Intersection syndrome
Intersection syndrome is commonly known as tenosynovitis of the radial wrist extensors (extensor carpi radialis longus, extensor carpi radialis brevis, extensor pollicis brevis and abductor pollicis longus), causing pain and swelling of these muscle bellies 1. Intersection syndrome is a cause of radial-sided wrist and forearm pain and swelling in the distal dorsoradial forearm 2. This is typically noted as a pain just proximal and dorsal to the radial styloid, or also noted anatomically by 4 cm – 6 cm proximal to Lister’s tubercle 3. Intersection syndrome is often brought on by athletics or other activities that involve repetitive wrist flexion and extension 4. Intersection syndrome is thought to occur as a result of repetitive friction at the junction in which the tendons of the first dorsal compartment cross over the second, creating a tenosynovitis.
Multiple conditions can also cause radial-sided wrist and forearm pain. The most common are de Quervain tenosynovitis and thumb carpometacarpal arthritis 5.
Most cases of intersection syndrome respond to conservative treatment consisting of immobilization, activity modification, and pharmacologic intervention, followed by a program of supervised hand or occupational therapy. Refractory cases can be treated with tenosynovectomy 6.
Intersection syndrome key points
- Intersection syndrome is inflammatory tenosynovitis at the intersection of the 1st dorsal compartment (extensor pollicis brevis and abductor pollicis longus) and 2nd dorsal compartment (extensor carpi radialis longus, extensor carpi radialis brevis) of the wrist
- Patients report pain over dorsal forearm and wrist
- Examination reveals ttp dorsal radial forearm about 4-6 cm proximal to joint, worse with resisted wrist extension, thumb extension
- Diagnosis is primarily clinical but supported by ultrasound and MRI (magnetic resonance imaging)
- Treatment is primarily non-operative with medicine, splinting, corticosteroid injections, and very rarely surgical debridement or release
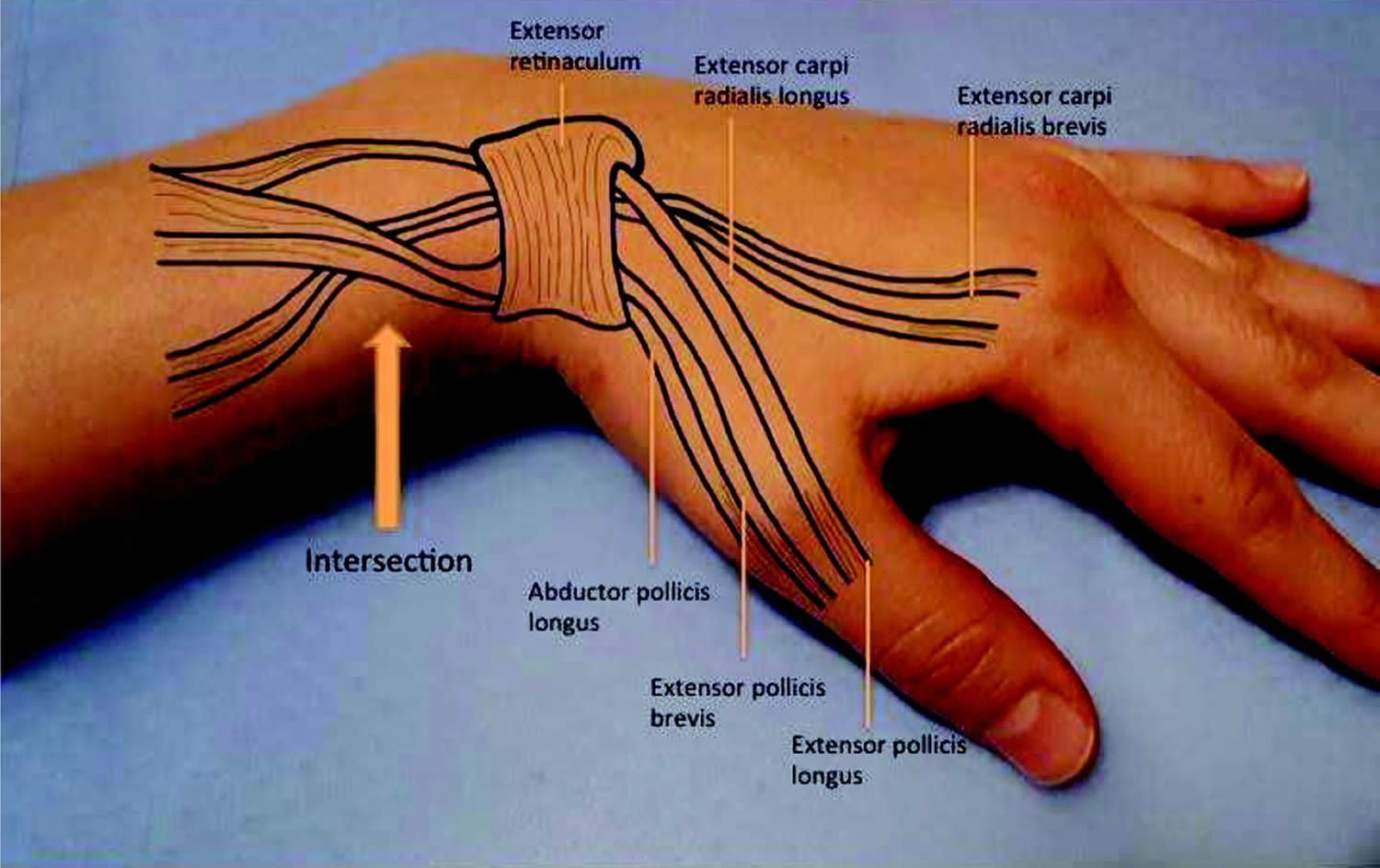
Figure 1. Intersection syndrome wrist
Intersection syndrome causes
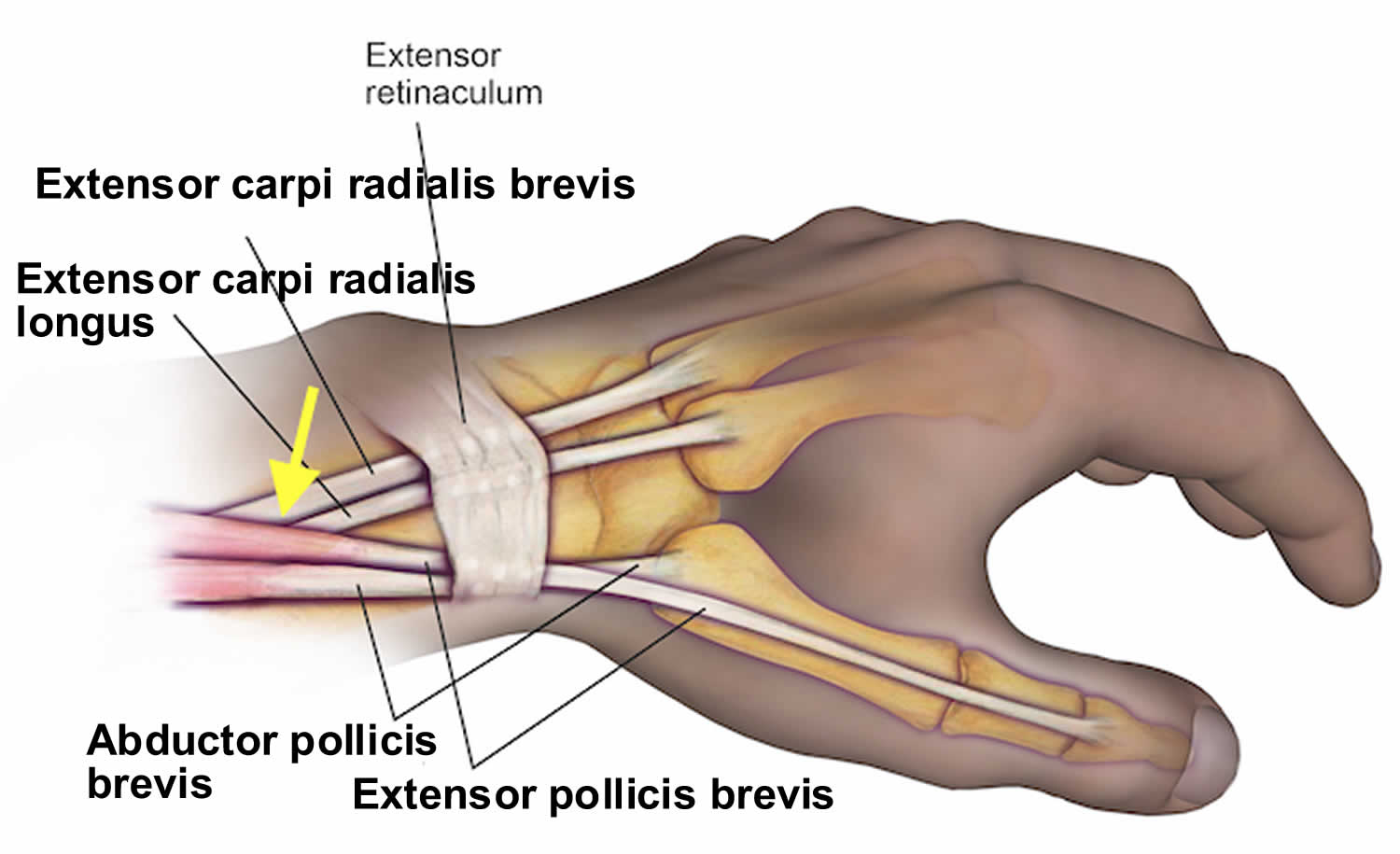
The first dorsal compartment of the wrist is comprised of the abductor pollicis longus and extensor pollicis brevis. These tendons have a unique anatomical pathway proximally in which they cross over the second dorsal compartment tendons just proximal to the extensor retinaculum and radial styloid. The second dorsal compartment of the wrist is comprised of the extensor carpi radialis brevis and extensor carpi radialis longus 7.
Intersection syndrome is typically the result of repetitive extension and flexion exercises or activities. Intersection syndrome is commonly seen in sporting activities such as rowing or canoeing, weightlifting, skiing, racquet sports, and horseback riding 8. There is no significant difference in injury pattern found in men versus women 3.
The repetitive extension-flexion of the wrist results in a friction injury at the crossover junction of the first dorsal compartment (abductor pollicis longus and extensor pollicis brevis) and the second dorsal compartment (extensor carpi radialis brevis/extensor carpi radialis longus) tendons leading to an inflammatory response and subsequently a tenosynovitis 1. The presentation is typically one that the patient complains of pain or tenderness over the dorsal aspect of the wrist proximal to the radial styloid. There may also be swelling and crepitus that is palpable on the exam with wrist and/or thumb extension 7.
Intersection syndrome symptoms
Patients with intersection syndrome complain of radial wrist or forearm pain. Symptoms may be exacerbated by repetitive wrist flexion and extension.
On examination, discrete swelling at this area of intersection often is present. Active or passive wrist motion produces a characteristic “wet leather” crepitus. The examiner must exclude other causes of radial forearm pain, such as the following:
- de Quervain tenosynovitis
- Thumb carpometacarpal arthritis
- Radial sensory nerve irritation (Wartenberg syndrome)
- Extensor pollicis longus tendinitis
Intersection syndrome diagnosis
Intersection syndrome is a clinical diagnosis, although a musculoskeletal ultrasound can easily confirm it. The initial steps for diagnosis include a focused physical exam of the elbow, wrist, and hand 3.
Anteroposterior (AP), lateral, and oblique radiographs of the wrist (including distal forearm) may be ordered 9. Ancillary studies do not help with the diagnosis of intersection syndrome but do allow the physician to exclude other causes of forearm pain. Radiographs can depict thumb carpometacarpal arthritis and osteophytes around the distal radius.
Magnetic resonance imaging (MRI) is rarely indicated. However, an MRI scan could be ordered if the physician is suspicious of a soft tissue mass as the cause of swelling 10.
Ultrasound will demonstrate peritendinous inflammation and edema, and can differentiate this from other causes of swelling such as ganglia 11.
Intersection syndrome treatment
Intersection syndrome treatment is conservative management with rest and activity modification. Corticosteroid injection has shown significant improvement and is a known next best step if little or no improvement has been made with other conservative treatment 3.
Anti-inflammatory medications are maybe useful for acute injury and pain relief. Common medications are ibuprofen, naproxen, meloxicam or diclofenac 12. Acetaminophen also may be utilized for pain relief as well. Typically rest and activity modification will be more effective. Ice is also an effective treatment. A temporary splint for protection and comfort at night may also be beneficial. There is no compelling evidenced based rehab protocol for intersection syndrome at this time. One may consider extrapolating the use of eccentric strengthening and stretching for rehab protocols.
When conservative measures are not effective corticosteroid injection under ultrasound guidance can be utilized. Using the ultrasound visualization technique noted in the evaluation process; confirm the diagnosis. The typical injection is a one to one mixture of a corticosteroid and anesthetic (0.5ml to 1ml of steroid, commonly used is triamcinolone 40mg/1ml along with a local anesthetic of choice at 0.5ml to 1ml). A 23 to 25 gauge needle at a length of 1 to 1.5 inch is preferred 13. Using the in-plane or out of plane needle injection technique, guide the needle to where the first dorsal compartment (abductor pollicis longus and extensor pollicis brevis) is crossed over the second dorsal compartment (extensor carpi radialis brevis/extensor carpi radialis longus) 13. After the injection is completed, have the patient pronate and supinate the wrist, observe for crepitus and tenderness with palpation. Resolution of the pain can help solidify the diagnosis. The steroid will take the time to reach full potential. We recommend that rehab exercises be used in tandem with the injection after day 3 to 5.
Cortisone injections near the skin may cause depigmentation in patients who are dark skinned. These injections also may lead to subcutaneous fat atrophy or necrosis, infection, and tendon rupture, although, fortunately, these complications are rare.
Surgical debridement and release is only rarely required, when symptoms persist despite an adequate course of conservative treatment (including activity modification).
Intersection syndrome surgery
The second extensor compartment is approached through a dorsal longitudinal incision, beginning over the area of swelling and continuing distally 3-4 cm. Bluntly dissect down to the dorsal forearm fascia and divide longitudinally. Protect major veins and, particularly, branches of the radial sensory nerve that are located in this region. Completely mobilize the extensor carpi radialis longus and extensor carpi radialis brevis tendons by longitudinally incising the extensor retinaculum over the second compartment.
A bursa also may form between the overlying extensor pollicis brevis and abductor pollicis longus tendons. When present, this bursa should be resected.
Perform a thorough tenosynovectomy while elevating and protecting the tendons. This also may require mobilization of the extensor pollicis brevis and abductor pollicis longus, which then are retracted proximally and distally to provide complete access to the second compartment. The extensor retinaculum is not repaired. Skin is closed in routine fashion.
Immobilize the area in a compressive dressing and well-padded volar thumb spica splint, maintaining the wrist at 20º of extension for 7-10 days.
At the first postoperative visit, place the patient in a removable splint and encourage early wrist range-of-motion (ROM) exercises. Some patients require postoperative therapy similar to that used prior to surgery.
Occupational therapy generally is initiated early for patients with labor-intensive occupations. The goals of therapy are strengthening, full range-of-motion and modification of equipment. The rehabilitation period may last 4-6 weeks.
Intersection syndrome prognosis
Most patients with intersection syndrome respond to a program of conservative management. They may need to maintain changes in work or avocational activities to prevent recurrence of symptoms. Individuals who require surgery rarely experience recurrence of symptoms.
No large series documenting treatment outcome exist in the literature. Eight patients in one study all responded to immobilization and corticosteroid injection. Grundberg and Reagan state that about 60% of patients in their practice with intersection syndrome respond to conservative management 14. They report that 100% of their patients who require surgery obtain long-term symptomatic relief. In the author’s experience, nonoperative treatment of intersection syndrome is successful in approximately 75% of cases; surgical decompression of the second extensor compartment is effective in the remainder of patients.
- Michols NJ, Kiel J. Intersection Syndrome. [Updated 2019 Apr 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430899[↩][↩]
- Browne J, Helms CA. Intersection syndrome of the forearm. Arthritis Rheum. 2006 Jun. 54(6):2038.[↩]
- Browne J, Helms CA. Intersection syndrome of the forearm. Arthritis Rheum. 2006 Jun;54(6):2038.[↩][↩][↩][↩]
- Elmgreen SB, Krogh S, Kasch H. [Intersection syndrome in a tetraplegic hand cyclist]. Ugeskr Laeger. 2018 Jun 18. 180, 25[↩]
- Sato J, Ishii Y, Noguchi H. Clinical and ultrasound features in patients with intersection syndrome or de Quervain’s disease. J Hand Surg Eur Vol. 2016 Feb. 41 (2):220-5.[↩]
- Intersection Syndrome. https://emedicine.medscape.com/article/1242239-overview[↩]
- McNally E, Wilson D, Seiler S. Rowing injuries. Semin Musculoskelet Radiol. 2005 Dec;9(4):379-96.[↩][↩]
- Tagliafico AS, Ameri P, Michaud J, Derchi LE, Sormani MP, Martinoli C. Wrist injuries in nonprofessional tennis players: relationships with different grips. Am J Sports Med. 2009 Apr. 37(4):760-7.[↩]
- [Guideline] ACR Appropriateness Criteria: Chronic Wrist Pain. American College of Radiology. https://acsearch.acr.org/docs/69427/Narrative/[↩]
- Lee RP, Hatem SF, Recht MP. Extended MRI findings of intersection syndrome. Skeletal Radiol. 2009 Feb. 38(2):157-63.[↩]
- Draghi F, Bortolotto C. Intersection syndrome: ultrasound imaging. Skeletal Radiol. 2014 Mar. 43(3):283-7.[↩]
- Servi JT. Wrist pain from overuse: detecting and relieving intersection syndrome. Phys Sportsmed. 1997 Dec;25(12):41-4.[↩]
- Giovagnorio F, Miozzi F. Ultrasound findings in intersection syndrome. J Med Ultrason (2001). 2012 Oct;39(4):217-20.[↩][↩]
- Grundberg AB, Reagan DS. Pathologic anatomy of the forearm: intersection syndrome. J Hand Surg [Am]. 1985 Mar. 10(2):299-302.[↩]