Mean arterial pressure
Mean arterial pressure (MAP) is a term used in medicine to describe the average blood pressure in a patient’s arteries during one cardiac cycle. Mean arterial pressure is defined as the average arterial pressure during a single cardiac cycle. Mean arterial pressure (MAP) is considered a better indicator of perfusion to vital organs than systolic blood pressure (SBP).
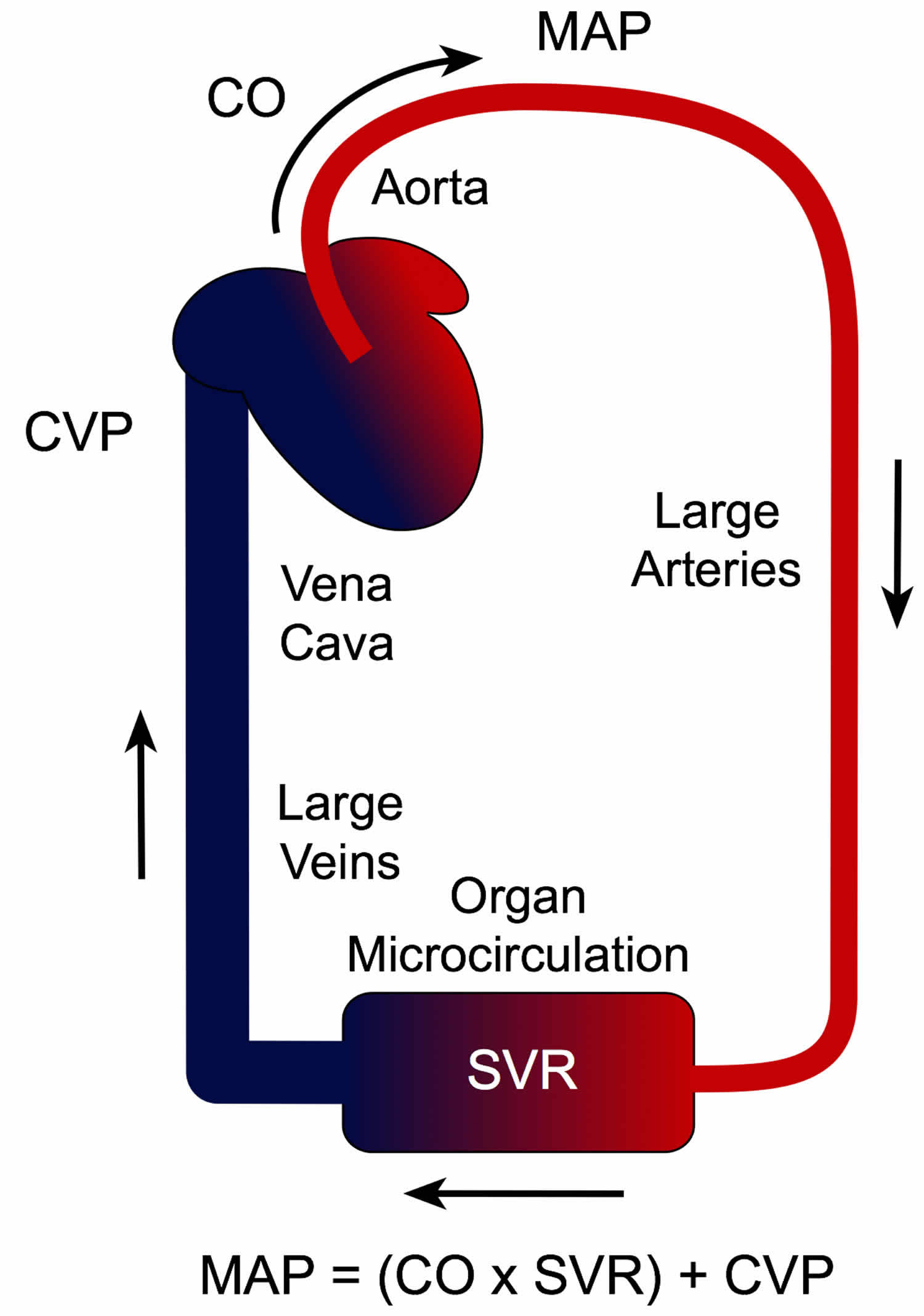
The definition of mean arterial pressure (MAP) is the average arterial pressure throughout one cardiac cycle, systole, and diastole 1. Mean arterial pressure (MAP) is influenced by cardiac output (CO), systemic vascular resistance (SVR) and central venous pressure (CVP), each of which is under the influence of several variables (see Figure 2 below) 2.
Therefore, changes in either cardiac output (CO) or systemic vascular resistance (SVR) will affect mean arterial pressure (MAP). As shown in the graph (see Figure 2 below) , increasing cardiac output (CO) increases mean arterial pressure. Likewise, increasing systemic vascular resistance (SVR) increases mean arterial pressure at any given cardiac output (CO). If cardiac output (CO) and systemic vascular resistance (SVR) change reciprocally and proportionately, then mean arterial pressure will not change. For example, if cardiac output (CO) doubles and systemic vascular resistance (SVR) decreases by one-half, mean arterial pressure does not change (if central venous pressure (CVP) = 0). It is important to note that variables found in equation 1 are all interdependent. This means that changing one variable changes all of the others.
Mean arterial pressure is normally between 65 and 110 mmHg, with a mean arterial pressure (MAP) of over 70mmHg needed for basic organ function 3.
In septic shock, a mean arterial pressure (MAP) of 65 mmHg is considered sufficient for end-organ perfusion 4.
Mean arterial pressure formula:
- Mean arterial pressure = (cardiac output x systemic vascular resistance) + central venous pressure
Central venous pressure is usually small enough to be neglected in this formula.
Cardiac output is calculated as the product of heart rate and stroke volume. The determination of stroke volume is by ventricular inotropy and preload. Preload is affected by blood volume and the compliance of veins. Increasing the blood volume increases the preload, increasing the stroke volume, and therefore increasing cardiac output. Afterload also affects the stroke volume in that an increase in afterload will decrease stroke volume. Heart rate is affected by the chronotropy, dromotropy, and lusitropy of the myocardium.
Systemic vascular resistance is determined primarily by the radius of the blood vessels. Decreasing the radius of the vessels increases vascular resistance. Increasing the radius of the vessels would have the opposite effect. Blood viscosity can also affect systemic vascular resistance. An increase in hematocrit will increase blood viscosity and increase systemic vascular resistance. Viscosity, however, is considered only to play a minor role in systemic vascular resistance 5.
The mean arterial pressure (MAP) can also be calculated by the following formula 6:
- Mean arterial pressure (MAP) = [(2/3) x (diastolic blood pressure)] + [(1/3) x (systolic blood pressure)]
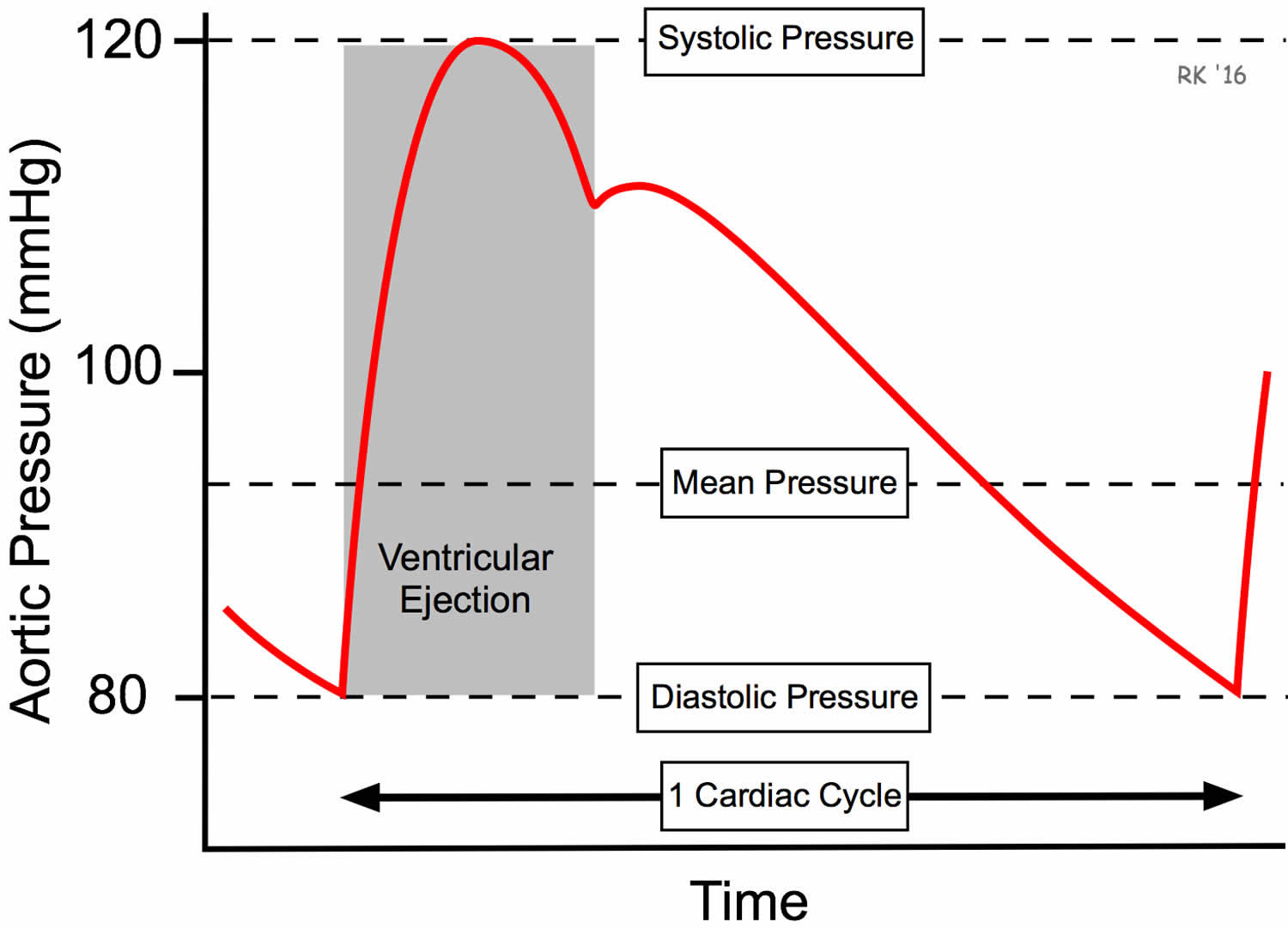
In practice, mean arterial pressure (MAP) is not determined by knowing the cardiac output (CO) and systemic vascular resistance (SVR), but rather by direct or indirect measurements of arterial pressure. From the aortic pressure trace over time (see Figure 1), the shape of the pressure trace yields a mean pressure value (geometric mean) that is less than the arithmetic average of the systolic and diastolic pressures as shown to the right.
At normal resting heart rates, mean arterial pressure can be approximated by the following equation 7:
- Mean arterial pressure (MAP) = diastolic blood pressure + [(1/3) x (systolic blood pressure – diastolic blood pressure)]
For example, if systolic pressure is 120 mmHg and diastolic pressure is 80 mmHg (as shown in the Figure 1), then the mean arterial pressure is approximately 93 mmHg using this calculation. At high heart rates, however, mean arterial pressure is closer to the arithmetic average of systolic and diastolic pressure (therefore, almost 100 mmHg in this example) because of the change in shape of the arterial pressure pulse (it becomes narrower). To determine mean arterial pressure with absolute accuracy, analog electronic circuitry or digital techniques are used. In normal clinical practice, however, systolic and diastolic pressures are measured with a sphygmomanometer, not mean arterial pressure. Once these values are known, a mean arterial pressure (MAP) value can easily be determined. An oscillometric blood pressure device can also be used to measure mean arterial pressure (MAP). Echocardiography can be used to evaluate the function of the myocardium further, determine the left ventricular ejection fraction, and cardiac output. Central venous catheters, placed in the right atrium, can be used to measure central venous pressure when necessary. Mean arterial pressure (MAP) measurement is only measured when systemic vascular resistance (SVR) needs to be calculated 7.
Figure 1. Mean arterial pressure
Figure 2. Mean arterial pressure is determined by the cardiac output (CO), systemic vascular resistance (SVR), and central venous pressure (CVP)
Figure 3. Mean arterial pressure
Mean arterial pressure equation
A common method used to estimate the mean arterial pressure (MAP) is the following formula 6:
- Mean arterial pressure (MAP) = [(2/3) x (diastolic blood pressure)] + [(1/3) x (systolic blood pressure)]
Another method used to estimate the mean arterial pressure (MAP) is the following formula 1:
- Mean arterial pressure (MAP) = diastolic blood pressure + 1/3 (systolic blood pressure – diastolic blood pressure)
- Mean arterial pressure (MAP) = diastolic blood pressure + 1/3 (pulse pressure)
Pulse pressure is the change in blood pressure seen during a contraction of the heart (the difference between diastolic and systolic blood pressure). The normal pulse pressure is 30-40 mmHg. A pressure that exceeds this is called a wide pulse pressure. A pressure that is smaller than this (<25 mmHg) is a narrow pulse pressure.
This method is often more conducive to measuring mean arterial pressure (MAP) in most clinical settings as it offers a quick means of calculation if the blood pressure is known.
A third method used to estimate the mean arterial pressure (MAP) is the following formula 7:
- Mean arterial pressure (MAP) = (cardiac output x systemic vascular resistance) + central venous pressure
Central venous pressure (CVP) is usually small enough (normally near 0 mmHg) to be neglected in this formula.
Cardiac output (CO) is defined as the amount of blood pumped by the left ventricle in unit time. Cardiac output is an indicator of the left ventricular function.
- Cardiac output = Stroke Volume x Heart Rate
Therefore, if there are 70 beats per minute, and 70 ml blood is ejected with each beat of the heart, the cardiac output is 4900 ml/minute. The normal cardiac output is 5-6L/min and it can increase up to 5 times during exercise.
Systemic vascular resistance (SVR) also referred to as the total peripheral resistance refers to the cumulative resistance of the thousands of arterioles in your body, or the lungs, respectively. Systemic vascular resistance is approximately equal to the resistance of the arterioles, since the arterioles are the chief resistance blood vessels in your body.
Systemic vascular resistance occurs when arterioles are unable to completely relieve pressure in the arteries. When the heart contracts, blood enters the arteries faster than it can leave, and the arteries stretch from the pressure. Although the blood vessels return to their normal state during diastole, the heart will contract again before all the blood has completely flowed into the arterioles. This inhibits the arterioles’ ability to fully relieve the pressure in the arteries, causing systemic vascular resistance.
- Systemic Vascular Resistance = (Mean Arterial Pressure – Central Venous Pressure) / Cardiac Output
Mean arterial pressure regulation
Mean arterial pressure regulation is on the cellular level through a complex interplay between the cardiovascular, renal, and autonomic nervous systems. Mean arterial pressure functions to perfuse blood to all the tissues of the body to keep them functional. Mechanisms are in place to ensure that the mean arterial pressure remains at least 60 mmHg so that blood can effectively reach all tissues.
The cardiovascular system determines the mean arterial pressure through cardiac output and systemic vascular resistance. Cardiac output is regulated on the level of intravascular volume, preload, afterload, myocardial contractility, heart rate, and conduction velocity. Systemic vascular resistance regulation is via vasoconstriction and dilation.
The renal system affects mean arterial pressure via the renin-angiotensin-aldosterone system; this is a cascade that ends in the release of aldosterone, which increases sodium reabsorption in the distal convoluted tubules of the kidneys and ultimately increases plasma volume.
The autonomic nervous system plays a role in regulating mean arterial pressure via baroreceptors located in the carotid sinus and aortic arch. The autonomic nervous system can affect both cardiac output and systemic vascular resistance to maintain mean arterial pressure in the ideal range.
Alterations in systemic vascular resistance and cardiac output are responsible for changes in mean arterial pressure.
The most influential variable in determining the systemic vascular resistance is the radius of the blood vessels themselves. The radius of these vessels is influenced both by local mediators and the autonomic nervous system. Endothelial cells lining the blood vessels produce and respond to vasoactive substances to either dilate or constrict the vessels depending on the body’s needs.
When mean arterial pressure is elevated, shearing forces on the vessel walls induce synthesis of nitric oxide (NO) in endothelial cells. Nitric oxide (NO) diffuses into vascular smooth muscle cells where it activates guanylyl cyclase and results in the dephosphorylation of GTP to cGMP. The cGMP acts as a second messenger within the cell, ultimately leading to smooth muscle relaxation and dilation of the vessel. Other vasodilating compounds produced locally are bradykinin and the various prostaglandins, which act through similar mechanisms to result in the relaxation of vascular smooth muscle 8.
Endothelin is a local vasoactive compound that has the opposite effects as nitric oxide (NO) on vascular smooth muscle. A reduced mean arterial pressure triggers the production of endothelin within the endothelial cells. Endothelin then diffuses into the vascular smooth muscle cells to bind the ET-1 receptor, a Gq-coupled receptor, resulting in the formation of IP3 and calcium release from the sarcoplasmic reticulum, which leads to smooth muscle contraction and constriction of the vessel 9.
The autonomic nervous system also plays a vital role in regulating mean arterial pressure via the baroreceptor reflex. The arterial baroreceptors found in the carotid sinus and aortic arch act through a negative feedback system to maintain the mean arterial pressure in the ideal range. Baroreceptors communicate with the nucleus tractus solitarius in the medulla of the brainstem via the glossopharyngeal nerve (cranial nerve IX) in the carotid sinus and the vagus nerve (cranial nerve X) in the aortic arch. The nucleus tractus solitarius determines the sympathetic or parasympathetic tone to either raise or lower mean arterial pressure according to the body’s needs 10.
When mean arterial pressure is elevated, increasing baroreceptor stimulation, the nucleus tractus solitarius decreases sympathetic output and increases parasympathetic output. The increase in parasympathetic tone will decrease myocardial chronotropy and dromotropy, with less pronounced effects on inotropy and lusitropy, via the effect of acetylcholine on M2 muscarinic receptors in the myocardium. M2 receptors are Gi-coupled, inhibiting adenylate cyclase and causing a decrease in cAMP levels within the cell. The result is a decrease in cardiac output and a subsequent decrease in mean arterial pressure.
Conversely, when the mean arterial pressure decreases, baroreceptor firing decreases and the nucleus tractus solitarius acts to reduce parasympathetic tone and increase sympathetic tone. The increase in sympathetic tone will increase myocardial chronotropy, dromotropy, inotropy, and lusitropy via the effect of epinephrine and norepinephrine on beta1 adrenergic receptors in the myocardium. Beta1 receptors are Gs-coupled, activating adenylate cyclase and causing an increase in cAMP levels within the cell. In addition to this, epinephrine and norepinephrine act on vascular smooth muscle cells via alpha1 adrenergic receptors to induce vasoconstriction of both arteries and veins. Alpha1 receptors are Gq-coupled and act via the same mechanism as the ET-1 receptor mentioned above. The combination of these events increases both cardiac output and systemic vascular resistance, effectively increasing mean arterial pressure.
Increased sympathetic tone also occurs during exercise, severe hemorrhage, and in times of psychologic stress.
The renal system helps to maintain mean arterial pressure primarily through the regulation of plasma volume, which directly affects cardiac output. A drop in renal perfusion triggers the release of renin, launching the renin-angiotensin-aldosterone cascade. Aldosterone acts on the distal convoluted renal tubules to increase sodium reabsorption and therefore increase water reuptake and plasma volume. Angiotensin II acts on the vasculature via the AT1 receptor to induce smooth muscle contraction, resulting in vasoconstriction. The AT1 receptor is Gq-coupled and works via the same mechanism as the ET-1 and alpha1 receptors mentioned above. Together these changes will increase both cardiac output and systemic vascular resistance to increase mean arterial pressure.
- DeMers D, Wachs D. Physiology, Mean Arterial Pressure. [Updated 2019 Feb 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538226[↩][↩]
- Berlin DA, Bakker J. Starling curves and central venous pressure. Crit Care. 2015 Feb 16;19:55.[↩]
- Moran D, Epstein Y, Keren G, Laor A, Sherez J, Shapiro Y. Calculation of mean arterial pressure during exercise as a function of heart rate. Appl Human Sci. 1995 Nov;14(6):293-5.[↩]
- Rodriguez R, Cucci M, Kane S, Fernandez E, Benken S. Novel Vasopressors in the Treatment of Vasodilatory Shock: A Systematic Review of Angiotensin II, Selepressin, and Terlipressin. J Intensive Care Med. 2018 Dec 18;:885066618818460.[↩]
- Magder S. Volume and its relationship to cardiac output and venous return. Crit Care. 2016 Sep 10;20:271.[↩]
- Delong C, Sharma S. Physiology, Peripheral Vascular Resistance. [Updated 2019 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538308[↩][↩]
- Mean Arterial Pressure. https://www.cvphysiology.com/Blood%20Pressure/BP006[↩][↩][↩]
- Lundberg JO, Weitzberg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov. 2008 Feb;7(2):156-67.[↩]
- Trindade M, Oigman W, Fritsch Neves M. Potential Role of Endothelin in Early Vascular Aging. Curr Hypertens Rev. 2017;13(1):33-40.[↩]
- Andresen MC, Doyle MW, Jin YH, Bailey TW. Cellular mechanisms of baroreceptor integration at the nucleus tractus solitarius. Ann. N. Y. Acad. Sci. 2001 Jun;940:132-41.[↩]