Migraine postdrome
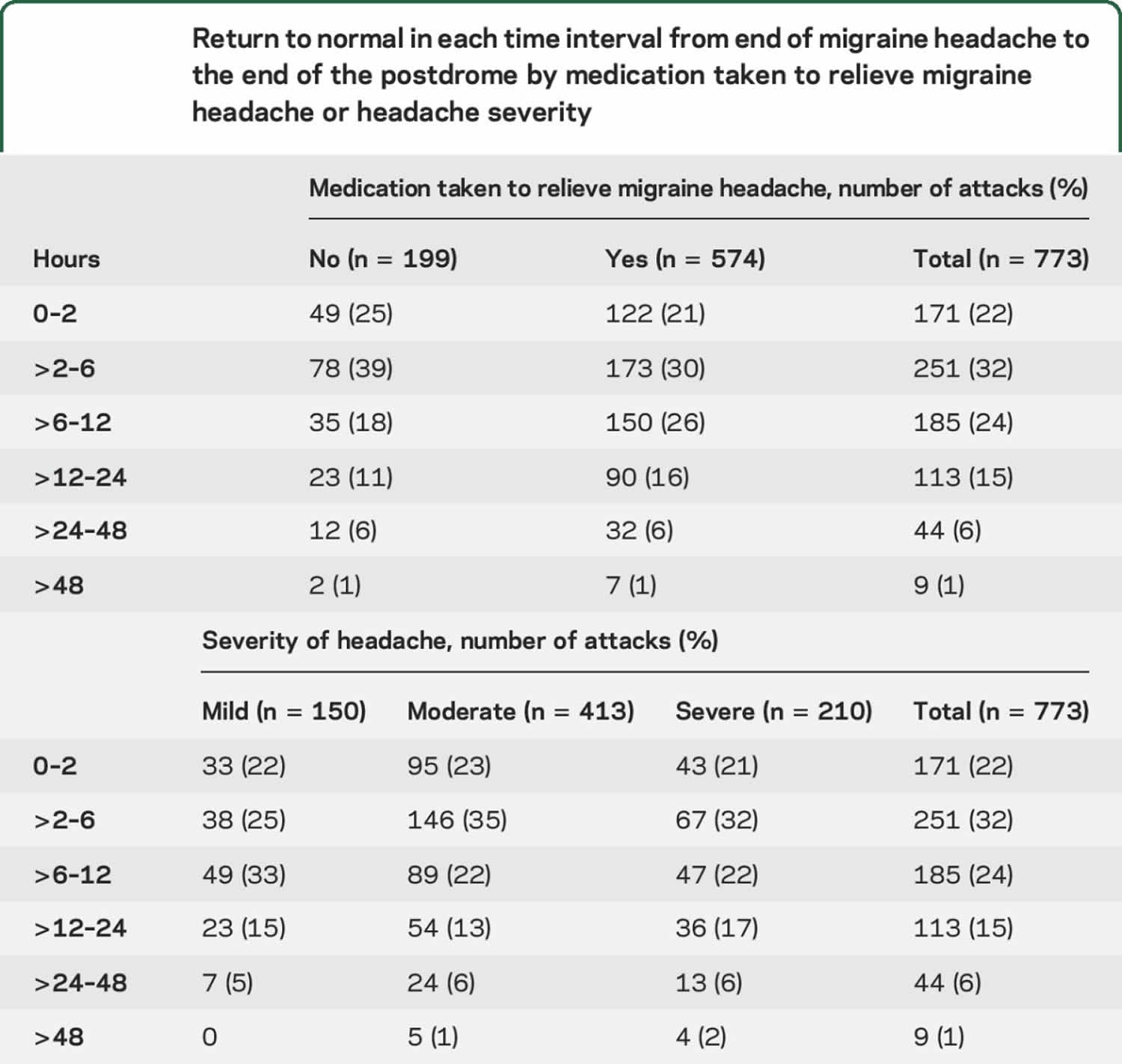
Migraine postdrome also called the “migraine hangover,” are symptoms following the migraine headache, which is the fourth and final phase of a migraine attack 1. Common migraine postdrome symptoms may include feeling exhausted, weak, fatigue, tiredness, nausea, sensitivity to light, dizziness, body aches, difficulty concentrating, confused 2 and reduced mood after a migraine 3. One postdrome sufferer described the day after a migraine headache as feeling like “a mental fog, one so heavy that even routine tasks take on an otherworldly quality.” Migraine postdrome symptoms last hours or even several days 4. This study 5 showed that postdrome symptoms are a frequent feature of migraine attacks in patients who report nonheadache symptoms, with more than 80% of attacks being followed by such symptoms. While not everyone with migraine suffers from postdrome, those who do report it can be as debilitating as the migraine pain itself. Interestingly, the treatment type including medication taken to relieve the migraine headache and attack headache severity did not seem to influence the duration of the migraine postdrome (see Table 3 below) 5.
In one study, 47 of 50 patients remained symptomatic after their headache had ended 3. In that study, the most frequent symptoms were changes in mood (72%), muscular weakness (54%), and reduced appetite. In another study, 78 out of 100 unselected migraineurs reported resolution symptoms in a given attack 6; most common were asthenia (55%), tiredness (46%), somnolence (29%), and concentration difficulties (28%). A large clinic-based sample found that 562 of 827 patients retrospectively reported postdromes; in 88%, they lasted less than 24 hours. Tiredness was the most common symptom in 72% 4. In a US study designed to test a postdrome instrument, patients (n = 32) again reported tiredness, nausea, and concentration difficulties most commonly 2.
Migraine postdrome while disabling for many patients 6, has not been prospectively documented 5 and is not defined in the International Classification of Headache Disorders 7.
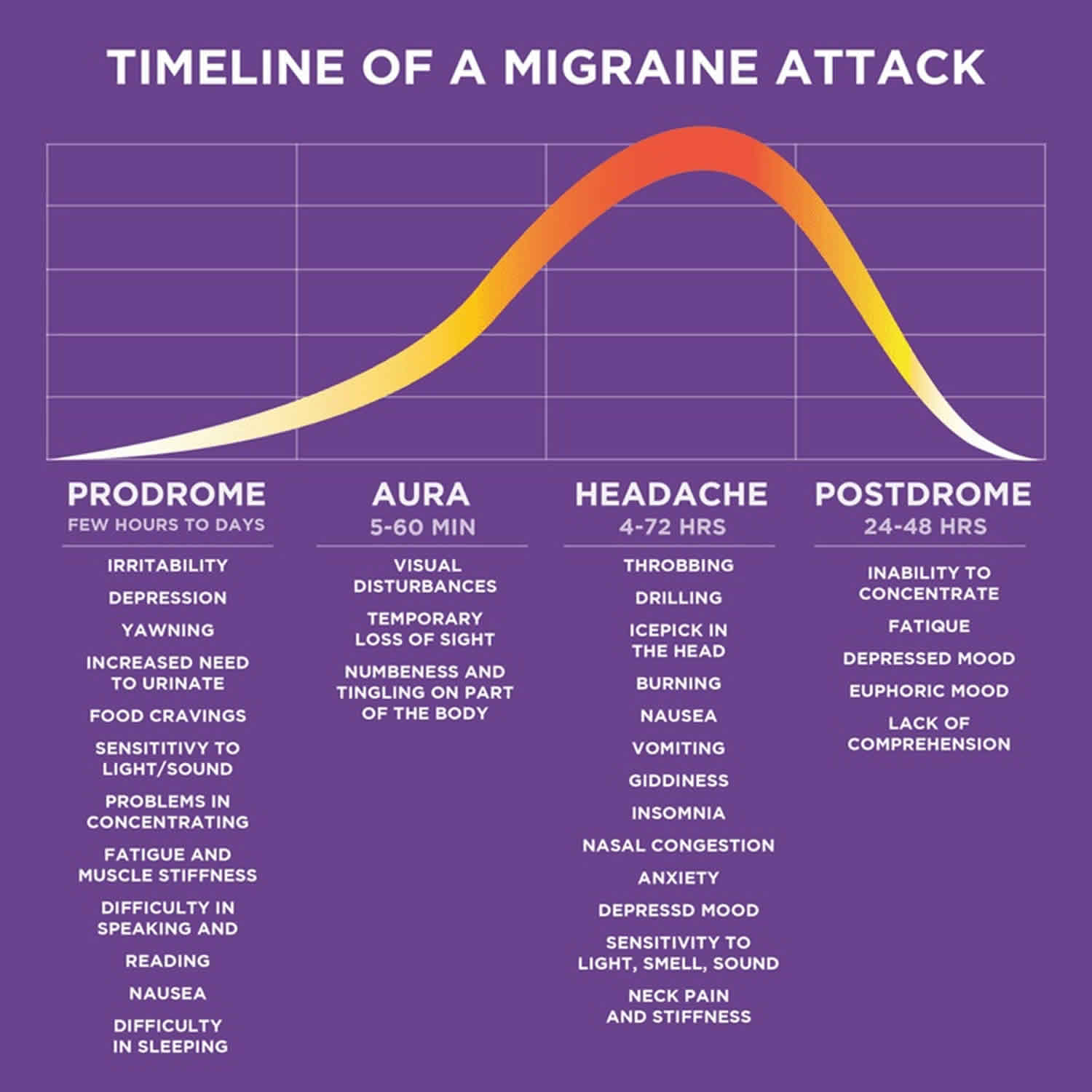
The migraine attack is typically divided into 4 nonobligatory phases: the prodrome phase, the aura, the headache phase, and the postdrome. Nonheadache symptoms may start before the headache phase begins or during the prodrome period 8, the headache phase or the postdrome. These symptoms involve brain activation of cortical and subcortical structures 9.
Migraine postdrome causes
Just as it can be difficult to determine what triggers migraine attacks in individual people, there’s no singular known cause behind migraine postdrome. Postdrome is actually part of the migraine attack itself. The profound changes in activity and blood flow that occur during the aura and head pain phase of the attack, persists even after the pain has ended. Not every migraine will be followed by a postdrome phase, and the severity of the migraine doesn’t always correspond to the intensity of the postdrome that follows.
Migraine pathophysiology involves dysfunction of diencephalic and brainstem centers thought to be involved in pain processing and other sensory modalities modulation 10. Pontine and midbrain structures have altered function during migraine attacks and after remissions that occur with triptans. Although triptans effectively treat migraine headache, they do not alter the fundamental brainstem mechanisms responsible for migraine generation 10. This may explain why although head pain is ameliorated by triptans, nonheadache symptoms persist.
Migraine postdrome prevention
Migraine postdrome or migraine hangovers can be reduced, or better managed, by maintaining good headache hygiene. When consistently practiced, these preventative measures can reduce the severity and length of a migraine postdrome. Drinking plenty of water and resting can be beneficial as your body recovers after a migraine. Some people report fewer postdrome experiences when they follow their migraine attacks with calming activities like yoga, or when they avoid electronic devices. If you have postdrome and want to experiment with ways to avoid or lessen your postdrome symptoms, remember: different “fixes” will work for different people, and it’s OK if they don’t work for you. A soda might help your friend recover during postdrome, but it’s not guaranteed to speed up your healing process. Healthy and careful experimentation can help you find things that help with your postdrome.
Caffeine during the prodrome phase can have a positive effect for some people, but others find it makes their symptoms worse. Many find comfort food, ice packs, heating pads, massages and additional rest helps to soothe their migraine hangover. Ignoring or pushing through the effects of the postdrome phase doesn’t give the body necessary time to recover, and can increase the risk of having another attack. Take it easy and rest during this time.
Lifestyle changes
Migraine is not a predictable disorder for all people. Simple things like changes to a normal routine can lead to a severely disabling migraine attack. Understanding how lifestyle affects the severity and frequency of attacks can be a large part of successful migraine prevention.
It is unrealistic to expect anyone to completely change a certain lifestyle. However, certain things are relatively easy to do. For example:
- Maintain regular sleep patterns. Go to sleep and wake up at the same time each day.
- Exercise regularly. For example, aerobic exercise for at least 30 minutes three times a week will help reduce frequency or severity of migraine.
- Eat regular meals, do not skip meals, and eat a good, healthy breakfast.
- Reduce stress. Limit stress by avoiding conflicts and resolving disputes calmly. Some people find it helpful to take a daily “stress break.”
- Avoiding known triggers (see Table 1 on common triggers).
Establishing daily routines that help reduce migraine attacks is important for long-term migraine prevention. For example:
- Schedule a relaxation period that includes relaxation strategies such as:
- Take slow, deep breaths.
- Focus the mind on a relaxing image or scene.
- Try soft relaxing lighting and sounds.
- Exercise on a regular basis, even if your daily routine changes (such as when traveling, when you have house guests, or when your workload increases).
- Maintain the medication treatment plan designed by you and your physician. Early intervention may help prevent the migraine from progressing into a severe, disabling attack.
Trigger avoidance
Triggers are specific factors that may increase your risk of having a migraine attack. The migraine sufferer has a sensitive nervous system that, under certain circumstances, can lead to migraine. Triggers do not “cause” migraine. Instead, they are thought to activate processes that cause migraine in people who are prone to the condition. A certain trigger will not induce a migraine in every person. In a single migraine sufferer, a trigger may not cause a migraine every time. By keeping a headache diary, you will be able to identify some triggers for your particular headaches. Once you have identified triggers, it will be easier for you to avoid them and reduce your chances of having a migraine attack.
Table 1. Migraine common triggers
| Common Triggers | ||
| Categories | Triggers | Examples |
| Dietary | Skipping meals/fasting Food Items | Aged cheese Alcohol/red wineChemicals [eg. MSG (monosodium glutamate)] Caffeine withdrawalProcessed meats (containing nitrates) |
| Medications | Nitroglycerine | |
| Chronobiology | Change in sleep patterns | Napping Oversleeping Too little sleep |
| Environmental | Weather changes | Extreme heat or cold |
| Bright lights | Sun without eye shades | |
| Odors/pollution | Smog, perfumes, chemicals Flashing lights or screens | |
| Hormonal | Estrogen level changes (rapid fluctuations in estrogen levels) | Menstruation Hormone replacement therapies Birth control pills Menopause |
| Stress | Work | Unrealistic timeliness |
| Home | Financial issues | |
| Family | Job changes / moving Childbirth / marriage Death/loss | |
| Stress Letdown | Discontinuation of work | Weekends / vacations Ending a project or stressful task (such as a presentation) |
| Physical | Injuries | Head trauma |
| Over-exertion | Exercising when out of shape or in heat | |
Migraine postdrome symptoms
Patients defined the onset of postdrome as when they no longer experienced the migraine pain. Postdrome was often described as “[being] or [feeling] wiped out” and “headache hangover” 11. For those having a severe migraine episode, the shift from headache to postdrome can be difficult to identify. The pain can manifest itself into areas of the body not previously affected: stiffness in the neck and shoulders, tenderness in the scalp and dizziness are common “migraine hangover” symptoms.
Everyone experiences the postdrome phase differently: it does not necessarily occur in everyone with migraine, nor does it happen after every attack. These inconsistencies can be confusing, and often cause “migraine hangover” to be mistaken for a different medical condition.
The symptoms most frequently reported by the patients who participated in the focus groups were: tiredness, difficulty concentrating, weakness, dizziness, lightheadedness, and decreased energy 11. Patients also reported decreased activity level as a result of experiencing postdrome symptoms. Postdrome symptoms were reported to impact the ability to work, to affect family interactions and social life, and to cause cognitive impairment 11.
Giffin et al. 5 divided postdromal symptoms into 3 broad groups:
- Cognitive/mood/energy,
- Autonomic, and
- Gastrointestinal symptoms, as well as sensory sensitivity.
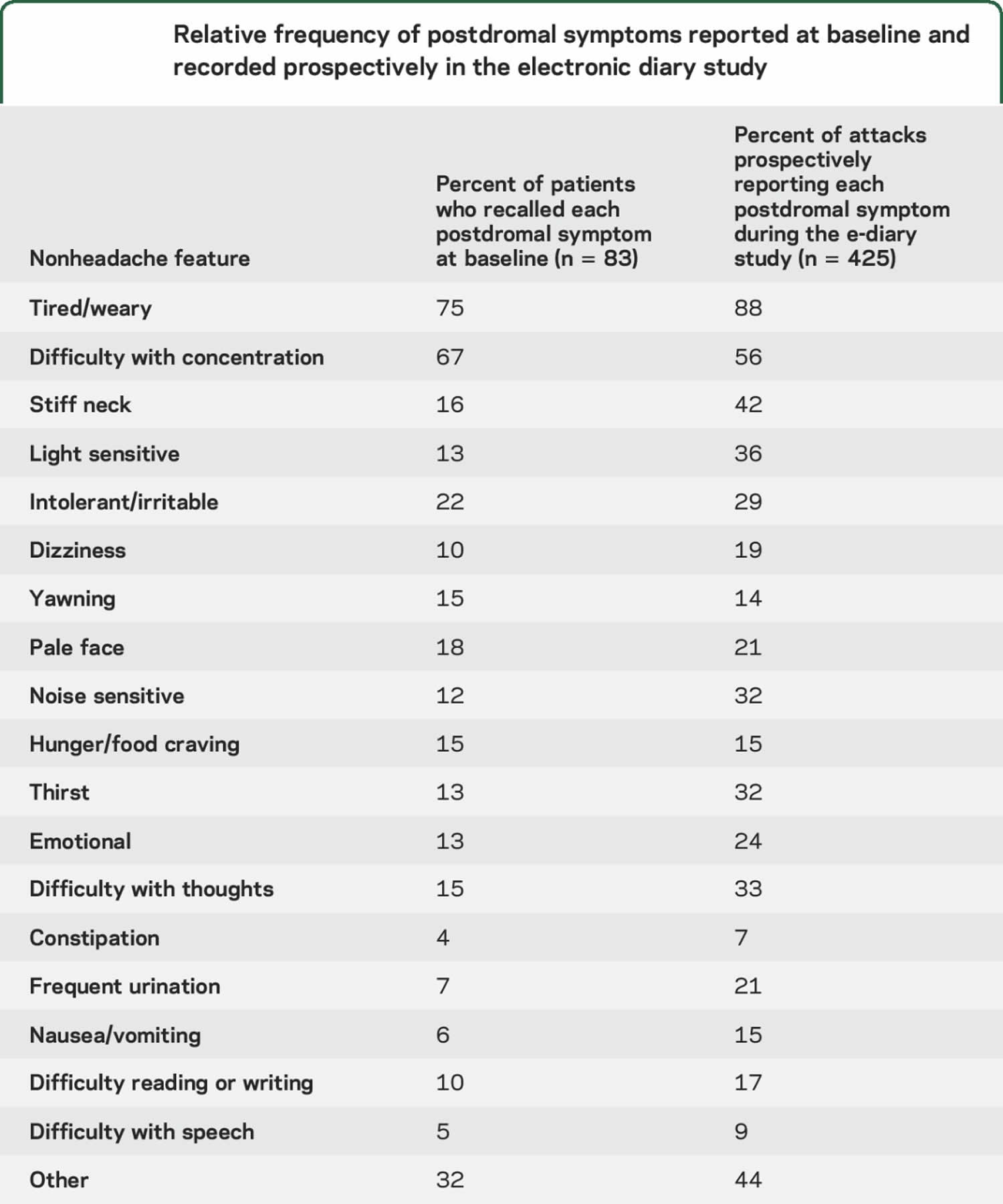
Being tired or weariness was the most common symptom, reported in 88% of postdromes in Giffin et al. study 5. Other frequently reported symptoms included difficulty with concentration (56%) and stiff neck (42%). Typical migraine attack symptoms of nausea, photophobia, and phonophobia were also common (Table 1). Mean quality of life score, as measured on a visual analogue rating score, was 57/100, compared to 51 in the premonitory phase, 33 during the headache phase, and 81 between attacks.
Table 2. Relative frequency of postdromal symptoms reported at baseline and recorded prospectively in the electronic diary study
[Source 5 ]Time to recovery in the migraine postdrome
There was a return to normal within 6 hours of the end of the headache in 422 of 773 (54%) migraine attacks with a postdrome; only 7% lasted more than 24 hours (Table 2). Headache severity did not predict length of the postdrome 5.
Table 3. Return to normal in each time interval from end of migraine headache to the end of the postdrome by medication taken to relieve migraine headache or headache severity
Migraine postdrome treatment
Avoiding factors that you know trigger migraines may help reduce your likelihood of migraine postdrome or at least reduce the duration and severity as well as the potential for triggering another full-blown attack. For many people, stress can trigger or exacerbate their migraine, so take time after a migraine attack to focus on your mental health and take care of yourself. Regular exercise, a consistent sleeping pattern and a healthy diet can help reduce stress, as can relaxation techniques like meditation. Eat healthy, nutritious meals frequently and try to get more sleep. If light is a migraine trigger for you, don’t be afraid to keep things dark for a few days as you go through the postdrome phase.
If you’re experiencing migraine postdrome, take this time to focus on yourself and your well-being to help your body recover from each migraine attack and its after effects.
Maintaining a headache diary will help you track your symptoms and their changes during the prodrome, aura, headache and postdrome phases, which can help you identify patterns, like behaviors or foods correspond with your attacks, helping you reduce your exposure to triggers. Working with a headache specialist will help you better understand your unique migraine experience, identify patterns that help you manage your migraine and postdrome and find medications that may relieve some symptoms and obtain a better understanding of your unique headache disorder and how best to treat it.
- Migraine Hangover. https://americanmigrainefoundation.org/resource-library/migraine-hangover/[↩]
- Ng-Mak DS, Fitzgerald KA, Norquist JM, et al. Key concepts of migraine postdrome: a qualitative study to develop a post-migraine questionnaire. Headache 2011;51:105–117.[↩][↩]
- Blau JN. Resolution of migraine attacks: sleep and the recovery phase. J Neurol Neurosurg Psychiatry 1982;45:223–226.[↩][↩]
- Kelman L. The postdrome of the acute migraine attack. Cephalalgia 2006;26:214–220.[↩][↩]
- Giffin NJ, Lipton RB, Silberstein SD, Olesen J, Goadsby PJ. The migraine postdrome: An electronic diary study. Neurology. 2016;87(3):309–313. doi:10.1212/WNL.0000000000002789 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4955275[↩][↩][↩][↩][↩][↩][↩]
- Quintela E, Castillo J, Munoz P, Pascual J. Premonitory and resolution symptoms in migraine: a prospective study in 100 unselected patients. Cephalalgia 2006;26:1051–1060.[↩][↩]
- Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808.[↩]
- Giffin NJ, Ruggiero L, Lipton RB, et al. Premonitory symptoms in migraine: an electronic diary study. Neurology 2003;60:935–940.[↩]
- Maniyar FH, Sprenger T, Monteith T, Schankin C, Goadsby PJ. Brain activations in the premonitory phase of nitroglycerin triggered migraine attacks. Brain 2014;137:232–242.[↩]
- Akerman S, Holland P, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci 2011;12:570–584.[↩][↩]
- Key concepts of migraine postdrome: a qualitative study to develop a post-migraine questionnaire. Headache. 2011 Jan;51(1):105-17. doi: 10.1111/j.1526-4610.2010.01817.x. https://doi.org/10.1111/j.1526-4610.2010.01817.x[↩][↩][↩]