What is a hymen
Hymen is a very thin piece of skin-like tissue with a small, circular opening in the center that partly covers the opening of the vagina. The first time a girl has sex the hymen stretches and may tear and bleed a little. That is why people say the hymen is “broken.” Other things also can cause the hymen to stretch, such as putting in a tampon (although that usually doesn’t happen).
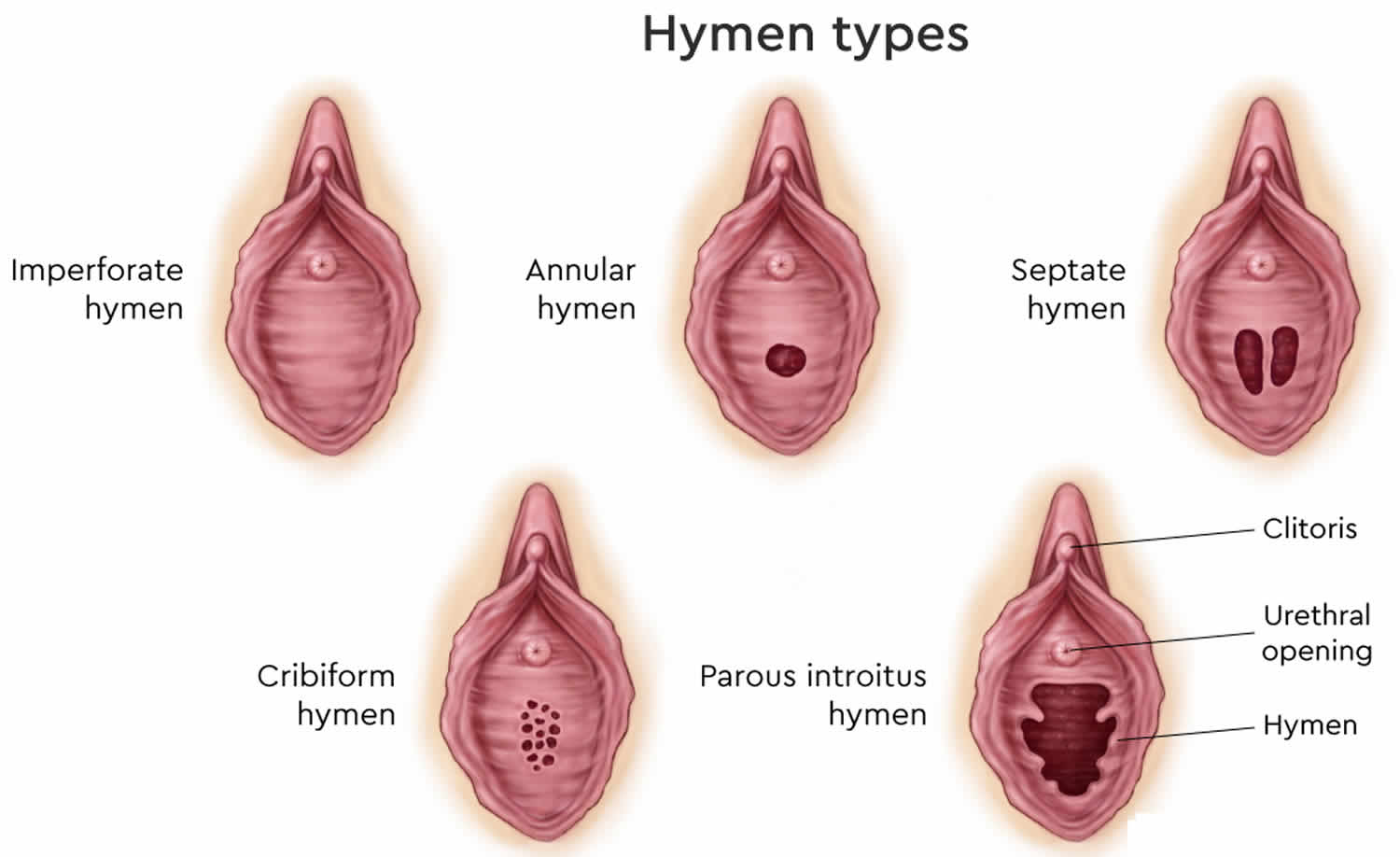
Hymens are often different from person to person. Hymens can come in different shapes. The most common hymen in young women is shaped like a half moon. This shape allows menstrual blood to flow out of the vagina.
Most women find their hymens have stretched or torn after their first sexual experience, and the hymen may bleed a little (this usually causes little, if any, pain). Some women who have had sex don’t have much of a change in their hymens, though.
Figure 1. Hymen types
Hymen types
Imperforate hymen
In the case of a completely imperforate hymen, this membrane does not have an opening, so it blocks the vaginal canal. “Imperforate” means lacking the normal opening. Imperforate hymen is the most common congenital (present at birth) genital tract anomaly in females ranging from 1/1000 to 1/10,000 in prevalence 1. If the hymen is only partially imperforate, there is a small opening to the vagina, but extra tissue prevents the vagina from being completely open. Imperforate hymens can vary in the amount of obstruction.
Imperforate hymen is the most common type of blockage of the vagina. Imperforate hymen is something a girl is born with. No one knows why this happens. There is nothing that the mother did to cause it.
An imperforate hymen can sometimes be diagnosed at birth. More often, the diagnosis is made during the teen years. Imperforate hymen presentation is often late with amenorrhea in adolescence 2. Menstrual blood cannot flow out of the vagina. This usually causes the blood to back up into the vagina which often develops into a vaginal mass and abdominal and/or back pain. Some girls may also have pain with bowel movements and trouble passing urine. Hydrocolpos is cystic dilation of the vagina with fluid accumulation due to stimulation of secretory glands of the reproductive tract secondary to vaginal obstruction. Hydrocolpos may lead to obstructive uropathy through the compression of the lower urinary tract, resulting in hydronephrosis and hydroureters 3.
The treatment for an imperforate hymen is minor surgery to remove the extra hymenal tissue and create a normal sized vaginal opening so that menstrual blood can flow out of the vagina.
Figure 2. Imperforate hymen
[Source 2 ]Imperforate hymen causes
An imperforate hymen is caused by failure of the hymen to perforate (open) during a baby’s growth and development inside her mother’s uterus.
Who gets an imperforate hymen?
An imperforate hymen is a condition that girls are born with. It generally affects 1 to 2% of all girls. Nobody knows why it occurs.
Imperforate hymen signs and symptoms
Signs in a newborn:
- A complete imperforate hymen may be detected in a newborn. There may be a bulge in the hymeneal membrane that is caused by a buildup of normal mucus in the vagina that cannot drain.
Symptoms in an older girl:
In an older girl, a complete imperforation completely blocks menstrual flow, which causes abdominal pain. It may also cause other signs and symptoms such as:
- Amenorrhea (lack of period)
- Fullness in the lower abdomen
- Difficulty urinating or having a bowel movement
- Back pain
Partially imperforate hymen signs and symptoms
- A partially imperforate hymen does not block menstrual flow. Your daughter may complain of pain or trouble inserting and removing tampons. This symptom is usually not associated with other abnormalities of the vagina, uterus and ovaries.
Imperforate hymen diagnosis
Girls can be diagnosed with imperforate hymen at any age. It is most often diagnosed at birth or later at puberty.
At birth or early childhood, your doctor may see that there is no opening in the hymen during a physical exam.
At puberty, girls usually do not have any problems from an imperforate hymen until they start their period. The imperforate hymen blocks the blood from flowing out. As the blood backs up the vagina, it causes:
- Mass or fullness in the lower part of the belly (from the build up of blood that can’t come out)
- Stomach pain
- Back pain
- Problems with urinating and bowel movements
The provider will do a pelvic exam. The provider may also do a pelvic ultrasound and imaging studies of the kidneys. This is done to ensure that the problem is imperforate hymen rather than another problem. The provider may recommend that the girl see a specialist to make sure that the diagnosis is imperforate hymen.
Imperforate hymen treatment
A minor surgery can fix an imperforate hymen. The surgeon makes a small cut or incision and removes the extra hymen membrane.
- Girls who are diagnosed with imperforate hymen as babies most often have surgery when they are older and have just started puberty. The surgery is done in early puberty when breast development and pubic hair growth has begun.
- Girls who are diagnosed when they are older have the same surgery. The surgery allows retained menstrual blood to leave the body.
Girls recover from this surgery in a few days.
After surgery, the girl may have to insert dilators into the vagina for 15 minutes each day. A dilator looks like a tampon. This keeps the incision from closing on itself and keeps the vagina open.
After treatment
After girls recover from the surgery, they will have normal periods. They can use tampons, have normal sexual intercourse, and have children.
What is the prognosis for imperforate hymen surgery?
Once the imperforate hymen has been surgically corrected, there should be no long-term issues. The vagina will function normally and your teenager will be able to comfortably have periods and use tampons if desired. Surgery does not interfere with the ability to have children in the future.
Septate hymen
A half moon of thin membrane normally surrounds a young girl’s vagina. A septate hymen is when the thin hymenal membrane has a band of extra tissue in the middle that causes two small vaginal openings instead of one. Young women with a septate hymen may have trouble getting a tampon in or trouble getting a tampon out after it expands with blood. Sexual intercourse will usually tear the extra tissue away, but there is also a minor surgery that can remove the extra tissue and create a normal sized vaginal opening.
After a septate hymen is successfully removed or tears on its own, you or your daughter should have a normal sexual and reproductive life. If a septate hymen isn’t removed, it will create infertility or provide a form of natural contraception.
What causes a septate hymen?
A septate hymen forms during embryological development when the tubes that eventually become a vagina don’t fuse together properly.
Septate hymen symptoms
Th symptoms of a septate hymen can include:
- trouble inserting or removing a tampon
- pain or bleeding during sexual intercourse when the hymen tears.
How is a septate hymen diagnosed?
Usually, a septate hymen doesn’t cause a problem until a girl’s teenage years. During an examination, your daughter’s gynecologist can confirm that there is a band of extra tissue running down the middle of her hymen.
How is a septate hymen treated?
Doctors will perform a minor surgical procedure to remove the extra tissue obstructing your daughter’s vagina.
Microperforate hymen
A microperforate hymen is a thin membrane that almost completely covers the opening to the vagina. Menstrual blood and mucus are usually able to flow out of the vagina but the opening is very small. Since it’s flowing through such a small hole, the period may last longer than the normal 4- to 7-day cycle. A young woman with a microperforate hymen usually will not be able to insert a tampon into her vagina and may not realize that she has a very tiny opening. If she is able to place a tampon into her vagina, she may not be able to remove it when it becomes filled with blood. Sometimes a microperforate hymen resolves spontaneously as the girl grows older, or it may tear away with some pain when she inserts a tampon or when she has sexual intercourse. There is also a minor surgery than can remove the extra tissue and create a normal sized vaginal opening.
What causes microperforate hymen?
A microperforate hymen occurs during embryological development when the hymenal tissue doesn’t form properly. After a microperforate hymen is successfully removed or tears on its own, your daughter should have a normal sexual and reproductive life.
Microperforate hymen symptoms
Common symptoms of microperforate hymen include:
- periods that last longer than the normal four to seven days
- inability to insert a tampon, or pain upon inserting one
- pain or bleeding during sexual intercourse when the hymen tears
How is microperforate hymen diagnosed?
Usually, a microperforate hymen doesn’t cause a problem until a girl’s teenage years. During an examination, your daughter’s gynecologist can confirm that there is extra tissue covering her hymen.
How is microperforate hymen treated?
Your daughter will undergo a minor surgical procedure to remove the microperforate hymen.
Hymen surgery
Hymen reconstruction surgery, which is also referred to as hymenorrhaphy or hymenoplasty, is defined as the process of restoring the hymeneal membrane’s gross anatomical integrity 4. Among the medical profession, hymen reconstruction receives particular attention and is debated because the surgery is not medically indicated and reveals contradictory social norms regarding virginity and marriageability for girls/women 5. A virgin is someone who has never had sexual intercourse. The belief that bed sheets must be stained with blood after first intercourse during the wedding night, as a sign of virginity, contradicts with the medical evidence that blood loss after first coitus does not always occur 6, and with the fact that there is a wide variety of appearances of the hymen in virgin girls and women 7. Moreover, an ‘intact hymen’ is not always a sign of not having engaged in sexual activity as there are other ways of preserving virginity while at the same time having engaged in sexual intercourse 8. Hymen reconstruction surgery is framed both as an operation that promotes certain harmful gender norms and at the same time, serves as a way of protecting young women and girls from the stigma or violence associated with ‘losing their virginity before marriage’ 9. Some studies showed that for some women who undergo hymen reconstruction, it is seen as a pragmatic choice, that allows them to meet societal expectations of virginity, marriageability and also avoid further acts of violence 10.
Hymen reconstruction surgery involves the restoration of the hymeneal membrane’s gross anatomical integrity.
Hymen reconstruction surgery complications include hemorrhage necessitated a new operation to achieve hemostasis, dyspareunia (painful sex) and the formation of a hematoma.
- Lacroix AE, Langaker MD. Physiology, Menarche. [Updated 2019 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470216[↩]
- Ramphul M, Perry L, Bhatia C. Neonatal imperforate hymen with hydrocolpos. BMJ Case Rep. 2016;2016:bcr2016215434. Published 2016 May 31. doi:10.1136/bcr-2016-215434 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4904433[↩][↩]
- Imperforate hymen causing bilateral hydroureteronephrosis in an infant with bicornuate uterus. Eksioglu AS, Maden HA, Cinar G, Tasci Yildiz Y. Case Rep Urol. 2012; 2012():102683.[↩]
- Leye E, Ogbe E, Heyerick M. ‘Doing hymen reconstruction’: an analysis of perceptions and experiences of Flemish gynaecologists. BMC Womens Health. 2018;18(1):91. Published 2018 Jun 13. doi:10.1186/s12905-018-0587-z https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6001123[↩]
- Johnsdotter S, Essen B. Genitals and ethnicity: the politics of genital modifications. Reprod Health Matters. 2010;18:29–37. doi: 10.1016/S0968-8080(10)35495-4[↩]
- Ayuandini S. Finger pricks and blood vials: how doctors medicalize ‘cultural’ solutions to demedicalize the ‘broken’ hymen in the Netherlands. Soc Sci Med. 2017;77:61–68. doi: 10.1016/j.socscimed.2017.01.016[↩]
- Adams JA, Botash AS, Kellogg N. Differences in Hymenal morphology between adolescent girls with and without a history of consensual sexual intercourse. Arch Pediatr Adolesc Med. 2004;158:280–285. doi: 10.1001/archpedi.158.3.280[↩]
- El Kak F, El Salibi N, Yasmine R, Ghandour L. Hymen protection and the sexual practices, perceptions, and attitudes of female university students from Lebanon. Int J Gynaecol Obstet. 2017;139:1–9. doi: 10.1002/ijgo.12285[↩]
- Cook RJ, Dickens BM. Hymen reconstruction: ethical and legal issues. Int J Gynaecol Obstet. 2009;107:266–269. doi: 10.1016/j.ijgo.2009.07.032[↩]
- Wild V, Poulin H, McDougall CW, Stöckl A, Biller-Andorno N. Hymen reconstruction as pragmatic empowerment? Results of a qualitative study from Tunisia. Soc Sci Med. 2015;147:54–61. doi: 10.1016/j.socscimed.2015.10.051[↩]