Mallampati classification
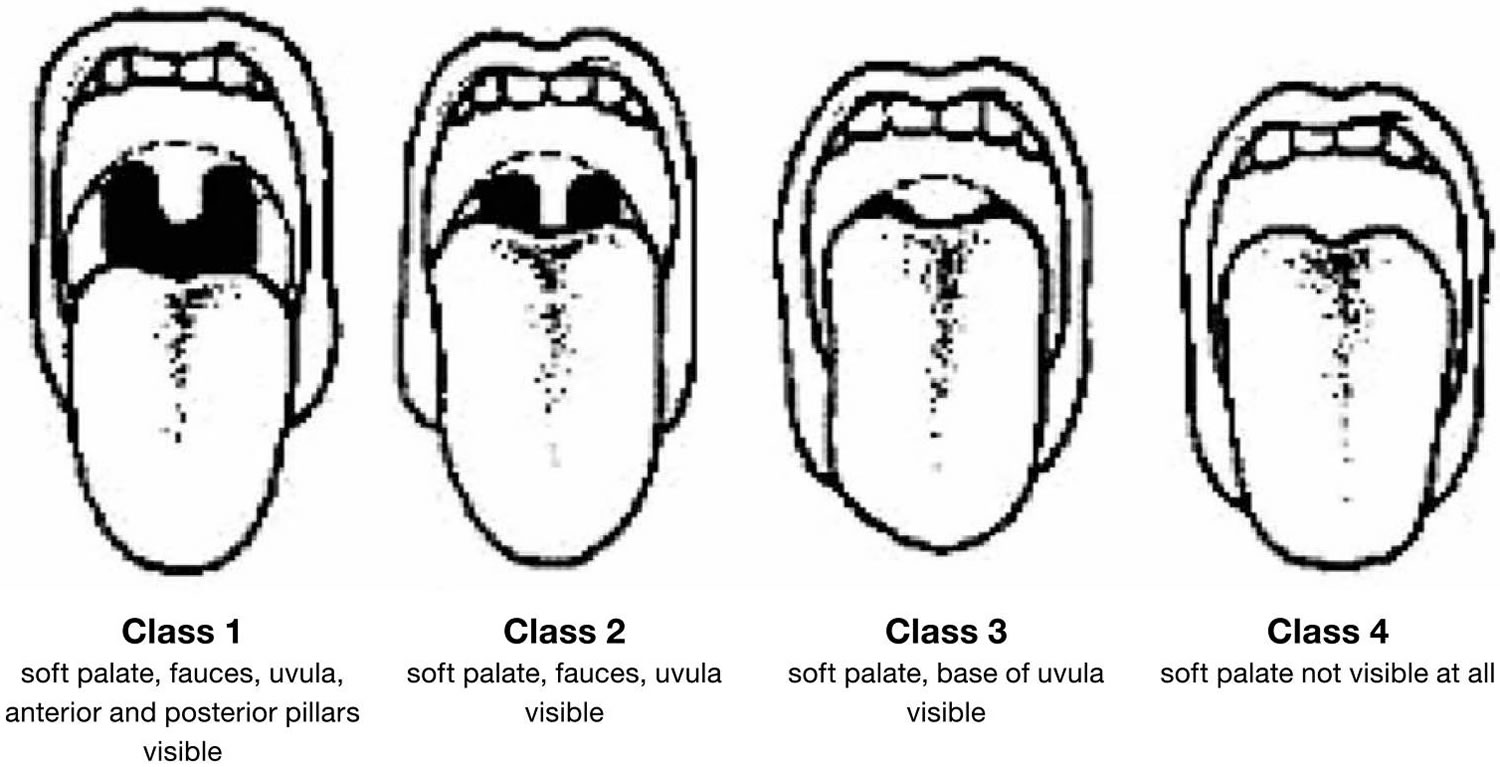
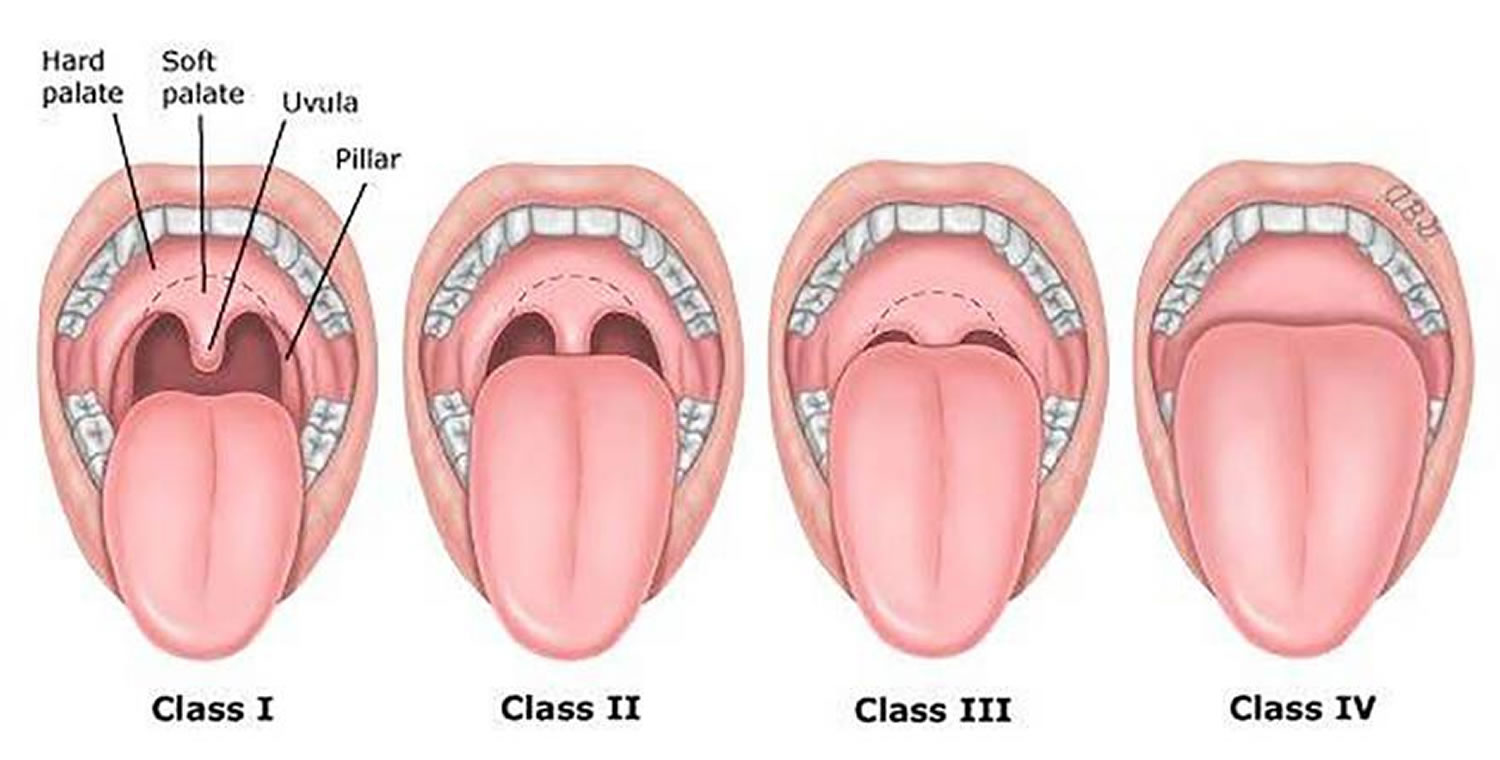
Mallampati test is a subjective evaluation of the ratio of oral cavity volume to tongue volume 1. Mallampati et al. 2 originally proposed three oropharyngeal classes, but modified this to comprise four classes on the basis of experience with the technique. Mallampati test is performed with the patient sitting up straight, the head in a neutral position, mouth fully opened and tongue fully extended (without speaking or saying “ahh”) and involves evaluating the visibility of anatomical structures, as shown in Figure 1. The difficulty of intubation is then classified, a Class 1 airway being the easiest to manage and control by intubation, and a Class 4 airway being potentially the most difficult.
The Mallampati score screening test is designed to help clinicians predict the potential difficulty of intubation during airway control and management, with those who score 3 or 4 being more difficult to intubate, and has been validated in children 3. The Mallampati scale is therefore useful for assessment and its use can prevent problems 4. The Mallampati test cannot be used to predict potential difficulty with perfect accuracy, however, and it would be dangerous to assume that an evaluation indicating an easy intubation will necessarily always be a simple intubation. A patient whose airway defies accurate prediction has the highest likelihood of catastrophe during induction.
The American Academy of Sleep Medicine and Dutch Central Accompagnement Organization both state that the Mallampati score has additional value in diagnosing obstructive sleep apnea in adults 5. There are several adult studies with mixed results regarding the utility of Mallampati score in predicting obstructive sleep apnea 6. There have been no studies in the pediatric population looking at the clinical use of Mallampati score to predict obstructive sleep apnea and its severity. Kumar et al 7 showed that both the Mallampati score and tonsillar size are independent predictors of obstructive sleep apnea 7. Oral examination including Mallampati score and tonsillar size should be considered when evaluating a patient for obstructive sleep apnea. Both the Mallampati score and tonsillar size can be used to prioritize children who may need polysomnography 7.
Modified Mallampati classification 8
- Class 0: Ability to see any part of the epiglottis upon mouth opening and tongue protrusion
- Class 1: Soft palate, fauces, uvula, pillars visible
- Class 2: Soft palate, fauces, uvula visible
- Class 3: Soft palate, base of uvula visible
- Class 4: Soft palate not visible at all
Predictive value of modified Mallampati classification 9
- Difficult laryngoscopy: Good accuracy (area under summary receiver operating characteristic [SROC] curve 0.89 ± 0.05)
- Difficult intubation: Good accuracy (area under sROC curve 0.83 ± 0.03)
- Difficult mask ventilation: Poor predictor overall, but class III-IV can suggest difficulty with mask ventilation
- Used alone, the Mallampati tests have limited accuracy for predicting the difficult airway and thus are not useful screening tests.
- Interobserver variability, measured by intraclass correlation coefficients, is well documented for the Mallampati classification.
- Mallampati classification is only one of 11 non-reassuring findings during airway examination.
Non-reassuring findings during airway physical examination 10
- Relatively long upper incisors
- Prominent “overbite” (maxillary incisors anterior to mandibular incisors)
- Patient cannot bring mandibular incisors anterior to (in front of) maxillary incisors
- Interincisor distance less than 3 cm
- Uvula not visible when tongue is protruded with patient in sitting position (eg, Mallampati class >2)
- Palate highly arched or very narrow
- Mandibular space stiff, indurated, occupied by mass, or nonresilient
- Thyromental distance less than 3 ordinary finger breadths
- Short neck length
- Thick neck circumference
- Patient cannot touch tip of chin to chest or cannot extend neck
Figure 1. Modified Mallampati classification system
- Mallampati S. Clinical sign to predict difficult tracheal intubation (hypothesis). Canadian Anaesthetists Society Journal. 1983;30:316–7.
- Mallampati S, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Canadian Anaesthetists Society Journal. 1985;32:429–34.
- Inal MT, Memis D, Sahin SH, et al. Comparison of different tests to determine difficult intubation in pediatric patients. Rev Bras Anesthesiol. 2014;64(6):391–4.
- Kluger MT, et al. Inadequate pre-operative evaluation and preparation: a review of 197 reports from the Australian incident monitoring study. Anaesthesia. 2000;55:1173–8.
- Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD, Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009 Jun 15; 5(3):263-76.
- Bins S, Koster TD, de Heij AH, et al. No evidence for diagnostic value of Mallampati score in patients suspected of having obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2011;145:199–203.
- Kumar HV, Schroeder JW, Gang Z, Sheldon SH. Mallampati score and pediatric obstructive sleep apnea. J Clin Sleep Med. 2014;10(9):985–990. Published 2014 Sep 15. doi:10.5664/jcsm.4032 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153107
- Mallampati SR, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985 Jul. 32 (4):429-34.
- Kheterpal S, et al. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009 Apr. 110 (4):891-7.
- Apfelbaum JL, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013 Feb. 118 (2):251-70.