome. N Am J Sports Phys Ther. 2009;4(1):29-37. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2953318/[↩]