What is jejunostomy tube
A jejunostomy tube or J-tube, is a soft plastic feeding tube that is placed through the skin of the abdomen into the jejunum (middle section of the small intestine) bypassing the stomach entirely. Jejunostomy tube is done when the stomach has to be bypassed. Often this is due to severe reflux disease, or dysmotility. The jejunostomy tube delivers food and medicine until you are healthy enough to eat by mouth.
There are a number of reasons why a jejunostomy tube may be beneficial for you. Jejunostomy tubes may be used in infants and children who have issues with swallowing due to surgery. They may also be used in patients who are unable to swallow as a result of central nervous system disorders, patients who require feeding supplementation or special diets or to administer frequent doses of multiple medications. Patients who are chronically ill or neurologically impaired may require a tube indefinitely.
Jejunostomy is an alternative for patients who may not be able to have a feeding tube in their stomach.
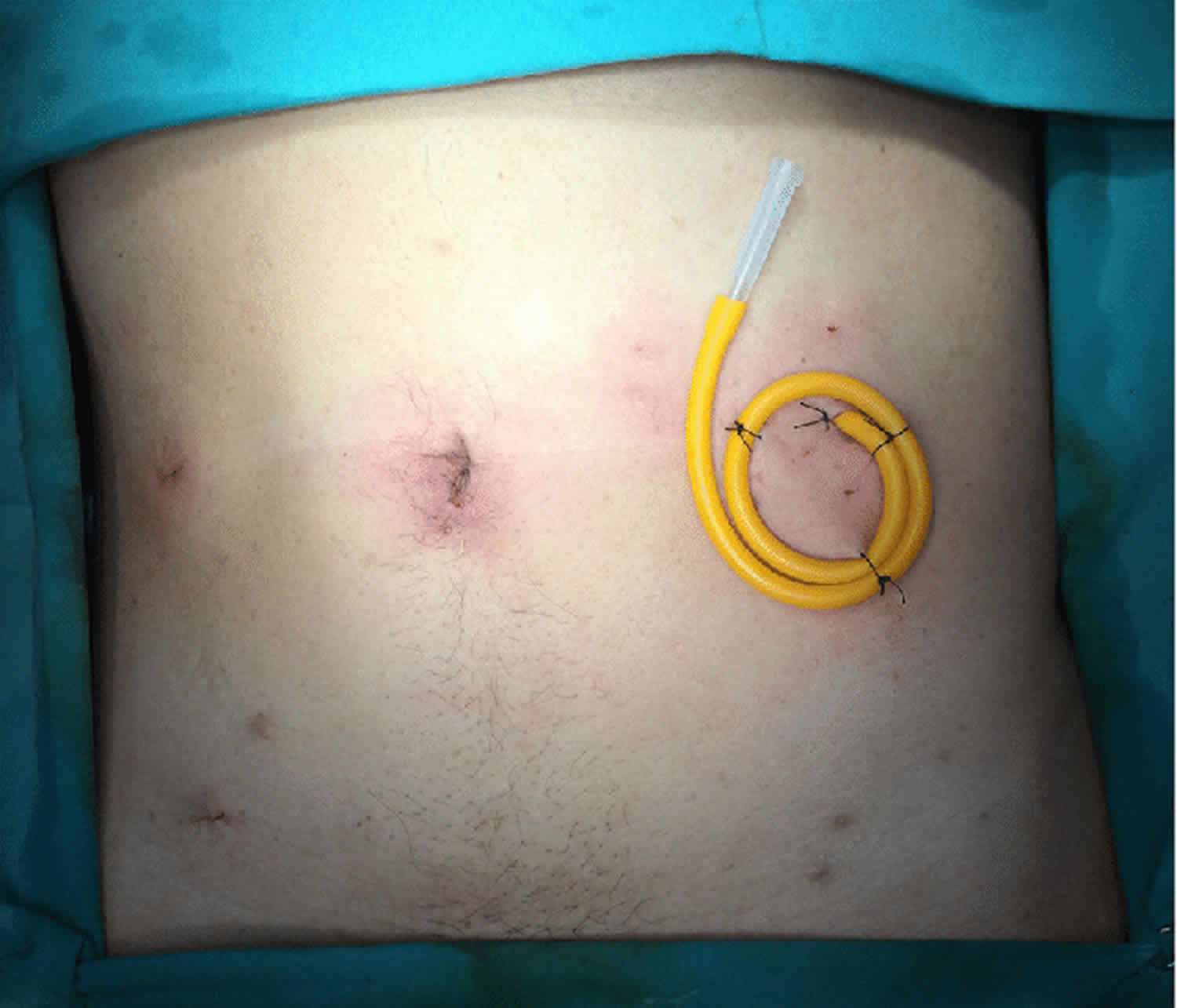
The jejunostomy tube may be placed laparoscopically (through a microscope inserted through the belly button) or surgically. Jejunostomy tube, like the gastrostomy tube (G-Tube), may be an actual tube or a button. Only liquids may pass through the jejunostomy tube.
The jejunostomy tube is put in place by one of these methods:
- Surgical – the tube is secured to the skin by stitching the tube’s external fixation disc to it. Occasionally it may be secured by an internal fixation disc.
- Via a percutaneous endoscopic gastrostomy (PEG) tube (a feeding tube placed into the stomach) – a much thinner jejunostomy extension tube is passed through the PEG tube into the jejunum. Careful placement of the jejunostomy tube is verified by X-Ray. The percutaneous endoscopic gastrostomy (PEG) tube is retained in the stomach by a disc to ensure it does not fall out. However, the jejunostomy extension tube is only secured by an adaptor at the end of the PEG tube.
- Radiologically – the tube is placed under X-Ray control, and is usually secured by stitching the external fixation disc to the skin.
You’ll need to know how to care for the jejunostomy tube and the skin where the tube enters the body.
Follow any specific instructions your nurse/doctor gives you. Use the information below as a reminder of what to do.
It is important to take good care of the skin around the tube to avoid getting an infection or skin irritation.
You will also learn how to change the dressing around the tube every day.
Make sure you keep the tube protected by taping it to the skin.
Your nurse may replace the tube every now and then.
Call your health care provider right away if any of the following occur:
- The tube is pulled out
- There is redness, swelling, smell, pus (unusual color) at the tube site
- There is bleeding around the tube
- The stitches are coming out
- There is leaking around the tube
- Skin or scarring is growing around the tube
- Vomiting
- Your stomach is bloated
Jejunostomy tube placement
If you have been unable to eat for over seven days, you may need to receive nutrients intravenously (called parenteral feeding) or via a tube into the stomach or small bowel (called enteral feeding). There are a number of ways that enteral feeding can be carried out, such as placing a tube through the nose and into the stomach. This is called a nasogastric (NG) or nasoenteric feeding tube, and is the preferred option if your anticipated need is less than 30 days.
However, nasoenteric tubes are not suitable for use longer than 30 days, as they can cause considerable discomfort and complications such as inflamed sinuses. If your need is anticipated to be for longer than 30 days, a better option for you is direct enteral access. This involves placing a tube directly into your stomach or bowel. This used to require surgery, but minimally invasive techniques are now available as an alternative, such as percutaneous image-guided jejunostomy.
During a percutaneous image-guided jejunostomy, an interventional radiologist will place a tube directly through the abdominal wall and into part of your small intestine called the jejunum, providing a way for nutrients to enter your body.
How does the procedure work?
The procedure is carried out using fluoroscopic guidance. The interventional radiologist will first inflate your stomach using a nasogastric tube. This will aid the fluoroscopy, the required puncture and enlargement of the tract. In rare cases, nasogastric access may not be possible, so the stomach is inflated using a needle introduced into the stomach, under image guidance.
To minimise the risk of puncturing the colon, the interventional radiologist may administer a contrast liquid into your colon the day before the jejunostomy procedure, to help visualise the colon.
During the jejunostomy procedure, the interventional radiologist will puncture the skin where the tube will be inserted, and then direct the needle under image guidance to the small intestine. The needle may be attached to an anchor, which the interventional radiologist will direct into the jejunum using a guidewire. To ensure there is enough space for the tube, the tract will be expanded using dilators or tiny balloons, which the interventional radiologist will insert using a separate guidewire.
The interventional radiologist will then insert a jejunostomy tube over the guidewire, using fluoroscopy to confirm its position. Once it has been confirmed that the tube is correctly placed, the interventional radiologist will remove the guidewires and secure the tube to the skin using anchors.
Jejunostomy tube care
Some aspects of care are dependent on the jejunostomy tube placement method used and what fixation devices in place.
If the external fixation device is STITCHED to the skin, this means there is no internal fixation disc. If the stitches come out there is a very high risk that the jejunostomy tube will also come out. The stitches need to be replaced, if you are agreeable, or the jejunostomy tube can be secured with an appropriate dressing over the fixation device, or with a suitable retaining type device e.g. ‘skin fix’ discs or Statlocks.
Your stoma site should be treated as a sterile wound for the first 7-10 days. Dressings are not usually necessary unless there is excessive fluid, or they are the only way in which to secure the jejunostomy tube. After this time the stoma can be washed with soap and water and dried thoroughly. Avoid using talcum powder and creams around this area. The external disc, clamp and adaptor end should be washed with soap and water. A soft toothbrush is useful to clean the adaptor thoroughly.
If the external fixation device is NOT STITCHED in place, this means an internal fixation disc/device secures the jejunostomy tube internally. The external fixation device can be released, and the stoma cleaned as before. DO NOT turn/rotate the jejunostomy tube. All other care is as described above.
Note that some hospitals now place Freka 15fr PEG tubes directly into the jejunum which can cause confusion with ongoing care. Stoma care following placement procedure is as above but the tube should NOT BE ADVANCED or ROTATED as this could cause a perforation.
Sometimes the jejunum is accessed by inserting a much thinner jejunostomy extension tube through an existing PEG tube. The PEG is retained in the stomach by an internal fixation disc through which the jejunostomy extension tube passes. Care of the stoma is as for any PEG tube except that the tube should NOT BE ROTATED as the jejunal extension has no retaining disc and could displace. There will be a special adaptor on the end of the PEG tube to facilitate use of the PEG and jejunal extension.
Radiologically placed tubes are usually stitched in place; therefore care is as described previously.
Jejunostomy tubes, if long term, can be replaced with another type of tube called ‘balloon retained tubes/buttons’.
Cleaning the skin around the jejunostomy tube
To clean the skin, you will need to change the bandages once a day or more if the area becomes wet or dirty.
The skin area should always be kept clean and dry. You will need:
- Warm soapy water and a washcloth
- Dry, clean towel
- Plastic bag
- Ointment or hydrogen peroxide (if your doctor recommends)
- Q-tips
Follow these guidelines every day for good health and skin care:
- Wash your hands well for a few minutes with soap and water.
- Remove any dressings or bandages on the skin. Place them in the plastic bag and throw the bag away.
- Check the skin for redness, odor, pain, puss, or swelling. Make sure the stitches are still in place.
- Use the clean towel or Q-tip to clean the skin around the jejunostomy tube 1 to 3 times a day with mild soap and water. Try to remove any drainage or crusting on the skin and tube. Be gentle. Dry the skin well with a clean towel.
- If there is drainage, place a small piece of gauze under the disc around the tube.
- DO NOT rotate the tube. This may cause it to become blocked.
Replacing the dressings around the jejunostomy tube
You will need:
- Gauze pads, dressings, or bandages
- Tape
Your nurse will show you how to place the new bandages or gauze around the tube and tape it securely to the abdomen.
Usually, split gauze strips are slipped over the tube and taped down on all four sides. Tape the tube down as well.
DO NOT use creams, powders, or sprays near the site unless the nurse says it is OK.
Jejunostomy tube maintenance
The following applies to all jejunostomy tubes regardless of how they are placed.
- As jejunostomy tubes are usually fine bore tubes, it is essential to ensure a thorough flushing regimen is in place. COOLED BOILED WATER is required and a new syringe used daily. To flush the jejunostomy tube, follow the instructions your nurse gave you. You will use the syringe to slowly push warm water into the side opening of the J-port.
- All medications need to be reviewed as bypassing the stomach can affect the absorption of some drugs and dosage may need to be altered. The correct preparation of medications, as far as possible is essential, i.e. liquid/soluble/dispersible.
Jejunostomy tube complications
Problems encountered with jejunostomy tubes are similar to those with PEG tubes. It is very common for air or gas to be present in the abdominal cavity as well as bruising. However, these usually have no adverse clinical effect.
Minor complications that you may experience include incorrect tube placement or tube movement, granulation tissue formation (skin that is red and sore as it heals) and minor bleeding from the site. Some patients develop a condition called intussusception, when part of the intestine folds onto another section of the intestine, causing bowel obstruction. Another possible complication is local infection.
Other procedure-related complications include damage to the abdominal or gastric walls caused by decreased blood supply and leakage from the catheter. Major complications are rare, but include perforation of the small intestine and inflammation of the lungs or airways caused by inhaling food or other substances.
Overgranulation of stoma site
This is excessive growth of ‘tissue’ around the stoma site. This can be caused by incorrect position of the external fixation disc and/or infection. If external fixation disc is not stitched to skin, ensure it is in correct position. Keeping the stoma site clean and dry can help minimize this problem. Some physicians may use silver nitrate to cauterize the tissue. Steroid creams may also be used, but long-term use does predispose to candida infections (fungal). A snug fitting tube that does not leak and avoiding trauma to the site will help avoid this common and recurrent problem. Call nutrition nurse/doctor if infection is suspected.
Tube blockage
This could possibly be due to inadequate flushing of tube, or delay in flushing tube after feed has finished. Blockage could also be caused by medication formulation, or the way it is administered.
To unblock tube:
- use warm boiled water to flush tube
- try using soda water or bicarbonate of soda/water solution to flush
- massage tube along its length between the thumb and forefinger and try flushing periodically
- wrap a hot flannel around the tube; ensure you protect your skin
If you are unable to unblock the tube then you will need to go to hospital.
Tube damage/ repair
Adaptors, clamps and external fixation devices can be replaced in the community – contact nutrition nurses.
Tube falls out
This has to be dealt with as soon as possible as the stoma will start to close. If able, and willing to do so, gently re-insert tube back into stoma (if tube is clean). Secure in place and summon help. If not able to re-insert tube, patient will need to go to hospital immediately.