Monteggia fracture
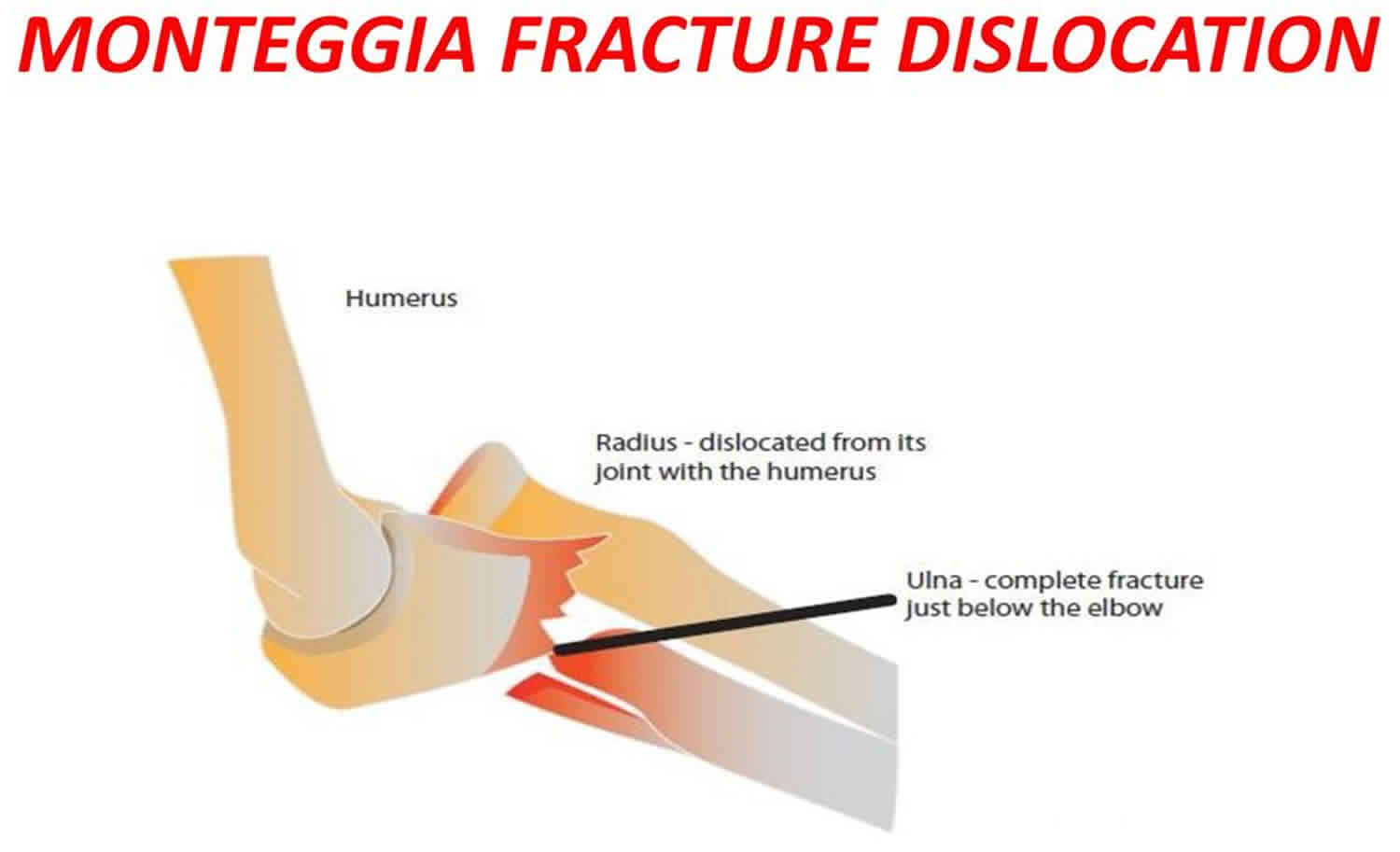
Monteggia fracture refers to a dislocation of the radial head in association with a fracture of the ulna (one of the bones of the forearm) at the elbow joint. Treatment of a Monteggia fracture-dislocation is with surgery to repair the ulna fracture. During the surgery, the radial head will return to its correct position.
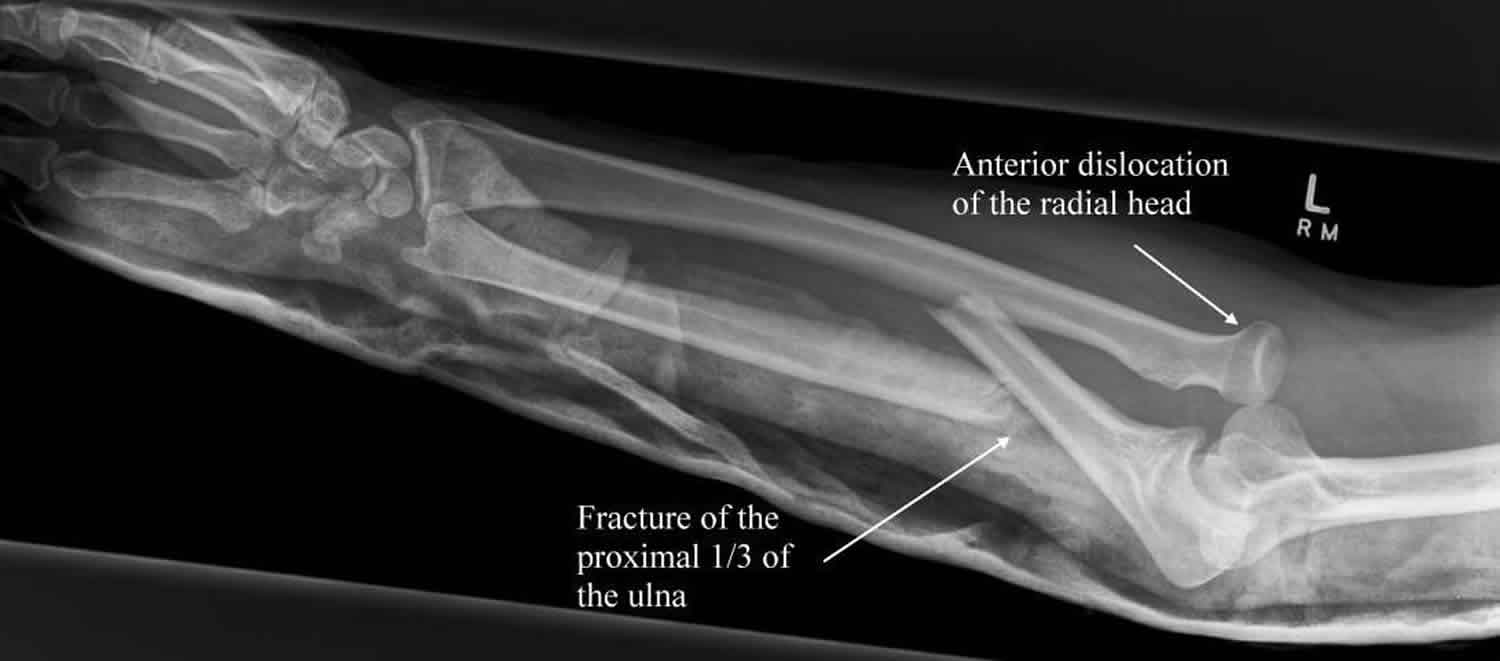
Figure 1. Monteggia fracture dislocation
Elbow anatomy
The elbow is a joint made up of three bones—the humerus, radius, and ulna.
- The humerus is the upper arm bone between the shoulder and the elbow.
- The radius is one of the forearm bones between the elbow and wrist. The radius is on the “thumb side” of the forearm.
- The ulna is the other forearm bone between the elbow and wrist, running next to the radius. The ulna is on the “pinky finger side” of the forearm.
Ligaments on the inner and outer sides of the elbow hold the joint together and muscles surround the joint on the front and back sides. The elbow joint is crossed by three major nerves.
The annular and radial collateral ligaments stabilize the radial head. These ligaments stretch or rupture during radial head dislocation 1. The radial head articulates with the humeral capitellum and the radial notch of the proximal ulna. The radius and ulna are closely invested by the interosseous membrane, which accounts for the increased risk of displacement or injury to the radius when the ulna fractures.
The distal ulna and radius also articulate at the distal radioulnar joint 2. The ulna provides a stable platform for rotation of the radius and forearm. The ulna and interosseous membrane also may provide stable platforms for dislocation of the proximal radius, leading to the Monteggia fracture.
The posterior interosseous nerve travels around the neck of the radius and dives under the supinator as it courses into the forearm. The median and ulnar nerves enter the antecubital fossa just distal to the elbow. The close proximity of these nerves may lead to injuries when a Monteggia fracture occurs. Neural injuries are generally traction injuries and result from stretching around the displaced bone or from energy dispersed during the initial injury.
Figure 2. Elbow joint
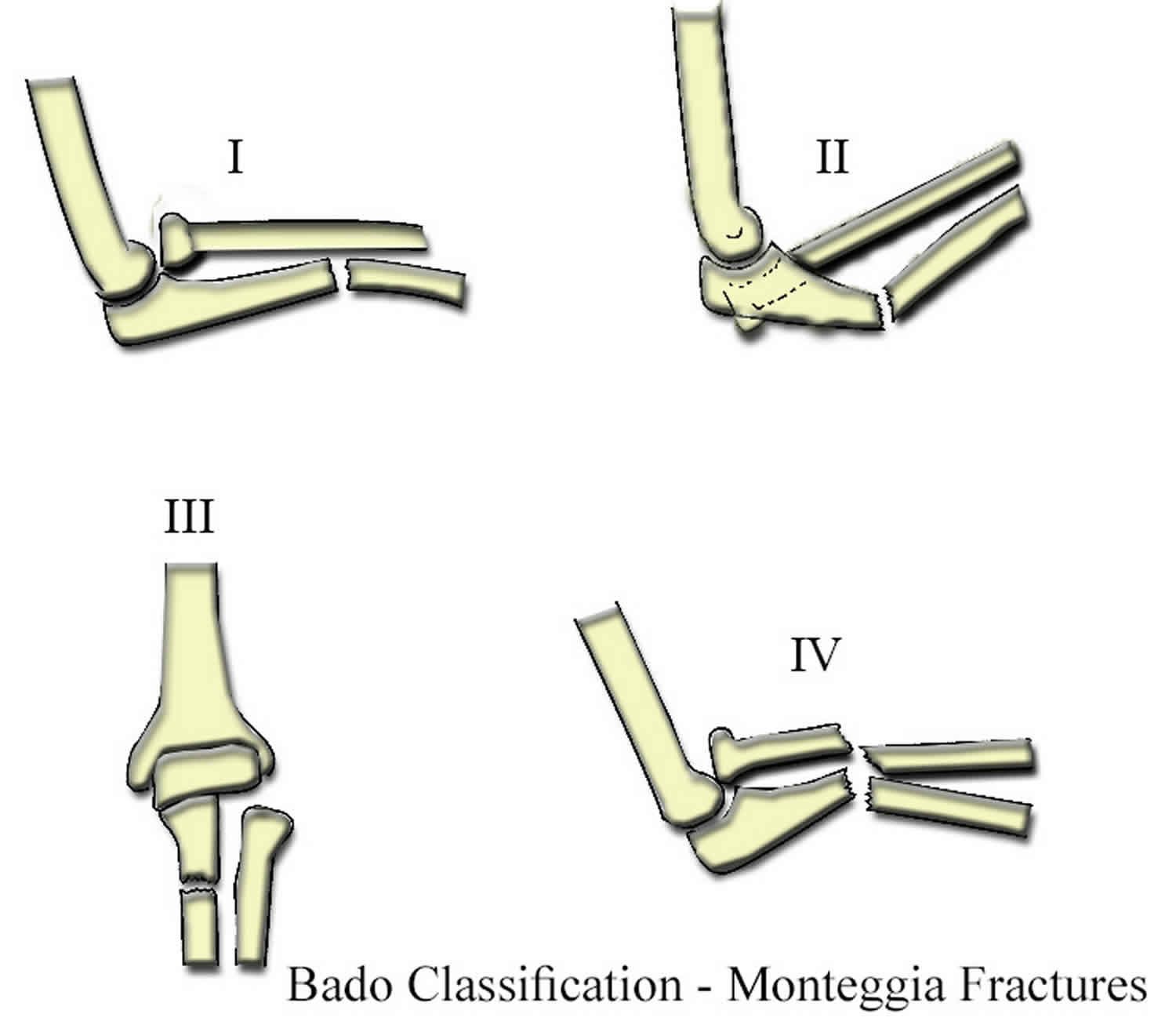
Monteggia fracture types
In 1967, Bado coined the term Monteggia lesion and classified the injury into the following four types 3:
- Type 1 – Fracture of the proximal or middle third of the ulna with anterior dislocation of the radial head
- classic Monteggia fracture-dislocations
- this type was originally described by Monteggia in 1814
- most common type
- Type 2 – Fracture of the proximal or middle third of the ulna with posterior dislocation of the radial head
- Type 3 – Fracture of the ulnar metaphysis with lateral dislocation of the radial head
- Type 4 – Fracture of the proximal or middle third of the ulna and radius with anterior dislocation of the radial head
The Bado classification of Monteggia fracture types is based on the recognition that the direction in which the apex of the ulnar fracture points is the same direction as the radial head dislocation 4.
Of the Monteggia fractures, Bado type 1 is the most common (59%), followed by type 3 (26%), type 2 (5%), and type 4 (1%).
Monteggia fractures in the pediatric population typically manifest with unique features that have led to a decreased emphasis on the direction of the radial head dislocation and an increased focus on the character of the fracture of the ulna. When the various fracture types occur in the immature bone of children, distinct patterns result and influence treatment considerations.
Monteggia fractures in children may be categorized according to the type of ulnar injury, as follows:
- Plastic deformation
- Incomplete (greenstick or buckle) fracture
- Complete transverse or short oblique fracture
- Comminuted or long oblique fracture
Plastic deformation of the ulna in association with anterior radial head dislocation represents up to 31% of anterior Monteggia lesions. Poor recognition of this injury pattern can lead to recurrent or persistent dislocation because the radial head reduction remains unstable until the plastic deformity is corrected. Incomplete fractures of the ulna and greenstick fractures represent other variants that must be corrected along with the radial head dislocation.
Figure 3. Monteggia fracture types
Monteggia fracture causes
Usually a Monteggia fracture is caused by falling on an outstretched hand with forced pronation 5. If the elbow is flexed, the chance of a type 2 or 3 lesion is greater. In some cases, a direct blow to the forearm can produce similar injuries.
Evans 6 and Penrose 7 studied the cause of Monteggia fractures on cadavers by stabilizing the humerus in a vise and subjecting different forces to the forearm. Penrose considered type 2 lesions a variation of posterior elbow dislocation. Bado believed that the type 3 lesion, the result of a direct lateral force on the elbow, was primarily observed in children.
In essence, high-energy trauma (e.g., a motor vehicle collision) and low-energy trauma (e.g., a fall from a standing position) can result in the described injuries. A high index of suspicion, therefore, should be maintained with any ulna fracture.
Monteggia fracture symptoms
No matter where the break occurs, most elbow fractures result in sudden, intense pain in the elbow and forearm.
Monteggia fracture symptoms include:
- Pain at the elbow that may be severe
- Swelling around the elbow
- Bones appearing ‘out of place’ at the elbow
- Bruising around the elbow
- Reduced movement at the elbow
- Numbness or tingling in the elbow, forearm or hand
- Weakness at the elbow, wrist, fingers or thumb
Monteggia fracture complications
Potential complications from a Monteggia fracture can be divided into two broad categories: acute and chronic.
Acute complications include the following:
- Bleeding
- Nerve injury – this can result in pain, tingling, numbness or weakness in the forearm or hand. Nerve injuries usually heal over 1-6 months.
- Swelling
- Compartment syndrome
- Loss of initial reduction
- Failure to diagnose the correct pathology
Chronic complications include the following:
- Malunion – this is when the fracture heals in an abnormal way, so that the normal bone structure is disrupted
- Nonunion – this is when the fracture ends don’t knit together, leaving two separate pieces of bone
- Radioulnar synostosis
- Elbow stiffness
- Myositis ossificans
- Infection – This is mainly a problem if the injury is treated with an operation, or if the bone has broken through the skin with the initial injury.
- Chronic pain – this is especially so if the fracture doesn’t heal properly, or the dislocation isn’t addressed properly.
Many of the complications listed are significantly reduced with timely diagnosis, adequate reduction, stable surgical fixation, and appropriate postoperative care.
Most nerve injuries are neurapraxias of the radial and median nerves, and function usually returns within 1-6 months. Baseline electrodiagnostic studies are obtained early. If nerve function does not return within 2-3 months, surgical exploration may be indicated. If the nerve injury results from reduction or operative treatment, it should be addressed immediately. Prolonged or complete nerve dysfunction requires early splinting and therapy and may result in the need for tendon transfers.
Li et al 8 conducted a study of the pathology of posterior interosseous nerve injury associated with Monteggia fracture-dislocation in children. For all eight patients, closed reduction was attempted before exploration of the posterior interosseous nerve. The nerve was found to be trapped acutely posterior to the radiocapitellar joint in four of five patients with Bado type 3 Monteggia fractures. In the remaining patients, chronic compressive changes and epineural fibrosis of radial nerve were observed, related to the time between injury and operation.
After microsurgical neurolysis, complete recovery of nerve function was obtained for all eight patients 8. The authors concluded that immediate surgical exploration of the posterior interosseous nerve should be performed for all children with Bado type 3 Monteggia fracture-dislocation in whom there is decreased or absent function of muscles innervated by the posterior interosseous nerve in the presence of an irreducible radial head 8.
If the radial head dislocates after surgery, improper ulnar reduction must be considered. If this is the case, the hardware should be removed and a proper reduction of the ulna should take place. If dislocation of the radial head is recognized more than 6 weeks after the surgery, a radial head excision should be performed. Treatment of chronic radial head dislocation in children with Monteggia fracture has been controversial, but some suggest that surgical treatment may be warranted 9.
In the case of nonunion or malunion, bone grafting and revision internal fixation may be considered.
Chronic pain may be the result of hardware or improper reduction. If all mechanical causes have been excluded, consulting a pain management specialist should be considered.
Monteggia fracture diagnosis
After discussing your symptoms and medical history, your doctor will perform a careful examination of your arm to determine the extent of the injury. He or she will look for:
- Tenderness
- Swelling
- Bruising
- Limited movement
- Change in color in the hand, an indication that circulation has been affected
During the physical examination, your doctor will also check to see whether any injury to the nerves or blood vessels has occurred.
The main investigation required is an X-ray. This will show the bony structures in the elbow and forearm and reveal any fractures and/or dislocations that are present. In the case of a Monteggia fracture, it will show a fracture of the ulna bone (in the forearm), and a dislocation of the radius (the other forearm bone) where it meets the elbow.
Monteggia fracture treatment
Indications for treatment of Monteggia fractures are based on the specific fracture pattern and the age of the patient (ie, pediatric or adult) 10. Most Monteggia fractures are treated with an operation. This is because it is a particularly unstable type of injury that needs to be stabilized with plates, screws or pins. The specific operation that is required depends on where the forearm bone (ulna) has been broken. It is especially important that the dislocation is fixed quickly after the injury has happened. For this reason, if there is a delay in getting to the operating theater for any reason, the dislocation may be fixed (without fixing the fracture) in the emergency room under sedation.
Certain types of Monteggia fractures, when they occur in children, do not require an operation and can be managed with a cast. Nonoperative treatment is successful for most Monteggia injuries in children, for the following reasons 11:
- The majority of the fractures are inherently stable
- Children require a shorter time for both the osseous and the ligamentous injuries to heal
- Children have little trouble regaining motion lost through stiffness, despite immobilization of the fractures for the duration of the initial healing period (3-6 weeks)
- The potential may exist for remodeling of mild residual angular deformities (< 10°)
Although most pediatric fracture patterns can be managed conservatively with closed reduction and long arm casting, most adult fractures require open reduction and internal fixation (ORIF). Few contraindications for surgery exist. Once the radial head is reduced in closed injuries, surgical treatment may be delayed until the patient is stable and the surgery may be performed in a more elective fashion.
Closed reduction of the radial head dislocation under sedation should be performed on an emergency basis within 6-8 hours of the injury. This is usually achieved with supination of the forearm, but it may require traction and direct pressure on the radial head. If closed reduction is unsuccessful, the patient should be taken to the operating room within this same time frame for open reduction. Delay in reduction of the radius may lead to permanent articular damage, further nerve injury, or both.
The stability of the reduction depends on the fracture pattern. Greenstick fractures have plastic deformation that may resist maintenance of reduction and necessitate completion of the fracture to keep the radial head reduced. However, completing the fracture may make it more difficult to maintain rotational alignment of the ulna. This difficulty can be alleviated with appropriate reduction techniques. Greenstick proximal ulna fractures require appropriate reduction using supination in addition to flexion and extension maneuvers 12.
An open fracture requires immediate operative intervention. In closed injuries, once the radial head is reduced, the forearm is splinted, and operative fixation of the ulna fracture may then be carried out electively. Whereas adults usually require operative internal fixation to stabilize the ulna and prevent further displacement forces on the radiocapitellar joint, children with closed Monteggia fractures are generally treated in a closed fashion. A posterior long arm splint with the elbow in 90° of flexion and full supination is the immobilization method of choice for types 1, 3, and 4. Type 2 injuries (posterior lesions) are best splinted in 70° elbow flexion with supination.
If the wound is open and heavily contaminated, serial debridement may be indicated before plate fixation. In medically unstable patients, emergency treatment of the open wound is still necessary. The procedure can be limited to irrigation and debridement of the open wound and closed reduction at the bedside, performed with regional anesthesia or, if absolutely necessary, with local anesthesia and sedation. If the patient is unable to tolerate operative treatment, the fracture-dislocation may be treated with cast immobilization after reduction of the radius and irrigation and debridement if the fracture is open.
Future research will help identify appropriate treatment protocols for achieving optimum long-term outcomes. The most important step is to educate the specialist, emergency physician, and primary care physician regarding correct diagnosis and treatment of these injuries.
Long-term monitoring
The patient should be evaluated at 5-7 days. If nonsurgical management has been employed, consideration should be given to leaving the splint or cast on and overwrapping to avoid loss of reduction by removing the immobilization. Follow-up radiography at 2, 4, and 6 weeks and then every 3 months thereafter is recommended to monitor healing and union of the fracture.
The average duration of casting is 6 weeks for pediatric patients and 8-12 weeks for adults. A posterior long arm cast in 90-110° flexion and supination should be used to maintain reduction based on fracture type. If surgery was performed, a wound check is necessary, with suture removal 5-7 days after the operative procedure. Surgical repair should allow for a shorter period of cast immobilization and early range-of-motion (ROM) in a brace, beginning 2-4 weeks after the procedure.
In pediatric patients, hardware removal commonly takes place 6-12 months after healing to prevent growth disturbance. In adults, hardware removal is optional; it may be considered in cases of pain, infection, or malunion/nonunion. For this reason, these patients should be followed for at least 1 year 13.
Surgical therapy
Open fractures require emergency surgical consultation. The initial treating physician may reduce the radial head dislocation and splint this fracture. Otherwise, an orthopedic surgeon should be consulted immediately to reduce the radial head. Anatomic reduction of the ulna is usually required before radial head reduction. Unless the fracture is open, surgical treatment is performed on an elective basis. Whereas most adults require operative treatment, most pediatric fractures are treated with closed reduction.
Operative fixation of complete fractures of the ulna with proximal radioulnar joint dislocation is recommended in children. The complete disruption of bone continuity is likely to be associated with substantial soft-tissue trauma in these injuries. Shortening and angulation of complete fractures after cast immobilization is not uncommon. Anatomic reduction of the ulnar fracture and radial head often requires operative treatment.
In the past, transverse and short oblique fractures were adequately treated with intramedullary wire fixation. Intramedullary wires, however, cannot be relied on to maintain reduction of complete fractures that are either long oblique in pattern or comminuted; the wires therefore are not used anymore. These fractures are likely to displace or even shorten; consequently, they should be fixed with a plate and screws.
As a result of the rapidity of osseous repair and the tolerance of cast immobilization in children, the use of plate-and-screw constructs that are smaller (typically a one-third tubular or semitubular plate) and shorter (two or three holes [four or six cortices] proximal and distal to the fracture) than those recommended for adults are usually adequate.
Postoperative care
Follow-up appointments are scheduled for wound checks and suture removal according to the nature of the soft-tissue injury and operative treatment. If rigid fixation is achieved and the radiocapitellar joint remains stable, the patient is referred to begin range-of-motion (ROM) exercises under the close supervision of a qualified physical therapist.
Patients with stable injuries may be placed in range-of-motion braces for 6-8 weeks. Unstable injuries should remain in cast immobilization until stability is achieved at 4-6 weeks.
Significant concern exists regarding loss of elbow motion with prolonged immobilization. Chronic radiocapitellar instability is unusual and may be addressed surgically.
Monteggia fracture prognosis
In 1991, Anderson and Meyer used the following criteria to evaluate forearm fractures and their prognosis 14:
- Excellent – Union with less than 10° loss of elbow and wrist flexion/extension and less than 25% loss of forearm rotation
- Satisfactory – Union with less than 20° loss of elbow and wrist flexion/extension and less than 50% loss of forearm rotation
- Unsatisfactory – Union with greater than 30° loss of elbow and wrist flexion/extension and greater than 50% loss of forearm rotation
- Failure – Malunion, nonunion, or chronic osteomyelitis
Pain, nerve dysfunction, and cosmetic deformity are other factors to consider in evaluating the outcome of treatment in Monteggia fracture-dislocations. Bado type 2 Monteggia fractures that are associated with ulnohumeral dislocation have been noted to have outcome scores with greater disability than those without ulnohumeral dislocation 15.
In a retrospective study on the functional and radiologic long-term outcome of open reduction and internal fixation (ORIF) in 11 skeletally mature patients with Bado type 1 Monteggia fractures, Guitton et al 2 found that the mean arc of elbow flexion increased from 110º at early follow-up to 120º at late follow-up. The mean arc of forearm rotation increased from 145º to 149º. The mean Broberg and Morrey score increased from 89 points to 94 points, and the median Disabilities of the Arm, Shoulder, and Hand score was 7 points at long-term follow-up.
In a study evaluating long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in 22 children (14 boys, 8 girls; age range, 4 years to 15 years 11 months), Nakamura et al 15 noted that the postoperative Mayo Elbow Performance Index at follow-up ranged from 65 to 100, with 19 excellent results, two good results, one fair result, and zero poor results.
In 17 of the 22 patients, the radial head remained in a completely reduced position, and it was subluxated in five patients 15. Osteoarthritic changes were seen at the radiohumeral joint in four patients. Radiographically, there were 15 good results, seven fair results, and zero poor results. A good radiographic result was seen in all patients who underwent open reduction within 3 years after injury or before reaching 12 years of age.
Datta et al 16 conducted a prospective, longitudinal study of 21 children with Monteggia fracture with dislocation (18 type 1, three type 3), all of whom were treated by modified Hirayama corrective osteotomy of the ulna with wedge bone grafting, restoration of bone length, reconstruction of the annular ligament using the Bell Tawse method, and fixation of the radial head with transcapitellar Kirschner wire (K-wire). The average follow-up period was 5.5 years.
The investigators evaluated outcomes on the basis of the 100-point Mayo Elbow Performance Index, radiology, and questionnaire 16. The mean postoperative increase in Mayo Elbow Performance Index score was 30. Range of motion increased by an average of 30º. Subluxation of the radial head occurred in three patients; one patient experienced transient palsy of the posterior interosseous nerve; and distortion of the radial head (which had no bearing on function) occurred in three.
- Tan JW, Mu MZ, Liao GJ, Li JM. Pathology of the annular ligament in paediatric Monteggia fractures. Injury. 2008 Apr. 39 (4):451-5.[↩]
- Guitton TG, Ring D, Kloen P. Long-term evaluation of surgically treated anterior monteggia fractures in skeletally mature patients. J Hand Surg Am. 2009 Nov. 34 (9):1618-24.[↩][↩]
- Bado JL. The Monteggia lesion. Clin Orthop Relat Res. 1967 Jan-Feb. 50:71-86.[↩]
- Iyer RS, Thapa MM, Khanna PC et-al. Pediatric bone imaging: imaging elbow trauma in children–a review of acute and chronic injuries. AJR Am J Roentgenol. 2012;198 (5): 1053-68. doi:10.2214/AJR.10.7314[↩]
- Cooper G. Blueprints Orthopedics. Blackwell Publishers. (2005) ISBN:1405104015.[↩]
- EVANS EM. Pronation injuries of the forearm, with special reference to the anterior Monteggia fracture. J Bone Joint Surg Br. 1949 Nov. 31B (4):578-88, illust.[↩]
- PENROSE JH. The Monteggia fracture with posterior dislocation of the radial head. J Bone Joint Surg Br. 1951 Feb. 33-B (1):65-73.[↩]
- Li H, Cai QX, Shen PQ, Chen T, Zhang ZM, Zhao L. Posterior interosseous nerve entrapment after Monteggia fracture-dislocation in children. Chin J Traumatol. 2013. 16 (3):131-5.[↩][↩][↩]
- Di Gennaro GL, Martinelli A, Bettuzzi C, Antonioli D, Rotini R. Outcomes after surgical treatment of missed Monteggia fractures in children. Musculoskelet Surg. 2015 Sep. 99 Suppl 1:S75-82.[↩]
- Wong JC, Getz CL, Abboud JA. Adult Monteggia and Olecranon Fracture Dislocations of the Elbow. Hand Clin. 2015 Nov. 31 (4):565-80.[↩]
- Leonidou A, Pagkalos J, Lepetsos P, Antonis K, Flieger I, Tsiridis E, et al. Pediatric Monteggia fractures: a single-center study of the management of 40 patients. J Pediatr Orthop. 2012 Jun. 32(4):352-6.[↩]
- Van Tongel A, Ackerman P, Liekens K, Berghs B. Angulated greenstick fractures of the distal forearm in children: closed reduction by pronation or supination. Acta Orthop Belg. 2011 Feb. 77 (1):21-6.[↩]
- Delpont M, Louahem D, Cottalorda J. Monteggia injuries. Orthop Traumatol Surg Res. 2018 Feb. 104 (1S):S113-S120.[↩]
- Anderson LE, Meyer FN. Fractures of the shafts of the radius and ulna. Rockwood CA, Green DP, Bucholz R, eds. Fractures in Adults. 3rd ed. Philadelphia: JB Lippincott; 1991. Vol 1[↩]
- Nakamura K, Hirachi K, Uchiyama S, Takahara M, Minami A, Imaeda T, et al. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg Am. 2009 Jun. 91 (6):1394-404.[↩][↩][↩]
- Datta T, Chatterjee N, Pal AK, Das SK. Evaluation of outcome of corrective ulnar osteotomy with bone grafting and annular ligament reconstruction in neglected monteggia fracture dislocation in children. J Clin Diagn Res. 2014 Jun. 8 (6):LC01-4.[↩][↩]