What is hemiparesis
Hemiparesis is weakness of one side of your body, including one arm and one leg. The word, ‘hemi,’ means, ‘one side, while, ‘paresis,’ means, ‘weakness.’ Hemiparesis is commonly caused by either stroke or cerebral palsy, although it can also be caused by multiple sclerosis, myasthenia gravis, brain tumors, brain abscess, meningitis, viral encephalitis, metabolic syndromes, seizure with Todd’s paralysis, motor neuron disease, psychiatric disorders and other diseases of the nervous system or brain. Hemiparesis is a very common symptom that develops after stroke where motor impairments of the contralateral limb(s) occur. The limb(s) that are affected are on the opposite side to where the brain was damaged during the stroke.
Stroke is among the most common causes of adult-onset disability 1. 70–85% of first strokes are accompanied by hemiplegia 2. 6 months after stroke, only 60% of people with hemiparesis who need inpatient rehabilitation have achieved functional independence in simple activities of daily living (ADL) such as toileting and walking short distances 3. Patients with sensorimotor and visual-field loss are much more dependent on carers than those with pure motor impairments, but even the latter may walk too slowly to participate in out-of-home activities or may be unable to integrate the use of an affected arm into personal care 1.
Initially, motor impairments after stroke are experienced in as many as 80% of people in the form of hemiparesis but not all these people will develop spastic symptoms. That said, severe activity and motor problems are seen in most people who have had a stroke, regardless of whether spasticity is present or not. By three months post stroke 19% of people will experience spasticity and this figure increases to 38% of people after 12 months.
Sixty-five percent of those who display initial paralysis after stroke will retain excessive muscle activity in the upper limbs 26 weeks after the event.
Disabling spasticity (also called post-stroke spasticity), defined as spasticity which causes extreme discomfort and requires intervention, is experienced by 4% of people one year post-stroke. Post-stroke disabling spasticity occurs more commonly in younger survivors (under 55 years of age) of first-ever stroke.
Your brain is divided into two hemispheres, separated by a bundle of fibers called the corpus callosum. Generally speaking, the right side of your brain controls muscles and other functions on the left side of the body, while the left side of the brain controls much of the right side of the body. Thus hemiparesis almost always indicate a problem with one side of the brain.
Although your arms, legs, and possibly your torso are the regions of the body most obviously affected by hemiparesis, in most cases of hemiparesis these body regions are actually perfectly healthy. Instead, the problem resides in your brain, which is unable to produce, send, or interpret signals due to disease or trauma-related damage. Less frequently, hemiparesis results from damage to one side of the spinal cord, but these sorts of injuries more typically produce global problems, not just paralysis on one side of the body.
A stroke is a medical emergency. Strokes happen when blood flow to your brain stops. Within minutes, your brain cells begin to die. There are two types of strokes: ischemic stroke and hemorrhagic stroke. Ischemic strokes are the most common. They are caused by a blood clot. That clot blocks a blood vessel in the brain. With a hemorrhagic stroke, a blood vessel breaks and bleeds into the brain.
If you have a stroke, you may lose the ability to do something that is controlled by the injured part of your brain. For example, you could lose the use of an arm or leg. You could lose the ability to speak. The damage can be temporary or permanent. However, the sooner you get treatment after stroke symptoms start, the better the chance of getting blood flow to your brain. This prevents more damage. People who have had a stroke are more likely to have another stroke. The risk is especially high during the year after your first stroke.
Call for emergency help immediately if you have any of the following symptoms:
- Sudden weakness or numbness of the face, arm, or leg on one side of your body.
- Sudden dimness or loss of vision, particularly in one eye.
- Trouble talking or understanding what others are saying.
- Sudden severe headache with no known cause.
- Sudden unexplained dizziness.
- Falling or unstable walking.
Also, these symptoms can tell you if someone else is having a stroke.
It’s called the F.A.S.T. test:
- F is for Face drooping. Does one side of the face droop when the person tries to smile?
- A is for Arm weakness. When the person raises both arms, does one arm drift downward?
- S is for Speech difficulty. Can the person repeat a simple sentence (for example, “The sky is blue.”) correctly? Is his or her speech slurred?
- T is for Time to call for emergency help. It’s important to get help immediately if a person has any of these symptoms.
Another warning sign of a stroke is called a transient ischemic attack (TIA). A transient ischemic attack is a “mini-stroke.” It causes the same symptoms listed above. It may only last a few minutes. However, do not ignore it. Having a transient ischemic attack increases your risk of having a stroke later. Call your doctor immediately if you think you are having a transient ischemic attack.
If you have any of these symptoms, you must get to a hospital quickly to begin treatment. Acute stroke therapies try to stop a stroke while it is happening by quickly dissolving the blood clot or by stopping the bleeding. Post-stroke rehabilitation helps individuals overcome disabilities that result from stroke damage. Drug therapy with blood thinners is the most common treatment for stroke.
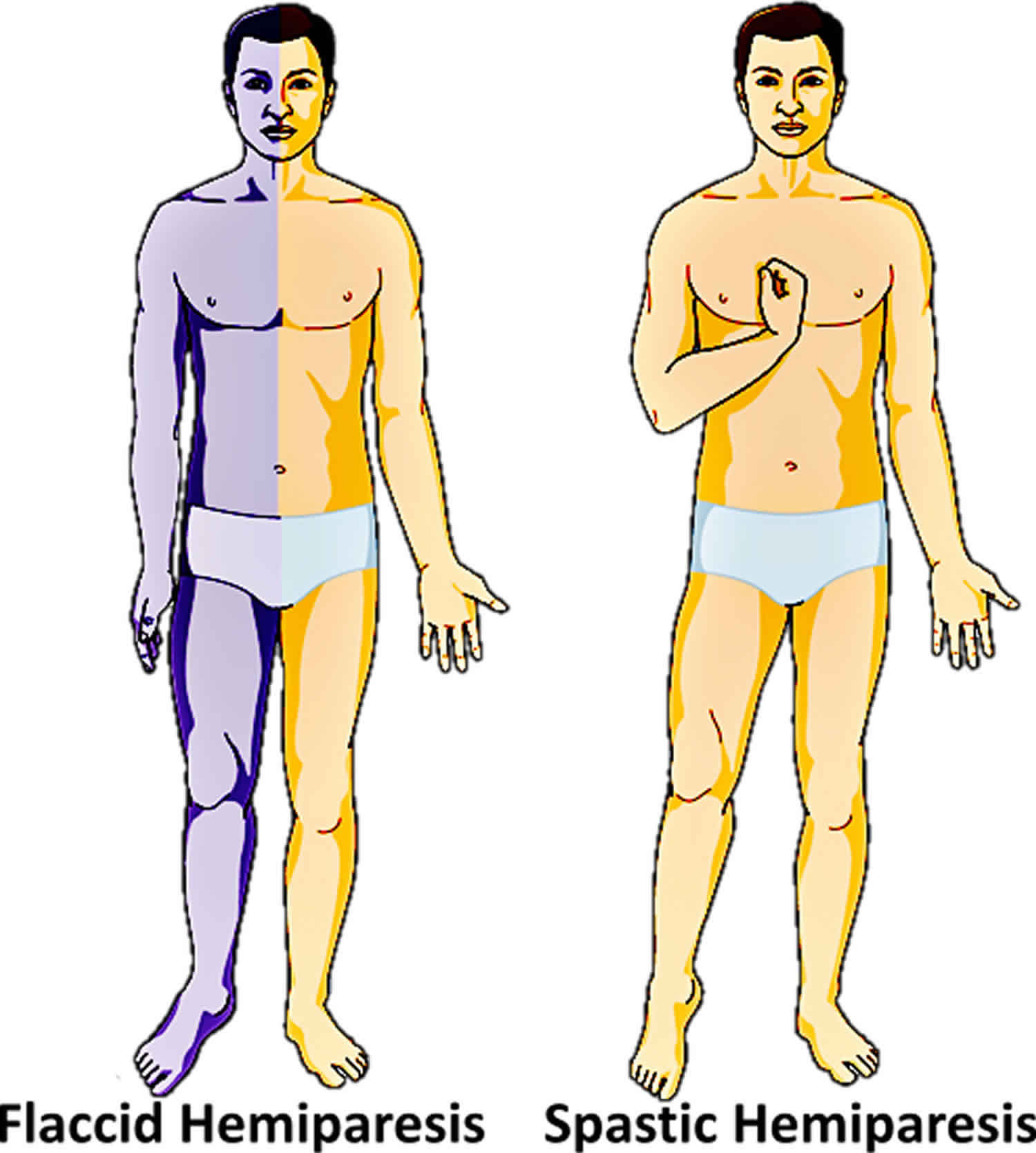
Figure 1. Hemiparesis
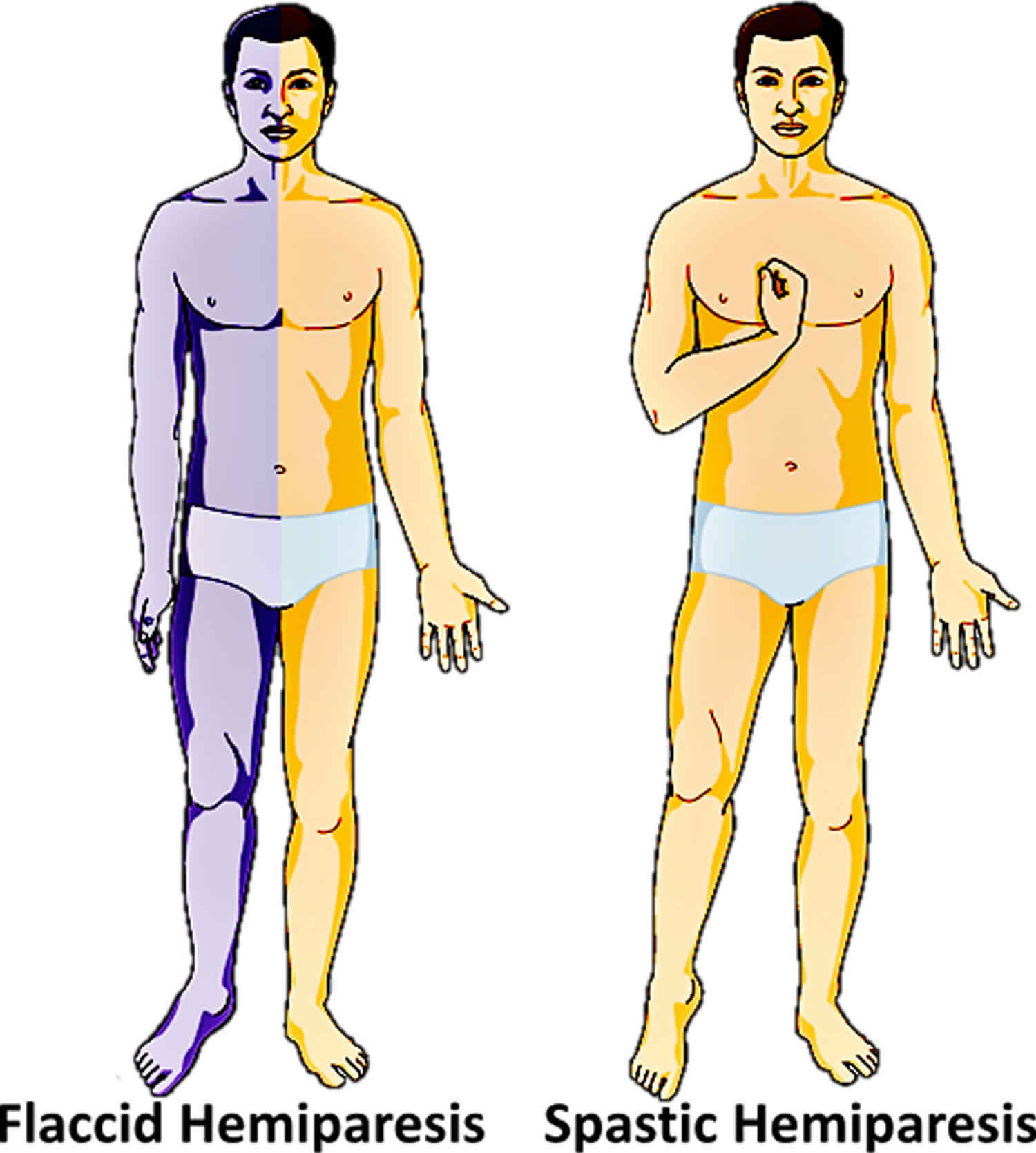
Figure 2. Primary motor cortex and somatosensory cortex of the cerebrum
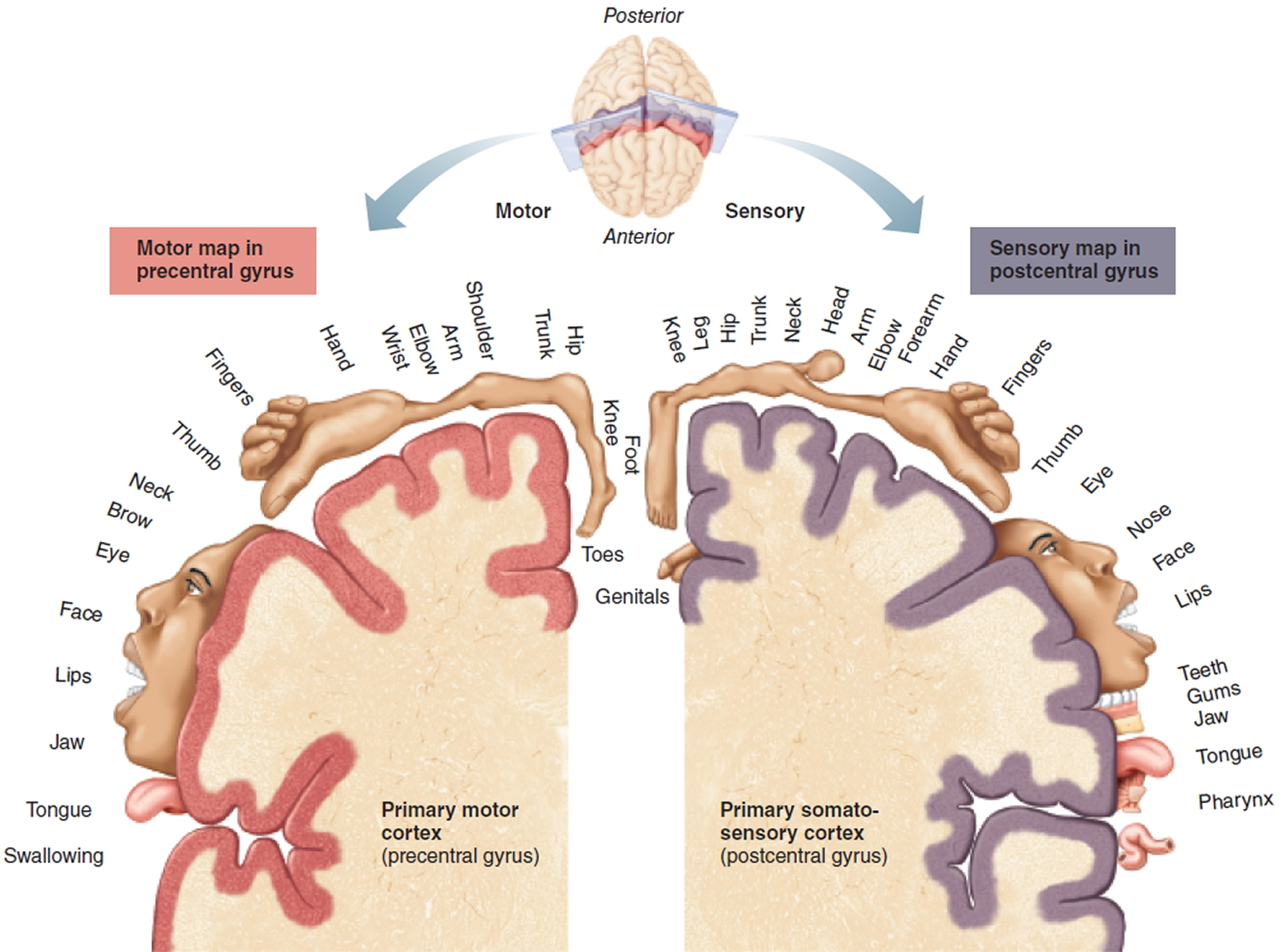
Figure 3. Brain blood supply
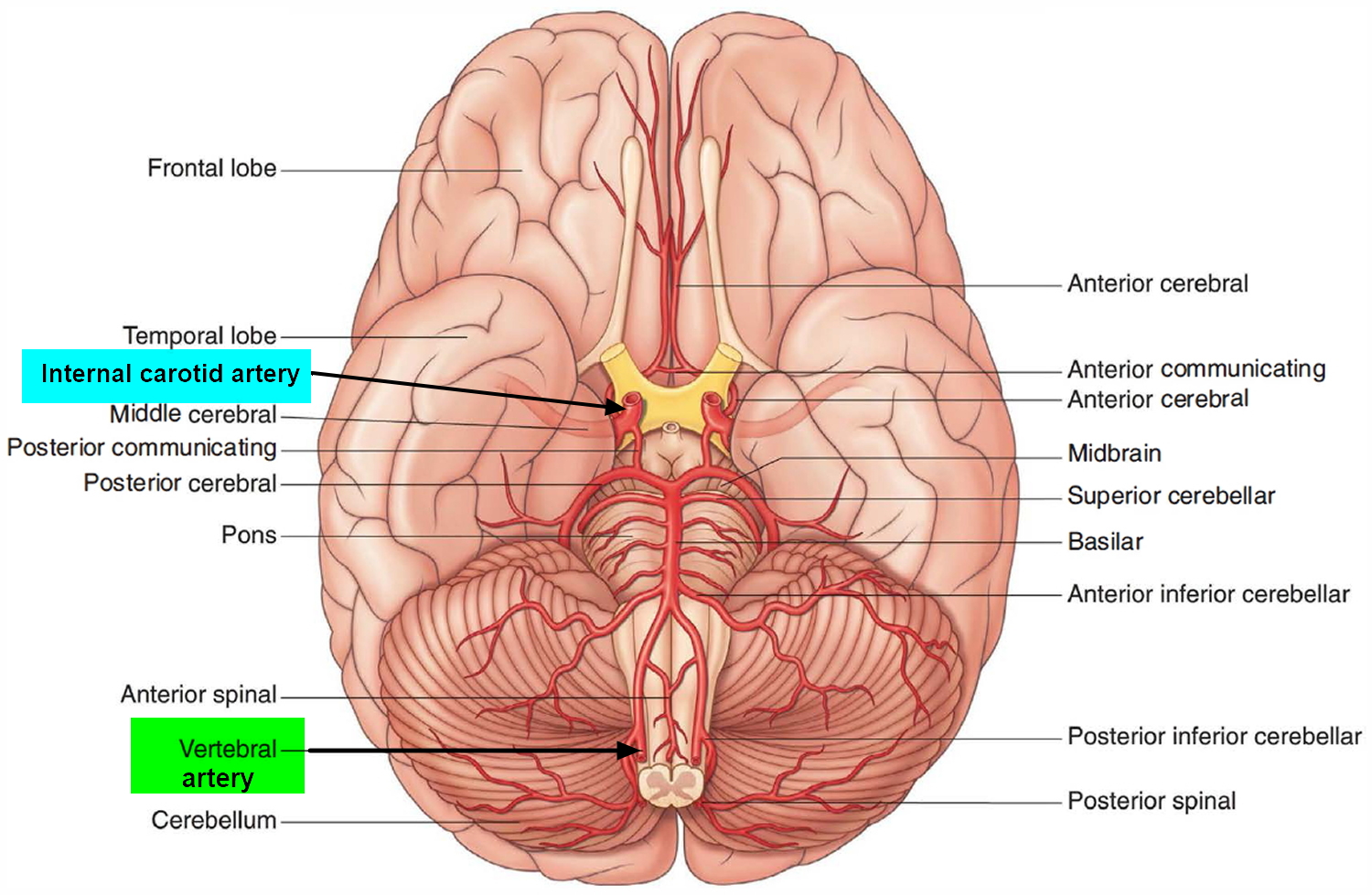
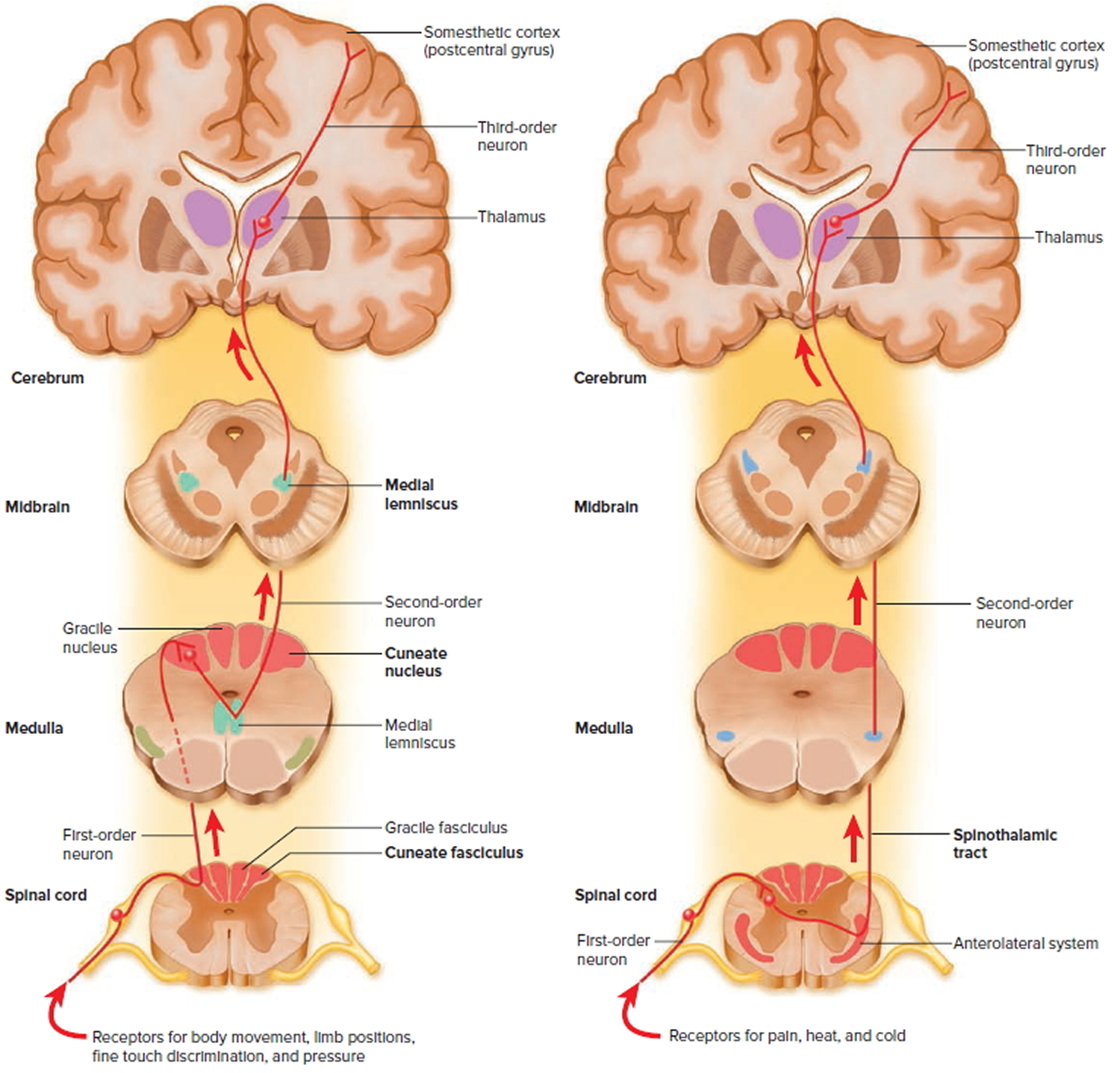
Figure 4. Spinal cord ascending tracts to the brain
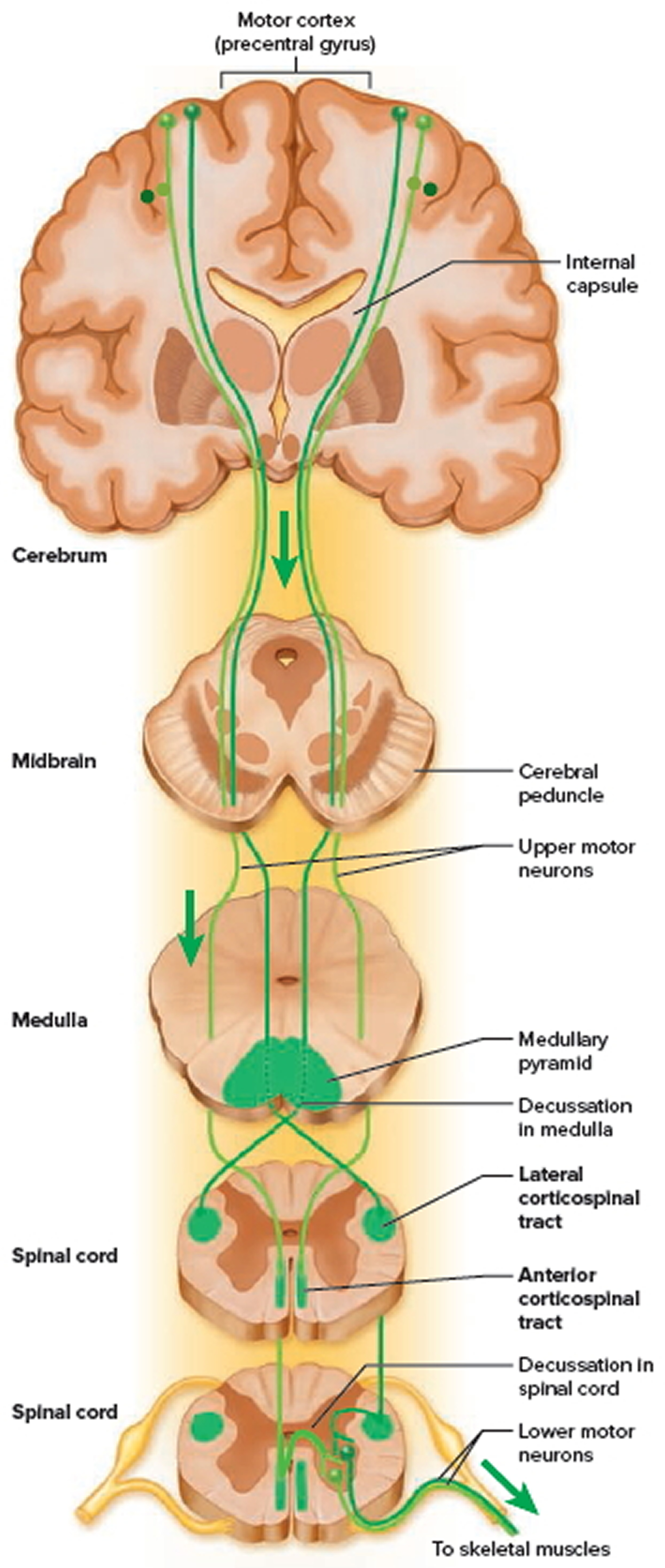
Figure 5. Spinal cord descending tracts from the brain
Ataxic hemiparesis
Ataxic hemiparesis is weakness of one side of the body with incoordination and unsteadiness that result from the brain’s failure to regulate the body’s posture and the strength and direction of limb movements 4. Ataxia is most often caused by disease activity in the cerebellum.
Although ataxia is caused mostly by cerebellar lesions, lesion in the basis pontis, corona radiata, thalamus, posterior limb of internal capsule also cause ataxia with ipsilateral pyramidal signs, and most of these regions are associated with occlusion of posterior circulation 5. Ataxic hemiparesis was initially described as a lacunar syndrome correlating with lacunar infarctions, which resulted from the occlusion of small penetrating arteries. However, recent studies demonstrated that cardioembolic and large-artery atherosclerosis as well as lacunar infarctions cause ataxic hemiparesis 6. Therefore, ataxic hemiparesis is not a rare clinical manifestation among ischemic stroke patients.
Spastic hemiparesis
For those who survive a first-ever stroke, the damage caused to the motor (movement) pathway in the brain as a consequence of the event can lead to post-stroke spasticity.
Spasticity is a movement disorder characterized by muscle overactivity which significantly impedes physical movements. Spasticity does not develop in all people who have had a stroke but in the cases when it does, it can be a cause of major physical and functional impairment. It is important to remember that not all motor impairments that are seen after stroke are caused by spasticity; diminished motor functionality is seen just as commonly in those who do not develop spasticity after a stroke.
In different people spasticity will manifest in different ways and the nature of the post-stroke spasticity will be determined by the degree and location of the damage to the brain as a result of the stroke.
Post-stroke spasticity has a significant impact on voluntary motor functioning which presents many problems for day to day living. If these problems cause pain or significantly impact daily activities it is important that the spasticity is treated to reduce this pain and discomfort. Encouraging evidence has been presented showing that if treatment is initiated early there is a reduced the risk of degeneration of muscle activity, secondary complications and functional impairment. It is for this reason that it is very important that people who have had a stroke take close care monitoring their symptoms so they can keep their doctor up to date and people who have had a stroke and who experience any of these symptoms must attend rehabilitation via a neurologist or rehabilitation physician right away.
Common symptoms of post-stroke spasticity include:
- Muscle stiffness and a feeling of tightness, especially in the upper limbs;
- Loss of control of small movements, like flicking the pages of a book;
- Loss of normal limb movements, like picking up a jar;
- Muscle overactivity leading to a reduced ability to relax. Overactivity of the muscles can be associated with very tight or flexed muscles;
- Muscle spasms like quick jolts of the muscles;
- Changes in limb posture; and
- Muscle fatigue, which feels like the muscles are sore, limp and tired.
People who have had a stroke and who experience any of these symptoms must attend rehabilitation via a neurologist or rehabilitation physician right away.
When the spasticity is acquired through brain or spinal injury/trauma, there is evidence to suggest that timely initiation of treatment will reduce the risk of secondary malformation in muscles and tissue, degeneration of muscle activity and impairments in muscle functioning. Therefore it is imperative you self-monitor your symptoms after a traumatic brain event, such as stroke, and have regular checkups with your doctor to ensure that any spasticity that develops is managed as soon as possible.
Post-stroke spasticity assessment
Post stroke spasticity will vary in severity depending on the nature of the damage caused by the stroke and engaging in different activities and functions will uncover the spasticity in different ways. It is for these reasons that when your doctor is conducting the spasticity assessment they need to be extensive and thorough. The doctor will probably begin with a verbal examination. It is very important when you are asked to describe your symptoms at this stage you are clear and descriptive. This will be the first step in aiding your doctor to establish the correct diagnosis.
A physical assessment of spasticity is then conducted. A wide range of physical and reflex testing is used to develop an appropriate treatment and rehabilitation plan. There are multiple scales and tools available for conducting a physical assessment, each with advantages and disadvantages. Often, to conduct a well-round physical review, more than one tool will need to be used.
Spasticity is most often measured by assessing muscle resistance to passive movements using the Modified Ashworth Scale (MAS) or the Tardieu Scale, which are clinical rating tools. Both scales use a point system a clinical rating tool. The MAS uses a point scale to describe the degree of spasticity in a limb. A score of greater than 0, which is no resistance, indicates spasticity is present.
The degree of spasticity can change with various positions, tasks and movements, and therefore a well-rounded review using multiple tests, settings and movement-related tasks will also be conducted by the doctor.
After the MAS has been conducted and the basic severity of the spasticity has been determined it is important to have an assessment of the impact that spasticity may have on daily life, activity and motor functioning. This is sometimes difficult for a healthcare professional to determine as the degree of spasticity can change with various positions, tasks and movements.
Firstly the healthcare professional will ask questions in a semi-structured interview to determine how the person feels about their condition; are they experiencing pain or discomfort? Are they having difficulties sleeping or performing day to day activities? Are they aware of any increased muscle stiffness?
Then in order to conduct a well-rounded review and capture any activity related manifestations of the condition the following will then be observed and assessed:
- Muscle reflex activity;
- Flexibility;
- Active and rapid movements;
- Balance and risk of falling;
- Manual dexterity;
- Determining the unilateral motor performance (movements on one side of the body) and whether hemiparesis is present;
- The degree of mobility;
- Voluntary muscle activity related to specific activities; and
- Impact of spasticity on personal hygiene, dressing and limb positioning.
These scales will indicate to your doctor the severity of the spasticity but will not help them to understand what impact that spasticity will have on daily life, activity and motor functioning. This information is best provided by you (the person experiencing the symptoms) and it will help the healthcare team to develop a management plan that best suits your lifestyle and post stroke spasticity. The doctor will probably ask questions like:
- How you are coping both physically and mentally with your condition?
- Are you experiencing pain or discomfort?
- Are you having difficulties sleeping or performing day to day activities?
- Are you aware of any increased muscle stiffness?
Once the causes of the impairments have been established through continual observation and evaluation then the stroke rehabilitation program can be developed accordingly.
Post-stroke spasticity treatment
Muscle weakness, muscle overactivity and soft-tissue contracture are the major causes of impairment in spastic limbs, and are therefore the focus points for treatment.
Treatment for spasticity must begin with physical intervention, usually by a physiotherapist or occupational therapist, before any pharmacological options are introduced. Not all people will tolerate pharmaceutical intervention and some types of spasticity will not respond well, if at all. If medication is determined to be a viable option, then the treatment plan will still include a mixture of physical interventions.
The treatment options for spasticity are diverse and, as such, involve a team of people who each bring separate specialities and focus to the rehabilitation program. A neurologist or rehabilitation physician is needed to coordinate the team, which can include general practitioners, nurses, physiotherapists, occupational therapists and neurosurgeons, as well as consultant physicians and specialists. Members of the support base, including family, friends, carers and nursing staff, also play an important role in treatment.
Treatment without medication can range from fairly mild physical interventions to quite invasive surgery that should only be used in the most unmanageable cases.
The first line treatments for spasticity include:
- Avoiding stimuli that may trigger muscle spasticity and further rigidity. These can include urinary tract infections, bladder distention, kidney stones (urolithiasis), bowel impaction, bed sores (decubitus ulcers) and osteomyelitis. If worse than usual spastic symptoms are being experienced, the first action is to rule out these stimuli and treat them if they are present;
- Physical therapies, such as stretching out the muscles, can be efficacious in relieving some of the stiffness and rigidity associated with spasticity. In order to maintain the stretches for a longer period, limb casting can be used;
- Exercise;
- Applying heat or cold packs or cooler sprays is a simple physical therapy that may cause some relief;
- Occupational therapy;
- Bracing and splinting the muscles helps stop spasms, and reduces muscle damage as a result; and
- Ultrasound therapy.
In more severe cases when the spasticity is causing major discomfort and rigidity is severely affecting daily routine, the following options can be considered:
- Short-wave diathermy is a treatment designed to increase blood flow in the problem area in order to reduce pain and promote healing;
- A form of muscle–tendon surgery involving the lengthening and release of the muscle–tendon connections; or
- Procedures to destroy the nerves, such as neurectomy, myeltomy and rhizotomy, are the absolute last line therapy.
Neurodevelopmental treatment
The major aims for post-stroke spasticity treatment are neurodevelopmental, in that the focus is on normalising muscle tone and movement patterns. While muscle tone can be reduced, and accordingly give relief from pain and discomfort, this does not necessarily result in improvements in movement, activity or functioning. Therefore spasticity will only be treated if it is causing pain, discomfort or if it interferes with personal care.
An ingrown toenail, skin reactions, urinary tract infections or stool impaction are known to worsen spasticity and therefore before any treatment is initialized, the doctor will make sure that the spasticity is not worsened due to a manageable condition. If these are present, they need to be treated before physical and pharmacological treatments for post-stroke spasticity are begun.
As with any spasticity treatment program, treatment for post-stroke spasticity must begin with physical intervention before any pharmacological options are introduced, and even then physical therapy will need to remain an active part of the rehabilitation program.
Specific physical therapies which have shown positive improvements in spasticity include:
- Stretching;
- Vibration;
- Splinting of the muscles; and
- EMG biofeedback (helps people to consciously control their muscle tension by being made aware it is happening).
Medications
Pharmacological spasticity treatments are often unsatisfactory as the side effects may be greater than the benefit from the medications. Chemical neurolysis with alcohol and phenol reduces muscle tone effectively for a few months before it needs to be injected again, however repeat injections become less effective over time due to fibrosis (excess collagen in a tissue).
The current leading intervention for treating the spastic muscle is Botulinum toxin (BoNT – Botox) injections directly into the muscles of concern.
Botulinum toxin (BoNTA)
Botulinum toxin (BoNTA – Botox, Dysport) type A is a naturally produced protein which, when administered intramuscularly, can relieve spasticity by blocking acetylcholine release at the neuromuscular junction. BoNTA is considered to be the treatment which most effectively reduces spasticity. It is has been shown to significantly reduce both upper and lower limb spasticity resulting from stroke as indicated by a decrease in the mean MAS score after 4 weeks treatment has been reported to improve quality of life. If BoNTA injections are administrated early in the course of the post stroke spasticity, they may help to reduce overall spasticity. However, your doctor will be able to advise if this treatment is appropriate for you.
Botulinum toxin is considered to be the treatment that most effectively reduces spasticity. It combats the major impairment associated with function reduction in spastic muscles by:
- Reducing spastic co-contraction;
- Decreasing spastic dystonia; and
- Helping to ease the stretching and lengthening of the muscle.
Botox side effects can develop when the toxin spreads. It is important to seek medical attention immediately if any difficulties in speech, breathing or swallowing occur.
Medications with spasticity reduction as a primary indication include:
- Oral or intrathecal baclofen (e.g. Lioresal, Baclohexal, GenRX Baclofen, Clofen);and
- Dantrolene (Dantrium).
Other effective agents used to treat spasticity, although not primarily indicated for it, include:
- Gabapentin (e.g. Neurontin, Gabatine, Gabaran, Nupentin, GenRX Gabapentin, Pendine);
- Pregabalin (Lyrica)
- Tiagabine (Gabitril);
- Diazepam (e.g. Diazepam Elixir, Ducene);
- Clonidine (Catapres); and
- Tizanidine.
It is sometimes necessary for people to use alternative administration methods if oral administration is difficult, and to ensure the medication is fully absorbed. For example, intrathecal injections of baclofen (Lioresal Intrathecal) or dantolene (Dantrium Powder for Injection) be used instead of oral medication.
Post-stroke spasticity prognosis
Usually post-stroke spasticity symptoms will develop to their maximum severity by 3 months after the event. After this time any progression of spasticity is believed to be due to changes in the muscles as a result of the spasticity.
Post-stroke spasticity is often associated with secondary complications, pain and impaired motor performance. Quite commonly people will compensate for certain aspects of their spasticity with certain movements and postures and as a result changes in muscles and soft-tissues can develop.
Once spasticity symptoms have developed they may not persist. Initial blood circulation disturbances or transient cerebral oedema may be responsible for symptoms of spasticity immediately after the stroke which may subside completely within 3 months. This indicates the importance of continual evaluation by a neurologist and physiotherapist after a stroke.
If you have developed post-stroke spasticity and experience pain as a consequence, or if your spasticity is significantly interfering with daily activities, you must be treated and treatment should begin as soon as possible. There is evidence to suggest that timely initiation of treatment will reduce the risk of secondary malformation in muscles and tissue, degeneration of muscle activity and impairments in muscle functioning. Therefore it is imperative you self-monitor your symptoms after a stroke and have regular checkups with your doctor to ensure that any spasticity that develops is managed as soon as possible.
Hemiparesis vs Hemiplegia
Hemiplegia is total paralysis of one side of your body, including one arm and one leg. Hemiplegia may come on suddenly, or develop slowly over time. A condition related to hemiplegia, spastic hemiplegia, causes the muscles to get stuck in a contraction, resulting in little muscle control, chronic muscle pain, and unpredictable movements. People with hemiplegia often show other signs of brain damage or head injury and may experience issues with other areas of their bodies.
Hemiplegia, like other forms of paralysis, is characterized by significant loss of sensation and control in the affected area. People with hemiplegia may experience intermittent pain and may be better able to control their limbs at some times than at others.
Hemiparesis causes
Certain risk factors contribute to having a stroke. Some risk factors for stroke can be changed, treated, or controlled. For example, high blood pressure is the biggest risk factor for stroke. High blood pressure can be controlled. Other risk factors include:
- Smoking
- Being overweight.
- Being inactive.
- Uncontrolled diabetes.
- High cholesterol.
- Over age 55 years.
- Family history of stroke.
- Being African American.
- Being female.
- Having a previous stroke or transient ischemic attack (TIA).
Neurologic deficits reflect the area of brain involved. Anterior circulation stroke typically causes unilateral symptoms. Posterior circulation stroke can cause unilateral or bilateral deficits and is more likely to affect consciousness, especially when the basilar artery is involved.
Stroke Syndromes:
- Middle cerebral artery (common): Contralateral hemiparesis (worse in the arm and face than in the leg), dysarthria, hemianesthesia, contralateral homonymous hemianopia, aphasia (if the dominant hemisphere is affected) or apraxia and sensory neglect (if the nondominant hemisphere is affected)
- Anterior cerebral artery (uncommon): Contralateral hemiparesis (maximal in the leg), urinary incontinence, apathy, confusion, poor judgment, mutism, grasp reflex, gait apraxia
- Lacunar infarcts:
- Absence of cortical deficits plus one of the following:
- Pure motor hemiparesis
- Pure sensory hemianesthesia
- Ataxic hemiparesis
- Dysarthria–clumsy hand syndrome
- Posterior cerebral artery: Contralateral homonymous hemianopia, unilateral cortical blindness, memory loss, unilateral 3rd cranial nerve palsy, hemiballismus
- Vertebrobasilar system: Unilateral or bilateral cranial nerve deficits (e.g., nystagmus, vertigo, dysphagia, dysarthria, diplopia, blindness), truncal or limb ataxia, spastic paresis, crossed sensory and motor deficits*, impaired consciousness, coma, death (if basilar artery occlusion is complete), tachycardia, labile BP. (Note: *Ipsilateral facial sensory loss or motor weakness with contralateral body hemianesthesia or hemiparesis indicates a lesion at the pons or medulla)
Risk factors for stroke
The following are the modifiable factors that contribute the most to increased risk of stroke:
- Hypertension
- Cigarette smoking
- Dyslipidemia
- Diabetes
- Insulin resistance 7
- Abdominal obesity
- Alcoholism
- Lack of physical activity
- High-risk diet (eg, high in saturated fats, trans fats, and calories)
- Psychosocial stress (eg, depression)
- Heart disorders (particularly disorders that predispose to emboli, such as acute MI, infective endocarditis, and atrial fibrillation)
- Hypercoagulability (thrombotic stroke only)
- Intracranial aneurysms (subarachnoid hemorrhage only)
- Use of certain drugs (eg, cocaine, amphetamines)
- Vasculitis
- Unmodifiable risk factors include the following:
- Prior stroke
- Older age
- Family history of stroke
Stroke stages
Following a stroke, the brain and body progress through the following series of stages 8:
- Transischemic attack
- Flaccidity
- Spasticity
- Synergy
A gradual progression from one stage to the next usually occurs; however, the stages are not mutually exclusive but instead can occur simultaneously in the affected limb.
Flaccid stage
Once the inciting injury to the brain occurs, the flaccid stage evolves with a state of areflexia. This stage of areflexia includes loss of muscle tone and volitional motor activity, variable sensory loss, and loss of muscle stretch reflexes.
Muscular support of the humeral head in the glenoid fossa by the supraspinatus and deltoid muscles is lost. This leads to downward and outward subluxation of the humeral head, with the only support coming from the joint capsule.
The shoulder capsule is thin and is composed of 2 tissue layers. The inner synovial layer, the stratum synovium, is highly vascular but poorly innervated, making it insensitive to pain but highly reactive to heat and cold. The outer layer, the stratum fibrosum, is poorly vascularized but richly innervated, predisposing it to pain from stretch. For this reason, Faghri and coauthors 9 suggest that added capsular stretch in a flaccid shoulder may predispose the capsule to irreversible damage and the shoulder to pain.
Flaccidity of the trapezius, rhomboids, and serratus anterior muscles leads to depression, protraction, and downward rotation of the scapula, which Cailliet 8 believes leads to significant angular changes of the glenoid fossa, subsequently contributing to subluxation. Also, the spine begins to flex laterally toward the hemiparetic side because of the elimination of the righting reflex, further altering the scapulothoracic relationship.
However, Prevost and colleagues 10 compared the affected and unaffected shoulders by using a 3-dimensional (3-D) radiographic technique that determines the true position of the humeral head in relation to the scapula. This technique revealed less downward rotation of the glenoid fossa than originally expected, and no significant relationship was found between the extent of scapular orientation and the severity of subluxation.
Subsequently, it was concluded that scapular position does not contribute as much to inferior subluxation as was originally thought. Teasell points out that this now appears to be the most widely accepted viewpoint 11.
Spastic stage
As stroke recovery evolves, flaccidity may progress to spasticity. Cailliet explained that normally, the brainstem contains upper extremity flexor patterns and lower extremity extensor patterns that are refined and coordinated by the premotor and neocortexes 8. Following a stroke, the connections that control these reflexes can be interrupted, resulting in the release of these basic patterns and the evolution of spasticity and synergy patterns.
If the neurologic deficits become severe enough, primitive tonic neck reflexes may develop. When such neck reflexes are present, the elbow extends when the head turns toward the affected side, and the elbow flexes when the head turns away. The presence of primitive tonic neck reflexes is considered to be prognostically unfavorable for motor recovery.
The first evidence of upper extremity spasticity is internal rotation of the humerus from the subscapularis and pectoralis major; there is debate as to which muscle contributes more strongly to this pattern. The pattern may then progress into the forearm pronators (ie, pronator quadratus, pronator teres, flexor carpi radialis).
Spastic involvement of the rhomboids leads to scapular depression and downward rotation, while the latissimus dorsi contributes to adduction, extension, and internal rotation of the humerus. Biceps brachii spasticity further depresses the head of the humerus and flexes the elbow.
Teasell noted that as spasticity and synergy evolve, there is a failure of the antagonist muscles to relax when the agonist muscles contract, thus creating cocontraction 11. For example, during internal rotation, excessive spasticity of the internal rotators of the humerus (ie, subscapularis, pectoralis major, latissimus, teres major) overwhelms the external rotators (ie, supraspinatus, infraspinatus, teres minor).
The muscles causing downward and outward rotation of the scapula, the rhomboids, overwhelm the trapezius and serratus anterior muscles. Spastic, unilateral paraspinal muscles overwhelm those on the contralateral side, causing lateral flexion of the spine toward the affected side.
Synergy stage
If neurologic impairment of the completed stroke progresses, synergy patterns, which tend to worsen with initiated efforts, may emerge. Cailliet 8 proposes that the synergy component that usually occurs first is spastic elbow flexion; the shoulder phase is weaker and usually requires a more reflexive status to occur.
The restrictions created by the synergy patterns create therapeutic challenges to attaining meaningful upper extremity function. Upper extremity flexor synergy patterns include the following:
- Shoulder/scapular depression (downward rotation and retraction)
- Humeral adduction/internal rotation
- Elbow flexion
- Forearm pronation (rarely supination)
- Wrist/finger flexion (thumb-in-hand position)
When treating patients in flexion synergy, aim therapy at retraining the overwhelmed agonists, stressing the desired components of function, and releasing the uninhibited flexion patterns by initiating opposite movements at the “key points of control.”
Stroke prevention
Changing those risk factors you can control will help reduce your risk of stroke. This includes:
- Stop smoking.
- Reduce your alcohol intake.
- Control your blood pressure.
- Control your cholesterol.
- Control your blood sugar with medicine, diet, and exercise if you have diabetes.
- Get regular physical activity
- Maintain a healthy weight.
Have regular checkups so that your doctor can help you manage health conditions that increase your risk of having a stroke. Ask your doctor for advice on making lifestyle changes to decrease your risk of stroke. Talk to your doctor about whether taking aspirin in low doses would help reduce your risk of stroke or transient ischemic attack. Aspirin can help keep your blood from forming clots that block your arteries. If taking low-dose aspirin is right for you, it is important to follow your doctor’s instructions so that you get the most benefit with the fewest side effects.
How is stroke diagnosed?
Immediate medical care is critical after having a stroke. Your doctor will ask about your symptoms and health history. Then he or she will perform a physical exam. Your doctor also will want to check your blood pressure and listen to your heart. He or she will want to know if you fell and suffered a head injury. If your doctor suspects you have had a stroke, you will have more tests. These tests include:
- Blood tests. This will give your doctor information about how quickly your blood is clotting, your blood sugar levels, a chemical imbalance, and infection.
- Controlling how quickly your blood clots and your blood sugar level is necessary to prevent further damage.
- Computerized tomography (CT) brain scan. A CT scan is similar to an X-ray. This test will be performed on your head to see your brain. Pictures from the scan can tell your doctor if you have had bleeding, a tumor, a stroke, or other medical conditions. Sometimes, a dye will be injected into your arm to “light up” your blood vessels. This gives your doctor better details of what’s going on in your brain and neck.
- Magnetic resonance imaging (MRI). An MRI is another type of scan that allows your doctor to see your brain. An MRI is sensitive enough to examine damaged brain tissue and bleeding. Sometimes, a dye is used for an MRI, as well.
- Carotid ultrasound. This test uses sound waves to create pictures of the inside of the carotid arteries in your neck. It can show your doctor how well your blood is flowing through your carotid arteries. Also, it shows whether you have a buildup of fatty deposits (plaques) in those arteries.
- Cerebral angiogram. This test involves inserting a thin, flexible tube into your groin (near your upper thigh). The tube travels through your major arteries and into your carotid artery. Dye is used for this test too. Once it is in, an X-ray will help your doctor get a clear view of the arteries in your neck and brain.
- Transesophageal echocardiogram. An echocardiogram uses sound waves to give your doctor clear pictures of your heart. An echocardiogram can detect the source of blood clots in your heart that may have traveled to your brain and caused your stroke. During this test, a flexible tube attached to a small device (transducer) is inserted down your throat. It connects the back of your mouth to your stomach. This gives your doctor clear pictures of your heart and any blood clots.
Hemiparesis treatment
Hemiparesis treatment depends on treating the underlying cause of hemiparesis. There’s no single treatment approach that works for all people. Instead, treatment is largely dependent on the cause of hemiparesis. Some treatment options include:
- Blood thinners to reduce cardiovascular blockages and decrease the chances of future strokes.
- Antibiotics, usually delivered intravenously, to combat brain infections.
- Surgery to remove swelling on the brain or objects lodged in the brain.
- Muscle relaxant drugs.
- Surgery to address secondary issues, particularly involuntary muscle contractions, spinal damage, or damage to the ligaments or tendons on the unaffected side of the body.
- Physical therapy designed to help the brain work around the injuries. Physical therapy can also strengthen the unaffected side and help you reduce the loss of muscle control and tone.
- Support groups, family education, and advocacy.
- Psychotherapy to help you deal with the psychological effects of the disease.
- Exercise therapy to help you remain healthy in spite of your disability.
Stroke treatment
Quick, emergency care is important in treating a stroke. Emergency room treatment depends on whether you had an ischemic or hemorrhagic stroke. Immediate treatment options include the use of blood-thinning (clot bluster) medicine, surgery, or other procedures.
Following immediate treatment, controlling the underlying health conditions that caused your stroke is important. That means controlling your diabetes, blood pressure, cholesterol, and making lifestyle changes.
Stroke rehabilitation is an important part of recovery after a stroke. It helps build your strength, coordination, endurance, and confidence. A main goal of stroke rehabilitation is to help you learn how to live with the effects of the stroke. This will help you be as independent as possible. It may include physical therapy, occupational therapy, speech therapy, and swallowing therapy. Your doctor will decide what kind of rehabilitation will be helpful for you. Rehabilitation can begin as soon as the stroke is over and you are stable. In many cases, it starts in the hospital as soon as 24 to 48 hours after a stroke. Most people need to continue rehabilitation for months or years after a stroke.
If you have a loved one who had a stroke, he or she will need your help and support. Some places offer classes for stroke survivors and their families. You may be able to go to some of your loved one’s rehabilitation sessions. This is a good way to learn how stroke rehabilitation works and how you can help your loved one get better.
Find out what he or she can do alone, what they can do with help, and what they can’t do at all. Tell the rehabilitation staff what activities your loved one enjoys. Help your loved one practice the skills learned in stroke rehabilitation. For example, avoid helping your loved one do things that he or she is able to do alone. Practicing skills will build your loved one’s confidence.
Living with stroke
Living with stroke will mean managing your health conditions that cause it. Also, it will mean living with the temporary or permanent side effects. The following are the most common side effects of stroke:
- Weakness or paralysis on one side of the body.
- Problems with speech and language.
- Poor balance or clumsy movement.
- Ignoring or being unaware of one side of the body.
- Trouble swallowing.
- Problems with bladder or bowel control.
- Problems with memory, thinking, or problem solving.
- Poor vision and/or changes in vision.
- Numbness.
Brain injury and loss of function from a stroke can lead to emotional changes, too. Soon after the stroke, you may have trouble controlling your emotions. Your moods may change more quickly than they did before the stroke. For example, you may suddenly start crying or laughing for no reason. Usually, this gets better over time.
It is normal to feel depressed, sad, or frustrated as you get used to the changes caused by a stroke. These reactions can be treated. Talk to your doctor about how you are feeling so that he or she can help.
Driving is another issue if you have had a stroke. Your doctor can advise you if it is safe for you to drive again. Having a stroke can affect your mobility, vision, and thinking. Your reaction time may be slower. These changes can make driving a car unsafe for you and for other people on the road. If your doctor says that it is safe for you to drive again, contact your state’s department of motor vehicles. Ask about the rules for people who have had a stroke. You may have to take a driving test or a class. Driver training programs are often available through rehabilitation centers.
It can be frustrating if you can’t drive after having a stroke. Other options for getting around include public transportation, specialized vans, taxis, and getting rides from friends and family members. Community resources such as senior citizen groups and local volunteer agencies may also be able to help.
References- Strategies for stroke rehabilitation. Lancet Neurol. 2004 Sep; 3(9): 528–536. doi: 10.1016/S1474-4422(04)00851-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164204/
- Dobkin B. The clinical science of neurologic rehabilitation. New York: Oxford University Press; 2003.
- The relation between impairments and functional outcomes poststroke. Patel AT, Duncan PW, Lai SM, Studenski S. Arch Phys Med Rehabil. 2000 Oct; 81(10):1357-63.
- An overview of the patient with ataxia. Mariotti C, Fancellu R, Di Donato S. J Neurol. 2005 May; 252(5):511-8.
- Fisher CM. Ataxic hemiparesis: a pathologic study. Arch Neurol. 1978;35:126–8.
- Hiraga A. Ataxic hemiparesis. In: Manto M, Gruol DL, Schmahmann J, Koibuchi N, Rossi F, editors. Handbook of the cerebellum and cerebellar disorders. Dordrecht: Springer; 2013. pp. 1669–86.
- Kernan WN, Viscoli CM, Furie KL, et al: Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med 374 (14):1321–1331, 2016. doi: 10.1056/NEJMoa1506930
- Cailliet R. The shoulder in the hemiplegic patient. Shoulder Pain. 3rd ed. FA Davis; 1991. 193-226.
- Faghri PD, Rodgers MM, Glaser RM, Bors JG, Ho C, Akuthota P. The effects of functional electrical stimulation on shoulder subluxation, arm function recovery, and shoulder pain in hemiplegic stroke patients. Arch Phys Med Rehabil. 1994 Jan. 75(1):73-9.
- Prévost R, Arsenault AB, Dutil E, Drouin G. Shoulder subluxation in hemiplegia: a radiologic correlational study. Arch Phys Med Rehabil. 1987 Nov. 68(11):782-5.
- Teasell RW. The painful hemiplegic shoulder. Physical Medicine and Rehabilitation: State of the Art Reviews. 1998. 12(3):489-500.