Left anterior fascicular block
Left anterior fascicular block or LAFB also known left anterior hemiblock, is a heart disease in which scarring occurs in a section of the left ventricle identifiable from an abnormal electrocardiogram (ECG). LAFB occurs when the anterior fascicle of the left bundle branch is unable to conduct electrical signals. As a result, the impulses are sent to the left ventricle via the posterior fascicle. This results in a conduction delay and a slight widening of the QRS. The normal sequence of activation is altered in LAFB, with a resultant characteristic appearance on the ECG, associated with marked left axis deviation. LAFB has usually been considered a benign electrocardiographic finding and is therefore often neglected 1. However, recent studies showed that LAFB in elderly patients without clinical marker of cardiovascular disease, LAFB was associated with an increased risk of atrial fibrillation, congestive heart failure, and death 2. After adjusting for other potential confounding variables, LAFB posed a 57 percent greater risk for sudden cardiac death, an 89 percent greater risk for atrial fibrillation, and a 143 percent greater risk for heart failure. This study may suggest that LAFB, even in the absence of known high blood pressure or diabetes, should be thought of as a cardiovascular risk factor.
LAFB has recently attracted increasing attention 3. Left anterior fascicular block (LAFB) is caused by conduction failure or slowed conduction in the left anterior fascicle 4. The left anterior fascicle is delicate to injury leading to a high incidence of LAFB because the left anterior fascicle is thin and long, crosses the left ventricular (LV) out-flow tract, and blood is supplied from a single vessel.
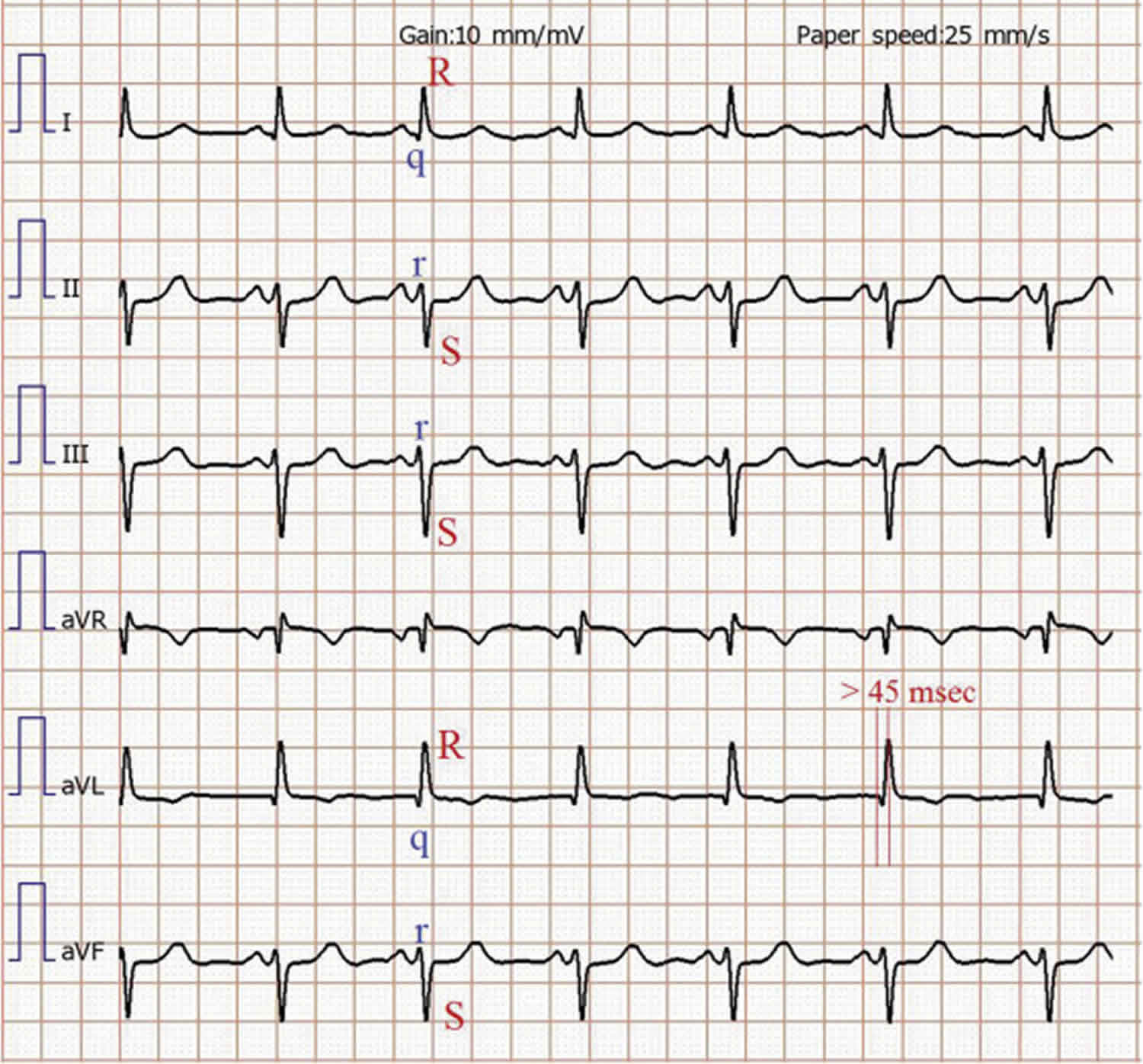
Figure 1. Left anterior fascicular block
Footnote: Left anterior fascicular block. Note the qR complexes in leads I and aVL and rS complexes in II, III, and aVF. Also note the prolonged R-wave peak time in aVL (the time from onset of the QRS to the peak of the R wave ≥45 msec).
Left anterior fascicular block causes
LAFB is a blockage of one of the electrical branches that delivers electrical signals to a part of the left ventricle, one of two chambers in the heart. Left anterior fascicular block results when the anterior fascicle of the left bundle branch is no longer able to conduct action potentials. Small studies suggest it is associated with fibrosis or scarring of the left ventricle, but the clinical ramifications of this have not been previously studied. It is unknown how many people LAFB affects.
The left superior anterior fascicle is anatomically narrow, like a single conducting wire. It is supplied by the left anterior descending (LAD) artery, and its narrowness and vulnerable blood supply make it susceptible to ischemic damage 5. When an LAFB exists, depolarization no longer begins in the septum, but instead at the endocardial surface of the inferoseptal wall of the heart via the posterior-inferior fascicle. The depolarization wave spreads towards the epicardium first, which creates a small positive deflection in the inferior leads.
Depolarization then proceeds upward towards the base of the heart, and left (where there is more myocardium). This produces a large negative deflection in the inferior leads, and a corresponding positive deflection in the lateral leads.
The changes to depolarization caused by the left anterior fascicular block result in a characteristic leftward axis on ECG (Figure 1).
- LAFB can be seen in approximately 4% of cases of acute myocardial infarction
- It is the most common type of intraventricular conduction defect seen in acute anterior myocardial infarction, and the left anterior descending artery is usually the culprit vessel.
- It can be seen with acute inferior wall myocardial infarction.
- Left anterior fascicular block is also associated with hypertensive heart disease, aortic valvular disease, cardiomyopathies, and degenerative fibrotic disease of the cardiac skeleton.
Left anterior fascicular block symptoms
The LAFB itself does not cause any symptoms. If action potentials do not go through the normal LAFB to the left ventricular myocardium to induce contraction of the heart muscle cells, then the action potentials will eventually get there by traveling through the posterior fascicle and right bundle branch. They will ultimately reach the muscle cells that the left anterior fascicle normally supplies by spreading electrical activity slowly from myocyte to myocyte through “intercolated disks.”
Left anterior fascicular block diagnosis
Typical characteristics of ECG criteria required for LAFB diagnosis on limb leads and precordial leads 6:
- Left axis deviation of at least -45 degrees;
- Lead aVL is qR pattern;
- Sharp R waves and deep S waves on leads II, III, and aVF;
- QRS widens no more than 0.02 s in pure LAFB, but the presence of myocardial infarction or left ventricular enlargement may produce a more substantial QRS widening;
- Deeper S waves on precordial leads 7.
Simulation study demonstrated that the LAFB-induced ECG patterns can be caused either by conduction block in the left anterior fascicle or by slowed conduction in the impaired myocardium. The main differences were the duration of QRS and wave amplitude. The presences of decreased amplitude and prolonged duration of QRS are good clinical indicators of impaired conduction in ventricular myocardium. Remarkably, the decreasing amplitude of conduction velocity in ventricular myocardium played an important role in affecting the ECG patterns. The changes of QRS morphologies were insensitive when the degree of decrease of the velocity was small. Obvious prolongation and amplitude changing of QRS were observed until the velocity decreased to 30% of the normal case. The area of slowed ventricular activation also affected the ECG patterns. Wider S waves on the precordial leads would be observed with the expansion of the slowed conduction area. This phenomenon has been shown in previous research (Bacharova et al., 2013, 2015). However, the QRS morphologies on the limb leads were presented in different patterns (e.g. Q waves were observed on leads III and aVF). This indicated that the QRS complex morphology not only reveals the presence of regional slowed ventricular activation, but also contains information about the location of the impaired myocardium. So the relationship between the area of slowed conduction velocity and ECG patterns needs further research.
Left anterior fascicular block treatment
There currently is no treatment for people with LAFB. If there is an underlying heart disease the treatment is directed at the underlying disease.
- Elizari MV, Acunzo RS, Ferreiro M. Hemiblocks revisited. Circulation. 2007;115(9):1154–1163.[↩]
- Mandyam MC, Soliman EZ, Heckbert SR, Vittinghoff E, Marcus GM. Long-term outcomes of left anterior fascicular block in the absence of overt cardiovascular disease. JAMA. 2013;309(15):1587–1588. doi:10.1001/jama.2013.2729 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3979298[↩]
- Nguyen KT, Vittinghoff E, Dewland TA, et al. Electrocardiographic predictors of incident atrial fibrillation. Am J Cardiol. 2016;118(5):714–719. doi: 10.1016/j.amjcard.2016.06.008[↩]
- Gao Y, Xia L, Gong YL, Zheng DC. Electrocardiogram (ECG) patterns of left anterior fascicular block and conduction impairment in ventricular myocardium: a whole-heart model-based simulation study. J Zhejiang Univ Sci B. 2018;19(1):49–56. doi:10.1631/jzus.B1700029 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5802974[↩]
- Piktel JS. Cardiac Rhythm Disturbances. In: Tintinalli JE, ed. Tintinalli’s Emergency Medicine. Seventh Edition ed. New York: McGraw-Hill; 2011.[↩]
- Gao Y, Xia L, Gong YL, Zheng DC. Electrocardiogram (ECG) patterns of left anterior fascicular block and conduction impairment in ventricular myocardium: a whole-heart model-based simulation study. J Zhejiang Univ Sci B. 2018;19(1):49–56. doi:10.1631/jzus.B1700029 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5802974 [↩]
- Elizari MV, Acunzo RS, Ferreiro M. Hemiblocks revisited. Circulation. 2007;115(9):1154–1163. doi: 10.1161/CIRCULATIONAHA.106.637389.[↩]