Mitral stenosis
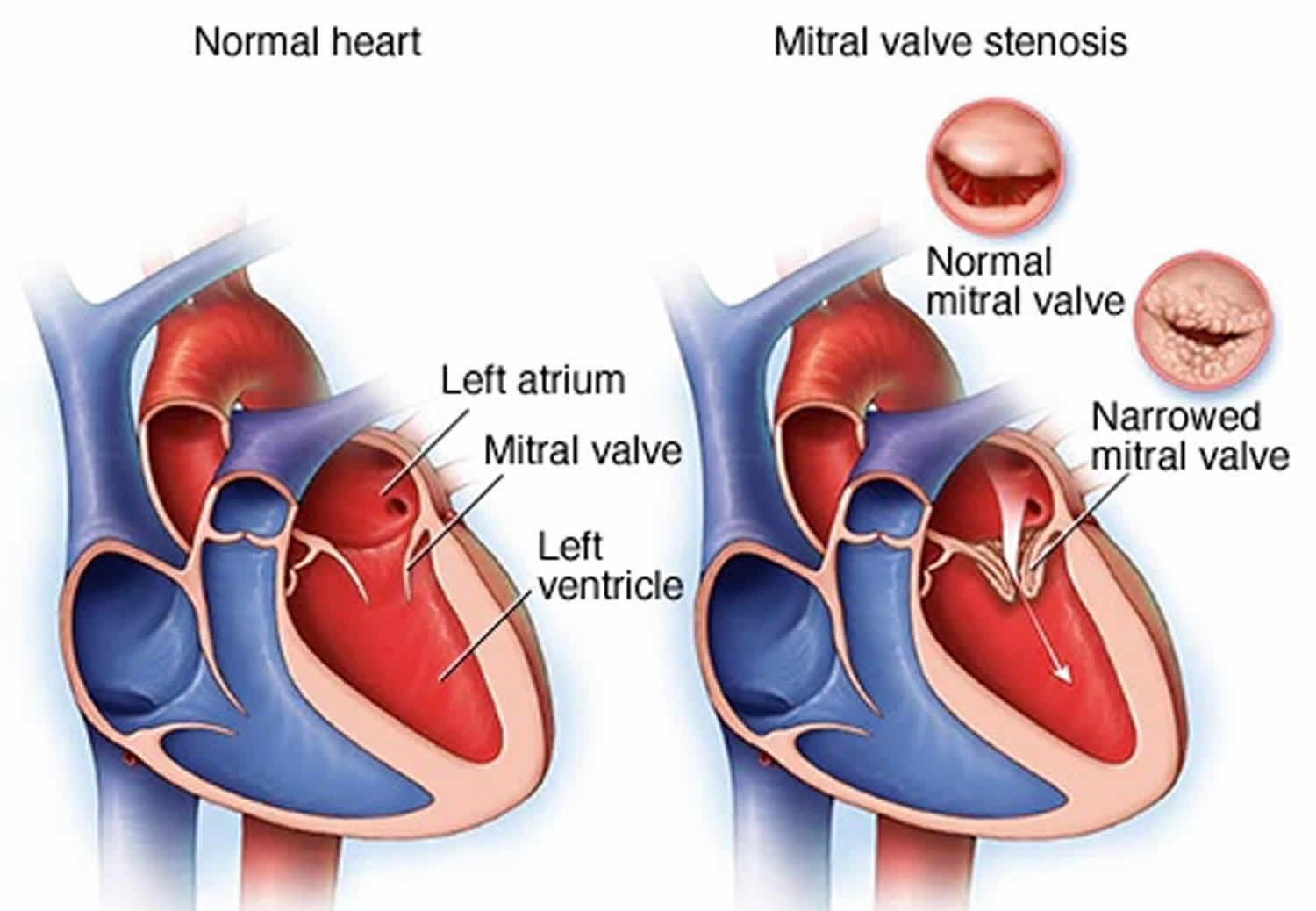
Mitral stenosis also called mitral valve stenosis is a narrowing or blockage of the mitral valve where the mitral valve does not open as wide as it should, restricting the flow of blood through the heart 1, 2. The narrowed mitral valve causes blood to backup in your heart’s upper-left chamber (the left atrium) instead of flowing into the lower-left chamber (the left ventricle). Most adults with mitral stenosis had rheumatic fever when they were younger 3, 4, 5. A rheumatic fever is a childhood illness that sometimes occurs after untreated strep throat or scarlet fever. Rheumatic fever is very rare in the United States due to the use of effective antibiotics to prevent infections. In the United States, mitral stenosis secondary to rheumatic heart disease most commonly presents in the immigrant population and those with limited access to healthcare facilities 6. Rheumatic mitral stenosis usually presents in patients between 20 and 40 years of age and about 10 to 15 years after the onset of rheumatic fever. When rheumatic fever damages the mitral valve, the condition is called rheumatic mitral valve disease. Mitral valve stenosis may also be associated with aging and a buildup of calcium on the ring around the mitral valve where the leaflet and heart muscle meet, this condition is also called calcific degenerative mitral valve stenosis disease or mitral annular calcification (MAC), but this condition is far less common and more often seen in the elderly 7. Risk factors for rheumatic mitral stenosis include a history of rheumatic fever and a previously untreated streptococcus infection 8. Some data suggest that patients with chronic kidney diseases and dialysis are at increased risk for calcific, degenerative mitral stenosis 9.
Mitral valve stenosis symptoms may appear or worsen anytime your heart rate increases, such as during exercise. An episode of rapid heartbeats may accompany these symptoms. Or they may be triggered by pregnancy or other body stress, such as an infection.
The mitral valve opens when blood flows from the left atrium to the left ventricle. Then the flaps close to prevent the blood that has just passed into the left ventricle from flowing backward. A defective mitral valve fails to either open or close fully. In mitral valve stenosis, pressure that builds up in the heart is then sent back to the lungs, resulting in fluid buildup (congestion) and shortness of breath.
Symptoms of mitral valve stenosis most often appear in between the ages of 15 and 40 in developed nations, but they can occur at any age even during childhood.
The mitral valve is a 2 leaflets or cusps (bileaflet valve or bicuspid valve) positioned between the left atrium and left ventricle (other heart valves i.e., tricuspid, pulmonary and aortic valves have three leaflets or cusps) (see Figure 1 to 5). The normal mitral orifice area is 4 to 6 square centimeters (4 to 6 cm²) 2. Under normal physiologic conditions, the mitral valve opens during left ventricular diastole to allow blood to flow from the left atrium to the left ventricle. The pressure in the left atrium and the left ventricle during diastole are equal. The left ventricle gets filled with blood during early ventricular diastole. There is only a small amount of blood that remains in the left atrium. With the contraction of the left atrium (the “atrial kick”) during late ventricular diastole, this small amount of blood fills the left ventricle 10, 11, 12 .
Mitral valve areas less than 2 square centimeters (<2 cm²) causes an impediment to the blood flow from the left atrium into the left ventricle. This creates a pressure gradient across the mitral valve. As the gradient across the mitral valve increases, the left ventricle requires the atrial kick to fill with blood.
Mitral valve area less than 1 square centimeter (<1 cm²) causes an increase in left atrial pressure. The normal left ventricular diastolic pressure is 5 mmHg. A pressure gradient across the mitral valve of 20 mmHg due to severe mitral stenosis will cause a left atrial pressure of about 25 mmHg. This left atrial pressure is transmitted to the pulmonary vasculature resulting in pulmonary hypertension.
As left atrial pressure remains elevated, the left atrium will increase in size. As the left atrium increases in size, there is a greater chance of developing atrial fibrillation. If atrial fibrillation develops, the atrial kick is lost.
Thus, in severe mitral stenosis, the left ventricular filling is dependent on the atrial kick. With the loss of the atrial kick, there is a decrease in cardiac output and sudden development of congestive heart failure.
New York Heart Association (NYHA) classification system groups heart failure into four categories by number. You may see Roman numerals used for these category names.
- Class 1 (I) heart failure. There are no heart failure symptoms.
- Class 2 (II) heart failure. Everyday activities can be done without difficulty. But exertion causes shortness of breath or fatigue.
- Class 3 (III) heart failure. It’s difficult to complete everyday activities.
- Class 4 (IV) heart failure. Shortness of breath occurs even at rest. This category includes the most severe heart failure.
Mitral stenosis progresses slowly from initial signs of mitral stenosis to New York Heart Association (NYHA) functional class 2 symptoms to atrial fibrillation to NYHA functional class 3 or 4 symptoms 13.
If mitral valve stenosis is not treated, it can lead to:
- Atrial fibrillation – an irregular and fast heartbeat.
- Pulmonary hypertension – high blood pressure in the blood vessels that supply the lungs.
- Heart failure – where the heart cannot pump blood around the body properly.
- Thromboembolism – a circulating blood clot that breaks off from its original site and travels through the bloodstream to obstruct a blood vessel, causing tissue ischemia and organ damage.
You might not need treatment if you do not have any symptoms. Your heart doctor (cardiologist) may just suggest having regular check-ups to monitor your condition. If you have very severe mitral stenosis, you should get an echocardiogram every year. Those with less severe mitral stenosis need an echocardiogram about every 3 to 5 years. Ask your heart doctor (cardiologist) how often you need one.
If you have symptoms or the problem with your mitral valve stenosis is severe, your doctor may recommend:
- medicine to relieve your symptoms – such as medicines called diuretics to reduce breathlessness and medicines for atrial fibrillation
- mitral valve surgery – to replace the valve or stretch it with a small balloon (balloon valvuloplasty)
Treatment depends on how severe is your mitral valve stenosis and whether it’s getting worse. Untreated, mitral valve stenosis can lead to serious heart complications.
Call your doctor for an immediate appointment if you develop fatigue or shortness of breath during physical activity, heart palpitations, or chest pain.
If you have been diagnosed with mitral valve stenosis but haven’t had symptoms, talk to your doctor about follow-up evaluations.
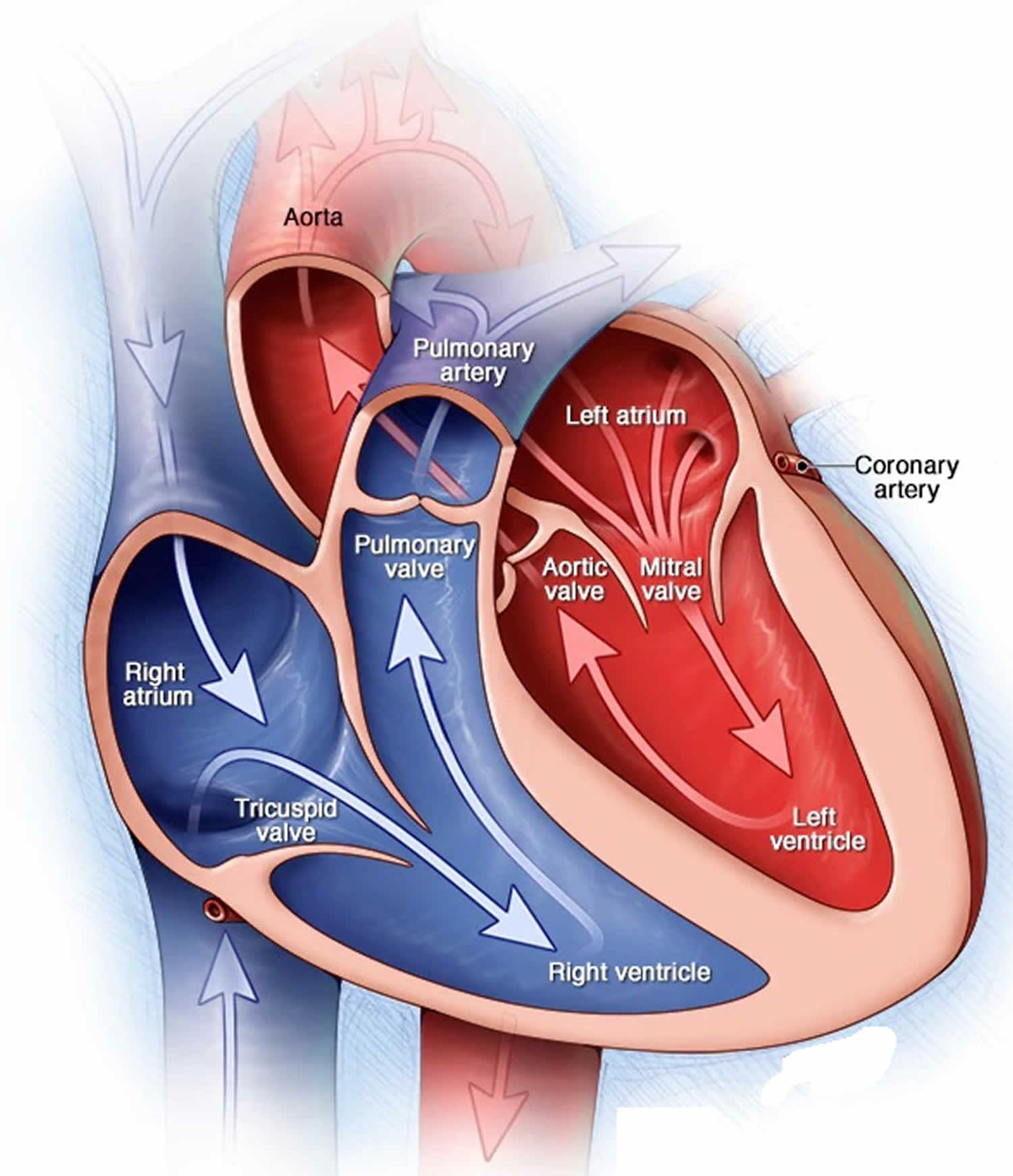
How your heart works
Your heart is a muscular organ that pumps blood to your body. Your heart, the center of your circulatory system, consists of four chambers. The two upper chambers (atria) receive blood. The two lower chambers (ventricles) pump blood. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of your heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings. Four heart valves open and close to let blood flow in only one direction through your heart. The mitral valve — which lies between the two chambers on the left side of your heart — comprises two flaps of tissue called leaflets.
The circulatory system consists of a network of blood vessels, such as arteries, veins, and capillaries. These blood vessels carry blood to and from all areas of your body.
An electrical system controls your heart and uses electrical signals to contract the heart’s walls. When the heart walls contract, blood is pumped into your circulatory system. Inlet and outlet valves in your heart chambers ensure that blood flows in the right direction.
Your heart is vital to your health and nearly everything that goes on in your body. Without your heart’s pumping action, blood can’t move throughout your body.
Your blood carries the oxygen and nutrients that your organs need to work well. Blood also carries carbon dioxide (a waste product) to your lungs so you can breathe it out.
A healthy heart supplies your body with the right amount of blood and oxygen at the rate needed to work well. If disease or injury weakens your heart, your body’s organs won’t receive enough blood to work normally.
Your heart has 2 sides, separated by an inner wall called the septum. The right side of the heart pumps blood to your lungs to pick up oxygen. The left side of your heart receives the oxygen-rich blood from the lungs and pumps it to the body.
Figure 1. Human heart anatomy
Figure 2. The anatomy of the heart chambers
Figure 3. Normal heart blood flow
Figure 4. Heart valves including mitral valve
Footnote: The mitral valve has 2 flaps; the other heart valves have three.
Figure 5. Human heart valves and function
 Footnotes: Heart valves are like doors that open and close. Heart valves open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, heart valves permit blood to flow in only one direction.
Footnotes: Heart valves are like doors that open and close. Heart valves open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, heart valves permit blood to flow in only one direction.Figure 6. Mitral valve stenosis
Heart Chambers
Your heart has 4 chambers 14, 2 on the right and 2 on the left:
- 2 upper chambers are called atrium (two is called an atria). The atria collect blood as it flows into your heart.
- 2 lower chambers are called ventricles.
- Right ventricle (RV) pumps Deoxygenated blood out of your heart to your lungs. Deoxygenated blood, also known as venous blood, is blood that has a lower oxygen concentration and a higher concentration of carbon dioxide than oxygenated blood.
- Left ventricle (LV) pumps Oxygenated blood out of your heart to other parts of your body. Oxygenated blood, also known as arterial blood, is blood rich in oxygen, typically bright red, that is pumped from the left ventricle of your heart to your body through arteries (aorta) after picking up oxygen in your lungs.
Your heart also has 4 valves that open and close to let blood flow from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart in only one direction when the heart contracts (beats). The four heart valves are:
- Tricuspid valve, located between the right atrium and right ventricle
- Pulmonary or pulmonic valve, between the right ventricle and the pulmonary artery. The pulmonary artery carries blood from your heart to your lungs.
- Mitral valve, between the left atrium and left ventricle
- Aortic valve, between the left ventricle and the aorta. This aorta carries blood from the heart to the body.
Each valve has a set of flaps also called leaflets or cusps. The mitral valve has two flaps; the others have three. Valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward. Blood flow occurs only when there’s a difference in pressure across the valves, which causes them to open. Under normal conditions, the valves permit blood to flow in only one direction.
Your heart 4 chambers and 4 valves and is connected to various blood vessels. Veins are blood vessels that carry blood from the body to your heart. Arteries are blood vessels that carry blood away from your heart to your body.
Your heart pumps blood to your lungs and to all the body’s tissues by a sequence of highly organized contractions of the four chambers. For your heart to function properly, the four chambers must beat in an organized way.
When your heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope 15.
- The First heart sound (S1) — the “lub” —is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The Second heart sound (S2) — the “DUB” —is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
Blood Flow
The Right Side of Your Heart
In figure 5 above, the superior vena cava (SVC) and inferior vena cava (IVC) are shown in blue to the left of the heart muscle as you look at the picture. The superior vena cava (SVC) and inferior vena cava (IVC) are the largest veins in your body.
After your body’s organs and tissues have used the oxygen in your blood, the vena cavae carry the oxygen-poor blood (deoxygenated blood or venous blood) back to the right atrium of your heart.
- The superior vena cava (SVC) carries oxygen-poor blood from the upper parts of your body, including your head, chest, arms, and neck.
- The inferior vena cava (IVC) carries oxygen-poor blood from the lower parts of your body from the abdomen and lower extremities back to the right side of your heart for oxygenation.
The oxygen-poor blood (deoxygenated blood or venous blood) from the vena cavae flows into your heart’s right atrium. From the right atrium, blood is pumped into the right ventricle. And then from the right ventricle, blood is pumped to your lungs through the pulmonary arteries (shown in blue in the center of figure 5).
Once in the lungs, the blood travels through many small, thin blood vessels called capillaries. There, the blood picks up more oxygen and transfers carbon dioxide to the lungs—a process called gas exchange.
The oxygen-rich blood passes from your lungs back to your heart through the pulmonary veins (shown in red to the left of the right atrium in figure 5).
The Left Side of Your Heart
Oxygen-rich blood from your lungs passes through the pulmonary veins (shown in red to the right of the left atrium in figure 5 above). The blood enters the left atrium and is pumped into the left ventricle.
From the left ventricle, the oxygen-rich blood is pumped to the rest of your body through the aorta. The aorta is the main artery that carries oxygen-rich blood to your body.
Like all of your organs, your heart needs oxygen-rich blood. As blood is pumped out of your heart’s left ventricle, some of it flows into the coronary arteries (shown in red in figure 5).
Your coronary arteries are located on your heart’s surface at the beginning of the aorta. They carry oxygen-rich blood to all parts of your heart.
For the heart to work well, your blood must flow in only one direction. Your heart’s valves make this possible. Both of your heart’s ventricles have an “in” (inlet) valve from the atria and an “out” (outlet) valve leading to your arteries.
Healthy valves open and close in exact coordination with the pumping action of your heart’s atria and ventricles. Each valve has a set of flaps called leaflets or cusps that seal or open the valve. This allows blood to pass through the chambers and into your arteries without backing up or flowing backward.
What is ejection fraction?
Ejection fraction (EF) is a measurement of your heart’s ability to pump oxygen-rich blood out to your body, expressed as a percentage (%), of how much oxygen-rich blood the left ventricle (LV) pumps out with each heart contraction 16. Ejection fraction (EF) refers to how well your heart pumps blood. Ejection fraction (EF) is the amount of blood pumped out of your heart’s lower chambers (ventricles) each time it contracts. An ejection fraction (EF) of 60 percent means that 60 percent of the total amount of blood in the left ventricle (LV) is pushed out with each heartbeat. A normal heart’s ejection fraction (normal EF) is between 50 and 70 percent 16. With each heartbeat, 50% to 70% of the blood in your left ventricle gets pumped out to your body. However, it is important to note that you can have a normal ejection fraction measurement and still have heart failure. This is called heart failure with preserved ejection fraction (HFpEF) previously known as diastolic heart failure. Heart failure with preserved ejection fraction (HFpEF) happens when your heart’s muscle has become so thick and stiff that the ventricle holds a smaller than usual volume of blood. In this case, your heart might still have an ejection fraction that falls in the normal range (EF≥50%) because your heart is pumping out a normal percentage of the blood that enters it. But in heart failure with preserved ejection fraction (HFpEF), the total amount of blood pumped isn’t enough to meet your body’s needs.
To understand ejection fraction (EF), it’s helpful to understand how blood flows through your heart:
- Blood enters your heart through the top right section (right atrium).
- Between heartbeats, there’s a short pause (diastole, the phase of the heartbeat when your heart muscle relaxes and allows heart chambers to fill with blood). This is when blood flows through a valve down to the left ventricle.
- Once the ventricle is full, the next heartbeat pumps out (ejects) a portion of the blood out to the body. Also called systole, the phase of the heartbeat when your heart muscle contracts and pumps blood from the heart chambers into the arteries.
Table 1. Ejection Fraction Percentage
| Sex | Normal | Mildly Abnormal | Moderately Abnormal | Severely Abnormal |
|---|---|---|---|---|
| Male | 52% to 72% | 41% to 51% | 30% to 40% | Below 30% |
| Female | 54% to 74% | 41% to 53% | 30% to 40% | Below 30% |
Types of ejection fraction
There are 2 types of ejection fraction: left ventricular ejection fraction (LVEF) and right ventricular ejection fraction (RVEF). Left ventricular ejection fraction (LVEF) measures how much blood gets pumped from the left ventricle with each contraction. Typically, ejection fraction refers to left ventricular. Right ventricular ejection fraction (RVEF) measures how much blood is pumped out of the right side of the heart, to the lungs.
Left ventricular ejection fraction (LVEF)
Ejection fraction (EF) typically refers to the left side of your heart or left ventricular ejection fraction (LVEF). It shows how much oxygen-rich blood is pumped out of the left ventricle (LV) to most of your body’s organs with each contraction. Left ventricular ejection fraction (LVEF) helps determine the severity of dysfunction on the left side of your heart.
Right ventricular ejection fraction (RVEF)
Right ventricular ejection fraction (RVEF) measures the amount of oxygen-poor blood or deoxygenated blood or venous blood pumped out of the right side of your heart to your lungs for oxygen. Right ventricular ejection fraction (RVEF) is important if you have right-sided heart failure. But this condition is not as common as left-sided heart failure.
What’s an unhealthy ejection fraction?
Ejection fraction (EF) refers to how well your heart pumps blood. The ejection fraction is the percentage of blood pumped out of the ventricle after a heart contraction. Ejection fraction (EF) is the amount of blood pumped out of your heart’s lower chambers (ventricles) each time it contracts. Your ejection fraction is an indicator of how well your heart is working. A low ejection fraction typically means you have or are at risk for heart failure. An ejection fraction (EF) from 41 to 49 percent (EF from 41% to 49%) might be considered too low. The lower your heart’s ejection fraction, the weaker your heart’s pumping action is. This occurs in people with severe heart failure. You can also have a low ejection fraction in the earlier stages of heart failure. However, ejection fraction (EF) does not always indicate that a person is developing heart failure, but it could indicate damage, perhaps from a previous heart attack. Some people with a normal ejection fraction also have heart failure. This is known as heart failure with preserved ejection fraction (HFpEF). An ejection fraction measurement under 40 percent (EF<40%) might be evidence of heart failure or cardiomyopathy (disease of the heart muscle that makes it harder for the heart to pump blood). In severe cases, ejection fraction (EF) can be even lower than 40.
According to the American Heart Association:
- Ejection fraction 50 to 70% (EF = 50% to 70%): Normal heart function.
- Ejection fraction 41 to 49% (EF = 41% to 49%): A mildly reduced left ventricle (LV) ejection fraction. Can indicate previous heart damage from heart attack or cardiomyopathy. You might not experience heart failure symptoms. Or, you may have symptoms with physical activity but not at rest.
- Ejection fraction less than 40% (EF < 40%): Your heart pumping ability is below normal. The lower the ejection fraction, the higher the risk of life-threatening complications, like cardiac arrest. Symptoms may be severe and may affect you even when sitting still.
- Ejection fraction greater than 75% (EF > 75%): Can indicate a heart condition like hypertrophic cardiomyopathy (HCM), a genetic heart condition where the heart muscle thickens, making it harder for the heart to pump blood effectively. This thickening can lead to various symptoms and complications, including shortness of breath, chest pain, and an increased risk of arrhythmias and a common cause of sudden cardiac arrest.
The lower your ejection fraction, the more severe your heart failure symptoms may be. You might experience:
- Confusion.
- Fatigue.
- Heart palpitations.
- Nausea.
- Shortness of breath (dyspnea).
- Water retention in your abdomen or feet.
- Weakness.
Some things that may cause a reduced ejection fraction are:
- Weakness of the heart muscle, such as cardiomyopathy.
- Heart attack that damaged the heart muscle.
- Heart valve disease.
- Long-term, uncontrolled high blood pressure.
What is the formula for ejection fraction?
The ejection fraction (EF) formula equals the amount of blood pumped out of the ventricle with each contraction (stroke volume or SV) divided by the end-diastolic volume (EDV), the total amount of blood in the ventricle. To express as a percentage, you would multiply by 100.
- Ejection fraction (EF) = (stroke volume [SV]/end-diastolic volume [EDV]) x 100
Stroke volume (SV) is the volume of blood pumped out of the heart’s left ventricle during each systolic cardiac contraction. Ventricular stroke volume (SV) is often thought of as the amount of blood (mL) ejected per beat by the left ventricle into the aorta (or from the right ventricle into the pulmonary artery). Moreover, a more precise definition for stroke volume (SV) and one that is used in echocardiography when assessing ventricular function is the difference between the ventricular end-diastolic volume (EDV) and the end-systolic volume (ESV). The end-diastolic volume (EDV) is the filled volume of the ventricle before contraction, and the end-systolic volume (ESV) is the residual volume of blood remaining in the ventricle after ejection. In a typical heart, the end-diastolic volume (EDV) is about 120 mL of blood and the end-systolic volume (ESV) is about 50 mL of blood 18. The difference in the end-diastolic volume (EDV) and the end-systolic volume (ESV), 70 mL, that is Stroke volume (SV) = end-diastolic volume (EDV) – end-systolic volume (ESV). Therefore, any factor that alters either the EDV or the ESV will change the SV. For example, an increase in EDV increases SV, whereas an increase in ESV decreases SV.
Mitral stenosis classification
Classification of severity of mitral valve stenosis
Mild
- Mean gradient (mmHg) less than 5
- Pulmonary artery systolic pressure (mmHg) less than 30
- Valve area (cm²) less than 1.5
Moderate
- Mean gradient (mmHg) 5 to 10
- Pulmonary artery systolic pressure (mmHg) 30 to 50
- Valve area (cm²) 1.0 to 1.5
Severe
- Mean gradient (mmHg) less than 10
- Pulmonary artery systolic pressure (mmHg) greater than 50
- Valve area (cm²) less than 1.0
Mitral valve anatomy according to the Wilkins Score
Grade 1
- Mobility: Highly mobile valve with only leaflet tips restricted
- Thickening: Leaflet near normal in thickness (4 mm to 5 mm)
- Calcification: A single area of increased echo brightness
- Subvalvular Thickening: Minimal thickening just below the mitral leaflets
Grade 2
- Mobility: Leaflet mid to base portions have normal mobility
- Thickening: Mid leaflets normal, considerable thickening of margins (5-8 mm)
- Calcification: Scattered areas of brightness confirmed to leaflet margins
- Subvalvular Thickening: Thickening of chordal structures extending to one of the chordal length
Grade 3
- Mobility: Valve continues to move forward in diastole, mainly from the base
- Thickening: Thickening extending through the entire leaflet (5 mm to 8 mm)
- Calcification: Brightness extending into the mid portions of the leaflets
- Subvalvular Thickening: Thickening extended to distal third to the chords
Grade 4
- Mobility: No or minimal forward movement of the leaflets in diastole
- Thickening: Considerable thickening of all leaflet tissue (more than 8 mm to 10 mm)
- Calcification: Extensive brightness throughout much of the leaflet tissue
- Subvalvular Thickening: Extensive thickening and shortening of all chordal structures extending down to the papillary muscles.
Mitral stenosis causes
Causes of mitral valve stenosis include:
- Rheumatic fever. A complication of strep throat, rheumatic fever can damage the mitral valve. Rheumatic fever is the most common cause of mitral valve stenosis. When rheumatic fever damages the mitral valve, the condition is called rheumatic mitral valve disease. It can damage the mitral valve by causing the flaps to thicken or fuse. Signs and symptoms of mitral valve stenosis might not show up for years.
- Calcium deposits. As you age, calcium deposits can build up around the ring around the mitral valve (annulus), which can occasionally cause mitral valve stenosis. The condition is called mitral annular calcification (MAC) or calcific degenerative mitral valve stenosis disease. Severe mitral annular calcification (MAC) can cause mitral stenosis symptoms. It’s difficult to treat even with surgery. People with calcium around the mitral valve often have similar problems with the heart’s aortic valve called aortic valve stenosis.
- Radiation therapy also known as radiotherapy. Radiation therapy is a cancer treatment that uses targeted radiation to kill or damage cancer cells, preventing their growth and spread. Radiation to the chest area can sometimes cause the mitral valve to thicken and harden. The heart valve damage typically occurs 20 to 30 years after radiation therapy.
- Congenital heart defect is a heart condition that is present at birth. Rarely, some babies are born with a narrowed mitral valve.
- Other causes. Other causes of mitral stenosis include lupus, other autoimmune conditions, infective endocarditis, endocardial fibroelastosis (a rare heart condition, primarily affecting infants and children, characterized by thickening of the endocardium or the inner lining of the heart due to excessive proliferation of fibrous and elastic tissues, potentially leading to heart failure and other complications), malignant carcinoid syndrome, systemic lupus erythematosus (SLE), Whipple disease, Fabry disease, and rheumatoid arthritis 2.
Mitral stenosis is usually caused by rheumatic fever or rheumatic heart disease. This is where an infection causes the heart to become inflamed. Over time, it can cause the flaps of the mitral valve to become hard and thick. Other causes include hard deposits that form around the mitral valve with age or a problem with the heart from birth (congenital heart disease).
Risk factors for mitral stenosis
Mitral valve stenosis is less common today than it once was because the most common cause, rheumatic fever, is rare in the United States. However, rheumatic fever remains a problem in developing nations.
Risk factors for mitral valve stenosis include:
- History of rheumatic fever
- Untreated strep infections. A history of untreated strep throat or rheumatic fever increases the risk of mitral valve stenosis. However, rheumatic fever is rare in the United States. But it’s still a problem in developing nations.
- Aging. Older adults are at increased risk of calcium buildup around the mitral valve.
- Radiation therapy. Radiation causes changes in the mitral valve shape and structure. Rarely, people who receive radiation therapy to the chest area for certain types of cancer may develop mitral valve stenosis.
- Illicit drug use. Methylenedioxymethamphetamine also called MDMA, molly or ecstasy, increases the risk of mitral valve disease.
- Use of certain medicines. Some migraine medicines have an ingredient called ergot alkaloids. Ergotamine (Ergomar) is an example. Ergot alkaloids may rarely cause heart valve scarring that leads to mitral stenosis. Older weight-loss medicines that contained fenfluramine or dexfenfluramine also are linked to heart valve disease and other heart problems. Fen-phen is an example. It’s no longer sold in the United States.
Mitral stenosis prevention
The best way to prevent mitral valve stenosis is to prevent its most common cause, rheumatic fever. You can do this by making sure you and your children see your doctor for sore throats. Untreated strep throat infections can develop into rheumatic fever. Fortunately, strep throat is usually easily treated with antibiotics.
Rheumatic fever prophylaxis with Benzathine penicillin is the primary prevention treatment in patients with streptococcal pharyngitis.
Mitral stenosis symptoms
Most people with mitral stenosis may feel fine with mitral valve stenosis or you may have minimal symptoms for decades. Mitral valve stenosis usually progresses slowly over time. When symptoms do happen, they may get worse with exercise or any activity that increases your heart rate. Mitral stenosis causes blood flow through the narrowed valve opening from the left atrium to the left ventricle to be reduced. As a result, the volume of blood bringing oxygen from the lungs is reduced, which can make you feel tired and short of breath. The volume and pressure from blood remaining in the left atrium increases which then causes the left atrium to enlarge and fluid to build up in the lungs. Mitral stenosis presents 20 to 40 years after an episode of rheumatic fever.
See your doctor if you develop:
- Trouble breathing or shortness of breath (dyspnea) at night when you lie down or after exercise (breathlessness)
- Dizziness or fainting.
- Coughing, which sometimes produces a pinkish, blood-tinged sputum
- Fatigue and tiredness
- Chest pain or chest discomfort that gets worse with activity and goes away with rest
- Fluid buildup in the lungs (pulmonary edema)
- Frequent respiratory infections such as bronchitis
- Heart palpitations (the feeling that the heart has skipped a beat) or irregular heartbeats called arrhythmias.
- Swelling (edema) of the feet and ankles
- A hoarse or husky-sounding voice.
Symptoms may begin with an episode of atrial fibrillation. Pregnancy, a respiratory infection, endocarditis, or other heart conditions may also cause symptoms. Mitral stenosis may eventually lead to heart failure, stroke, or blood clots to various parts of the body (thromboembolism).
Mitral valve stenosis may also produce signs that your doctor will find during your examination. These may include:
- Heart murmur
- Fluid buildup in the lungs (pulmonary edema)
- Irregular heart rhythms (arrhythmias)
On auscultation, the first heart sound (S1) is usually loud and maybe palpable due to increased force in the closing of the mitral valve.
The P2 (pulmonic) component of the second heart sound (S2) will be loud if severe pulmonary hypertension is due to mitral stenosis.
An opening snap is an additional sound that may be heard after the A2 (represents the closure of the aortic valve) component of the second heart sound (S2). This is the forceful opening of the mitral valve when the pressure in the left atrium is greater than the pressure in the left ventricle.
A mid-diastolic rumbling murmur with presystolic accentuation is heard after the opening snap. This murmur is a low pitch sound. It is best heard with the bell of the stethoscope at the apex. The murmur accentuates in the left lateral decubitus position and with isometric exercise.
Advanced mitral stenosis, presents with signs of right-sided heart failure (jugular venous distension, parasternal heave, hepatomegaly, ascites) and/or pulmonary hypertension.
Other signs include, atrial fibrillation, left parasternal heave (right ventricular hypertrophy due to pulmonary hypertension) and tapping the apical beat.
Mitral stenosis complications
Like other heart valve problems, mitral valve stenosis can strain your heart and decrease blood flow. Untreated, mitral valve stenosis can lead to complications such as:
- Pulmonary hypertension. This is a condition in which there’s increased pressure in the arteries that carry blood from your heart to your lungs (pulmonary arteries), causing your heart to work harder.
- Heart failure. A narrowed mitral valve interferes with blood flow. This can cause pressure to build in your lungs, leading to fluid accumulation. The fluid buildup strains the right side of the heart, leading to right heart failure. When blood and fluid back up into your lungs, it can cause a condition known as pulmonary edema. This can lead to shortness of breath and, sometimes, coughing up of blood-tinged sputum.
- Heart enlargement. The pressure buildup of mitral valve stenosis results in enlargement of your heart’s upper left chamber (atrium).
- Atrial fibrillation. The stretching and enlargement of your heart’s left atrium may lead to this heart rhythm irregularity in which the upper chambers of your heart beat chaotically and too quickly. Atrial fibrillation is a common complication of mitral stenosis. The risk increases with age and more-severe stenosis.
- Blood clots. Untreated atrial fibrillation can cause blood clots to form in the upper left chamber of your heart. Blood clots from your heart can break loose and travel to other parts of your body, causing serious problems, such as a embolic stroke if a clot blocks a blood vessel in your brain.
Mitral stenosis diagnosis
Your doctor will ask about your medical history and give you a physical examination that includes listening to your heart through a stethoscope. Mitral valve stenosis causes an abnormal heart sound, called a heart murmur.
Your doctor also will listen to your lungs to check lung congestion — a buildup of fluid in your lungs — that can occur with mitral valve stenosis.
Your doctor will then decide which tests are needed to make a diagnosis. For testing, you may be referred to a cardiologist.
Diagnostic tests
Common tests to diagnose mitral valve stenosis include:
- Transthoracic echocardiogram. Sound waves directed at your heart from a wandlike device (transducer) held on your chest produce video images of your heart in motion. This test is used to confirm the diagnosis of mitral stenosis.
- Transesophageal echocardiogram. A small transducer attached to the end of a tube inserted down your esophagus allows a closer look at the mitral valve than a regular echocardiogram does.
- Electrocardiogram (ECG). Wires (electrodes) attached to pads on your skin measure electrical impulses from your heart, providing information about your heart rhythm. You might walk on a treadmill or pedal a stationary bike during an ECG to see how your heart responds to exertion. On the ECG, the P wave changes suggest left atrial enlargement. The presence of right axis deviation and right ventricular hypertrophy suggests severe pulmonary hypertension. ECG frequently detects atrial arrhythmias such as atrial fibrillation.
- Chest X-ray. This enables your doctor to determine whether any chamber of the heart is enlarged and the condition of your lungs.
- Exercise stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart’s activity is checked. Exercise tests help show how the heart responds to physical activity and whether valve disease symptoms occur during exercise. If you can’t exercise, you might get medicines that affect the heart like exercise does.
- Cardiac computed tomography (CT ) scan or heart CT. A cardiac computed tomography (CT) scan is a procedure that utilizes multiple X-ray beams from different angles to acquire high-quality, three-dimensional (3D) images of your heart and the heart valves, along with the great vessels and surrounding structures. A cardiac CT is commonly done to see mitral stenosis that isn’t caused by rheumatic fever.
- Cardiac MRI or heart MRI. This test uses magnetic fields and radio waves to create detailed images of the heart. A cardiac MRI might be done to determine the severity of mitral valve stenosis.
- Cardiac catheterization. This test isn’t often used to diagnose mitral stenosis, but it may be done when other tests aren’t able to diagnose the condition or determine its severity. It involves threading a thin tube (catheter) through a blood vessel in your arm or groin to an artery in your heart and injecting dye through the catheter to make the artery visible on an X-ray. The dye helps the arteries show up more clearly on X-ray images and video. This provides a detailed picture of your heart.
Cardiac tests such as these help your doctor distinguish mitral valve stenosis from other heart conditions, including other mitral valve conditions. These tests also help reveal the cause of your mitral valve stenosis and whether the valve can be repaired.
Mitral stenosis Staging
After testing confirms a diagnosis of mitral or other heart valve disease, your heart doctor (cardiologist) may tell you the stage or severity of your heart condition. Staging helps determine the most appropriate treatment for you.
The stage of heart valve disease depends on many things, including your symptoms, the disease severity, the structure of the heart valve or valves, and blood flow through the heart and lungs 19. The definition of “severe” mitral stenosis is based on the severity of symptoms, as well as the severity at which intervention will improve symptoms 19. A mitral valve area ≤1.5 cm² is considered severe, which typically corresponds to a transmitral mean gradient of >5 mm Hg to 10 mm Hg at a normal heart rate.
Table 2. Stages of Mitral Valve Stenosis
| Stage | Definition | Valve Anatomy | Valve Hemodynamics | Hemodynamic Consequences | Symptoms |
|---|---|---|---|---|---|
| A | At risk of mitral stenosis | Mild valve doming during diastole | Normal transmitral flow velocity |
| None |
| B | Progressive mitral stenosis |
|
|
| None |
| C | Asymptomatic severe mitral stenosis |
|
|
| None |
| D | Symptomatic severe mitral stenosis |
|
|
|
|
Footnotes: The transmitral mean pressure gradient should be obtained to further determine the hemodynamic effect of the mitral stenosis and is usually >5 mm Hg to 10 mm Hg in severe mitral stenosis; however, because of the variability of the mean pressure gradient with heart rate and forward flow, it has not been included in the criteria for severity.
[Source 19 ]Mitral stenosis treatment
If you have mild to moderate mitral valve stenosis with no symptoms, you might not need immediate treatment. Instead, your doctor will monitor your mitral valve to see if your condition worsens.
Home remedies
To improve your quality of life if you have mitral valve stenosis, your doctor may recommend that you:
- Limit salt. Salt in food and drinks may increase pressure on your heart. Don’t add salt to food, and avoid high-sodium foods. Read food labels and ask for low-salt dishes when eating out.
- Maintain a healthy weight. Keep your weight within a range recommended by your doctor.
- Cut back on caffeine. Caffeine can worsen irregular heartbeats (arrhythmias). Ask your doctor about drinking beverages with caffeine, such as coffee or soft drinks.
- Seek prompt medical attention. If you notice frequent palpitations or feel your heart racing, seek medical help. Fast heart rhythms that aren’t treated can lead to rapid deterioration in people with mitral valve stenosis.
- Cut back on alcohol. Heavy alcohol use can cause arrhythmias and make symptoms worse. Ask your doctor about the effects of alcohol on your heart.
- Exercise. How long and hard you’re able to exercise may depend on the severity of your condition and the intensity of exercise. But everyone should engage in at least low-level, regular exercise for cardiovascular fitness. Ask your doctor for guidance before starting to exercise, especially if you’re considering competitive sports.
- See your doctor regularly. Establish a regular appointment schedule with your cardiologist or primary care provider.
Women with mitral valve stenosis need to discuss family planning with their doctors before becoming pregnant. Pregnancy causes the heart to work harder. How a heart with mitral valve stenosis tolerates the extra work depends on the degree of stenosis and how well the heart pumps. Throughout your pregnancy and after delivery, your cardiologist and obstetrician should monitor you.
Medications
No medications can correct a mitral valve defect. However, certain drugs can reduce symptoms by easing your heart’s workload and regulating its rhythm.
Your doctor might prescribe one or more of the following medications to reduce the symptoms of your mitral valve stenosis:
- Diuretics (water pills) to reduce fluid accumulation in your lungs or elsewhere.
- Blood thinners (anticoagulants) to help prevent blood clots if you have an irregular heartbeat called atrial fibrillation (AFib). A daily aspirin may be included.
- Beta blockers or calcium channel blockers to slow your heart rate and allow your heart to fill more effectively.
- Anti-arrhythmics to treat atrial fibrillation or other rhythm disturbances associated with mitral valve stenosis.
- Antibiotics to prevent a recurrence of rheumatic fever if that’s what caused your mitral stenosis. Rheumatic fever prophylaxis with Benzathine penicillin is the primary prevention treatment in patients with streptococcal pharyngitis.
Your cardiologist can provide you more information and can answer your questions about preventing endocarditis.
Figure 7. American Heart Association prevention of infective endocarditis
Procedures
A diseased or damaged mitral valve might eventually need to be repaired or replaced, even if you don’t have mitral valve disease symptoms. If you need surgery for another heart condition, a surgeon might do mitral valve repair or replacement at the same time as that treatment.
Percutaneous balloon mitral valvuloplasty
Balloon valvuloplasty also called percutaneous mitral commissurotomy or balloon valvotomy, is a procedure that can be used to widen the mitral valve if you have mitral stenosis. It’s usually done using local anaesthetic, where you remain awake but your skin is numbed. In this procedure a doctor inserts a soft, thin tube (catheter) tipped with a balloon in an artery in your arm or groin and guides it to the narrowed valve. Once in position, the balloon is inflated to widen the valve, improving blood flow. The balloon is then deflated, and the catheter with balloon is removed.
For some people, balloon valvuloplasty can relieve the signs and symptoms of mitral valve stenosis. However, you may need additional procedures to treat the narrowed valve over time.
Not everyone with mitral valve stenosis is a candidate for balloon valvuloplasty. This procedure is generally less effective than replacing the mitral valve, but recovery tends to be quicker and it may be a better option if your valve is not too narrow or you’re at an increased risk of surgery complications for example, if you’re pregnant or frail. Talk to your doctor to decide whether it’s an option for you.
Mitral valve surgery
Surgical options include:
- Commissurotomy. If balloon valvuloplasty isn’t an option, a cardiac surgeon might perform open-heart surgery to remove calcium deposits and other scar tissue to clear the valve passageway. Open commissurotomy requires that you be put on a heart-lung bypass machine during the surgery. You may need the procedure repeated if your mitral valve stenosis redevelops.
- Mitral valve replacement. If the mitral valve can’t be repaired, surgeons may perform mitral valve replacement. Mitral valve replacement is usually only done if you have mitral stenosis or mitral prolapse or regurgitation and are unable to have a valve repair. In mitral valve replacement, your surgeon removes the damaged valve and replaces it with a mechanical valve or a valve made from cow, pig or human heart tissue (biological tissue valve). Biological tissue valves degenerate over time, and often eventually need to be replaced. The operation is carried out under general anesthetic, where you’re asleep. Your surgeon will usually replace the valve through a single cut along the middle of your chest. People with mechanical valves will need to take blood-thinning medications for life to prevent blood clots. Most people experience a significant improvement in their symptoms after surgery, but speak to your surgeon about the possible complications. The risk of serious problems is generally higher than with mitral valve repair. Your doctor will discuss with you the benefits and risks of each type of valve and discuss which valve may be appropriate for you.
Mitral stenosis prognosis
Mitral valve stenosis can remain asymptomatic for years, especially when resulting from rheumatic fever. It can take decades following rheumatic fever before mitral valve stenosis develops 20. Once symptoms become apparent, the progression of the disease generally accelerates, particularly when it is secondary to rheumatic fever. Prior to the era of open-heart surgery, the prognosis for most patients with mitral stenosis was poor. In the era of mitral valve replacement, the prognosis is excellent. But older age, poor health, and a lot of calcium buildup on or around the mitral valves increase the risk of surgery complications. Survival is significantly better for patients undergoing an open mitral valve replacement compared to a commissurotomy. Today, there is an 80% survival at ten years, but in patients who have developed pulmonary hypertension secondary to mitral valve stenos survival is around three years 2. Other complications that may result in high morbidity include embolic stroke and persistent atrial fibrillation 21.
The prognosis (outlook) for children born with mitral valve stenosis depends large on the severity of their condition, often requiring screening for related heart problems throughout their lives 22.
- Shah SN, Sharma S, Bossuah KA. Mitral Stenosis (Nursing) [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568793[↩]
- Shah SN, Sharma S. Mitral Stenosis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430742[↩][↩][↩][↩]
- Brown KN, Ahmed I, Kanmanthareddy A. Catheter Management of Mitral Stenosis. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538483[↩]
- Harb, S.C., Griffin, B.P. Mitral Valve Disease: a Comprehensive Review. Curr Cardiol Rep 19, 73 (2017). https://doi.org/10.1007/s11886-017-0883-5[↩]
- Horstkotte D. Arrhythmias in the natural history of mitral stenosis. Acta Cardiol. 1992;47(2):105-13.[↩]
- Pressman GS, Ranjan R, Park DH, Shim CY, Hong GR. Degenerative Mitral Stenosis Versus Rheumatic Mitral Stenosis. Am J Cardiol. 2020 May 15;125(10):1536-1542. doi: 10.1016/j.amjcard.2020.02.020[↩]
- Ukita Y, Yuda S, Sugio H, Yonezawa A, Takayanagi Y, Masuda-Yamamoto H, Tanaka-Saito N, Ohnishi H, Miura T. Prevalence and clinical characteristics of degenerative mitral stenosis. J Cardiol. 2016 Sep;68(3):248-52. doi: 10.1016/j.jjcc.2015.09.021[↩]
- Wunderlich NC, Dalvi B, Ho SY, Küx H, Siegel RJ. Rheumatic Mitral Valve Stenosis: Diagnosis and Treatment Options. Curr Cardiol Rep. 2019 Feb 28;21(3):14. doi: 10.1007/s11886-019-1099-7[↩]
- Sequeira A, Morris L, Patel B, Duvall L, Gali D, Menendez D, Alexander G. Calcific mitral stenosis in the hemodialysis patient. Hemodial Int. 2014 Jan;18(1):212-4. doi: 10.1111/hdi.12094[↩]
- Imran TF, Awtry EH. Severe Mitral Stenosis. N Engl J Med. 2018 Jul 19;379(3):e6. doi: 10.1056/NEJMicm1715321[↩]
- Maeder MT, Weber L, Buser M, Gerhard M, Haager PK, Maisano F, Rickli H. Pulmonary Hypertension in Aortic and Mitral Valve Disease. Front Cardiovasc Med. 2018 May 23;5:40. doi: 10.3389/fcvm.2018.00040[↩]
- Banovic M, DaCosta M. Degenerative Mitral Stenosis: From Pathophysiology to Challenging Interventional Treatment. Curr Probl Cardiol. 2019 Jan;44(1):10-35. doi: 10.1016/j.cpcardiol.2018.03.004[↩]
- Shah SN, Sharma S. Mitral Stenosis. [Updated 2019 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430742[↩]
- American Heart Association. About Arrhythmia. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/AboutArrhythmia/About-Arrhythmia_UCM_002010_Article.jsp[↩]
- Centers for Disease Control and Prevention. Division of Birth Defects and Developmental Disabilities. Congenital Heart Defects (CHDs). https://www.cdc.gov/ncbddd/heartdefects/index.html[↩]
- Ejection Fraction Heart Failure Measurement. https://www.heart.org/en/health-topics/heart-failure/diagnosing-heart-failure/ejection-fraction-heart-failure-measurement[↩][↩]
- Ejection Fraction. https://my.clevelandclinic.org/health/articles/16950-ejection-fraction[↩]
- Regulation of Stroke Volume. https://cvphysiology.com/cardiac-function/cf002[↩]
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227. doi: 10.1161/CIR.0000000000000923 Erratum in: Circulation. 2024 Sep 17;150(12):e267. doi: 10.1161/CIR.0000000000001284[↩][↩][↩]
- Généreux P. Staging of Valve Disease Based on the Extent of Cardiac Damage: Ready for the Guidelines? JACC Cardiovasc Imaging. 2022 Jun;15(6):971-973. doi: 10.1016/j.jcmg.2022.04.012[↩]
- Pradhan RR, Jha A, Nepal G, Sharma M. Rheumatic Heart Disease with Multiple Systemic Emboli: A Rare Occurrence in a Single Subject. Cureus. 2018 Jul 11;10(7):e2964. doi: 10.7759/cureus.2964[↩]
- Wald RM, Mertens LL. Hypoplastic Left Heart Syndrome Across the Lifespan: Clinical Considerations for Care of the Fetus, Child, and Adult. Can J Cardiol. 2022 Jul;38(7):930-945. doi: 10.1016/j.cjca.2022.04.028[↩]