Lymphocytic pleocytosis
Lymphocytic pleocytosis is an abnormal increase in the amount of lymphocytes in the cerebrospinal fluid (CSF). It is usually considered to be a sign of infection or inflammation within the nervous system, and is encountered in a number of neurological diseases, such as pseudomigraine (syndrome of transient headache and neurological deficits with cerebrospinal fluid lymphocytosis [HaNDL]), Susac’s syndrome, and encephalitis. While lymphocytes make up roughly a quarter of all white blood cells (WBC) in the body, they are generally rare in the CSF. Under normal conditions, there are usually less than 5 white blood cells per µL of CSF. In a pleocytic setting, the number of lymphocytes can jump to more than 1,000 cells per µL. Increases in lymphocyte count are often accompanied by an increase in cerebrospinal protein concentrations in addition to pleocytosis of other types of white blood cells.
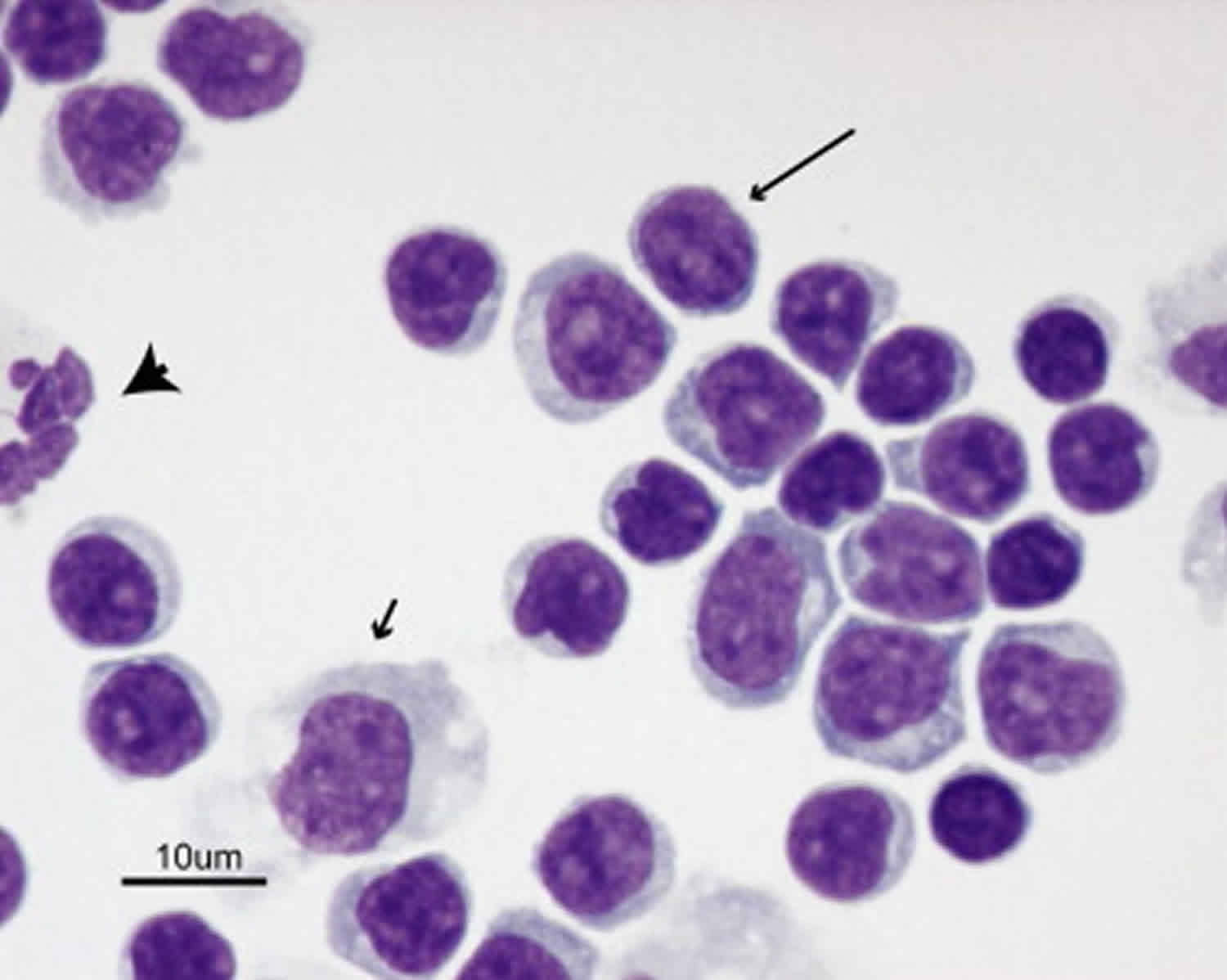
Lymphocytes are a type of white blood cell. Lymphocytes are part of your immune system and work to fight off infections. Lymphocytes occur in two forms: B cells, which produce antibodies, and T cells, which recognize foreign substances and process them for removal.
Lymphocytic pleocytosis causes
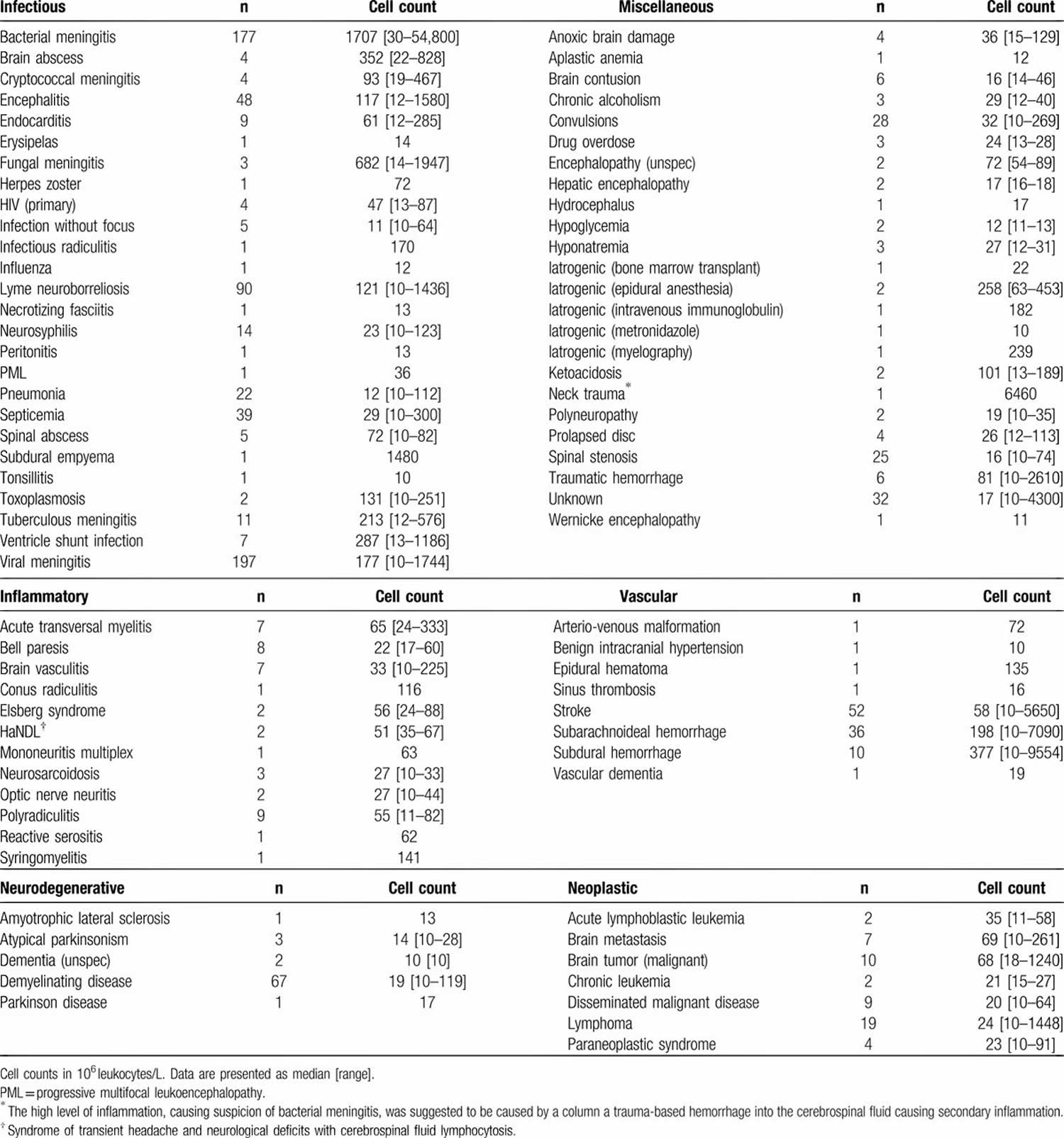
In a study involving a total of 1058 CSF samples from 1054 patients in Denmark between 2003 to 2010, infections were the most common cause of CSF pleocytosis (61.4%) followed by miscellaneous causes (12.7%), vascular (9.7%), neurodegenerative (7%), neoplastic (5%), and inflammatory conditions (4.2%) 1. Only infections presented with CSF leukocyte counts >100 × 106/L. Infections represented 82.6% of all cases with a leukocyte count >100 × 106/L whereas 56.3% of cases with at leukocyte counts <100 × 106 /L were dominated by disease not related to infection.
Eighty-one cases (7.7%) presented with CSF pleocytosis due to infections with a focus outside the CNS such as pneumonia, endocarditis, and septicemia. No microorganisms were detected and the samples assumed to represent sterile inflammation secondary to other infection.
In 32 cases (3%), no diagnosis was established. These cases were labeled “unknown.”
Infectious causes of CSF pleocytosis were further divided into the following groups: acute bacterial, chronic bacterial, fungal, and viral CNS infections and inflammation secondary to an infectious focus outside the CNS (extra-CNS). Only 2 cases of parasitic CNS infections were identified and they were not included in this context.
Other causes of lymphocytic pleocytosis include:
- Autoimmune disorders such as paraneoplastic anti-NMDA receptor encephalitis, Hashimoto’s encephalopathy (also known as steroid-responsive encephalopathy associated with autoimmune thyroiditis (SREAT), SLE, vasculitides, demyelinating diseases.
- Marburg variant multiple sclerosis (MS) called fulminant multiple sclerosis: an acute, fulminant form of multiple sclerosis (MS), often with large white matter lesions (>2cm). Median age is 37 and 1 year mortality is high.
- Acute Disseminated Encephalomyelitis (ADEM): Acute disseminated encephalomyelitis (ADEM) is characterized by a brief but widespread attack of inflammation in the brain and spinal cord that damages myelin – the protective covering of nerve fibers. ADEM often follows viral or bacterial infections, or less often, vaccination for measles, mumps, or rubella. The symptoms of ADEM appear rapidly, beginning with encephalitis-like symptoms such as fever, fatigue, headache, nausea and vomiting, and in the most severe cases, seizures and coma. ADEM typically damages white matter (brain tissue that takes its name from the white color of myelin), leading to neurological symptoms such as visual loss (due to inflammation of the optic nerve) in one or both eyes, weakness even to the point of paralysis, and difficulty coordinating voluntary muscle movements (such as those used in walking). ADEM is sometimes misdiagnosed as a severe first attack of multiple sclerosis (MS), since the symptoms and the appearance of the white matter injury on brain imaging may be similar. However, ADEM has several features which differentiate it from MS. First, unlike MS patients, persons with ADEM will have rapid onset of fever, a history of recent infection or immunization, and some degree of impairment of consciousness, perhaps even coma; these features are not typically seen in MS. Children are more likely than adults to have ADEM, whereas MS is a rare diagnosis in children. In addition, ADEM usually consists of a single episode or attack of widespread myelin damage, while MS features many attacks over the course of time. Doctors will often use imaging techniques, such as MRI (magnetic resonance imaging), to search for old and new lesions (areas of damage) on the brain. The presence of older brain lesions on MRI suggest that the condition may be MS rather than ADEM, since MS can cause brain lesions before symptoms become obvious. In rare situations, a brain biopsy may be necessary to differentiate between ADEM and some other diseases that involve inflammation and damage to myelin.
- Medications such nonsteroidal anti-inflammatory drugs (NSAIDs), Septra (combination of sulfamethoxazole and trimethoprim) and intravenous immunoglobulin (IVIg)
- Levamisole-induced encephalitis: very rare but has been seen in case reports, apparently first reported in 1988, usually seen with diffuse cerebral lesions with early mental symptoms and motor weakness usually 10-14 days after exposure.
Table 1. Lymphocytic pleocytosis causes
[Source 1 ]Lymphocytic pleocytosis treatment
Lymphocytic pleocytosis treatment is to treat underlting disease responsible for the increase in the amount of lymphocytes in the cerebrospinal fluid (CSF).
- Baunbæk Egelund G, Ertner G, Langholz Kristensen K, Vestergaard Jensen A, Benfield TL, Brandt CT. Cerebrospinal fluid pleocytosis in infectious and noninfectious central nervous system disease: A retrospective cohort study. Medicine (Baltimore). 2017;96(18):e6686. doi:10.1097/MD.0000000000006686 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5419909[↩][↩]