Myeloma protein
Multiple myeloma is a cancer of plasma cells. Plasma cells develop from one type of white blood cell called B lymphocytes and are an important part of the immune system. Their primary function is to produce antibodies – targeted immunoglobulin proteins that help protect the body against infections. Normally, plasma cells are produced as needed. When the immune system is exposed to disease-causing bacteria and viruses (pathogens), some B cells become plasma cells and begin to produce antibodies. Multiple myeloma is a cancer of plasma cells. Plasma cells develop from one type of white blood cell called B lymphocytes and are an important part of the immune system. Their primary function is to produce antibodies – targeted immunoglobulin proteins that help protect the body against infections. Normally, plasma cells are produced as needed. When the immune system is exposed to disease-causing bacteria and viruses (pathogens), some B cells become plasma cells and begin to produce antibodies.
Sometimes, however, a plasma cell may become malignant. It begins to divide uncontrollably, generating numerous copies of itself (clones) that form tumors in the bone marrow and crowd out other types of normal cells. In time, these tumors interfere with normal cell production and erode the surrounding bone, producing soft spots and holes (lytic lesions). Depending on the number of tumors, this condition has different names:
- Plasmacytoma—a single plasma cell tumor forms in the bone or elsewhere in the body
- Multiple myeloma—more than one plasma cell tumor forms in the bone. Multiple myeloma is relatively uncommon and comprises about 1% of cancers. The American Cancer Society estimates that about 30,000 new cases of multiple myeloma are diagnosed each year in the U.S. and that 12,500 people with multiple myeloma die. The cause of multiple myeloma is not yet known. The risk of developing it increases with age, with the majority of cases being diagnosed in people at least 65 years old. While there are a few families who have a higher incidence of multiple myeloma, most people will not have any affected relatives. It is thought that the disease may be associated with a decrease in immune system function, occupational exposure to toxins and/or solvents, genetic factors, certain viruses, and radiation exposure.
Since the malignant cells are clones, derived from a single plasma cell, they all produce identical antibodies called abnormal monoclonal immunoglobulins (M proteins), which are present in the blood and sometimes in the urine.
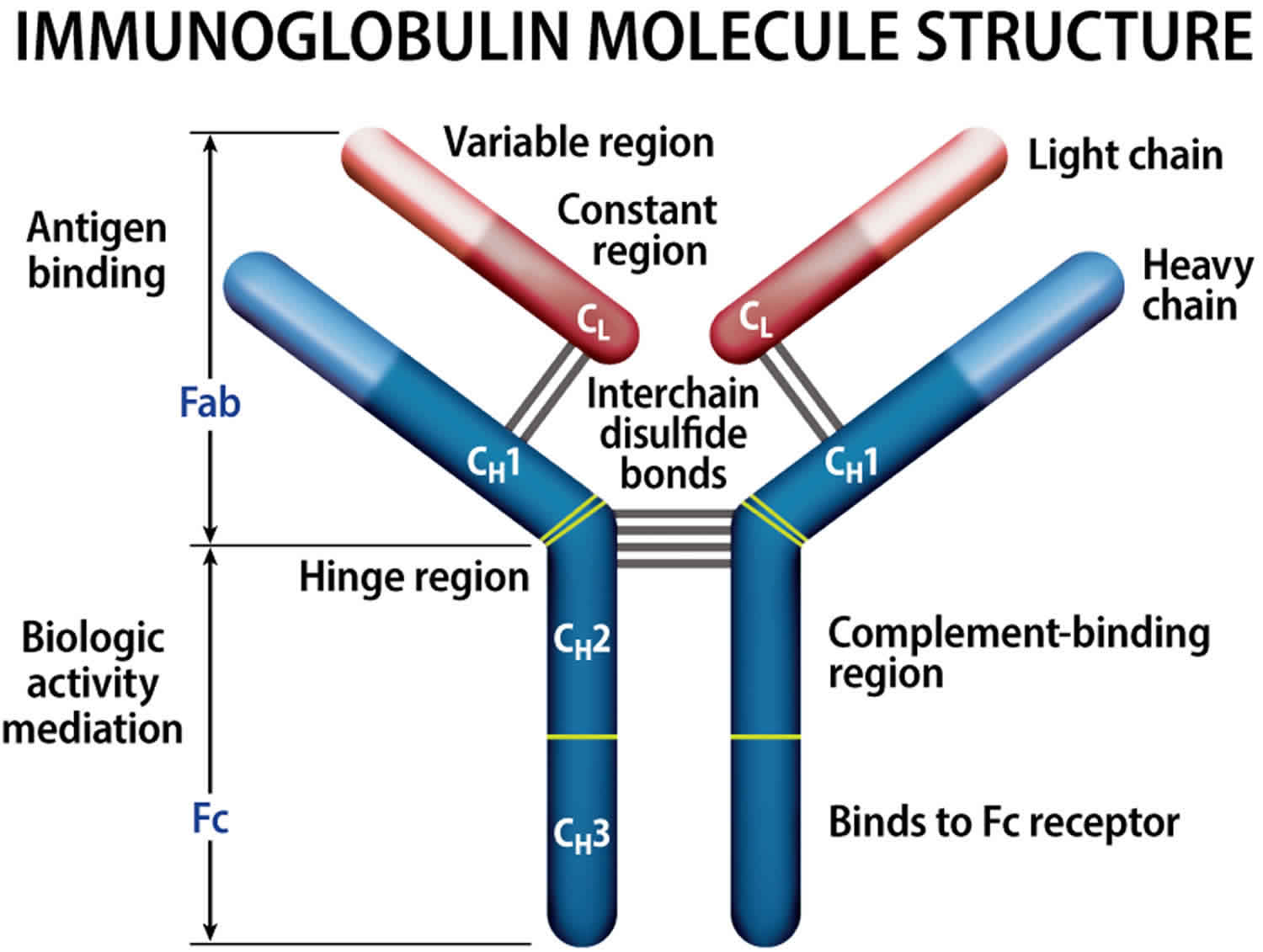
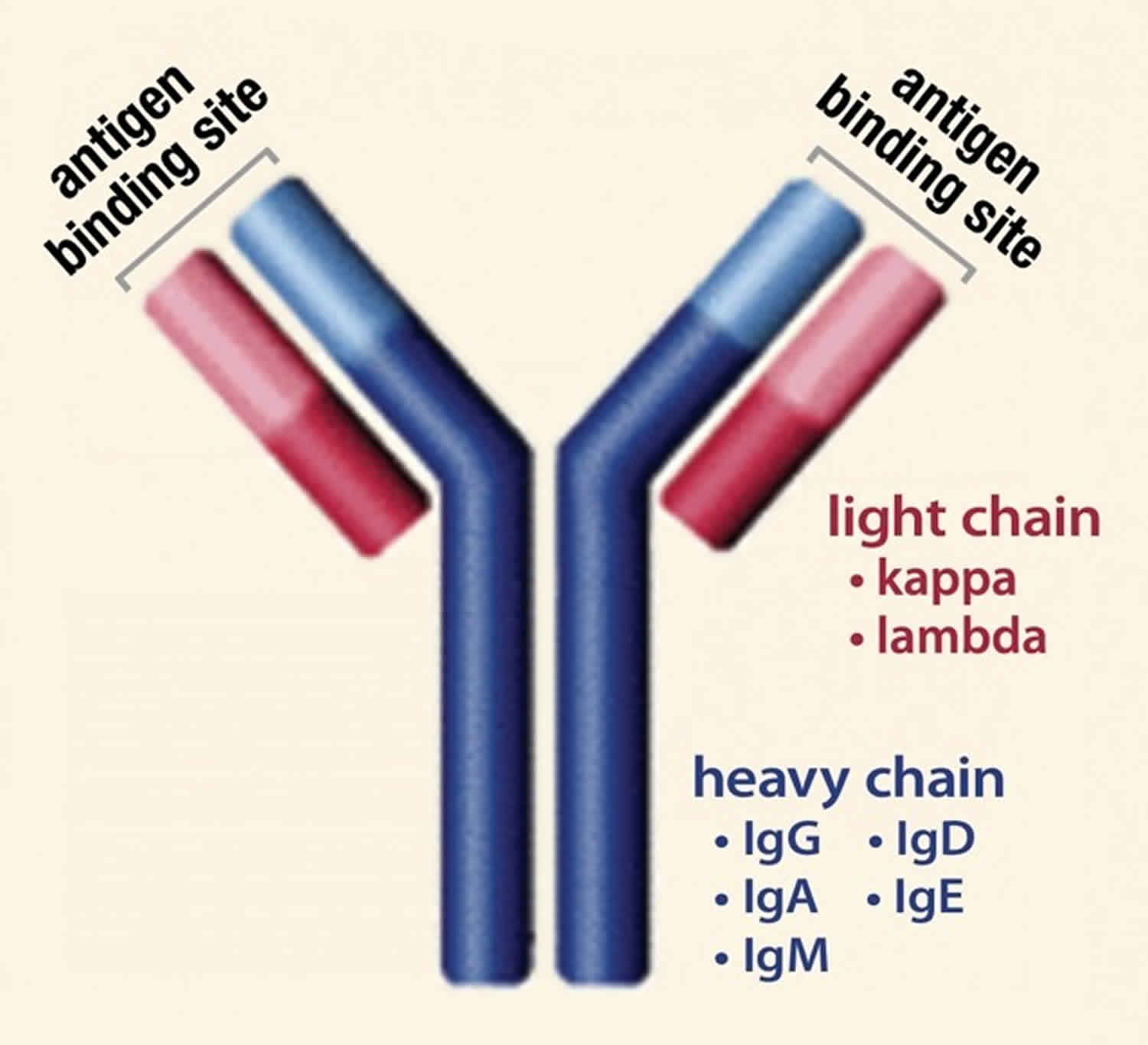
Normally, the body makes five different types of immunoglobulins – IgG, IgM, IgA, IgE and IgD. Each one has slightly different immune system functions. Each type of immunoglobulin is composed of four protein chains – two identical heavy (long) protein chains and two identical light (shorter) protein chains.
The heavy chains may consist of one of five different types that correspond with the type of immunoglobulin produced: gamma (IgG), mu (IgM), alpha (IgA), epsilon (IgE) and delta (IgD).
The light chains consist of one of two different types called kappa and lambda.
Within a plasma cell, two heavy chains of one type and two light chains of one type become attached to form one intact immunoglobulin molecule. Each particular plasma cell will produce only one type of immunoglobulin.
Subtypes of immunoglobulins
- IgG kappa
- IgA kappa
- IgD kappa
- IgE kappa
- IgM kappa
- IgG lambda
- IgA lambda
- IgD lambda
- IgE lambda
- IgM lambda
In people with multiple myeloma, the malignant plasma cells produce only one type of intact (whole) immunoglobulin in large amounts and/or produce an excess of only one of the light chains, or rarely heavy chain-only types. These identical immunoglobulins or light chains are also known as Monoclonal proteins or M proteins. Though the type of M protein produced by malignant cells may vary from one person to the next, within one particular person it is always the same since it is produced by identical or cloned plasma cells.
The type of myeloma a person has is often referred to by the type of M protein produced, whether an intact immunoglobulin or light chain.
- Intact immunoglobulin—people are most likely to have IgG and IgA myelomas, with IgG types making up about 60% of myelomas and IgA types making up about 20% of myelomas. Cases of IgE and IgD are rarely reported. Some people who produce monoclonal IgM may have a related but different condition called Waldenström macroglobulinemia.
- Light chain—myeloma patients producing an abnormal amount of only light chains are in the minority. They comprise about 20% of cases. The M-proteins that they produce are called free light chains (Bence Jones) proteins. Surplus free light chains are released into the bloodstream and since they are relatively small molecules, they are filtered by the kidneys and released into the urine. Free light chains are typically found in small quantities in the blood and large quantities in the urine.
Sometimes people will produce small amounts of identical copies of the same immunoglobulin (also known as monoclonal gammopathy) but not have any of the signs, symptoms, or complications of multiple myeloma. This condition is referred to as monoclonal gammopathy of undetermined significance or MGUS. Often, this condition is only discovered when routine tests reveal abnormal amounts of protein in the blood. About 1% of these people per year progress to multiple myeloma or some other related disease, such as lymphoma. Generally, these people do not require any treatment, but they are closely monitored. Some of the tests used to diagnose and/or follow multiple myeloma are used to monitor people with monoclonal gammopathy of undetermined significance (MGUS).
Figure 1. Immunoglobulin structure
Multiple myeloma types
Multiple myeloma has different types and subtypes. These types are based on the immunoglobulin (protein) produced by the myeloma cell. The various immunoglobulins have different functions in the body. Each immunoglobulin is made up of two heavy chains and two light chains.
- The five types of heavy protein chains are G, A, D, E, and M.
- The two types of light protein chains are kappa (κ) and lambda (λ).
Furthermore, there are different subtypes of myeloma.
Normal plasma cells secrete immunoglobulins (antibodies) to fight infections. Immunoglobulins are proteins that attach to substances entering the body that the body recognizes as foreign.
Normal immunoglobulins are called “polyclonal protein.” Myeloma cells, which are cancerous plasma cells, secrete monoclonal protein. Monoclonal protein is an abnormal immunoglobulin that cannot properly fight infection.
Healthy plasma cells or myeloma cells can produce immunoglobulins. These immunoglobulins made up of two heavy chains and two light chains that are bound together.
The five possible types of immunoglobulin (abbreviated “Ig”) are heavy chains: IgG, IgA, IgD, IgE, and IgM.
The possible types of light chains are either kappa (κ) or lambda (λ).
Myeloma cells make immunoglobulins. These immunoglobulins are made up of only one type of heavy chain (G, A, D, E, or M) and one type of light chain (kappa or lambda). The most common type of myeloma is IgG kappa. In IgG kappa myeloma, the myeloma cells produce an immunoglobulin made from two IgG heavy chains bound to two kappa light chains.
About 15% of patients have light chain myeloma. In this type of myeloma, the myeloma cells secrete only light chain protein and no heavy chains. It is also known as “Bence-Jones myeloma” (after the doctor who discovered it).
One to two-percent of patients have “non-secretory myeloma.” In non-secretory myeloma, the myeloma cells produce very little or no monoclonal protein of any type.
Your doctor will order tests to identify your type of myeloma. It’s important to know which type you have as you will be able to better understand your test results.You will be able to determine if your level of monoclonal protein is stable, increasing, or decreasing.
Table 1. Types of Myeloma
| Disease Type | Description |
| Myeloma IgG k or λ IgA k or λ Rarer subtypes: IgD, E, or M |
|
| Light Chain only or Bence Jones (BJ) myeloma: k or λ types |
|
| Non-secretory myeloma: |
|
| IgM myeloma: k or λ subtypes |
|
Multiple myeloma tests and staging
The goals of testing for multiple myeloma are to diagnose the condition, determine its severity and spread, monitor its progress, detect complications as they arise, and monitor the effectiveness of treatment.
There is no one single test that can diagnose multiple myeloma. Typically, the disease is diagnosed using a combination of a person’s signs and symptoms, medical history, physical examination, laboratory tests, and/or imaging tests.
Laboratory tests
Multiple myeloma may first be detected during routine wellness testing. It may be suspected when a person has:
- Elevated total protein
- Elevated calcium
- Low white or red blood cell count
- Moderate to large amounts of protein in the urine
Findings such as these may raise suspicions but are not diagnostic as similar results may be seen with a variety of other conditions. Rather, they indicate the need for further testing.
Tests used as a follow-up to abnormal routine tests and to help diagnose the disease may include one or more of the following:
- Protein and immunofixation electrophoresis. These tests are used to help diagnose and monitor multiple myeloma. Protein electrophoresis separates the proteins in a blood or urine sample into several groups based on their electrical charge and size. In most people with multiple myeloma, large amounts of an abnormal immunoglobulin protein (M-protein) may show up as a large peak on the electrophoresis scan, also known as an M spike. The amount of normal immunoglobulins in the sample may be visibly decreased as well. Usually, both a blood and a urine sample will be tested to detect free light chains and intact immunoglobulins. Immunofixation electrophoresis is done to identify the specific type of protein that is being produced by the malignant plasma cells. The amount of protein produced may vary throughout the course of the disease, but the type will remain the same.
- Urine free light chains (Bence Jones protein). These can be detected in the urine of some people with multiple myeloma. The sample tested is usually a 24-hour urine (a collection of all urine voided over a 24-hour period) because the total amount of free light chains in 24 hours is related to the amount of tumor that is present. Either the kappa or lambda light chains (but not both in the same person) may be measured to help diagnose multiple myeloma and monitor the effectiveness of treatment.
- Serum free light chains. Serum free light chains test measures the amount of free light chains in the blood. Even in normal circumstances (and for unknown reasons), plasma cells produce an excess of light chains compared to heavy chains, and there is usually a small amount of light chains that do not become incorporated into intact immunoglobulins. These remain as free light chains and are released into the bloodstream. Most people with multiple myeloma produce increased amounts of either kappa or lambda free light chains, which can be measured in blood. Consequently, the ratio of kappa to lambda light chains is abnormal and is a sensitive indicator for this disease. This test is used to help diagnose and to monitor progression and/or treatment.
- Quantitative immunoglobulins. Each of these tests measures amounts of a different type of immunoglobulin, or antibody, in the blood. The multiple myeloma protein may be an IgG, IgA or, rarely, an IgD or IgE immunoglobulin. People with a monoclonal IgM immunoglobulin may have a related but different disease (Waldenstrom macroglobulinemia). Tests for IgG, IgA, and IgM may be ordered to help diagnose multiple myeloma and to monitor the course of the disease and its effect on the production of normal immunoglobulins. Note that the test does not differentiate abnormal immunoglobulin produced by myeloma cells and the non-tumor immunoglobulin of the same type produced by normal plasma cells.
- Serum immunoglobulin heavy chain/light chain. These tests can identify separately the different light chain types of each immunoglobulin class, including IgG-kappa, IgG-lambda, IgA-kappa, IgA-lambda, IgM-kappa, and IgM-lambda. The molecules are then measured in pairs (e.g., IgG-kappa / IgG-lambda) to calculate ratios of involved monoclonal immunoglobulin to background uninvolved immunoglobulin concentrations. The tests can be used to monitor people with multiple myeloma.
- Bone marrow aspiration and biopsy. Multiple myeloma is a disease of the bone marrow. People usually require a bone marrow evaluation to confirm the diagnosis, evaluate how many malignant plasma cells are present in the marrow, and determine to what degree they have affected the production of normal white blood cells, red blood cells, and platelets.
- Cytogenetic analysis. In these tests, which include karyotyping and florescence in situ hybridization (FISH), cells are examined under a microscope to look for abnormal chromosomes. Abnormalities like chromosome translocations (mismatched parts) or deletions are sometimes associated with multiple myeloma. Finding these abnormalities can provide information about an individual’s prognosis.
Other laboratory tests
Other tests that may be done as part of an initial diagnostic workup, to monitor the progress of the disease, and to help detect and address complications include:
- Comprehensive metabolic panel (CMP), a group of tests used to evaluate kidney and other organ function, electrolyte status, and to determine calcium, albumin, and total protein levels
- Complete blood count (CBC), counts and evaluates white blood cells, red blood cells, and platelets and determines the extent of anemia (measures hemoglobin)
- Uric acid levels may be elevated as a complication of multiple myeloma.
- Beta-2 microglobulin, a protein on the cell surface of myeloma and other cells; increased levels may indicate a poorer prognosis; this test may be used to help stage the disease.
- Serum viscosity, a measure of how “thick” the fluid portion of the blood is; when levels of the abnormal protein become very high, serum viscosity may increase and cause symptoms.
Serum and Urine Protein Electrophoresis
Serum protein electrophoresis is a test that measures the amount of heavy chain monoclonal protein made by myeloma cells.
serum protein electrophoresis separates all the proteins in the blood according to their electrical charge. Urine protein electrophoresis, or urine protein electrophoresis, does the same thing for proteins in the urine.
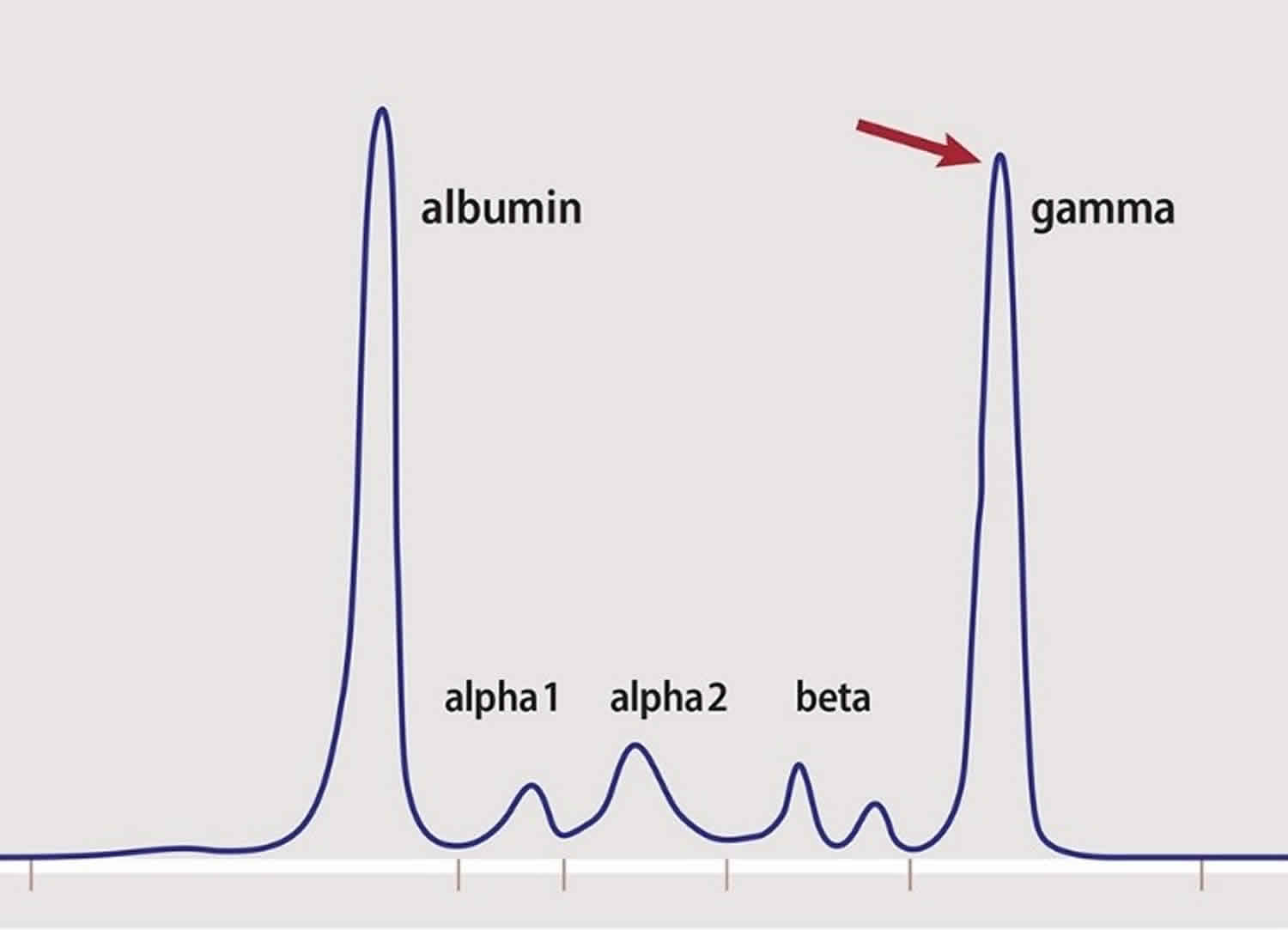
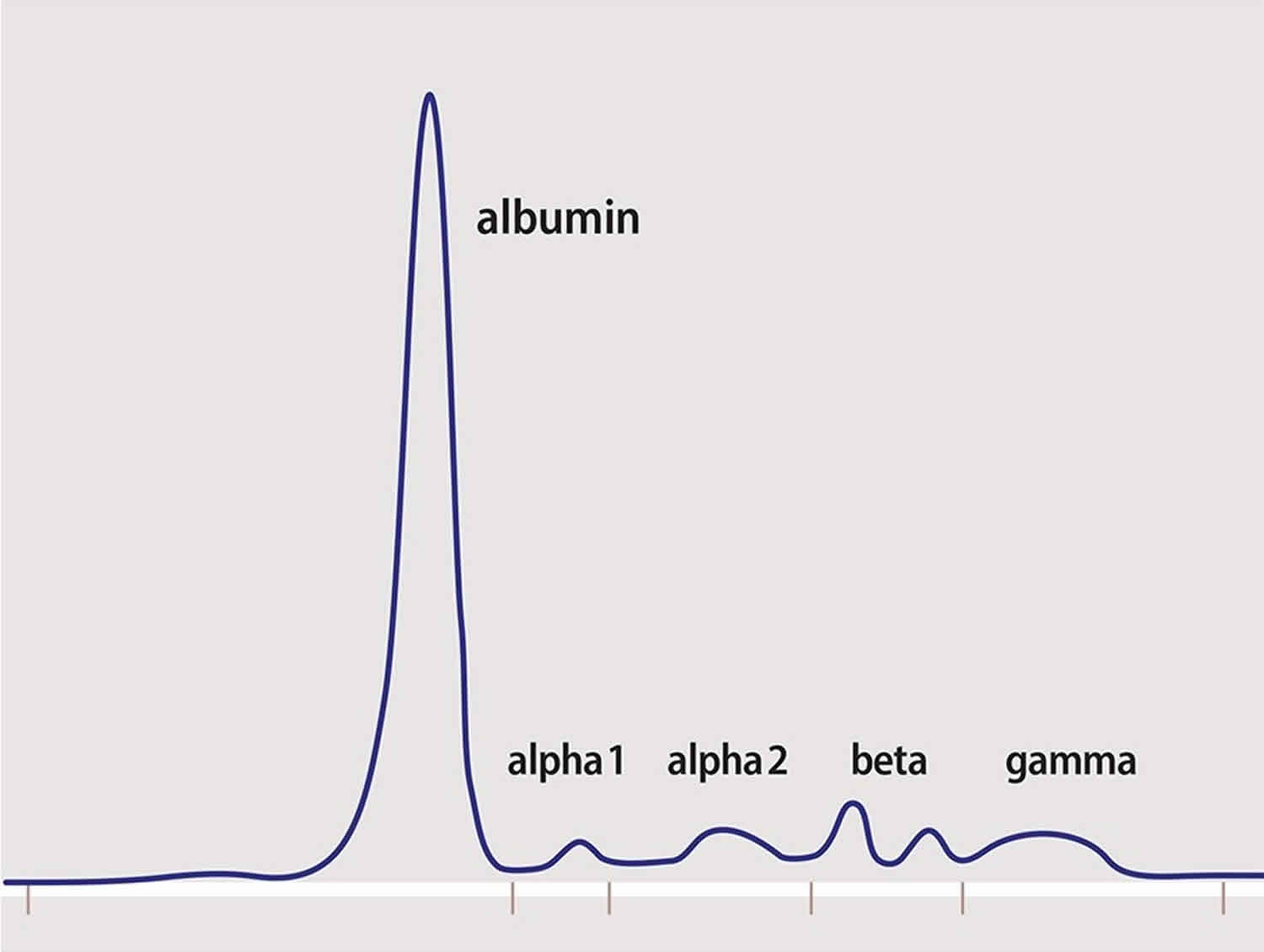
The graph number one (Figure 2) represents a normal serum protein electrophoresis result. It shows:
- a peak in the measurement of albumin (the most plentiful protein in the blood)
- lower levels of the other proteins, grouped into areas labeled alpha 1 and 2
- beta (with two bumps also known as 1 and 2)
- gamma, which is where the antibody proteins lie on the graph
Figure 3 represents the result for a patient with myeloma. In addition to the spike for albumin, there is another tall spike. The red arrow in the gamma region of the graph indicates this spike.
A pathologist measures the area under the spike, or curve, and subtracts the normal level of gamma globulins from the total. The result is your level of monoclonal protein (M-protein).
Serum protein electrophoresis and urine protein electrophoresis tell your doctor how MUCH monoclonal protein there is, but not the type. Monoclonal protein is the output of myeloma cells in most people with myeloma. Yet, every person’s myeloma is unique. The output of monoclonal protein can vary from patient to patient. It can also can vary in how that amount relates to the behavior of the myeloma.
Serum protein electrophoresis and urine protein electrophoresis don’t measure myeloma cells; they measure the output of myeloma cells. People’s myeloma cells don’t reproduce at the same rate or secrete the same amount of protein per cell.
A caveat with serum protein electrophoresis: Immunoglobulin A-type (IgA) myeloma monoclonal protein does not separate out in the gamma region of the graph. It can get “stuck” with the beta or even alpha proteins. Patients with IgA myeloma should discuss the best way to measure their monoclonal protein with their doctors.
Figure 2. Normal serum protein electrophoresis
Figure 3. Multiple myeloma serum protein electrophoresis
Immunofixation electrophoresis of blood or urine
Immunofixation electrophoresis of blood or urine (immunofixation electrophoresis of blood or urine) is the counterpart to serum protein electrophoresis and urine protein electrophoresis. Immunofixation electrophoresis of blood or urine tells your doctor the TYPE of monoclonal protein in your blood and/or urine but not the amount. Immunofixation electrophoresis of blood or urine testing separates proteins by electrical charge. Immunofixation electrophoresis of blood or urine measures only the monoclonal (M protein) — or abnormal —proteins, not the normal (polyclonal) ones
The result is either negative or positive for the presence of a particular type of monoclonal protein.
*Note: Darzalex can influence the results of immunofixation electrophoresis of blood or urine if a patient has IgG Kappa myeloma and is being evaluated for complete response. The patient may be in a very deep complete response, but a tiny band of IgG Kappa will show up on the test.
Quantitative immunoglobulin testing
Quantitative immunoglobulins testing is often done as part of early screening for multiple myeloma. It is usually done if the total protein level is elevated. Quantitative immunoglobulins testing measures total immunoglobulin protein in your blood, both normal and abnormal. If quantitative immunoglobulins testing detects an increase an immunoglobulin, you must undergo further testing with immunofixation electrophoresis of blood or urine. The goal is to see if the increase is from abnormal (monoclonal) protein.
Some doctors also use quantitative immunoglobulins testing to follow patients with IgA myeloma because it’s difficult to assess IgA with serum protein electrophoresis.
Serum free light chain assay
The serum free light chain assay (brand name Freelite®) is used for diagnosis and monitoring of myeloma. Immunoglobulin proteins are made up of two kinds of molecules, heavy chains and light chains (Figure 1 above).
These heavy and light chains are usually bound together as “intact immunoglobulins.” For reasons scientists do not yet know, the plasma cells produce more light chains than heavy chains. The excess, or unbound, light chains circulate freely in the blood. Hence, they are called “free” light chains. These free light chains are present in both healthy individuals and in patients with myeloma and related disorders. Related disorders include:
- monoclonal gammopathy of undetermined significance (MGUS)
- smoldering multiple myeloma
- amyloidosis
- light chain deposition disease
- Waldenström’s macroglobulinemia
Patients with myeloma may learn that their cells secrete:
- both heavy and light chains
- only heavy chains
- only light chains
Some patients, when assessed by serum protein electrophoresis, appear to secrete no M-protein at all. These patients’ myeloma cells secrete no heavy chain protein, only a very small amount of light chain protein. The Freelite test is used for patients who:
- only secrete light chains, which is often called “Bence-Jones myeloma.” (The name “Bence-Jones myeloma is for the name of the doctor who first found and identified light chain protein in the urine).
- secrete both heavy and light chains
- secrete very low levels of protein, also known as “oligosecretory myeloma”
The Freelite assay is also used to:
- diagnose and monitor patients with MGUS, a non-cancerous elevation in monoclonal protein. The Freelite assay can help to assess if a patient’s MGUS may develop into active myeloma.
- monitor patients with smoldering multiple myeloma or asymptomatic myeloma.
Serum Heavy and Light Chain Assay
The Hevylite® assay is a blood test that measures the intact immunoglobulins. It measures:
- the intact heavy and light chain protein made by the myeloma cells
- the heavy- and light-chain-bound immunoglobulin protein made by normal plasma cells
If your myeloma protein is, for example, IgA kappa, the intact immunoglobulin that is its normal counterpart will be IgA lambda.
Non-laboratory tests
- X-ray, ordered to help diagnose, stage, and monitor; may detect holes in bones, extent of bone damage, and the number and size of tumors in the bones.
- MRI (magnetic resonance imaging), may be more sensitive than X-ray for evaluating bone destruction.
- CT (computed tomography)/PET (positron emission tomography), may be used to look for bone tumors when an x-ray result is negative but an individual still has bone pain.
Multiple myeloma staging
Multiple myeloma staging helps to determine a person’s prognosis and allows the person and their healthcare practitioner to develop an individualized monitoring and treatment plan. Staging evaluates the:
- Amount of abnormal immunoglobulin being produced
- Amount of calcium in the blood
- Degree and severity of bone damage
- Extent of anemia
There are different staging systems available to assess the amount of tumor tissue present (tumor burden) and organ dysfunction. Some test results, such as blood levels of beta-2 microglobulin and albumin, are especially important in myeloma staging.
Multiple myeloma treatment
At this time, multiple myeloma is not considered curable, although current treatments may produce a complete remission (disappearance but not cure of the disease) in some people. The goals of treatment are to relieve pain and other symptoms, to decrease the amount of cancer present or eliminate it, to slow the progress of the disease, and/or to detect and minimize complications as they occur.
People who do not have significant signs or symptoms are monitored but may not receive any treatment. Healthcare practitioners generally recommend that people with multiple myeloma stay as active as possible to help preserve the calcium in their bones and drink plenty of fluids to help with kidney function.
Complications such as infections, anemia, and bleeding should be promptly addressed with measures such as antibiotics and, when necessary, blood transfusions. Other supportive treatments may include injections of immunoglobulins to help fight infections and plasmapheresis to remove excess M protein from the blood. Plasmapheresis helps reduce the thickness (viscosity) of the blood.
If treatment is indicated, a combination of the following may be used:
- Bisphosphonates—drugs that slow the weakening of bones
- Chemotherapy—drugs used to control or destroy cancerous plasma cells
- Targeted therapy—drugs that target the specific cancer’s cells, genes or proteins
- Radiation therapy—may be used to treat areas of bone that has not responded to chemotherapy
- Stem cell transplantation—this procedure involves killing cells within the bone marrow, including the myeloma cells, and then giving the patient healthy stem cells
When signs or symptoms appear, the treatment of multiple myeloma may be done in phases:
- Induction therapy: This is the first phase of treatment. Its goal is to reduce the amount of disease, and may include one or more of the following:
- Corticosteroid therapy.
- Biologic therapy with lenalidomide, pomalidomide, or thalidomide therapy.
- Targeted therapy with proteasome inhibitors (bortezomib, carfilzomib, and ixazomib) or monoclonal antibodies (daratumumab and elotuzumab).
- Chemotherapy.
- Histone deacetylase inhibitor therapy with panobinostat.
- A clinical trial of different combinations of treatment.
- Consolidation chemotherapy: This is the second phase of treatment. Treatment in the consolidation phase is to kill any remaining cancer cells. High-dose chemotherapy is followed by either:
- One autologous stem cell transplant, in which the patient’s stem cells from the blood or bone marrow are used; or
- Two autologous stem cell transplants followed by an autologous or allogeneic stem cell transplant, in which the patient receives stem cells from the blood or bone marrow of a donor; or
- One allogeneic stem cell transplant.
- Maintenance therapy: After the initial treatment, maintenance therapy is often given to help keep the disease in remission for a longer time. Several types of treatment are being studied for this use, including the following:
- Chemotherapy.
- Biologic therapy with interferon.
- Corticosteroid therapy.
- Lenalidomide therapy.
- Targeted therapy with a proteasome inhibitor (bortezomib).
Refractory multiple myeloma
Treatment of refractory multiple myeloma may include the following:
- Watchful waiting for patients whose disease is stable.
- A different treatment than treatment already given, for patients whose tumor kept growing during treatment. (See Multiple Myeloma treatment options.)
- A clinical trial of a new therapy.
- Types of Myeloma. https://www.myeloma.org/multiple-myeloma/newly-diagnosed/types-of-myeloma[↩]