Hyperkalemia
Hyperkalemia is the medical term that describes a potassium level in your blood that is greater than 5 mEq/L or greater than 5 mmol/L (Kim MJ, Valerio C, Knobloch GK. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2023 Jan;107(1):59-70.https://www.aafp.org/pubs/afp/issues/2023/0100/potassium-disorders-hypokalemia-hyperkalemia.html)), 1. Your blood potassium level is normally between 3.5 to 5.0 millimoles per liter (mmol/L) or 3.5 to 5.0 milliequivalent per liter (mEq/L) 2, 3, 4, 5, 6.
Potassium is a nutrient that is critical to the function of nerve and muscle cells, including those in your heart 7. Many people get all their potassium they need from what they eat and drink. And most people have an adequate intake of potassium. The body uses what it requires and the kidneys eliminate the rest in the urine. The body tries to keep the blood potassium level within a very narrow range. Levels are mainly controlled by aldosterone, a hormone produced by the adrenal glands that lie above your kidneys.
Sources of potassium in the diet include:
- Fruits, such as dried apricots, prunes, raisins, and bananas
- Vegetables, such as acorn squash, potatoes, spinach, tomatoes, collards and broccoli
- Lentils, kidney beans, soybeans, and nuts
- Milk and yogurt
- Meats, poultry, and fish
- Fruit from vines, such as grapes and blackberries
- Root vegetables, such as carrots and potatoes
- Citrus fruits, such as oranges and grapefruit
Your kidneys help to keep the right amount of potassium in your body. If you have chronic kidney disease, your kidneys may not remove extra potassium from the blood. Some medicines also can raise your potassium level. You may need a special diet to lower the amount of potassium that you eat.
In healthy people with normal kidney function, high dietary potassium intakes do not pose a health risk because the kidneys eliminate excess potassium in the urine 8. Although case reports indicate that very large doses of potassium supplements can cause heart abnormalities and death, the National Academies of Sciences, Engineering, and Medicine committee concluded that these reports do not provide sufficient evidence to set a Tolerable Upper Intake Level (UL) 9. In addition, there is no evidence that high intakes of potassium cause hyperkalemia in adults with normal kidney function or other adverse effects. Therefore, the committee did not set a Tolerable Upper Intake Level (UL) for potassium 9.
However, in people with impaired urinary potassium excretion due to chronic kidney disease or the use of certain medications, such as angiotensin converting enzyme (ACE) inhibitors or potassium-sparing diuretics, even dietary potassium intakes below the Adequate Intake (see Table 1) can cause hyperkalemia 9. Hyperkalemia can also occur in people with type 1 diabetes, congestive heart failure, adrenal insufficiency, or liver disease 10, 11. Individuals at risk of hyperkalemia should consult a physician or registered dietitian about appropriate potassium intakes from all sources.
Often a report of high blood potassium isn’t true hyperkalemia also known as pseudohyperkalemia. Instead, pseudohyperkalemia (false elevation in measured potassium) may be caused by the rupture of blood cells in the blood sample during or shortly after the blood draw due to specimen collection, handling, or other causes 12, 13. The ruptured cells leak their potassium into the sample. This falsely raises the amount of potassium in the blood sample, even though the potassium level in your body is actually normal. When this is suspected, a repeat blood sample is done 13.
Hyperkalemia is usually found when your doctor has ordered blood tests to help diagnose a condition you’re already experiencing or to monitor medications you’re taking. Hyperkalemia is usually not discovered by chance. A potassium blood test is used to detect abnormal concentrations of potassium, including high potassium (hyperkalemia) and low potassium (hypokalemia). It is often used as part of an electrolyte panel or basic metabolic panel for a routine physical. Talk to your doctor about what your results mean. You may need to change a medication that’s affecting your potassium level, or you may need to treat another medical condition that’s causing your high potassium level.
While mild hyperkalemia is usually asymptomatic, very high potassium levels (blood potassium level higher than 6.0 mmol/L) may cause life-threatening cardiac arrhythmias, heart palpitations, muscle weakness, paralysis and paresthesias (a burning or prickling sensation in the extremities) and requires immediate treatment 12, 10, 11, 14. Symptoms usually develop at higher levels, 6.5 mEq/L to 7 mEq/L, but the rate of change is more important than the numerical value 12.
Patients with chronic hyperkalemia may be asymptomatic at increased levels, while patients with dramatic, acute potassium shifts may develop severe symptoms at lower ones 12. Infants have higher baseline levels than children and adults 12.
Talk to your doctor about what your results mean. Hyperkalemia should always be confirmed before aggressive treatment in cases where the serum potassium is elevated without explanation 12. True hyperkalemia may be caused by increased potassium intake, transcellular movement of intracellular potassium into the extracellular space, and decreased renal excretion. The urgency of therapy depends on symptoms, serum levels, and causes of hyperkalemia 15, 16. You may need to change a medication that’s affecting your potassium level, or you may need to treat another medical condition that’s causing your high potassium level. Treatment of high potassium is often directed at the underlying cause. In some instances, you may need emergency medications or dialysis.
What is Potassium?
Potassium (K+) is a mineral that is vital to cell metabolism. Potassium is a major intracellular cation (positively charged ion) and a type of electrolyte that plays a significant role in the regulation of fluid volume and maintenance of the water-electrolyte balance 2, 17, 18. Potassium is present in all body tissues and is required for normal cell function because of its role in maintaining intracellular fluid volume and transmembrane electrochemical gradients 19, 20. Potassium helps transport nutrients into cells and removes waste products out of cells. Potassium is essential for the proper functioning of the heart, kidneys, muscles, nerves, and digestive system. Potassium is also important in muscle function, helping to transmit messages between nerves and muscles 19.
Potassium (K+) is a positively charged ion (cation), which is present throughout your body in both intracellular and extracellular fluids. The majority of body potassium, > 90%, are intracellular. It moves freely from intracellular fluid (ICF) to extracellular fluid (ECF) and vice versa when adenosine triphosphate (ATP) increases the permeability of the cell membrane. Potassium (K+) is mainly replaced inside or outside the cells by another cation, sodium (Na+). The movement of potassium into or out of the cells is linked to certain body hormones and also to certain physiological states. Standard laboratory tests measure extracellular fluid (ECF) potassium. Potassium enters the body rapidly during food ingestion. Insulin is produced when a meal is eaten; this causes the temporary movement of potassium from extracellular fluid (ECF) to intracellular fluid (ICF). Over the ensuing hours, the kidneys excrete the ingested potassium and homeostasis is returned. In the critically ill patient, suffering from high potassium level or hyperkalemia, this mechanism can be manipulated beneficially by administering high concentration (50%) intravenous glucose. Insulin can be added to the glucose, but glucose alone will stimulate insulin production and cause movement of potassium from extracellular fluid (ECF) to intracellular fluid (ICF). The stimulation of alpha receptors causes increased movement of potassium from intracellular fluid (ICF) to extracellular fluid (ECF). A noradrenaline infusion can elevate serum potassium levels. An adrenaline infusion, or elevated adrenaline levels, can lower serum potassium levels. Metabolic acidosis causes a rise in extracellular potassium levels (hyperkalemia). In this situation, excess of hydrogen ions (H+) are exchanged for intracellular potassium ions, probably as a result of the cellular response to a falling blood pH. Metabolic alkalosis causes the opposite effect, with potassium moving into the cells 21.
Potassium (K+), along with other electrolytes such as sodium (Na+), chloride (Cl–), and bicarbonate (HCO3–), helps regulate the amount of fluid in your body and maintains a stable acid-base balance. Potassium is present in all body fluids, but most potassium is found within the cells (intracellularly). Only a small amount is present in fluids outside the cells and in the liquid part of the blood (called serum or plasma).
The total amount of potassium (K+) in the adult body is about 45 millimole (mmol)/kg body weight (about 140 g for a 175 pound adult; 1 millimole [mmol] = 1 milliequivalent [mEq] = 39.1 mg of potassium) 22. Most potassium are found within the cells (intracellularly) and a small amount is in extracellular fluid. The intracellular concentration of potassium is about 30 times higher than the extracellular concentration, and this difference forms a transmembrane electrochemical gradient that is maintained via the Sodium-Potassium ATPase pumps (Na+-K+ ATPase ion pumps) 23. When activated, the sodium-potassium ATPase pump (Na+-K+ ATPase ion pumps) exchanges 2 extracellular potassium (K+) ions for 3 intracellular sodium (Na+) ions, influencing membrane potential based on physiological excitation or inhibition. These sodium-potassium ATPase pumps (Na+-K+ ATPase ion pumps) are partially responsible, along with the sodium-potassium-chloride (Na+-K+-2Cl) co-transporter and sodium-calcium (Ca) exchanger, for maintaining the potential difference across the resting cell membrane as well. In addition to maintaining cellular tonicity, this gradient is required for proper nerve transmission, muscle contraction, and kidney function 19, 24, 25.
Potassium (K+) homeostasis depends on external balance (dietary intake [typically 100 mmol per day] versus excretion [95% via the kidney; 5% via the colon]) and internal balance (the distribution of potassium (K+) between intracellular and extracellular fluid compartments). The uneven distribution of potassium (K+) across cell membranes means that a mere 1% shift in its distribution can cause a 50% change in plasma potassium (K+) concentration 18. Hormonal mechanisms involving insulin, beta-adrenergic agonists and aldosterone modulate potassium (K+) distribution by promoting rapid transfer of potassium (K+) across the plasma membrane 26. Your body uses what potassium (K+) it requires and your kidneys eliminate the rest in the urine. Your body tries to keep the blood potassium level within a very narrow range. Levels are mainly controlled by aldosterone, a hormone produced by the adrenal glands in the kidneys. Extrarenal potassium (K+) losses from the body are usually small, but can be marked in individuals with chronic diarrhea, severe burns or prolonged sweating 18, 26. Under normal circumstances, the kidney’s distal nephron secretes potassium (K+) and determines final urinary excretion. In patients with low potassium levels or hypokalemia (plasma K+ concentration <3.5 mmol/l), after the exclusion of extrarenal causes, alterations in sodium ion (Na+) delivery to the distal nephron, aldosterone status, or a specific inherited or acquired defect in distal nephron function (each of which affects distal nephron K+ secretion), should be considered 18.
Figure 1. Potassium physiology
Because most potassium (K+) ions are found within the cells (a major intracellular cation), it is widely distributed in foods once derived from living tissues. Potassium concentration is higher in fruits and vegetables than in cereals and meat. You get most of the potassium you need from the foods that you eat and most people have an adequate intake of potassium. Recommended adequate intakes for potassium were set by the Food and Nutrition Board of the Institute of Medicine at 4700 mg/day 20. However it should be noted that the Food and Nutrition Board of the Institute of Medicine Recommended adequate intakes (AIs) for potassium at 4700 mg/day for adults is substantially higher than the World Health Organization’s (WHO) guidelines, which recommend 3150 mg/day for adults 27. The National Health and Nutrition Examination Survey (NHANES) data indicates that 99.2% of potassium in the US diet is naturally occurring, with the remaining 0.8% coming from fortified foods 28. These naturally occurring potassium sources include milk and other non-alcoholic beverages, as well as potatoes and fruit, which rank highest as sources of potassium intake among American adults 29. In addition, Western dietary practices with higher consumption of cereal, low nutrient density processed foods and lower consumption of fruits and vegetables has led to a diet lower in potassium and higher in sodium in recent decades 20. Salting foods and discarding the liquid induces sodium (Na+) for potassium (K+) exchange and reduces the potassium content of foods. Few Americans meet the recommended intakes; the average intake is 2591 ± 9 mg/day 28. This large gap between potassium intakes and recommended intakes led to potassium being called a shortfall nutrient in the Dietary Guidelines for Americans 30.
Actual potassium requirements would vary with an individual’s genetics, blood pressure (BP) status, and sodium intake 19. Blood pressure is currently the primary criterion for determining potassium requirements, with African Americans being more vulnerable to high blood pressure (hypertension) and more responsive to potassium supplementation than whites; individuals with high blood pressure (hypertension) are more responsive to increasing potassium intakes than individuals with normal blood pressure, and potassium having a greater benefit for those consuming a high salt diet 31. Other benefits of increasing potassium consumption may include improved blood sugar (glucose) control, glucose intolerance and insulin resistance becoming a concern for individuals with high blood pressure (hypertension) prescribed potassium wasting diuretics (water pills) 32. These differences support personalized nutrition approaches. Understanding movement of potassium within the body may help to improve these health outcomes.
Potassium is absorbed via passive diffusion, primarily in the small intestine 23. About 90% of ingested potassium is absorbed and used to maintain its normal intracellular and extracellular concentrations 33. There is around 50 mEq/kg of potassium (K+) in the body such that total body potassium (K+) in a 70-kg person is 3,500 mEq. Around 98% of potassium (K+) is found mainly within cells, and about 2% of the bodies’ potassium (K+) is in the extracellular fluid. The normal concentration of potassium (K+) in the extracellular fluid is 3.5–5.3 mEq/L. Large deviations from these values are not compatible with life.
Approximately 90% of the daily potassium (K+) intake is excreted in the urine, whereas a smaller percentage (10%) is excreted by the gastrointestinal tract in the stool and a very small amount is lost in sweat 34, 26, 35. Therefore, within the body, the kidney is the major organ responsible for potassium (K+) homeostasis. The kidneys control potassium excretion in response to changes in dietary intakes, and potassium excretion increases rapidly in healthy people after potassium consumption, unless body stores are depleted 19. The kidney facilitates potassium (K+) homeostasis by adjusting renal potassium (K+) excretion over several hours in response to a potassium load. Initial changes in extracellular potassium (K+) concentration are buffered by movement of potassium (K+) into or out of skeletal muscle cells. Internal potassium (K+) balance is a term used to refer to regulation of potassium (K+) distribution between the intracellular and extracellular space. Insulin, catecholamines, and, to a lesser extent, aldosterone are critical factors responsible for maintaining the normal internal distribution of potassium (K+) 26, 35.
The kidneys can adapt to variable potassium intakes in healthy individuals even in the setting of high dietary intake, but a minimum of 5 mmol (about 195 mg) potassium is excreted daily in urine 22. To demonstrate this, studies have shown potassium (K+) levels are kept within the normal range even when there are increases to ~15 g daily of dietary potassium (K+) intake sustained for 20 days 36, 37. Recent findings have identified the presence of an enteric potassium (K+) sensing mechanism that initiates the renal secretory process upon K+ entry into the gastrointestinal tract 35. The distal convoluted tubule has been identified as a site critical for potassium (K+) homeostasis, where it acts as a potassium (K+) sensor capable of initiating potassium (K+) excretion independent of mineralocorticoid activity 35. Combined with other obligatory losses, potassium balance cannot be achieved with intakes less than about 400–800 mg/day 26, 35.
Assessing potassium status is not routinely done in clinical practice, and it is difficult to do because most potassium in the body is inside cells 38. Although blood potassium levels can provide some indication of potassium status, they often correlate poorly with tissue potassium stores 22, 39, 40. Other methods to measure potassium status include collecting balance data (measuring net potassium retention and loss); measuring the total amount of potassium or the total amount of exchangeable potassium in the body; and conducting tissue analyses (e.g., muscle biopsies), but all have limitations 39.
Normal serum concentrations of potassium range from about 3.6 to 5.0 mmol/L and are regulated by a variety of mechanisms 22, 10. Diarrhea, vomiting, kidney disease, use of certain medications, and other conditions that alter potassium excretion or cause transcellular potassium shifts can cause low potassium level also called hypokalemia (serum potassium levels below 3.6 mmol/L) or high potassium level also called hyperkalemia (serum potassium levels above 5.0 mmol/L) 10. Otherwise, in healthy individuals with normal kidney function, abnormally low or high blood levels of potassium are rare.
Because the blood concentration of potassium is so small, minor changes can have significant consequences. If potassium levels are too low (serum potassium levels below 3.6 mmol/L) or too high (serum potassium levels above 5.0 mmol/L), there can be serious health consequences; a person may be at risk for developing shock, respiratory failure, or heart rhythm disturbances. An abnormal potassium level can alter the function of the nerves and muscles; for example, the heart muscle may lose its ability to contract.
Your body needs potassium to:
- Build proteins
- Break down and use carbohydrates
- Build muscle
- Maintain normal body growth
- Control the electrical activity of the heart
- Control the acid-base balance
Reduced potassium consumption has been associated with hypertension and cardiovascular diseases, and appropriate consumption levels could be protective against these conditions 41. A recent meta-analysis including 11 cohort studies reported an inverse association between potassium intake and risk of stroke 42. Additionally, two meta-analyses of trials comparing increased potassium to lower potassium intake found that increased potassium intake lowers blood pressure 43, 44. These results were further supported by a systematic review without a meta-analysis, which concluded that increased potassium intake results in decreased blood pressure in adults 45. Thus, a public health intervention aimed at increasing potassium intake from food could be a cost-effective strategy to reduce the burden of cardiovascular morbidity and mortality. Moreover, increasing potassium consumption from food in the population is safe; in individuals without renal impairment caused by medical conditions or drug therapy, the body is able to efficiently adapt and excrete excess potassium via the urine when consumption 46.
The American Heart Association recommended potassium intake for an average adult is 4,700 milligrams (mg) per day. Most of us aren’t getting nearly that much. On average, adult males eat almost 3,200 mg/day, and adult females eat about 2,400 mg/day 47. Remember that potassium is only part of an overall heart-healthy eating pattern. Other dietary factors that may affect blood pressure include amount and type of dietary fat; cholesterol; protein, sugar and fiber; calcium and magnesium, and of course, sodium.
For example, the DASH (Dietary Approaches to Stop Hypertension) diet study found that a diet rich in fruits, vegetables, fat-free or low-fat (1 percent) milk and milk products, whole-grain foods, fish, poultry, beans, seeds and unsalted nuts reduced blood pressure compared to a typical American diet. The DASH eating plan also had less sodium; sweets, added sugars and sugar-containing beverages; saturated and trans fats; and red meats than the typical American diet.
People with kidney problems, especially those on dialysis, should not eat too many potassium-rich foods. Your health care provider will recommend a special diet.
What does potassium do?
Potassium (K+) is the principal positively charged ion (cation) in the fluid inside of cells, while sodium (Na+) is the principal cation in the extracellular fluid. Potassium (K+) concentrations are about 30 times higher inside than outside cells, while sodium (Na+) concentrations are more than 10 times lower inside than outside cells 48. The concentration differences of these charged particles causes a difference in electric potential between the inside and outside of cells, known as the membrane potential. A cell’s membrane potential is maintained by ion pumps in the cell membrane, especially the Sodium-Potassium ATPase pumps (Na+-K+ ATPase ion pumps). These sodium-potassium ATPase pumps (Na+-K+ ATPase ion pumps) use ATP (energy) to pump sodium (Na+) of the cell and potassium (K+) into the cell, leading to a potassium (K+) gradient across the cell membrane [potassium (K+) in > potassium (K+) out], which is partially responsible for maintaining the cell membrane potential (Figure 2). The sodium-potassium ATPase pumps (Na+-K+ ATPase ion pumps) activity has been estimated to account for 20%-40% of the resting energy consumption in a typical adult 48. The large proportion of energy dedicated to maintaining sodium/potassium concentration gradients emphasizes the importance of this function in sustaining life 48. The cell membrane potential created by potassium and sodium ions allows the cell generate an action potential–a “spike” of electrical discharge. The ability of cells to produce electrical discharge is critical for body functions such as nerve impulse transmission, muscle contraction, and heart function 49, 50, 51.
Potassium is also an essential mineral needed to regulate water balance, blood pressure and levels of acidity 52. The more potassium you eat, the more sodium you pass out of the body through urine. Increased potassium intake has no adverse effect on blood lipid concentration, catecholamine concentrations, or renal function in apparently healthy adults without impaired renal handling of potassium 47. The largest benefit was detected when sodium intake was more than 4 g/day, which is the intake of most populations globally 53, so increased potassium intake should benefit most people in most countries. However, the authors also found a statistically significant decrease in blood pressure with increased potassium when sodium intake was 2-4 g/day. Therefore, increased potassium can continue to be beneficial in terms of blood pressure even as individuals and populations decrease their sodium intake. Studies examining both nutrients simultaneously support this concept, showing an increased benefit with simultaneous reduction in sodium and increase in potassium compared with changes in one nutrient individually 54, 55.
Potassium also helps relax blood vessel walls, which helps lower blood pressure 47.
World Health Organization recommends an increase in potassium intake from food to reduce blood pressure and risk of cardiovascular disease, stroke and coronary heart disease in adults. World Health Organization suggests a potassium intake of at least 90 mmol/day (3510 mg/day) for adults (conditional recommendation) 46.
Potassium also acts as a cofactor for some enzymes activity. For example, the activation of Na+/K+-ATPase requires the presence of sodium and potassium. The presence of potassium is also required for the activity of pyruvate kinase, an important enzyme in carbohydrate metabolism 56.
Figure 2. Sodium-Potassium ATPase pump
What are normal potassium levels?
Normal serum potassium values are between 3.5 to 5.0 millimoles/L (mmol/L) or 3.5 to 5.0 milliequivalent/L (mEq/L) 2, 3, 4, 5. However, there can be slight variation between laboratories and for this reason, it is important to look for the specific reference interval listed on your test report. Potassium levels outside this range, 3.5 to 5.0 millimoles/L (mmol/L) or 3.5 to 5.0 milliequivalent/L (mEq/L), are not compatible with life with increased rates of death from several causes 57, 58.
Your health care provider may order a potassium blood test as part of your regular checkup or to monitor an existing condition, such as diabetes, kidney disease, or adrenal gland disorders. You may also need this test if you take medicines that could affect your potassium levels or if you have symptoms of having too much or too little potassium.
Interpretation of a potassium test requires carefully considering the result, the laboratory reference range, and your health situation. Because potassium is frequently measured with other electrolytes, levels may be evaluated together. For a blood test, the report should list the amount of potassium measured in either milliequivalents per liter (mEq/L) or millimoles per liter (mmol/L). The test report will also show a reference range, which the laboratory considers an expected range for potassium levels.
How much potassium do I need?
The amount of potassium you need each day depends on your age and sex. Average daily recommended amounts are listed below in milligrams (mg). Table 1 lists the current Adequate Intakes (AIs) for potassium for healthy individuals. Intake recommendations for potassium and other nutrients are provided in the Dietary Reference Intakes (DRIs) developed by an expert committee of the Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine 20. Dietary Reference Intake (DRI) is the general term for a set of reference values used for planning and assessing nutrient intakes of healthy people. These values, which vary by age and sex, include:
- Recommended Dietary Allowance (RDA): Average daily level of intake sufficient to meet the nutrient requirements of nearly all (97%–98%) healthy individuals; often used to plan nutritionally adequate diets for individuals.
- Adequate Intake (AI): Intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an RDA.
- Estimated Average Requirement (EAR): Average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals.
- Tolerable Upper Intake Level (UL): Maximum daily intake unlikely to cause adverse health effects.
When the Food and Nutrition Board evaluated the available data in 2005, it found the data insufficient to derive an Estimated Average Requirement (average daily level of intake estimated to meet the requirements of 50% of healthy individuals; usually used to assess the nutrient intakes of groups of people and to plan nutritionally adequate diets for them; can also be used to assess the nutrient intakes of individuals) for potassium, so the board established Adequate Intake (intake at this level is assumed to ensure nutritional adequacy; established when evidence is insufficient to develop an Recommended Dietary Allowance) for all ages based on potassium intakes in healthy populations 8. In 2019, a National Academies of Sciences, Engineering, and Medicine committee updated the Dietary Reference Intake (DRI) for potassium and sodium 20. The committee found the data insufficient to derive an Estimated Average Requirement (EAR) for potassium. Therefore, they established Adequate Intakes (AIs) for all ages based on the highest median potassium intakes in healthy children and adults, and on estimates of potassium intakes from breast milk and complementary foods in infats. The National Academies of Sciences, Engineering, and Medicine committee also used an expanded Dietary Reference Intake (DRI) model to include a recommended intake level for a nutrient to reduce the risk of chronic disease, what they termed the chronic disease risk reduction intake 8. In 2019, a National Academies of Sciences, Engineering, and Medicine committee updated the Dietary Reference Intake (DRI) for potassium and sodium 20. According to the model, a chronic disease risk reduction intake might be set for a nutrient like potassium when there is a causal relationship between a certain level of intake and a reduced risk of chronic disease based on evidence of at least moderate strength. However, the committee found the evidence to be insufficient to derive a chronic disease risk reduction intake for potassium 20.
Table 1. Average daily recommended intake for Potassium
| Birth to 6 months | 400 mg |
|---|---|
| Infants 7–12 months | 860 mg |
| Children 1–3 years | 2,000 mg |
| Children 4–8 years | 2,300 mg |
| Children 9–13 years (boys) | 2,500 mg |
| Children 9–13 years (girls) | 2,300 mg |
| Teens 14–18 years (boys) | 3,000 mg |
| Teens 14–18 years (girls) | 2,300 mg |
| Adults 19+ years (men) | 3,400 mg |
| Adults 19+ years (women) | 2,600 mg |
| Pregnant teens | 2,600 mg |
| Pregnant women | 2,900 mg |
| Breastfeeding teens | 2,500 mg |
| Breastfeeding women | 2,800 mg |
Footnote: *Adequate Intakes (AIs) do not apply to individuals with impaired potassium excretion because of medical conditions (e.g., kidney disease) or the use of medications that impair potassium excretion.
[Source 38 ]Signs and symptoms of hyperkalemia
The clinical presentation of hyperkalemia is highly variable with some patients presenting with an acute illness whilst others may be asymptomatic. Hyperkalemia is usually found when your doctor has ordered blood tests to help diagnose a condition you’re already experiencing or to monitor medications you’re taking. Hyperkalemia is usually not discovered by chance. The presence of arrhythmias, muscular weakness or paresthesia (burning or prickling sensation) in a patient at risk should raise the clinical suspicion of hyperkalemia. The clinical course is unpredictable and sudden death can occur in the absence of premonitory ECG changes. Recognition of hyperkalemia depends on laboratory tests and the ECG appearances.
If you have symptoms of hyperkalemia, particularly if you have kidney disease or are taking medications that raise your potassium level, call your doctor immediately. Hyperkalemia is a serious and potentially life-threatening disorder. It can cause:
- Muscle fatigue
- Weakness
- Paralysis
- Difficulty breathing
- Abnormal heart rhythms (arrhythmias) – slow, weak, or irregular pulse
- Palpitations
- Nausea or vomiting
- Chest pain
- Sudden collapse, when the heartbeat gets too slow or even stops
Talk to your doctor about what your results mean. You may need to change a medication that’s affecting your potassium level, or you may need to treat another medical condition that’s causing your high potassium level 59. Treatment of high potassium is often directed at the underlying cause. In some instances, you may need emergency medications or dialysis.
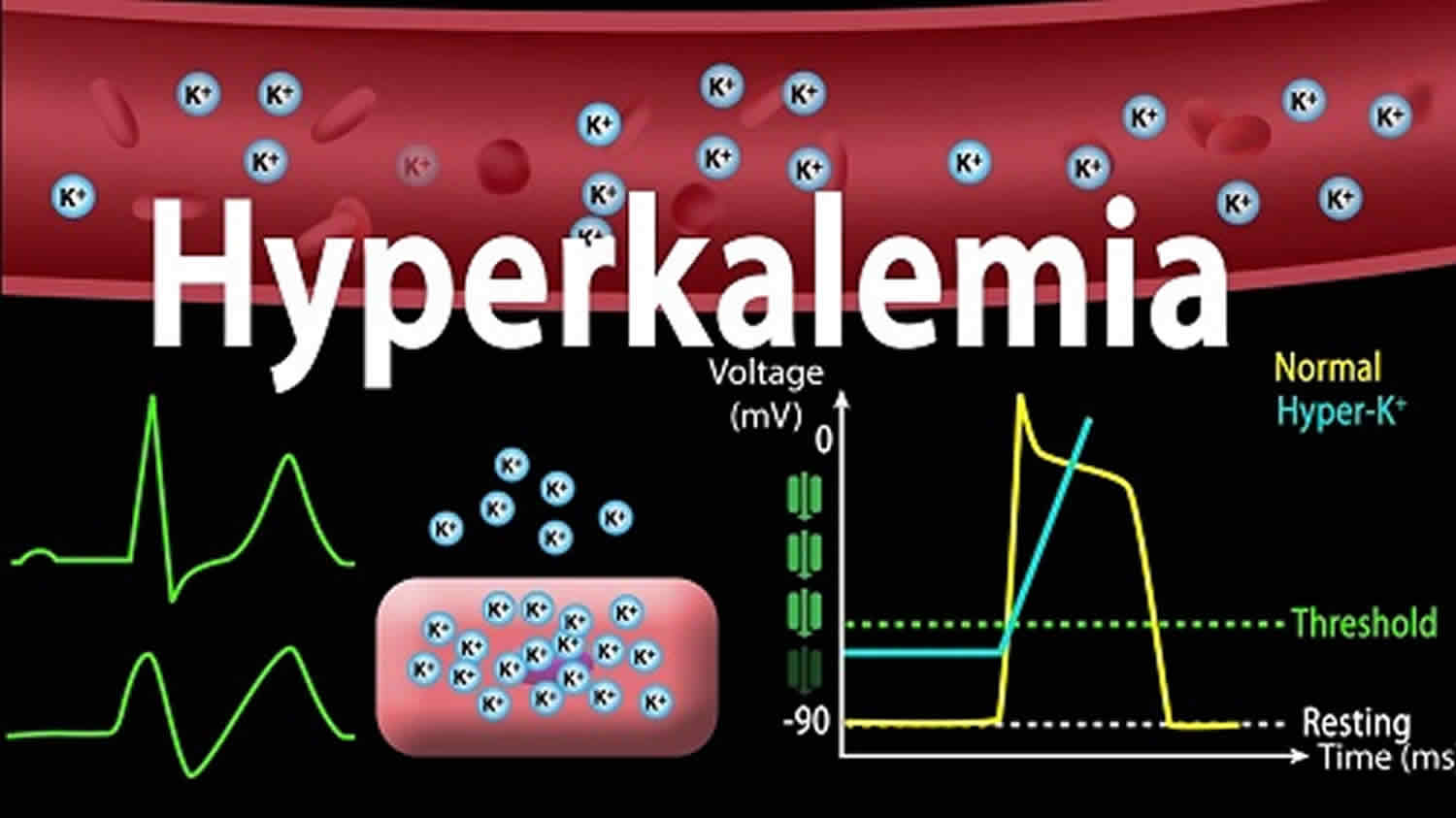
Signs of hyperkalemia
Hyperkalemia causes a rapid reduction in resting membrane potential leading to increased cardiac depolarization, and muscle excitability. This in turn can cause electrocardiographic (ECG or EKG) changes 60. The electrocardiographic (ECG or EKG) changes with hyperkalemia do not consistently follow a stepwise, dose-dependent pattern. In reality, many patients have rapid changes in their ECG. The risk of arrhythmias increase with potassium values > 6.5 mmol/L and even small elevations in potassium above this concentration can lead to rapid progression from peaked T waves to ventricular fibrillation or asystole 61. The longer a patient has high potassium concentrations, the greater the risk of sudden deterioration 62.
ECG changes in hyperkalemia
With mild to moderate hyperkalemia, there is reduction of the size of the P wave and development of peaked T waves. Severe hyperkalemia results in a widening of the QRS complex, and the ECG complex can evolve to a sinusoidal shape. There appears to be a direct effect of elevated potassium on some of the potassium channels that increases their activity and speeds membrane repolarization. Also, hyperkalemia causes an overall membrane depolarization that inactivates many sodium channels. The faster repolarization of the cardiac action potential causes the tenting of the T waves, and the inactivation of sodium channels causes a sluggish conduction of the electrical wave around the heart, which leads to smaller P waves and widening of the QRS comple.
Figure 3. Hyperkalemia EKG changes
Hyperkalemia causes
The most common cause of high blood potassium or hyperkalemia is pseudohyperkalemia, which is not reflective of the true serum potassium levels 12. Instead, pseudohyperkalemia may be caused by the rupture of blood cells in the blood sample (hemolysis of the sample) during or shortly after the blood draw. The ruptured blood cells leak their potassium into the sample. This falsely raises the amount of potassium in the blood sample (pseudohyperkalemia), even though the potassium level in your body is actually normal. When this is suspected, a repeat blood sample is done. Hemolysis is more common when a syringe is used than a vacuum device. Using tourniquets and excessive fist-pumping during the blood draw also increase the risk. Specimens drawn from patients with leukocytosis or thrombocytosis are also frequently associated with falsely elevated potassium concentrations 12.
The most common cause of genuinely high potassium (hyperkalemia) is related to your kidneys, such as 63:
- Acute kidney failure also called acute renal failure or acute kidney injury occurs when your kidneys suddenly become unable to filter waste products from your blood. Acute kidney failure can occur when 64:
- You have a condition that slows blood flow to your kidneys. Diseases and conditions that may slow blood flow to the kidneys and lead to kidney injury include:
- Blood or fluid loss
- Blood pressure medications
- Heart attack
- Heart disease
- Infection
- Liver failure
- Use of aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, others) or related drugs
- Severe allergic reaction (anaphylaxis)
- Severe burns
- Severe dehydration
- You experience direct damage to your kidneys. Diseases, conditions and agents that may damage the kidneys and lead to acute kidney failure include:
- Blood clots in the veins and arteries in and around the kidneys
- Cholesterol deposits that block blood flow in the kidneys
- Glomerulonephritis, inflammation of the tiny filters in the kidneys (glomeruli)
- Hemolytic uremic syndrome, a condition that results from premature destruction of red blood cells
- Infection, such as with the virus that causes coronavirus disease 2019 (COVID-19)
- Lupus, an immune system disorder causing glomerulonephritis
- Medications, such as certain chemotherapy drugs, antibiotics and dyes used during imaging tests
- Scleroderma, a group of rare diseases affecting the skin and connective tissues
- Thrombotic thrombocytopenic purpura, a rare blood disorder
- Toxins, such as alcohol, heavy metals and cocaine
- Muscle tissue breakdown (rhabdomyolysis) that leads to kidney damage caused by toxins from muscle tissue destruction
- Breakdown of tumor cells (tumor lysis syndrome), which leads to the release of toxins that can cause kidney injury
- Your kidneys’ urine drainage tubes (ureters) become blocked and wastes can’t leave your body through your urine. Diseases and conditions that block the passage of urine out of the body (urinary obstructions) and can lead to acute kidney injury include:
- Bladder cancer
- Blood clots in the urinary tract
- Cervical cancer
- Colon cancer
- Enlarged prostate
- Kidney stones
- Nerve damage involving the nerves that control the bladder
- Prostate cancer
- You have a condition that slows blood flow to your kidneys. Diseases and conditions that may slow blood flow to the kidneys and lead to kidney injury include:
- Chronic kidney disease also called chronic kidney failure, involves a gradual loss of kidney function. Chronic kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years. Diseases and conditions that cause chronic kidney disease include 65:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis, an inflammation of the kidney’s filtering units (glomeruli)
- Interstitial nephritis, an inflammation of the kidney’s tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis
Glomerular filtration rate (GFR) is a measure of how well your kidneys filter blood and it is equal to the total of the filtration rates of the functioning nephrons in the kidney 66. Normal GFR varies according to age, sex, and body size; in young adults, it is approximately 120 mL/minute/1.73 m² and declines with age. Acute or chronic kidney disease hyperkalemia is usually not seen until the glomerular filtration rate (GFR) falls below 30 mL/min/1.73 m² 12. This is commonly due to primary kidney dysfunction but may be due to acute volume depletion from dehydration or bleeding or decreased circulating blood volume due to congestive heart failure or cirrhosis. Tubular dysfunction due to aldosterone deficiency or insensitivity can also cause hyperkalemia.
Other causes of hyperkalemia include:
- Addison’s disease (adrenal failure). Disease in which the adrenal glands do not make enough aldosterone hormone (and cortisol), reducing the kidneys’ ability to remove potassium from the body
- Alcoholism or heavy drug use that causes rhabdomyolysis, a breakdown of muscle fibers that results in the release of potassium into the bloodstream
- Certain drugs can also cause high potassium in a small percent of people; among them are:
- Non-steroidal anti-inflammatory drugs (NSAIDs),
- Angiotensin-converting enzyme (ACE) inhibitors,
- Angiotensin 2 receptor blockers (ARBs),
- Beta blockers (such as propanolol and atenolol),
- Angiotensin-converting enzyme inhibitors (such as captopril, enalapril, and lisinopril), and
- Potassium-sparing diuretics (such as triamterene, amiloride, and spironolactone).
- Dehydration (which is when the body doesn’t have enough water and other fluids to work properly)
- Destruction of red blood cells due to severe injury or burns
- Excessive use of potassium supplements
- In patients on intravenous (IV) fluids, excessive IV potassium
- Type 1 diabetes
- Infection
ACE inhibitors and angiotensin receptor blockers (ARBs)
ACE inhibitors, such as benazepril (Lotensin®), and angiotensin 2 receptor blockers (ARBs) such as losartan (Cozaar®), are used to treat hypertension and heart failure, slow progression of kidney disease in patients with chronic kidney disease and type 2 diabetes, and decrease morbidity and mortality after myocardial infarction 67. These medications reduce urinary potassium excretion, which can lead to hyperkalemia. Experts recommend monitoring potassium status in people taking ACE inhibitors or angiotensin receptor blockers (ARBs), especially if they have other risk factors for hyperkalemia, such as impaired kidney function 67.
Potassium sparing diuretics
Potassium-sparing diuretics, such as amiloride (Midamor®) and spironolactone (Aldactone®), reduce the excretion of potassium in the urine and can cause hyperkalemia 68. Experts recommend monitoring potassium status in people taking these medications, especially if they have impaired kidney function or other risk factors for hyperkalemia 68.
Loop and thiazide diuretics
Treatment with loop diuretics, such as furosemide (Lasix®) and bumetanide (Bumex®), and thiazide diuretics, such as chlorothiazide (Diuril®) and metolazone (Zaroxolyn®), increases urinary potassium excretion and can lead to hypokalemia 68. Experts recommend monitoring potassium status in people taking these medications, and initiating potassium supplementation if warranted.
Intracellular potassium shifts
Cellular injury can release large quantities of intracellular potassium into the extracellular space. This can be due to rhabdomyolysis from a crush injury, excessive exercise, or other hemolytic processes. Metabolic acidosis may cause intracellular potassium to shift into the extracellular space without red cell injury. Metabolic acidosis is most frequently caused by decreased, effective circulating arterial blood volume. Sepsis or dehydration may lead to hypotension and decreased tissue perfusion leading to metabolic acidosis with subsequent potassium elevation.
Insulin deficiency and diabetic ketoacidosis may cause dramatic extracellular shifts causing measured serum potassium to be elevated in the setting of whole-body potassium depletion. Certain medications, such as succinylcholine, may cause severe, acute potassium elevations in patients with up-regulation of receptors, particularly in subacute neuromuscular disease. Tumor lysis syndrome, particularly in patients receiving chemotherapy for hematogenous malignancy, may cause acute hyperkalemia due to massive cancer cell death 69.
Hyperkalemic periodic paralysis (hyperPP or hyperKPP) is a rare, autosomal dominant condition caused by a mutation in the SCN4A gene that codes for voltage-gated sodium channel causing potassium to shift into the extracellular space due to impaired sodium channel function in skeletal muscle 70, 71. Hyperkalemic periodic paralysis (hyperPP) is characterized by attacks of flaccid limb weakness (which may also include weakness of the muscles of the eyes, throat, breathing muscles, and trunk), hyperkalemia (serum potassium concentration greater than 5 mmol/L) or an increase of serum potassium concentration of at least 1.5 mmol/L during an attack of weakness and/or provoking/worsening of an attack by oral potassium intake, normal serum potassium between attacks, and onset before age 20 years 72, 71. In approximately half of affected individuals, attacks of flaccid muscle weakness begin in the first decade of life, with 25% reporting their first attack at age ten years or older 71. Initially infrequent, the attacks then increase in frequency and severity over time until approximately age 50 years, after which the frequency of attacks declines considerably 71. The major attack trigger is eating potassium-rich foods; other triggers include: cold environment; rest after exercise, stress, or fatigue; alcohol; hunger; and changes in activity level. A spontaneous attack commonly starts in the morning before breakfast, lasts for 15 minutes to one hour, and then passes. Individuals with hyperPP frequently have myotonia (muscle stiffness), especially around the time of an episode of weakness. Paramyotonia (muscle stiffness aggravated by cold and exercise) is present in about 45% of affected individuals. More than 80% of individuals with hyperkalemic periodic paralysis (hyperPP) older than age 40 years report permanent muscle weakness and about one third develop a chronic progressive myopathy 71. Hyperkalemic periodic paralysis (hyperPP) is caused by a mutation in the SCN4A gene that codes for voltage-gated sodium channel Na1.4 70. Several diagnostic modalities exist in assisting diagnosis, such as genetic testing, although they are not always definitive. In case of diagnostic uncertainty, a provocative test can be employed, although the availability of genetic testing and electrophysiologic studies largely obviates the need for such dangerous tests. Treatment for hyperkalemic periodic paralysis (hyperPP) is both proactive and reactive, with avoidance of triggers being the mainstay of therapy. At the onset of weakness, attacks may be prevented or aborted with mild exercise and/or oral ingestion of carbohydrates, intravenously injected glucocorticoids, inhalation of salbutamol, or intravenous calcium gluconate 71. Hyperkalemic attacks of weakness can be prevented by frequent meals rich in carbohydrates; continuous use of a thiazide diuretic or a carbonic anhydrase inhibitor; and avoidance of potassium-rich medications and foods, fasting, strenuous work, and exposure to cold 71.
Increased potassium intake
Increased potassium intake from food is a very uncommon cause of hyperkalemia in adult patients with normal kidney function but can be an important cause in those with kidney disease. Foods with high potassium content include dried fruits, seaweed, nuts, molasses, avocados, and Lima beans. Many vegetables that are also high in potassium include spinach, potatoes, tomatoes, broccoli, beets, carrots, and squash. High-potassium-containing fruits include kiwis, mangoes, oranges, bananas, and cantaloupe. Red meats are also rich in potassium. While generally safe to consume even in large quantities by patients with normal potassium homeostasis, these foods should be avoided in patients with severe renal disease or other underlying conditions or medications predisposing them to hyperkalemia. Intravenous intake through high potassium-containing fluids, particularly total parenteral nutrition, medications with high potassium content, and massive blood transfusions can significantly elevate serum potassium levels.
Hyperkalemia prevention
Dietary changes can help prevent and treat hyperkalemia or high potassium levels. Talk to your doctor to understand any risk you might have for hyperkalemia. Your doctor may recommend foods that you may need to limit or avoid. These may include:
- asparagus, avocados, potatoes, tomatoes or tomato sauce, winter squash, pumpkin, cooked spinach
- oranges and orange juice, nectarines, kiwifruit, bananas, cantaloupe, honeydew, prunes and raisins or other dried fruit.
If you are on a low-salt diet, avoid taking salt substitutes 73.
[Source 74 ]Table 2. Food Sources of Potassium
| Food | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Apricots, dried, ½ cup | 755 | 16 |
| Lentils, cooked, 1 cup | 731 | 16 |
| Squash, acorn, mashed, 1 cup | 644 | 14 |
| Prunes, dried, ½ cup | 635 | 14 |
| Raisins, ½ cup | 618 | 13 |
| Potato, baked, flesh only, 1 medium | 610 | 13 |
| Kidney beans, canned, 1 cup | 607 | 13 |
| Orange juice, 1 cup | 496 | 11 |
| Soybeans, mature seeds, boiled, ½ cup | 443 | 9 |
| Banana, 1 medium | 422 | 9 |
| Milk, 1%, 1 cup | 366 | 8 |
| Spinach, raw, 2 cups | 334 | 7 |
| Chicken breast, boneless, grilled, 3 ounces | 332 | 7 |
| Yogurt, fruit variety, nonfat, 6 ounces | 330 | 7 |
| Salmon, Atlantic, farmed, cooked, 3 ounces | 326 | 7 |
| Beef, top sirloin, grilled, 3 ounces | 315 | 7 |
| Molasses, 1 tablespoon | 308 | 7 |
| Tomato, raw, 1 medium | 292 | 6 |
| Soymilk, 1 cup | 287 | 6 |
| Yogurt, Greek, plain, nonfat, 6 ounces | 240 | 5 |
| Broccoli, cooked, chopped, ½ cup | 229 | 5 |
| Cantaloupe, cubed, ½ cup | 214 | 5 |
| Turkey breast, roasted, 3 ounces | 212 | 5 |
| Asparagus, cooked, ½ cup | 202 | 4 |
| Apple, with skin, 1 medium | 195 | 4 |
| Cashew nuts, 1 ounce | 187 | 4 |
| Rice, brown, medium-grain, cooked, 1 cup | 154 | 3 |
| Tuna, light, canned in water, drained, 3 ounces | 153 | 3 |
| Coffee, brewed, 1 cup | 116 | 2 |
| Lettuce, iceberg, shredded, 1 cup | 102 | 2 |
| Peanut butter, 1 tablespoon | 90 | 2 |
| Tea, black, brewed, 1 cup | 88 | 2 |
| Flaxseed, whole, 1 tablespoon | 84 | 2 |
| Bread, whole-wheat, 1 slice | 81 | 2 |
| Egg, 1 large | 69 | 1 |
| Rice, white, medium-grain, cooked, 1 cup | 54 | 1 |
| Bread, white, 1 slice | 37 | 1 |
| Cheese, mozzarella, part skim, 1½ ounces | 36 | 1 |
| Oil (olive, corn, canola, or soybean), 1 tablespoon | 0 | 0 |
Footnote: *DV = Daily Value. The U.S. Food and Drug Administration (FDA) developed DVs (Daily Values) to help consumers compare the nutrient contents of foods and dietary supplements within the context of a total diet. The Daily Value (DV) for potassium is 4,700 mg for adults and children age 4 years and older 75. FDA requires the new food labels to list potassium content. Foods providing 20% or more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 76 ]Hyperkalemia diagnosis
Your health care provider will perform a physical exam and ask about your symptoms. Most patients with mild and even moderate hyperkalemia are relatively asymptomatic 12. High potassium is often discovered on screening blood tests done in patients with nonspecific complaints, to monitor medications you’re taking or those with suspected electrolyte abnormalities due to infection, dehydration, or hypoperfusion. High potassium is usually not discovered by chance. Causes include renal disease, diabetes, chemotherapy, major trauma, crush injury, or muscle pain suggestive of rhabdomyolysis. Medications that may predispose to the development of hyperkalemia include digoxin, potassium-sparing diuretics, non-steroidal anti-inflammatory drugs, ace-inhibitors or recent intravenous (IV) potassium, total parenteral nutrition, potassium penicillin, or succinylcholine. Patients may complain of weakness, fatigue, palpitations, or syncope.
Physical exam findings may include hypertension and edema in the setting of kidney disease. There may also be signs of hypoperfusion. Muscle tenderness may be present in patients with rhabdomyolysis. Jaundice may be seen in patients with hemolytic conditions. Patients may have muscle weakness, flaccid paralysis, or depressed deep tendon reflexes.
Tests that may be ordered include:
- Electrocardiogram (ECG). The first test that should be ordered in a patient with suspected hyperkalemia is an ECG since the most lethal complication of hyperkalemia is cardiac condition abnormalities which can lead to abnormal heart rhythms (arrhythmias) and death.
- Potassium level
Elevated potassium causes ECG changes in a dose-dependent manner 12:
- Potassium level = 5.5 to 6.5 mEq/L ECG will show tall, peaked T-waves
- Potassium level = 6.5 to 7.5 mEq/L ECG will show loss of P-waves
- Potassium level = 7 to 8 ECG mEq/L will show widening of the QRS complex
- Potassium level = 8 to 10 mEq/L will produce cardiac arrhythmias, sine wave pattern, and asystole
It should be noted that the rate of rising serum potassium is a greater factor than the potassium level 12. Patients with chronic hyperkalemia may have relatively normal EGCs even at high levels, and significant ECG changes may be present at much lower levels in patients with sudden spikes in serum potassium 12.
ECG features of hyperkalemia include 12:
- Small or absent P wave
- Prolonged PR interval
- Augmented R wave
- Wide QRS
- Peaked T waves
Since pseudohyperkalemia is so common, confirmation should be obtained in asymptomatic patients without typical ECG changes before initiating aggressive therapy 12.
Your doctor will also likely check your blood potassium level and do kidney blood tests on a regular basis if you:
- Have been prescribed extra potassium
- Have chronic kidney disease
- Take medicines to treat heart disease or high blood pressure
- Use salt substitutes
Additional laboratory testing should include serum blood urea nitrogen (BUN) and creatinine to assess renal function and urinalysis to screen for renal disease. Urine potassium, sodium, and osmolality may also help evaluate the cause. In patients with renal disease, the serum calcium level should also be checked because hypocalcemia may exacerbate the cardiac effects of hyperkalemia. A complete blood count to screen for leukocytosis or thrombocytosis may also be helpful. Serum glucose and blood gas analysis should be ordered in diabetics and patients with suspected acidosis. Lactate dehydrogenase should be ordered in patients with suspected hemolysis. Creatinine phosphokinases and urine myoglobin should be ordered in patients with suspected rhabdomyolysis. Uric acid and phosphorus should be ordered in patients with suspected tumor lysis syndrome. Digoxin toxicity may cause hyperkalemia, so serum levels should be checked in patients on digoxin. If no other cause is found, consider cortisol and aldosterone levels to assess for mineralocorticoid deficiency.
Hyperkalemia treatment
The urgency with which hyperkalemia should be managed depends on how rapidly the condition develops, the absolute serum potassium level, the degree of symptoms, and the cause 77, 78, 79. If your potassium level is very high (more than 5.5 mEq/L in patients at risk for ongoing hyperkalemia or confirmed hyperkalemia of 6.5 mEq/L), or if there are dangerous indications such as changes in an electrocardiogram (ECG), neuromuscular weakness or paralysis, emergency treatment is needed. That may involve supplying calcium to the body through an intravenous to treat the effects on muscles and the heart or administering glucose and insulin through an intravenous to decrease potassium levels long enough to correct the cause. There are also medicines that help remove the potassium from your intestines and in some cases, a diuretic may be given.
Emergency treatment may also include kidney dialysis if kidney function is deteriorating; medication to help remove potassium from the intestines before absorption; sodium bicarbonate if acidosis is the cause; and water pills, or diuretics.
A doctor may also advise stopping or reducing potassium supplements and stopping or changing the doses of certain medicines for heart disease and high blood pressure. Always follow your health provider’s instructions about taking or stopping medicines.
Hyperkalemia treatment is usually prescribed in the following manner 12:
- Exogenous sources of potassium should be immediately discontinued.
- Treatment of the reversible cause should begin along with the management of hyperkalemia.
- Calcium given into your veins (IV) to treat the muscle and heart effects of high potassium levels. Calcium therapy will stabilize the cardiac response to hyperkalemia and should be initiated first in the setting of cardiac toxicity. Calcium does not alter the serum concentration of potassium but is a first-line therapy in hyperkalemia-related arrhythmias and ECG changes. Calcium chloride contains three times more elemental calcium than calcium gluconate but is more irritating to peripheral vessels and more likely to cause tissue necrosis with extravasation, so it is usually only given through central venous lines or peripherally in cardiac arrest. Thus, calcium gluconate is the usual initial drug of choice in patients with evidence of cardiac toxicity 80. As a precaution, calcium should never be given in bicarbonate-containing fluids, as it can cause the precipitation of calcium carbonate.
- Insulin and glucose given into your veins (IV) to help lower potassium levels long enough to correct the cause or insulin alone in hyperglycemic patients, will drive the potassium back into the cells, effectively lowering serum potassium 81. A common regimen is ten units of regular insulin given with 50 ml of a 50% dextrose solution (D50). Patients should be monitored closely for the development of hypoglycemia (low blood sugar level). A 10% dextrose infusion at 50 to 75 ml/hour is associated with less hypoglycemia than bolus dosing with 50% dextrose solution (D50).
- Beta-2 adrenergic agents such as albuterol will also shift potassium intracellularly 82. To be effective, beta-2 agonists are given in much higher doses than those commonly used for bronchodilation. Intravenous epinephrine, however, should not be used to manage hyperkalemia due to an increased risk of causing angina.
- Sodium bicarbonate infusion may be helpful in patients with metabolic acidosis. Bolus dosing of sodium bicarbonate is less effective.
- Loop or thiazide diuretics may help enhance potassium excretion. They may be used in non-oliguric, volume-overloaded patients but should not be used as monotherapy in symptomatic patients. In hypervolemic patients with preserved kidney function (e.g., patients with congestive cardiac failure), 40 mg of intravenous furosemide is administered every 12 hours or may be given as a continuous infusion. In euvolemic or hypovolemic patients with preserved kidney function, an isotonic saline infusion is given before as needed to the patient before administering 40 mg of intravenous furosemide every 12 hours or a continuous furosemide infusion.
- Medicines that help remove potassium from the intestines before it is absorbed such as patiromer may be helpful, particularly in patients with renal insufficiency who cannot receive immediate dialysis. Sodium polystyrene sulfonate, though commonly used, is falling out of favor due to lack of effectiveness and adverse effects, particularly bowel necrosis in elderly patients. If used due to a lack of alternatives, it should not be given with sorbitol, which increases toxicity 83.
- Kidney dialysis should be performed in patients with end-stage renal disease or severe renal impairment.
Complications of hyperkalemia treatment 12:
- Hypokalemia
- Inability to control hyperkalemia
- Hypocalcemia as a result of bicarbonate infusion
- Hypoglycemia due to insulin
- Metabolic alkalosis from bicarbonate therapy
- Volume depletion from diuresis.
Changes in your diet can help both prevent and treat high potassium levels. You may be asked to:
- Limit or avoid asparagus, avocados, potatoes, tomatoes or tomato sauce, winter squash, pumpkin, and cooked spinach
- Limit or avoid oranges and orange juice, nectarines, kiwifruit, raisins, or other dried fruit, bananas, cantaloupe, honeydew, prunes, and nectarines
- Avoid taking salt substitutes if you are asked to eat a low-salt diet
Your doctor may make the following changes to your medicines:
- Reduce or stop potassium supplements
- Stop or change the doses of medicines you are taking, such as ones for heart disease and high blood pressure
- Take a certain type of water pill to reduce potassium and fluid levels if you have chronic kidney failure
Follow your doctor’s directions when taking your medicines:
- DO NOT stop or start taking medicines without first talking to your provider
- Take your medicines on time
- Tell your provider about any other medicines, vitamins, or supplements you are taking
For people with heart failure
There are some drugs that heart failure patients take that are associated with hyperkalemia. These are: diuretics, beta-blockers and angiotension converting enzyme inhibitors (ACE inhibitors). For patients with heart failure on these drugs, if any symptoms are experienced as above, you should tell your doctor to make sure that the symptoms are not related to hyperkalemia.
If your potassium level is too high, you may need to cut back on certain foods (see Table 2 and 3). These tips can also help:
- Soak or boil vegetables and fruits to leach out some of the potassium.
- Avoid foods that list potassium or K, KCl, or K+ — chemical symbols for potassium or related compounds — as ingredients on the label.
- Stay away from salt substitutes. Many are high in potassium. Read the ingredient lists carefully and check with your doctor before using one of these preparations.
- Avoid canned, salted, pickled, corned, spiced, or smoked meat and fish.
- Avoid imitation meat products containing soy or vegetable protein.
- Limit high-potassium fruits such as bananas, citrus fruits, and avocados.
- Avoid baked potatoes and baked acorn and butternut squash.
- Don’t use vegetables or meats prepared with sweet or salted sauces.
- Avoid all types of peas and beans, which are naturally high in potassium.
Table 3. Potassium levels in common foods
| Foods | High potassium | Medium potassium | Low potassium | No potassium |
|---|---|---|---|---|
| Fruits and vegetables | Artichokes, avocados, bananas, broccoli, coconut, dried fruits, leafy greens, kiwis, nectarines, oranges, papayas, potatoes, prunes, spinach, tomatoes, winter squash, yams | Apples, apricots, asparagus, carrots, cherries, corn, eggplant, peaches, pears, peppers, pineapple juice, radishes | Blueberries, cauliflower, cucumbers, grapefruit, grapes, green beans, lettuce, strawberries | |
| Meat and protein | Dried beans and peas, imitation bacon bits, nuts, soy products | Beef, eggs, fish, peanut butter, poultry, pork, veal | ||
| Dairy | Milk, yogurt | Sour cream | ||
| Grains and processed foods | Plain bagel, plain pasta, oatmeal, white bread, white rice | Bran muffins and cereals, corn tortillas, whole-wheat bread | Fruit punches, jelly beans, nondairy topping, nondairy creamers |
Hyperkalemia prognosis
The prognosis is excellent for patients with mild transient hyperkalemia due to too much potassium in the diet if the inciting cause is addressed and treated. Sudden onset, extreme hyperkalemia can cause cardiac arrhythmias that can be deadly in up to two-thirds of cases if not rapidly treated 12. Hyperkalemia is an independent risk factor for death in hospitalized patients 12.
- Hyperkalemia. University of Maryland Medical Center. http://umm.edu/health/medical/altmed/condition/hyperkalemia. Accessed Oct. 1, 2014.[↩]
- Sur M, Mohiuddin SS. Potassium. [Updated 2022 Dec 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539791[↩][↩][↩]
- Weiss JN, Qu Z, Shivkumar K. Electrophysiology of Hypokalemia and Hyperkalemia. Circ Arrhythm Electrophysiol. 2017 Mar;10(3):e004667. doi: 10.1161/CIRCEP.116.004667[↩][↩]
- Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 8: advanced challenges in resuscitation: section 1: life-threatening electrolyte abnormalities. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Circulation. 2000 Aug 22;102(8 Suppl):I217-22.[↩][↩]
- Rosano GMC, Tamargo J, Kjeldsen KP, Lainscak M, Agewall S, Anker SD, Ceconi C, Coats AJS, Drexel H, Filippatos G, Kaski JC, Lund L, Niessner A, Ponikowski P, Savarese G, Schmidt TA, Seferovic P, Wassmann S, Walther T, Lewis BS. Expert consensus document on the management of hyperkalaemia in patients with cardiovascular disease treated with renin angiotensin aldosterone system inhibitors: coordinated by the Working Group on Cardiovascular Pharmacotherapy of the European Society of Cardiology. Eur Heart J Cardiovasc Pharmacother. 2018 Jul 1;4(3):180-188. doi: 10.1093/ehjcvp/pvy015[↩][↩]
- Potassium, serum. Mayo Medical Laboratories. http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/81390. Accessed Oct. 1, 2014.[↩]
- Mayo Foundation for Medical Education and Research, MayoClinic. High potassium (hyperkalemia) Symptoms. http://www.mayoclinic.org/symptoms/hyperkalemia/basics/definition/SYM-20050776?p=1[↩]
- Institute of Medicine. Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate. Washington, DC; 2005.[↩][↩][↩]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Dietary Reference Intakes for Sodium and Potassium; Oria M, Harrison M, Stallings VA, editors. Dietary Reference Intakes for Sodium and Potassium. Washington (DC): National Academies Press (US); 2019 Mar 5. 4, Potassium: Dietary Reference Intakes for Adequacy. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545428[↩][↩][↩]
- Viera AJ, Wouk N. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2015 Sep 15;92(6):487-95. https://www.aafp.org/pubs/afp/issues/2015/0915/p487.html[↩][↩][↩][↩]
- Kim MJ, Valerio C, Knobloch GK. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2023 Jan;107(1):59-70. https://www.aafp.org/pubs/afp/issues/2023/0100/potassium-disorders-hypokalemia-hyperkalemia.html[↩][↩]
- Simon LV, Hashmi MF, Farrell MW. Hyperkalemia. [Updated 2023 Feb 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470284[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- High potassium (hyperkalemia). https://www.mayoclinic.org/symptoms/hyperkalemia/basics/causes/sym-20050776[↩][↩]
- High potassium (hyperkalemia). https://www.mayoclinic.org/symptoms/hyperkalemia/basics/definition/sym-20050776[↩]
- Lytvyn Y, Godoy LC, Scholtes RA, van Raalte DH, Cherney DZ. Mineralocorticoid Antagonism and Diabetic Kidney Disease. Curr Diab Rep. 2019 Jan 23;19(1):4. doi: 10.1007/s11892-019-1123-8[↩]
- Flury G. Das «gefährliche» EKG [The ‘Dangerous’ ECG]. Praxis (Bern 1994). 2019 Jan;108(1):45-52. German. doi: 10.1024/1661-8157/a003155[↩]
- Potassium. https://pubchem.ncbi.nlm.nih.gov/compound/potassium[↩]
- Unwin, R., Luft, F. & Shirley, D. Pathophysiology and management of hypokalemia: a clinical perspective. Nat Rev Nephrol 7, 75–84 (2011). https://doi.org/10.1038/nrneph.2010.175[↩][↩][↩][↩]
- Stone MS, Martyn L, Weaver CM. Potassium Intake, Bioavailability, Hypertension, and Glucose Control. Nutrients. 2016 Jul 22;8(7):444. doi: 10.3390/nu8070444[↩][↩][↩][↩][↩]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Dietary Reference Intakes for Sodium and Potassium; Oria M, Harrison M, Stallings VA, editors. Dietary Reference Intakes for Sodium and Potassium. Washington (DC): National Academies Press (US); 2019 Mar 5. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538102[↩][↩][↩][↩][↩][↩][↩]
- Brooks G. Potassium additive algorithm for use in continuous renal replacement therapy. Nurs Crit Care. 2006 Nov-Dec;11(6):273-80. doi: 10.1111/j.1478-5153.2006.00185.x[↩]
- Preuss HG, Clouatre DL. Sodium, chloride, and potassium. In: Erdman JW, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed. Washington, DC: Wiley-Blackwell; 2012:475-92.[↩][↩][↩][↩]
- Hinderling PH. The Pharmacokinetics of Potassium in Humans Is Unusual. J Clin Pharmacol. 2016 Oct;56(10):1212-20. doi: 10.1002/jcph.713[↩][↩]
- Palmer B.F. Regulation of potassium homeostasis. Clin. J. Am. Soc. Nephrol. 2015;10:1050–1060. doi: 10.2215/CJN.08580813[↩]
- Unwin R.J., Luft F.C., Shirley D.G. Pathophysiology and management of hypokalemia: A clinical perspective. Nat. Rev. Nephrol. 2011;7:75–84. doi: 10.1038/nrneph.2010.175[↩]
- Palmer BF, Clegg DJ. Physiology and Pathophysiology of Potassium Homeostasis: Core Curriculum 2019. Am J Kidney Dis. 2019 Nov;74(5):682-695. doi: 10.1053/j.ajkd.2019.03.427. Erratum in: Am J Kidney Dis. 2022 Nov;80(5):690.[↩][↩][↩][↩][↩]
- World Health Organisation (WHO) Guideline: Potassium Intake for Adults and Children. WHO; Geneva, Switzerland: 2012.[↩]
- Fulgoni VL 3rd, Keast DR, Bailey RL, Dwyer J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J Nutr. 2011 Oct;141(10):1847-54. doi: 10.3945/jn.111.142257[↩][↩]
- O’Neil C.E., Keast D.R., Fulgoni V.L., Nicklas T.A. Food sources of energy and nutrients among adults in the us: Nhanes 2003–2006. Nutrients. 2012;4:2097–2120. doi: 10.3390/nu4122097[↩]
- DeSalvo K.B., Olson R., Casavale K.O. Dietary guidelines for americans. JAMA. 2016;315:457–458. doi: 10.1001/jama.2015.18396[↩]
- Weaver C.M. Potassium and health. Adv. Nutr. (Bethesda Md.) 2013;4:S368–S377. doi: 10.3945/an.112.003533[↩]
- He F.J., MacGregor G.A. Beneficial effects of potassium on human health. Physiol. Plant. 2008;133:725–735. doi: 10.1111/j.1399-3054.2007.01033.x[↩]
- Bailey JL, Sands JM, Franch HA. Water, electrolytes, and acid-based metabolism. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, eds. Modern Nutrition in Health and Disease. 11th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2014:102-32.[↩]
- Shils M.E., Shike M. Modern Nutrition in Health and Disease. Lippincott Williams & Wilkins; Baltimore, MD, USA: 2006.[↩]
- Palmer BF, Clegg DJ. Physiology and pathophysiology of potassium homeostasis. Adv Physiol Educ. 2016 Dec;40(4):480-490. doi: 10.1152/advan.00121.2016[↩][↩][↩][↩][↩]
- Hené RJ, Koomans HA, Boer P, Dorhout Mees EJ. Adaptation to chronic potassium loading in normal man. Miner Electrolyte Metab. 1986;12(3):165-72.[↩]
- Rabelink TJ, Koomans HA, Hené RJ, Dorhout Mees EJ. Early and late adjustment to potassium loading in humans. Kidney Int. 1990 Nov;38(5):942-7. doi: 10.1038/ki.1990.295[↩]
- Potassium. https://ods.od.nih.gov/factsheets/Potassium-HealthProfessional[↩][↩]
- Patrick J. Assessment of body potassium stores. Kidney Int 1977;11:476-90. https://www.kidney-international.org/article/S0085-2538(15)31757-9/pdf[↩][↩]
- Chatterjee R, Yeh HC, Edelman D, Brancati F. Potassium and risk of Type 2 diabetes. Expert Rev Endocrinol Metab. 2011 Sep;6(5):665-672. doi: 10.1586/eem.11.60[↩]
- WHO. Diet, nutrition and the prevention of chronic disease. Report of a Joint WHO/FAO Expert Consultation. Geneva, World Health Organization (WHO), 2003. http://whqlibdoc.who.int/trs/WHO_TRS_916.pdf [↩]
- D’Elia L, Barba G, Cappuccio FP et al. Potassium intake, stroke, and cardiovascular disease a meta-analysis of prospective studies. Journal of the American College of Cardiology, 2011, 57(10):1210–1219. http://www.ncbi.nlm.nih.gov/pubmed/21371638[↩]
- Whelton PK, He J, Cutler JA et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. Journal of the American Medical Association, 1997, 277(20):1624–1632. http://www.ncbi.nlm.nih.gov/pubmed/9168293[↩]
- Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. Journal of Human Hypertension, 2003, 17(7):471–480. http://www.ncbi.nlm.nih.gov/pubmed/12821954[↩]
- Dietary Guidelines Advisory Committee. The report of the Dietary Guidelines Advisory Committee on Dietary Guidelines for Americans. Washington, D.C., Department of Health and Human Services and Department of Agriculture, 2005. http://www.health.gov/dietaryguidelines/dga2005/report/default.htm[↩]
- World Health Organization. Guideline: Potassium intake for adults and children. http://apps.who.int/iris/bitstream/10665/77986/1/9789241504829_eng.pdf[↩][↩]
- American Heart Association. A Primer on Potassium. https://sodiumbreakup.heart.org/a_primer_on_potassium?utm_source=SRI&utm_medium=HeartOrg&utm_term=Website&utm_content=SodiumAndSalt&utm_campaign=SodiumBreakup[↩][↩][↩]
- Potassium. https://lpi.oregonstate.edu/mic/minerals/potassium[↩][↩][↩]
- Clausen T. Quantification of Na+,K+ pumps and their transport rate in skeletal muscle: functional significance. J Gen Physiol. 2013 Oct;142(4):327-45. doi: 10.1085/jgp.201310980[↩]
- Larsen BR, Stoica A, MacAulay N. Managing Brain Extracellular K(+) during Neuronal Activity: The Physiological Role of the Na(+)/K(+)-ATPase Subunit Isoforms. Front Physiol. 2016 Apr 22;7:141. doi: 10.3389/fphys.2016.00141[↩]
- Shattock MJ, Ottolia M, Bers DM, Blaustein MP, Boguslavskyi A, Bossuyt J, Bridge JH, Chen-Izu Y, Clancy CE, Edwards A, Goldhaber J, Kaplan J, Lingrel JB, Pavlovic D, Philipson K, Sipido KR, Xie ZJ. Na+/Ca2+ exchange and Na+/K+-ATPase in the heart. J Physiol. 2015 Mar 15;593(6):1361-82. doi: 10.1113/jphysiol.2014.282319[↩]
- DrugBank. Potassium. http://www.drugbank.ca/drugs/DB01345[↩]
- Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol2009;38:791-813.[↩]
- Kawasaki T, Itoh K, Kawasaki M. Reduction in blood pressure with a sodium-reduced, potassium- and magnesium-enriched mineral salt in subjects with mild essential hypertension. Hypertens Res1998;21:235-43. https://www.ncbi.nlm.nih.gov/pubmed/9877516?access_num=9877516&link_type=MED&dopt=Abstract[↩]
- Chang HY, Hu YW, Yue CS, Wen YW, Yeh WT, Hsu LS, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr2006;83:1289-96. http://ajcn.nutrition.org/content/83/6/1289?ijkey=52dc92efe22c9a7ff1bd4e7366b4fcecb7f45e7e&keytype2=tf_ipsecsha[↩]
- Sheng H-W. Sodium, chloride and potassium. In: Stipanuk M, ed. Biochemical and Physiological Aspects of Human Nutrition. Philadelphia: W.B. Saunders Company; 2000:686-710.[↩]
- Goyal A, Spertus JA, Gosch K, Venkitachalam L, Jones PG, Van den Berghe G, Kosiborod M. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012 Jan 11;307(2):157-64. doi: 10.1001/jama.2011.1967[↩]
- Smyth A, Dunkler D, Gao P, Teo KK, Yusuf S, O’Donnell MJ, Mann JF, Clase CM; ONTARGET and TRANSCEND investigators. The relationship between estimated sodium and potassium excretion and subsequent renal outcomes. Kidney Int. 2014 Dec;86(6):1205-12. doi: 10.1038/ki.2014.214[↩]
- Rose BD. Causes of hyperkalemia. http://www.uptodate.com/home. Accessed Oct. 1, 2014.[↩]
- Mattu A, Brady WJ, Robinson DA. Electrocardiographic manifestations of hyperkalaemia. Am J Emerg Med 2000; 18: 721-729.[↩]
- Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med 1998;158: 917-924.[↩]
- Sood MM, Pauly RP. A case of severe hyperkalaemia: fast, safe and effective treatment is required. J Crit Care 2008; 23: 431–433.[↩]
- MayoClinic. Causes of Hyperkalemia. https://www.mayoclinic.org/symptoms/hyperkalemia/basics/causes/sym-20050776[↩]
- Acute kidney failure. https://www.mayoclinic.org/diseases-conditions/kidney-failure/symptoms-causes/syc-20369048[↩]
- Chronic kidney disease. https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521[↩]
- Frequently asked questions about GFR estimates. https://www.kidney.org/sites/default/files/441-8491_2202_faqs_aboutgfr_v5.pdf[↩]
- Raebel MA. Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. Cardiovasc Ther. 2012 Jun;30(3):e156-66. doi: 10.1111/j.1755-5922.2010.00258.x[↩][↩]
- Sarafidis PA, Georgianos PI, Lasaridis AN. Diuretics in clinical practice. Part II: electrolyte and acid-base disorders complicating diuretic therapy. Expert Opin Drug Saf. 2010 Mar;9(2):259-73. doi: 10.1517/14740330903499257[↩][↩][↩]
- Williams SM, Killeen AA. Tumor Lysis Syndrome. Arch Pathol Lab Med. 2019 Mar;143(3):386-393. doi: 10.5858/arpa.2017-0278-RS[↩]
- Sekhon DS, Vaqar S, Gupta V. Hyperkalemic Periodic Paralysis. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564319[↩][↩]
- Weber F. Hyperkalemic Periodic Paralysis. 2003 Jul 18 [Updated 2021 Jul 1]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1496[↩][↩][↩][↩][↩][↩][↩]
- Statland JM, Fontaine B, Hanna MG, Johnson NE, Kissel JT, Sansone VA, Shieh PB, Tawil RN, Trivedi J, Cannon SC, Griggs RC. Review of the Diagnosis and Treatment of Periodic Paralysis. Muscle Nerve. 2018 Apr;57(4):522-530. doi: 10.1002/mus.26009[↩]
- American Heart Association. Hyperkalemia (High Potassium). http://www.heart.org/HEARTORG/Conditions/HeartFailure/TreatmentOptionsForHeartFailure/Hyperkalemia-High-Potassium_UCM_488806_Article.jsp[↩]
- Kim MJ, Valerio C, Knobloch GK. Potassium Disorders: Hypokalemia and Hyperkalemia. Am Fam Physician. 2023 Jan;107(1):59-70.https://www.aafp.org/pubs/afp/issues/2023/0100/potassium-disorders-hypokalemia-hyperkalemia.html[↩]
- Food Labeling: Revision of the Nutrition and Supplement Facts Labels. https://www.federalregister.gov/documents/2016/05/27/2016-11867/food-labeling-revision-of-the-nutrition-and-supplement-facts-labels[↩]
- U.S. Department of Agriculture, Agricultural Research Service. USDA National Nutrient Database for Standard Reference, Release 28. https://ndb.nal.usda.gov/ndb/[↩]
- Campbell CA, Lam Q, Horvath AR. An evidence- and risk-based approach to a harmonized laboratory alert list in Australia and New Zealand. Clin Chem Lab Med. 2018 Dec 19;57(1):89-94. doi: 10.1515/cclm-2017-1114[↩]
- Butler J, Vijayakumar S, Pitt B. Revisiting hyperkalaemia guidelines: rebuttal. Eur J Heart Fail. 2018 Sep;20(9):1255. doi: 10.1002/ejhf.1249[↩]
- Butler J, Vijayakumar S, Pitt B. Need to revisit heart failure treatment guidelines for hyperkalaemia management during the use of mineralocorticoid receptor antagonists. Eur J Heart Fail. 2018 Sep;20(9):1247-1251. doi: 10.1002/ejhf.1217[↩]
- Long B, Warix JR, Koyfman A. Controversies in Management of Hyperkalemia. J Emerg Med. 2018 Aug;55(2):192-205. doi: 10.1016/j.jemermed.2018.04.004[↩]
- Sterns RH, Grieff M, Bernstein PL. Treatment of hyperkalemia: something old, something new. Kidney Int. 2016 Mar;89(3):546-54. doi: 10.1016/j.kint.2015.11.018[↩]
- Gosmanov AR, Wong JA, Thomason DB. Duality of G protein-coupled mechanisms for beta-adrenergic activation of NKCC activity in skeletal muscle. Am J Physiol Cell Physiol. 2002 Oct;283(4):C1025-32. doi: 10.1152/ajpcell.00096.2002[↩]
- Mistry M, Shea A, Giguère P, Nguyen ML. Evaluation of Sodium Polystyrene Sulfonate Dosing Strategies in the Inpatient Management of Hyperkalemia. Ann Pharmacother. 2016 Jun;50(6):455-62. doi: 10.1177/1060028016641427[↩]
- Harvard University. Harvard Health Publications. Heart failure and potassium. http://www.health.harvard.edu/heart-health/heart-failure-and-potassium[↩]